Conceptual Framework for Rape Survivors Diagnosed with PTSD in the North West Province of South Africa
Abstract
1. Introduction
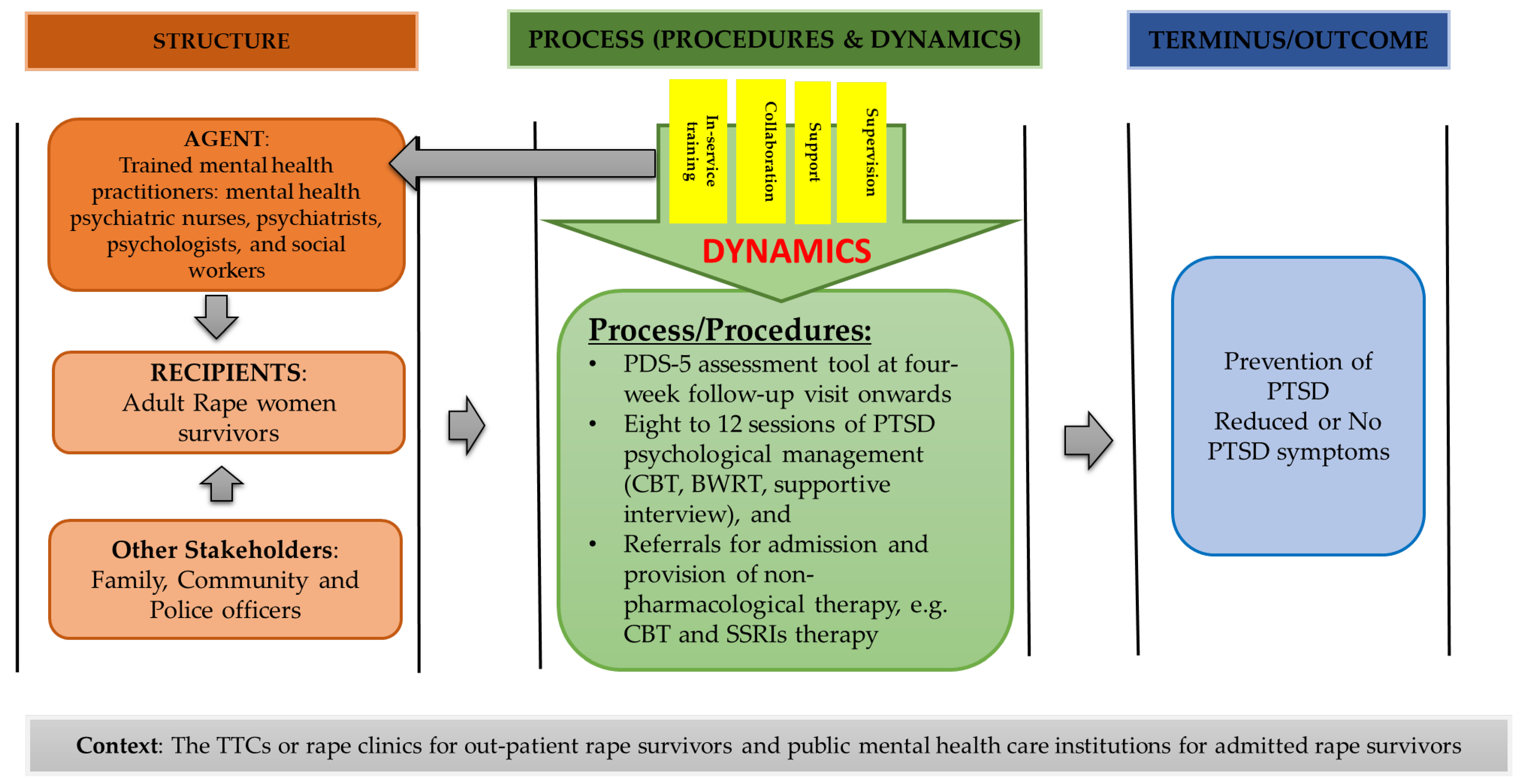
1.1. Conceptual Framework
1.2. Structure
1.3. Process
1.4. Outcome
1.5. Context
2. Methods
2.1. Study Design
2.2. Population and Sampling
2.3. Data Collection Procedure
2.4. Data Analysis
2.5. Ethical Considerations
3. Results and Discussion
3.1. Structure
3.2. Process and Outcome
“Mental health care practitioners working in TCCs must book rape survivors for follow-up at six weeks to assess them for PTSD symptoms using tools that are linked to statistical diagnostic manual, for example PCL-s and PDS-5…”(identified as a female, psychologist, 20 years of service).
