The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study
Abstract
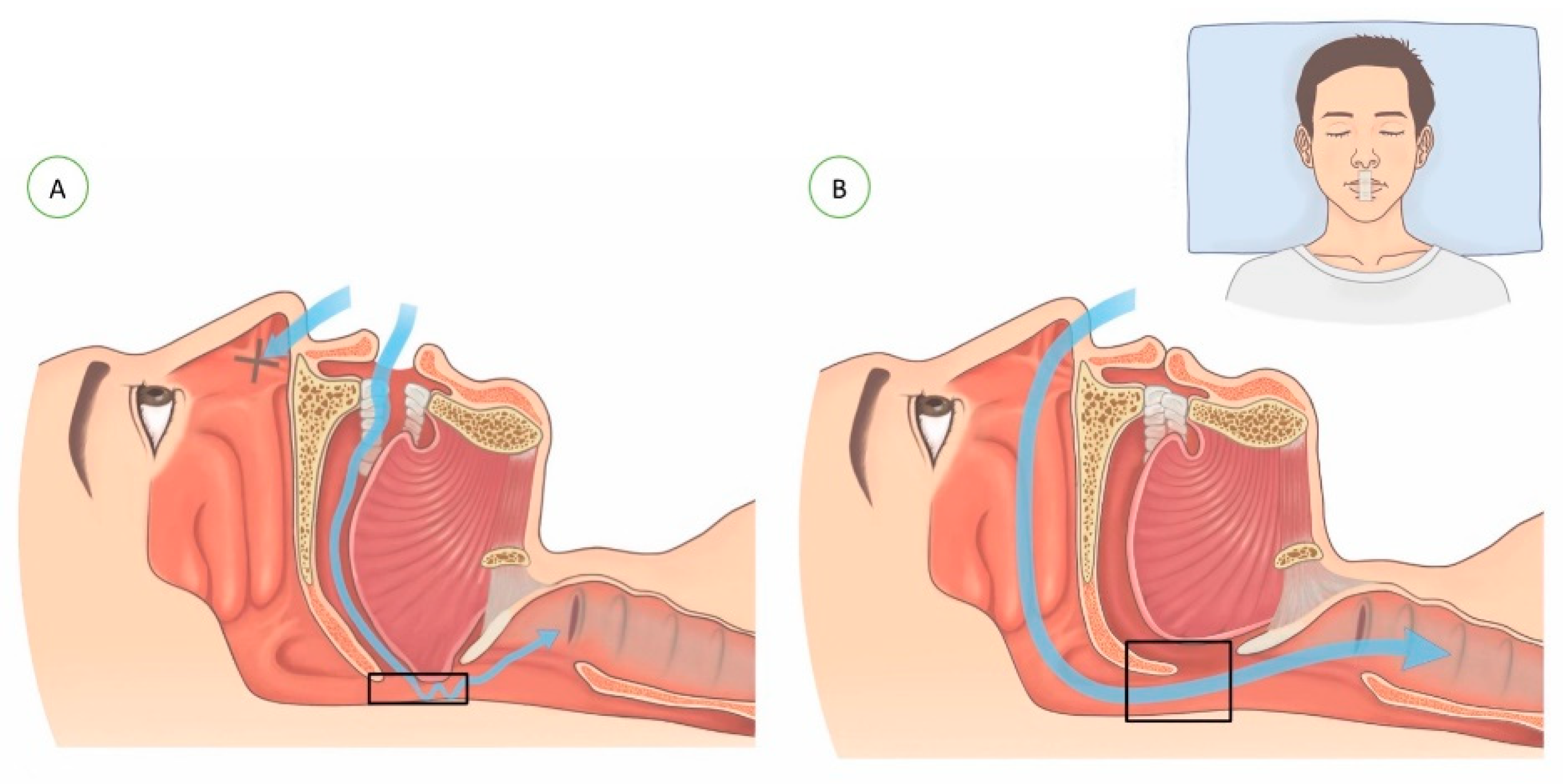
:1. Introduction
2. Methods
2.1. Ethics Statement
2.2. Study Population
2.3. Study Design
2.4. Home Sleep Test (HST)
2.5. Mouth-Taping
2.6. Data Collection
2.7. Statistical Analysis
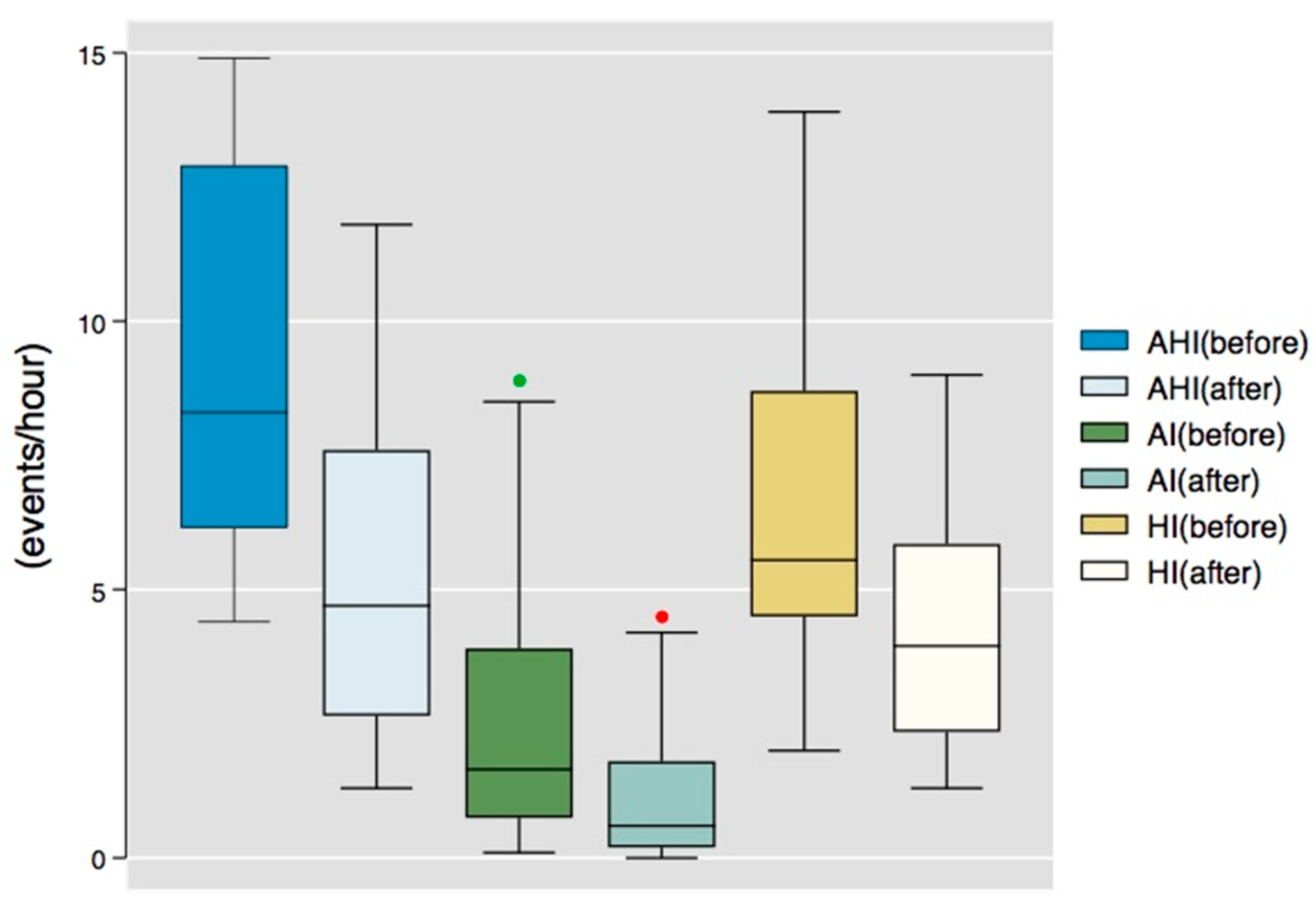
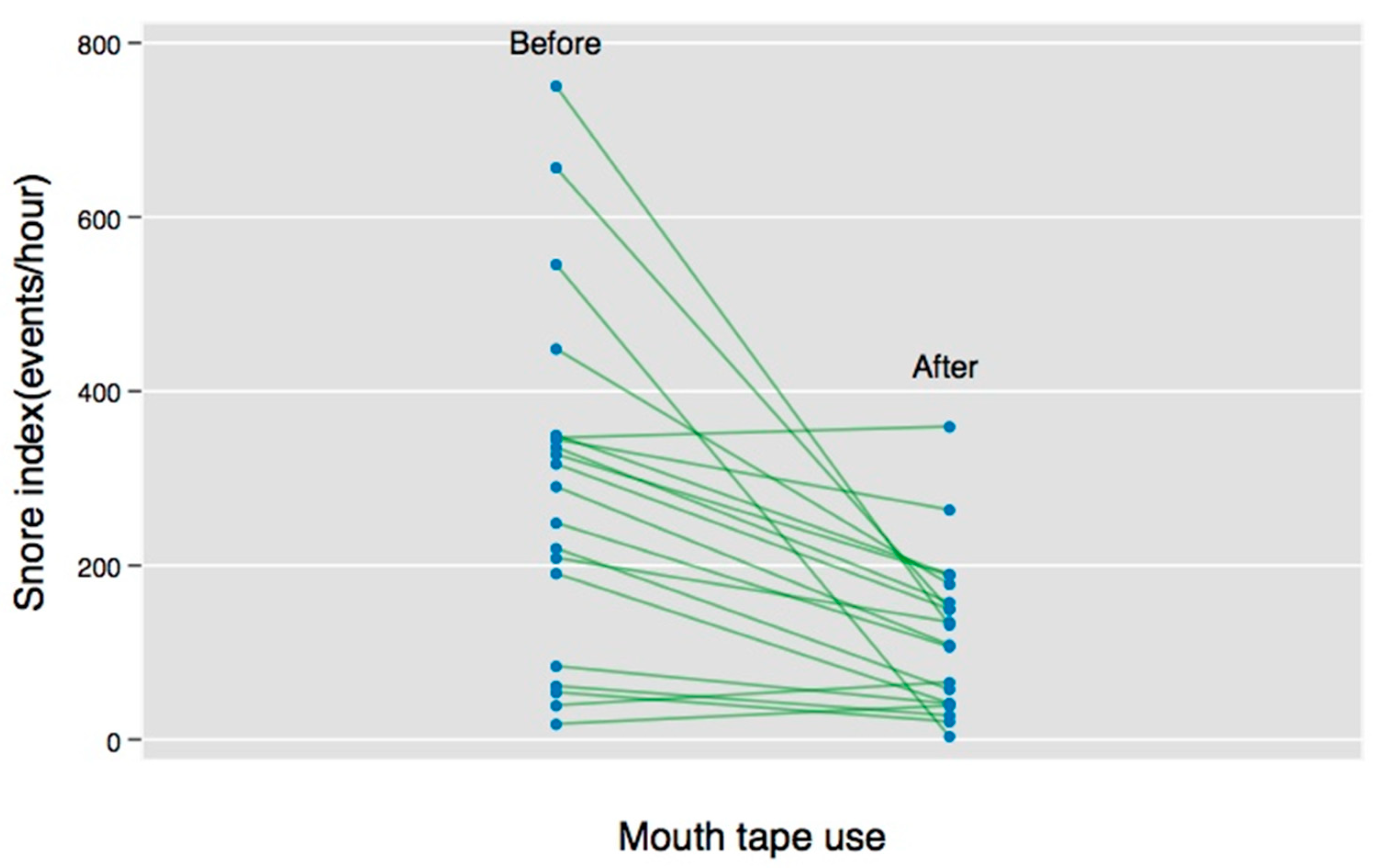
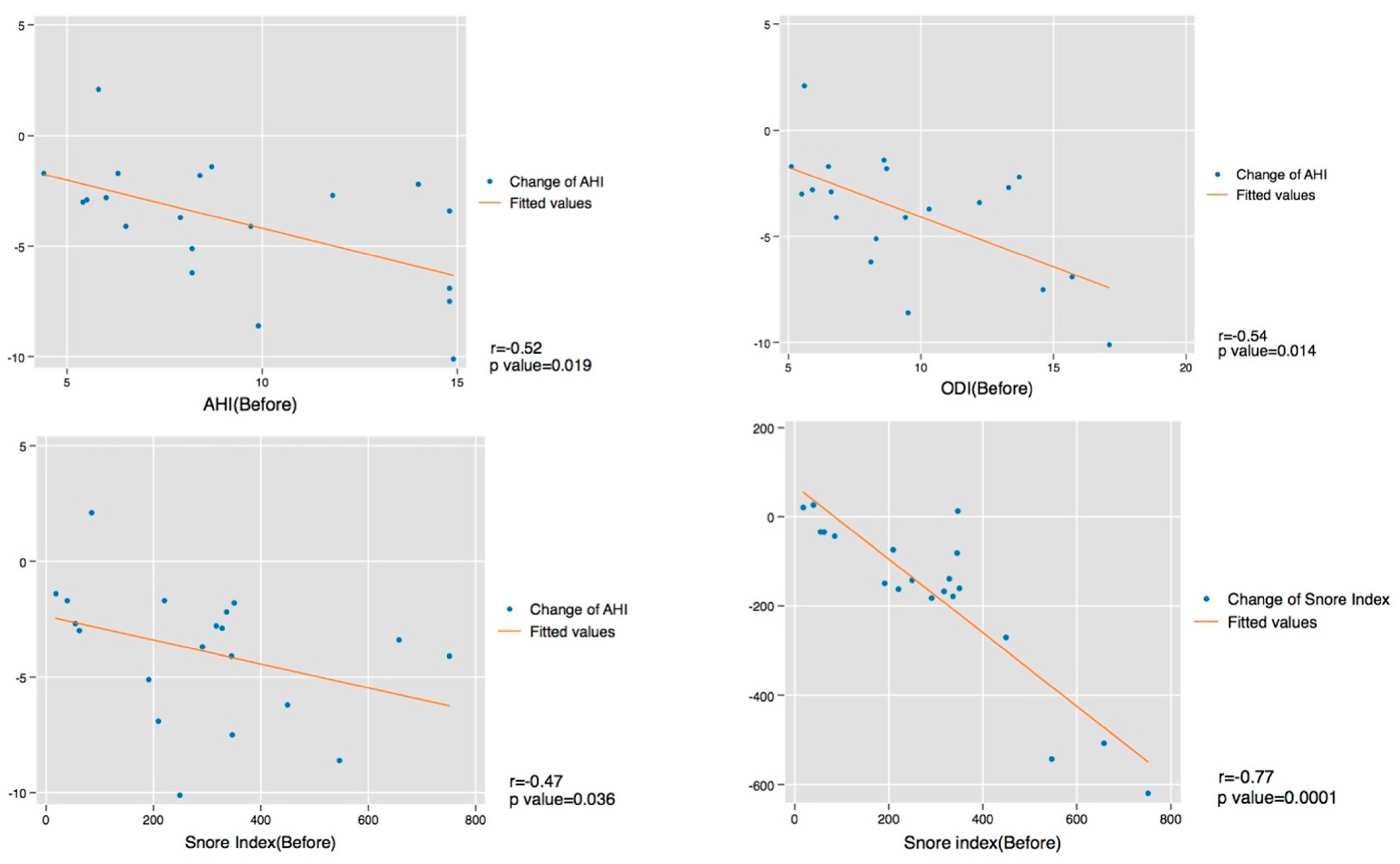
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, S.H.; Choi, J.H.; Shin, C.; Lee, H.M.; Kwon, S.Y.; Lee, S.H. How does open-mouth breathing influence upper airway anatomy? Laryngoscope 2007, 117, 1102–1106. [Google Scholar] [CrossRef] [PubMed]
- Georgalas, C. The role of the nose in snoring and obstructive sleep apnoea: An update. Eur. Arch. Otorhinolaryngol. 2011, 268, 1365–1373. [Google Scholar] [CrossRef] [PubMed]
- Warren, D.W.; Hairfield, W.M.; Seaton, D.; Morr, K.E.; Smith, L.R. The relationship between nasal airway size and nasal-oral breathing. Am. J. Orthod. Dentofacial. Orthop. 1988, 93, 289–293. [Google Scholar] [CrossRef]
- Meurice, J.C.; Marc, I.; Carrier, G.; Sériès, F. Effects of mouth opening on upper airway collapsibility in normal sleeping subjects. Am. I Respir. Crit. Care Med. 1996, 153. [Google Scholar] [CrossRef]
