Older Women Who Practiced Physical Exercises before the COVID-19 Pandemic Present Metabolic Alterations and Worsened Functional Physical Capacity after One Year of Social Isolation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Design of the Study
2.2. Combined-Exercise Training Program
2.3. Anthropometric Data
2.4. Physical Tests and Muscle Strength Assessments
2.5. Blood Sample Collection
2.6. Determination of Circulating Lipid and Protein Profiles
2.7. Statistical Analysis
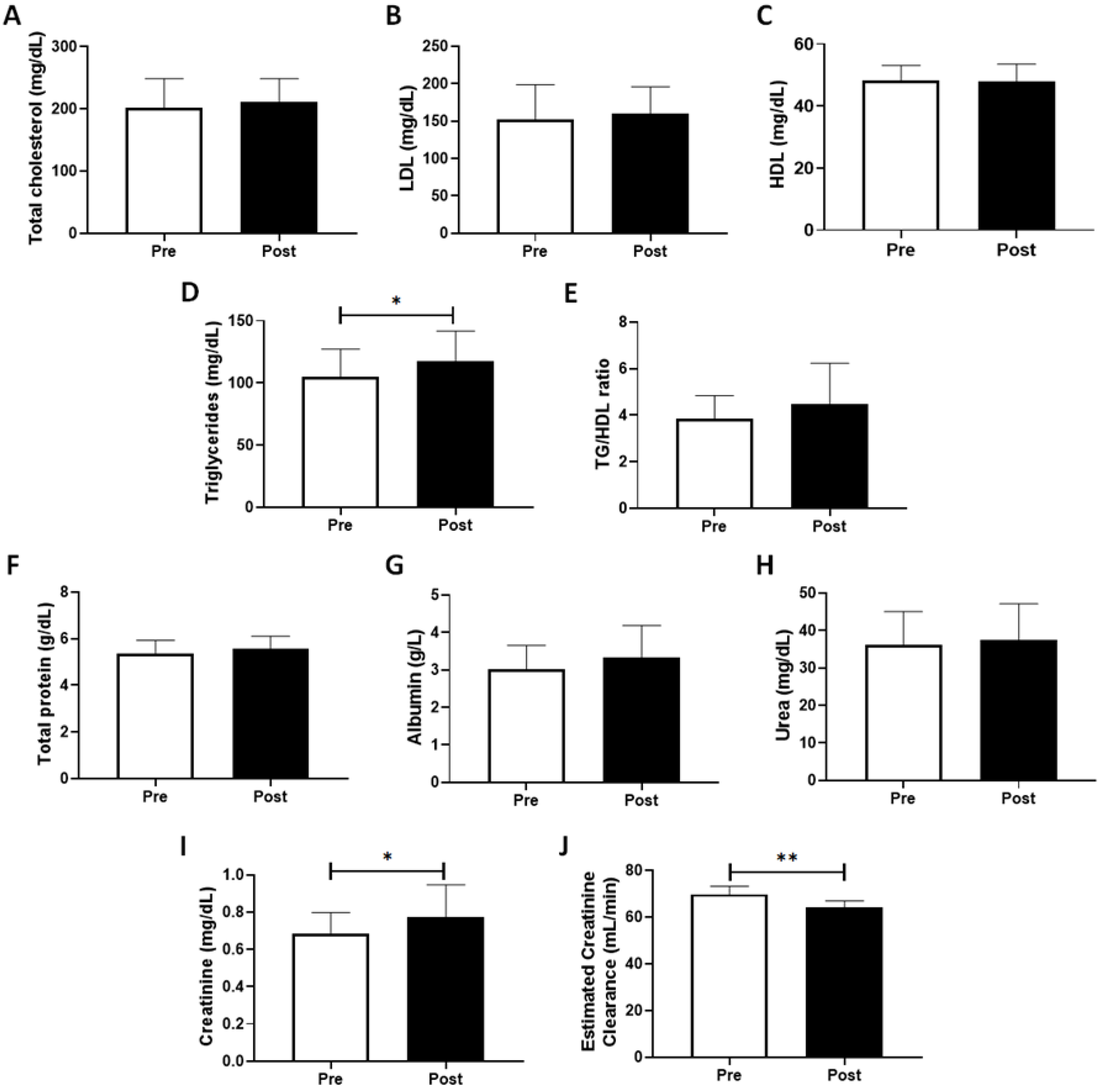
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Heath Organization (WHO). Ageing and Health 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 21 July 2022).