“…as such the same diagnostic tools must be used to assess them whey are admitted in psychiatric mental health care institutions”(identified as a male, psychiatrist, 28 years of service).
“…it is procedurally correct for mental health care practitioners to manage adult rape women survivors diagnosed with PTSD through using Cognitive Behavioural Therapy (CBT), Eye Movement Desensitization and Reprocessing Therapy (EMDR), exposure therapy, Cognitive Processing Therapy (CPT) or supportive counselling for effective management or remission of symptoms at least for 12 weeks”[23].
“The is a need to give rape survivors diagnosed with PTSD and admitted at the hospital selective serotherapy (SSRIs)”(identified male, psychiatrist, nine years of service).
“Have at least one or two sessions of Brain Working Recursive Therapy (BWRT) with rape survivors diagnosed with PTSD”(identified as a female, psychologist, 5 years of service).
“There is a need for experienced mental health care practitioners to support and supervise nurses and social workers caring for rape survivors on how to assess, diagnose and manage rape survivors with PTSD”(Identified female, psychiatric nurse, six years of service and identified female, psychologist, nine years of service).
“…also, mental health care practitioners working in public health care institutions should avail themselves to work in collaboration with TCCs staff members. For example, they may have a special day of working with TCCs staff to provide support and supervising them on how to assess and manage rape women survivors for PTSD when scheduled for follow-care until such time they are competent to assess and manage rape survivors on their own”(Identified female, psychiatric nurse, 14 years of service and identified female, psychiatric nurse, seven years of service).
“There is a need for a psychologist in public mental health care institutions to provide in-service training for nurses and social workers working in TCCs on how to assess and manage rape survivors diagnosed with PTSD”(identified female, social worker, 11 years of service).
“Also, the in-service training must be done for mental health care practitioners responsible for assessing and managing rape survivors diagnosed with PTSD in case there are new treatment modalities that can be used to manage rape survivors diagnosed with PTSD, including new assessment scales when adjusted according to the new diagnostic and statistical manual of mental health disorders”(identified male, psychologist, eight years of service).
3.3. Context
4. Practical Implications of the Study
5. Limitations
6. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- South African Police Services. Minister Bheki Cele: Quarter One Crime Statistics 2022/2023. Available online: https://www.gov.za/speeches/minister-bheki-cele-quarter-one-crime-statistics-20222023-19-aug-2022-0000 (accessed on 23 August 2022).
- Wyatt, G.E.; Davhana-Maselesele, M.; Zhang, M.; Wong, L.H.; Nicholson, F.; Sarkissian, A.; Makhado, L.; Myers, H.F. A longitudinal study of the aftermath of rape among rural South African women. Psychol. Trauma 2017, 9, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Olckers, C.J. A training programme in the DSM system for social workers. Ph.D. thesis, University of Pretoria, Pretoria, South Africa, 6 September 2013. [Google Scholar]
- Sepeng, N.V.; Makhado, L. Correlates of Post-Traumatic Stress Disorder diagnosis among rape survivors: Results and implications of a South African study. J. Psychol. Afr. 2018, 28, 468–471. [Google Scholar] [CrossRef]
- Bougard, N.B.; Booyens, K. Adult female rape victims’ views about the Thuthuzela Care Centres: A South African multidisciplinary service delivery model. Acta Criminol. Afr. J. Criminol. Vict. 2015, 2015, 19–33. [Google Scholar]
- Olckers, C.; Enslin, C. Psychological ownership in relation to workplace trust and turnover intent. J. Psychol. Africa 2016, 26, 119–126. [Google Scholar] [CrossRef]
- Le Page, K. What Is A Community Mental Health Team? Health Field. 2010. Available online: http://kate-le-page.suite101.com/what-is-a-community-mentalhealth-team (accessed on 18 May 2022).