- Koutsourelakis, I.; Vagiakis, E.; Roussos, C.; Zakynthinos, S. Obstructive sleep apnoea and oral breathing in patients free of nasal obstruction. Eur. Respir. J. 2006, 28, 1222–1228. [Google Scholar] [CrossRef]
- Kim, E.J.; Choi, J.H.; Kim, K.W.; Kim, T.H.; Lee, S.H.; Lee, H.M.; Shin, C.; Lee, K.Y.; Lee, S.H. The impacts of open-mouth breathing on upper airway space in obstructive sleep apnea: 3-D MDCT analysis. Eur. Arch. Otorhinolaryngol. 2011, 268, 533–539. [Google Scholar] [CrossRef]
- Harari, D.; Redlich, M.; Miri, S.; Hamud, T.; Gross, M. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope 2010, 120, 2089–2093. [Google Scholar] [CrossRef]
- Bachour, A.; Maasilta, P. Mouth breathing compromises adherence to nasal continuous positive airway pressure therapy. Chest 2004, 126, 1248–1254. [Google Scholar] [CrossRef]
- Poulet, C.; Veale, D.; Arnol, N.; Lévy, P.; Pepin, J.L.; Tyrrell, J. Psychological variables as predictors of adherence to treatment by continuous positive airway pressure. Sleep Med. 2009, 10, 993–999. [Google Scholar] [CrossRef]
- Madeiro, F.; Andrade, R.G.S.; Piccin, V.S.; Pinheiro, G.D.L.; Moriya, H.T.; Genta, P.R.; Lorenzi-Filho, G. Transmission of Oral Pressure Compromises Oronasal CPAP Efficacy in the Treatment of OSA. Chest 2019, 156, 1187–1194. [Google Scholar] [CrossRef]