- Oliveira, A.S. Transição demográfica, transição epidemiológica e envelhecimento populacional no Brasil. Hygeia Rev. Bras. Geogr. Médica Saúde 2019, 15, 69–79. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, J.L.; Mañas, A.; García-García, F.J.; Ara, I.; Carnicero, J.A.; Walter, S.; Rodríguez-Mañas, L. Sedentary behaviour, physical activity, and sarcopenia among older adults in the TSHA: Isotemporal substitution model. J. Cachex Sarcopenia Muscle 2019, 10, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Arocha Rodulfo, J.I. Sedentary lifestyle a disease from xxi century. Clin Investig Arter. 2019, 31, 233–240. [Google Scholar] [CrossRef]
- Bellettiere, J.; LaMonte, M.J.; Evenson, K.R.; Rillamas-Sun, E.; Kerr, J.; Lee, I.-M.; Di, C.; Rosenberg, D.E.; Stefanick, M.L.; Buchner, D.M.; et al. Sedentary Behavior and Cardiovascular Disease in Older Women: The Objective Physical Activity and Cardiovascular Health (OPACH) Study. Circulation 2019, 139, 1036–1046. [Google Scholar] [CrossRef] [PubMed]
- Östh, J.; Diwan, V.; Jirwe, M.; Diwan, V.; Choudhary, A.; Mahadik, V.K.; Pascoe, M.; Hallgren, M. Effects of yoga on well-being and healthy ageing: Study protocol for a randomised controlled trial (FitForAge). BMJ Open 2019, 9, e027386. [Google Scholar] [CrossRef] [PubMed]
- Langhammer, B.; Bergland, A.; Rydwik, E. The Importance of Physical Activity Exercise among Older People. BioMed Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef]
- Amirato, G.; Borges, J.; Marques, D.; Santos, J.; Santos, C.; Andrade, M.; Furtado, G.; Rossi, M.; Luis, L.; Zambonatto, R.; et al. L-Glutamine Supplementation Enhances Strength and Power of Knee Muscles and Improves Glycemia Control and Plasma Redox Balance in Exercising Elderly Women. Nutrients 2021, 13, 1025. [Google Scholar] [CrossRef]
- Bachi, A.L.L.; Barros, M.P.; Vieira, R.P.; Rocha, G.A.; De Andrade, P.B.M.; Victorino, A.B.; Ramos, L.R.; Gravina, C.F.; Lopes, J.D.; Vaisberg, M.; et al. Combined Exercise Training Performed by Elderly Women Reduces Redox Indexes and Proinflammatory Cytokines Related to Atherogenesis. Oxid. Med. Cell. Longev. 2019, 2019, 6469213. [Google Scholar] [CrossRef]
- Bachi, A.L.L.; Rocha, G.A.; Sprandel, M.C.O.; Ramos, L.R.; Gravina, C.F.; Pithon-Curi, T.C.; Vaisberg, M.; Maranhão, R.C. Exercise Training Improves Plasma Lipid and Inflammatory Profiles and Increases Cholesterol Transfer to High-Density Lipoprotein in Elderly Women. J. Am. Geriatr. Soc. 2015, 63, 1247–1249. [Google Scholar] [CrossRef]
- Santos, C.A.F.; Amirato, G.R.; Jacinto, A.F.; Pedrosa, A.V.; Caldo-Silva, A.; Sampaio, A.R.; Pimenta, N.; Santos, J.M.B.; Pochini, A.; Bachi, A.L.L. Vertical Jump Tests: A Safe Instrument to Improve the Accuracy of the Functional Capacity Assessment in Robust Older Women. Healthcare 2022, 10, 323. [Google Scholar] [CrossRef]
- Ramos, L.R. Determinant factors for healthy aging among senior citizens in a large city: The Epidoso Project in São Paulo. Cad Saude Publ. 2003, 19, 793–798. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.; Kunugi, H. Screening for Sarcopenia (Physical Frailty) in the COVID-19 Era. Int. J. Endocrinol. 2021, 2021, 5563960. [Google Scholar] [CrossRef] [PubMed]
- Niculescu, M.-S. Optical method for improving the accuracy of biochemical assays. In Proceedings of the E-Health and Bioengineering Conference (EHB), Sinaia, Romania, 22–24 June 2017; pp. 381–385. [Google Scholar] [CrossRef]
- McCullough, P.A. Effect of Lipid Modification on Progression of Coronary Calcification. J. Am. Soc. Nephrol. 2005, 16 (Suppl. 2), S115–S119. [Google Scholar] [CrossRef] [PubMed]