- Wheeler, K. Psychotherapy for the Advanced Practice Psychiatric Nurse: A How-To Guide for Evidence-Based Practice; Springer Publishing Company: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Chetty, D.; Hoque, M.E. Effectiveness of a nurse facilitated cognitive group intervention among mild to moderately-depressed-women in KwaZulu-Natal, South Africa. Afr. J. Psychiatry 2013, 16, 29–34. [Google Scholar] [CrossRef][Green Version]
- Moultrie, A.; Kleintjes, S. Women’s mental health in South Africa: Women’s health. S. Afr. Health Rev. 2006, 2006, 347–366. [Google Scholar]
- Kakuma, R.; Minas, H.; Van Ginneken, N.; Dal Poz, M.R.; Desiraju, K.; Morris, J.E.; Saxena, S.; Scheffler, R.M. Human resources for mental health care: Current situation and strategies for action. Lancet 2011, 378, 1654–1663. [Google Scholar] [CrossRef]
- Galvin, M.; Byansi, W. A systematic review of task shifting for mental health in sub-Saharan Africa. Int. J. Ment. Health 2020, 49, 336–360. [Google Scholar] [CrossRef]
- Lund, C.; Schneider, M.; Garman, E.C.; Davies, T.; Munodawafa, M.; Honikman, S.; Bhana, A.; Bass, J.; Bolton, P.; Dewey, M.; et al. Task-sharing of psychological treatment for antenatal depression in Khayelitsha, South Africa: Effects on antenatal and postnatal outcomes in an individual randomised controlled trial. Behav. Res. Ther. 2020, 130, 103466. [Google Scholar] [CrossRef]
- Mansfield, E. A CF for psychiatric-mental health nursing. J. Psychosoc. Nurs. Ment. Health Serv. 1980, 18, 34–41. [Google Scholar] [CrossRef]
- Hoeffer, B. Issues from the Advisory Board’s Perspective: A Sourcebook on Research in Psychiatric Mental Health Nursing; WICHE: Boulder, CO, USA, 1983; pp. 11–12.
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581. [Google Scholar] [CrossRef] [PubMed]
- Sanders, S.H.; Harden, R.N.; Vicente, P.J. Evidence-based clinical practice guidelines for interdisciplinary rehabilitation of chronic non-malignant pain syndrome patients. Pain Pract. 2005, 5, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Gatchel, R.J. Comorbidity of chronic pain and mental health disorders: The biopsychosocial perspective. Am. Psychol. 2004, 59, 795. [Google Scholar] [CrossRef] [PubMed]
- Bosco, M.A.; Gallinati, J.L.; Clark, M.E. Conceptualizing and treating comorbid chronic pain and PTSD. Pain Res. Treat. 2013, 2013, 174728. [Google Scholar] [CrossRef]
- Dickoff, J.; James, P.; Wiedenbach, E. Theory in a Practice Discipline: Part I—Practice Oriented Theory. Nurs Res. 1968, 17, 415–435. [Google Scholar] [CrossRef]
- Donabedian, A. Evaluating the quality of medical care. Milbank Meml. Fund Q. 1966, 44, 166–206. [Google Scholar] [CrossRef]
- Sepeng, N.V.; Makhado, L. Present practices of rape care management in Thuthuzela Care Centres of the North West Province. J. Psychol. Afr. 2019, 29, 516–519. [Google Scholar] [CrossRef]
- Sepeng, N.V.; Makhado, L.; Sehularo, L.A. Psychological management of rape survivors suffering from post-traumatic stress disorder: Practitioners’ perspectives. Afr. J. Nurs. Midwifery 2019, 21, 22. [Google Scholar] [CrossRef]
- American Psychiatric association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Edmonds, W.A.; Kennedy, T.D. An Applied Guide to Research Designs: Quantitative, Qualitative, and Mixed Methods; Sage Publications: New York, NY, USA, 2016. [Google Scholar]
- Foa, E.B.; McLean, C.P.; Zang, Y.; Zhong, J.; Powers, M.B.; Kauffman, B.Y.; Rauch, S.; Porter, K.; Knowles, K. Psychometric properties of the Posttraumatic Diagnostic Scale for DSM–5 (PDS–5). Psychol. Assess. 2016, 28, 1166. [Google Scholar] [CrossRef]
- Patel, A.; Panchal, H.; Piotrowski, Z.H.; Patel, D. Comprehensive medical care for victims of sexual assault: A survey of Illinois hospital emergency departments. Contraception 2008, 77, 426–430. [Google Scholar] [CrossRef]
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research; Sage Publications: New York, NY, USA, 2017. [Google Scholar]
- Mental Health Care Act 17 of 2002, Pretoria: Department of Health. Available online: https://www.gov.za/sites/default/files/gcis_document/201409/a17-02.pdf (accessed on 4 September 2021).
- Department of Social Development, South Africa. 1997. Available online: https://www.westerncape.gov.za/your_gov/61/documents/acts/1997 (accessed on 3 November 2022).