- Bachour, A.; Hurmerinta, K.; Maasilta, P. Mouth closing device (chinstrap) reduces mouth leak during nasal CPAP. Sleep Med. 2004, 5, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.W.; Young, T.H. Novel porous oral patches for patients with mild obstructive sleep apnea and mouth breathing: A pilot study. Otolaryngol. Head Neck Surg. 2015, 152, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Erman, M.K.; Stewart, D.; Einhorn, D.; Gordon, N.; Casal, E. Validation of the ApneaLink for the Screening of Sleep Apnea: A Novel and Simple Single-Channel Recording Device. J. Clin. Sleep Med. 2007, 03, 387–392. [Google Scholar] [CrossRef]
- Cho, J.H.; Kim, H.J. Validation of ApneaLink Plus for the diagnosis of sleep apnea. Sleep Breath 2017, 21, 799–807. [Google Scholar] [CrossRef]
- Marchi, N.A.; Ramponi, C.; Hirotsu, C.; Haba-Rubio, J.; Lutti, A.; Preisig, M.; Marques-Vidal, P.; Vollenweider, P.; Kherif, F.; Heinzer, R.; et al. Mean Oxygen Saturation during Sleep Is Related to Specific Brain Atrophy Pattern. Ann. Neurol. 2020, 87, 921–930. [Google Scholar] [CrossRef]
- Temirbekov, D.; Gunes, S.; Yazici, Z.M.; Sayin, I. The Ignored Parameter in the Diagnosis of Obstructive Sleep Apnea Syndrome: The Oxygen Desaturation Index. Turk Arch. Otorhinolaryngol. 2018, 56, 1–6. [Google Scholar] [CrossRef]