- Doewes, R.I.; Gharibian, G.; Zadeh, F.A.; Zaman, B.A.; Vahdat, S.; Akhavan-Sigari, R. An updated systematic review on the effects of aerobic exercise on human blood lipid profile. In Current Problems in Cardiology; Elsevier: Amsterdam, The Netherlands, 2022; p. 101108. [Google Scholar] [CrossRef]
- Zha, Y.; Qian, Q. Protein Nutrition and Malnutrition in CKD and ESRD. Nutrients 2017, 9, 208. [Google Scholar] [CrossRef]
- Hosten, A.O. BUN and Creatinine. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. [Google Scholar]
- Lustgarten, M.S.; Fielding, R.A. Metabolites related to renal function, immune activation, and carbamylation are associated with muscle composition in older adults. Exp. Gerontol. 2017, 100, 1–10. [Google Scholar] [CrossRef]
- Silveira-Rodrigues, J.G.; Pires, W.; Gomes, P.F.; Ogando, P.H.M.; Melo, B.P.; Aleixo, I.M.S.; Soares, D.D. Combined exercise training improves specific domains of cognitive functions and metabolic markers in middle-aged and older adults with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2021, 173, 108700. [Google Scholar] [CrossRef]
- Rothenbacher, D.; Dallmeier, D.; Christow, H.; Koenig, W.; Denkinger, M.; Klenk, J. Association of growth differentiation factor 15 with other key biomarkers, functional parameters and mortality in community-dwelling older adults. Age Ageing 2019, 48, 541–546. [Google Scholar] [CrossRef]
- Levin, A.T.; Hanage, W.P.; Owusu-Boaitey, N.; Cochran, K.B.; Walsh, S.P.; Meyerowitz-Katz, G. Assessing the age specificity of infection fatality rates for COVID-19: Systematic review, meta-analysis, and public policy implications. Eur. J. Epidemiol. 2020, 35, 1123–1138. [Google Scholar] [CrossRef]
- Goveas, J.S.; Shear, M.K. Grief and the COVID-19 Pandemic in Older Adults. Am. J. Geriatr. Psychiatry 2020, 28, 1119–1125. [Google Scholar] [CrossRef]
- Kotwal, A.A.; Cenzer, I.S.; Waite, L.J.; Covinsky, K.E.; Perissinotto, C.M.; Boscardin, W.J.; Hawkley, L.C.; Dale, W.; Smith, A.K.; Kotwal, M.A.A.; et al. The epidemiology of social isolation and loneliness among older adults during the last years of life. J. Am. Geriatr. Soc. 2021, 69, 3081–3091. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of social isolation due to COVID-19 on health in older people: Mental and physical effects and recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Bachi, A.L.; Suguri, V.M.; Ramos, L.R.; Mariano, M.; Vaisberg, M.; Lopes, J.D.; Bachi, A.L.; Suguri, V.M.; Ramos, L.R.; Mariano, M.; et al. Increased production of autoantibodies and specific antibodies in response to influenza virus vaccination in physically active older individuals. Results Immunol. 2013, 3, 10–16. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association With Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Alley, D.E.; Shardell, M.D.; Peters, K.W.; McLean, R.R.; Dam, T.-T.L.; Kenny, A.M.; Fragala, M.S.; Harris, T.B.; Kiel, D.; Guralnik, J.M.; et al. Grip Strength Cutpoints for the Identification of Clinically Relevant Weakness. J. Gerontol. Biol. Sci. Med. Sci. 2014, 69, 559–566. [Google Scholar] [CrossRef]
- Hicks, G.E.; Shardell, M.; Alley, D.E.; Miller, R.R.; Bandinelli, S.; Guralnik, J.M.; Lauretani, F.; Simonsick, E.M.; Ferrucci, L. Absolute Strength and Loss of Strength as Predictors of Mobility Decline in Older Adults: The InCHIANTI Study. J. Gerontol. Biol. Sci. Med. Sci. 2011, 67, 66–73. [Google Scholar] [CrossRef]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef]