- Gordon, J.S. Helping Survivors of Domestic Violence: The Effectiveness of Medical, Mental Health, and Community Services; Routledge: London, UK, 2016. [Google Scholar] [CrossRef]
- Welch, J.; Mason, F. Rape and sexual assault. BMJ 2007, 334, 1154–1158. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, C.T.; Cestodio, V.; Porter, K.J.; Marchant, K.M. The Moderating Roles of Emotion Regulation and Coping Self-Efficacy on the Association between PTSD Symptom Severity and Drug Use among Female Sexual Assault Survivors. In Psychological Trauma: Theory, Research, Practice, and Policy; American Psychological Association: Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- Foa, E.B.; McLean, C.P. The efficacy of exposure therapy for anxiety-related disorders and its underlying mechanisms: The case of OCD and PTSD. Annu. Rev. Clin. Psychol. 2016, 12, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Watts, T. BWRT: Reboot Your Life with BrainWorking Recursive Therapy; Crown House Publishing Ltd.: Carmarthen, UK, 2022. [Google Scholar]
- Ochberg, F. Post-Traumatic Therapy and Victims of Violence; Routledge: London, UK, 2013. [Google Scholar]
- National Collaborating Centre for Mental Health. Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care; NICE Clinical Guidelines [NG26]; Gaskell: Leicester, UK, 2005. Available online: http://www.ncbi.nlm.nih.gov/books/NBK56494/ (accessed on 8 June 2022).
- Kirkpatrick, H.A.; Heller, G.M. Post-traumatic stress disorder: Theory and treatment update. Int. J. Psychiatry Med. 2014, 47, 337–346. [Google Scholar] [CrossRef] [PubMed]
- McLean, C.P.; Foa, E.B. Prolonged exposure therapy for post-traumatic stress disorder: A review of evidence and dissemination. Expert Rev. Neurother. 2011, 11, 1151–1163. [Google Scholar] [CrossRef]
- Davis, R.G.; Ressler, K.J.; Schwartz, A.C.; Stephens, K.J.; Bradley, R.G. Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2008, 21, 218–222. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health and Development: Targeting People with Mental Health Conditions as a Vulnerable Group; WHO: Geneva, Switzerland, 2010; p. 74. Available online: https://pesquisa.bvsalud.org/portal/resource/pt/mis-31700 (accessed on 18 May 2022).
- Patel, V. Mental health in low-and middle-income countries. Br. Med. Bull. 2007, 81, 81–96. [Google Scholar] [CrossRef]
- Marsay, G. BrainWorking Recursive Therapy® a thoroughly modern therapy. Ment. Health Matters 2020, 7, 40–41. [Google Scholar]
- Wangamati, C.K.; Thorsen, V.C.; Gele, A.A.; Sundby, J. Post rape care services to minors in Kenya: Are the services healing or hurting survivors. Int. J. Women’s Health 2016, 8, 249. [Google Scholar] [CrossRef]
- Moylan, C.A.; Lindhorst, T. Institutionalising an ethic of coordinated care for rape victims: Exploring processes of legitimacy and decoupling in sexual assault response teams. Soc. Serv. Rev. 2015, 89, 138–165. [Google Scholar] [CrossRef]
- Abrahams, N.; Gevers, A. A rapid appraisal of the status of mental health support in post-rape care services in the Western Cape. S. Afr. J. Psychiatry 2017, 23, a959. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sepeng, N.V.; Makhado, T.G.; Makhado, L. Conceptual Framework for Rape Survivors Diagnosed with PTSD in the North West Province of South Africa. Healthcare 2023, 11, 127. https://doi.org/10.3390/healthcare11010127
Sepeng NV, Makhado TG, Makhado L. Conceptual Framework for Rape Survivors Diagnosed with PTSD in the North West Province of South Africa. Healthcare. 2023; 11(1):127. https://doi.org/10.3390/healthcare11010127
Chicago/Turabian StyleSepeng, Nombulelo Veronica, Thendo Gertie Makhado, and Lufuno Makhado. 2023. "Conceptual Framework for Rape Survivors Diagnosed with PTSD in the North West Province of South Africa" Healthcare 11, no. 1: 127. https://doi.org/10.3390/healthcare11010127
APA StyleSepeng, N. V., Makhado, T. G., & Makhado, L. (2023). Conceptual Framework for Rape Survivors Diagnosed with PTSD in the North West Province of South Africa. Healthcare, 11(1), 127. https://doi.org/10.3390/healthcare11010127