- Hsu, Y.B.; Lan, M.Y.; Huang, Y.C.; Kao, M.C.; Lan, M.C. Association Between Breathing Route, Oxygen Desaturation, and Upper Airway Morphology. Laryngoscope 2021, 131, E659–E664. [Google Scholar] [CrossRef]
- Mador, M.J.; Kufel, T.J.; Magalang, U.J.; Rajesh, S.K.; Watwe, V.; Grant, B.J. Prevalence of Positional Sleep Apnea in Patients Undergoing Polysomnography. Chest 2005, 128, 2130–2137. [Google Scholar] [CrossRef]
- Richard, W.; Kox, D.; den Herder, C.; Laman, M.; van Tinteren, H.; de Vries, N. The role of sleep position in obstructive sleep apnea syndrome. Eur. Arch. Otorhinolaryngol. 2006, 263, 946–950. [Google Scholar] [CrossRef]
- Sunwoo, W.S.; Hong, S.L.; Kim, S.W.; Park, S.J.; Han, D.H.; Kim, J.W.; Lee, C.H.; Rhee, C.S. Association between Positional Dependency and Obstruction Site in Obstructive Sleep Apnea Syndrome. Clin. Exp. Otorhinolaryngol. 2012, 5, 218–221. [Google Scholar] [CrossRef]
- Varghese, L.; Rebekah, G.; N., P.; Oliver, A.; Kurien, R. Oxygen desaturation index as alternative parameter in screening patients with severe obstructive sleep apnea. Sleep Sci. 2022, 15, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Jau, J.Y.; Kuo, T.B.J.; Li, L.P.H.; Chen, T.Y.; Lai, C.T.; Huang, P.H.; Yang, C.C.H. Mouth puffing phenomena of patients with obstructive sleep apnea when mouth-taped: Device’s efficacy confirmed with physical video observation. Sleep Breath 2022. [Google Scholar] [CrossRef] [PubMed]
- Foellner, S.; Guth, P.; Jorde, I.; Lucke, E.; Ganzert, C.; Stegemann-Koniszewski, S.; Schreiber, J. Prevention of leakage due to mouth opening through applying an oral shield device (Sominpax) during nasal CPAP therapy of patients with obstructive sleep apnea. Sleep Med. 2020, 66, 168–173. [Google Scholar] [CrossRef] [PubMed]
| n (%) or Median (IQR) | |
|---|---|
| Age (in years) | 38 (30–43) |
| Sex (male/female) | 19 (95.0%)/1 (5.0%) |
| Height (cm) | 175 (170.9–177.25) |
| Weight (kg) | 74 (67.7–79.5) |
| BMI (kg/m2) | 24.5 (23.6–26.0) |
| Mouth-Breathing | Nasal-Breathing | Changes (Percentage %) † | |||||
|---|---|---|---|---|---|---|---|
| HST Parameters | Median | IQR | Median | IQR | Median | IQR | p-Value |
| AHI (event/h) | 8.3 | 6.2–12.9 | 4.7 | 2.7–7.6 | −47% | −59%~−23% | 0.0002 |
| AI (event/h) | 1.7 | 0.8–3.9 | 0.6 | 0.2–1.8 | −51% | −76%~−18% | 0.002 |
| HI (event/h) | 5.6 | 4.5–8.7 | 4 | 2.4–5.9 | −44% | −56%~−14% | 0.003 |
| Supine AHI (event/h) | 9.4 | 7.3–15.7 | 5.5 | 3.8–8.9 | −41% | −54%~−41% | 0.0001 |
| Non-supine AHI (event/h) | 3.2 | 0.1–5.0 | 0.6 | 0.1–2.2 | −55% | −95%~−44% | 0.03 |
| Mean saturation (%) | 95 | 94.5–95.5 | 95 | 94.5–96 | 0% | −1%~1% | 0.9 |
| Lowest saturation (%) | 82.5 | 80.5–88 | 87 | 84–89.5 | 2% | −1%~8% | 0.049 |
| 90% saturation (%) | 1 | 0–2.5 | 0 | 0–1 | −67% | −100%~0% | 0.12 |
| ODI (event/h) | 8.7 | 6.6–12.8 | 5.8 | 3.3–8.1 | −36% | −58%~−20% | 0.0003 |
| Snoring index (event/h) | 303.8 | 137.8–348.3 | 121.1 | 41.8–168.4 | −47% | −59%~−23% | 0.0002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-C.; Lu, C.-T.; Cheng, W.-N.; Li, H.-Y. The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare 2022, 10, 1755. https://doi.org/10.3390/healthcare10091755
Lee Y-C, Lu C-T, Cheng W-N, Li H-Y. The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare. 2022; 10(9):1755. https://doi.org/10.3390/healthcare10091755
Chicago/Turabian StyleLee, Yi-Chieh, Chun-Ting Lu, Wen-Nuan Cheng, and Hsueh-Yu Li. 2022. "The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study" Healthcare 10, no. 9: 1755. https://doi.org/10.3390/healthcare10091755
APA StyleLee, Y.-C., Lu, C.-T., Cheng, W.-N., & Li, H.-Y. (2022). The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare, 10(9), 1755. https://doi.org/10.3390/healthcare10091755