- Raman, M.; Middleton, R.J.; Kalra, P.A.; Green, D. Estimating renal function in old people: An in-depth review. Int. Urol. Nephrol. 2017, 49, 1979–1988. [Google Scholar] [CrossRef]
- Sokoll, L.J.; Russell, R.M.; A Sadowski, J.; Morrow, F.D. Establishment of creatinine clearance reference values for older women. Clin. Chem. 1994, 40, 2276–2281. [Google Scholar] [CrossRef] [PubMed]
- Malavasi, V.L.; Valenti, A.C.; Ruggerini, S.; Manicardi, M.; Orlandi, C.; Sgreccia, D.; Vitolo, M.; Proietti, M.; Lip, G.Y.H.; Boriani, G. Kidney Function According to Different Equations in Patients Admitted to a Cardiology Unit and Impact on Outcome. J. Clin. Med. 2022, 11, 891. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Hong, X.; Gao, W.; Luo, S.; Cai, J.; Liu, G.; Huang, Y. Causal relationship between physical activity, leisure sedentary behaviors and COVID-19 risk: A Mendelian randomization study. J. Transl. Med. 2022, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Leiva, A.M.; Martínez, M.A.; Cristi-Montero, C.; Salas, C.; Ramírez-Campillo, R.; Martínez, X.D.; Aguilar-Farías, N.; Celis-Morales, C. Sedentary lifestyle is associated with metabolic and cardiovascular risk factors independent of physical activity. Rev. Med. Chil. 2017, 145, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Boardley, D.; Fahlman, M.; Topp, R.; Morgan, A.L.; McNevin, N. The impact of exercise training on blood lipids in older adults. Am. J. Geriatr. Cardiol. 2007, 16, 30–35. [Google Scholar] [CrossRef]
- Sher, N.M.; Nazli, R.; Zafar, H.; Fatima, S. Effects of lipid based Multiple Micronutrients Supplement on the birth outcome of underweight pre-eclamptic women: A randomized clinical trial. Pak. J. Med Sci. 2022, 38, 219–226. [Google Scholar] [CrossRef]
- Liu, H.; Liu, J.; Liu, J.; Xin, S.; Lyu, Z.; Fu, X. Triglyceride to High-Density Lipoprotein Cholesterol (TG/HDL-C) Ratio, a Simple but Effective Indicator in Predicting Type 2 Diabetes Mellitus in Older Adults. Front. Endocrinol. 2022, 13, 828581. [Google Scholar] [CrossRef]
- Young, K.A.; Maturu, A.; Lorenzo, C.; Langefeld, C.D.; Wagenknecht, L.E.; Chen, Y.-D.I.; Taylor, K.D.; Rotter, J.I.; Norris, J.M.; Rasouli, N. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance, β-cell function, and diabetes in Hispanics and African Americans. J. Diabetes Its Complicat. 2019, 33, 118–122. [Google Scholar] [CrossRef]
- Wu, L.; Parhofer, K.G. Diabetic dyslipidemia. Metabolism 2014, 63, 1469–1479. [Google Scholar] [CrossRef]
- De Lima, M.P.; Conopca, S.J.; Miyabara, R.; Romeiro, G.; Campos, L.A.; Baltatu, O.C. Cardiovascular and Quality of Life Outcomes of a 3-Month Physical Exercise Program in Two Brazilian Communities. Front. Med. 2020, 7, 568796. [Google Scholar] [CrossRef]
- Bagheri, B.; Radmard, N.; Faghani-Makrani, A.; Rasouli, M. Serum Creatinine and Occurrence and Severity of Coronary Artery Disease. Med. Arch. 2019, 73, 154–156. [Google Scholar] [CrossRef] [PubMed]
- Onat, A.; Yüksel, H.; Can, G.; Koroglu, B.; Kaya, A.; Altay, S. Serum creatinine is associated with coronary disease risk even in the absence of metabolic disorders. Scand. J. Clin. Lab. Investig. 2013, 73, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Farasat, T.; Sharif, S.; Naz, S.; Fazal, S. Significant association of serum creatinine with HbA1C in impaired glucose tolerant Pakistani subjects. Pak. J. Med Sci. 1969, 31, 991–994. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, B.; Zargari, M.; MeShKInI, F.; DInarvanD, K.; Mokhberi, V.; Azizi, S.; Rasouli, M. Uric Acid and Coronary Artery Disease, Two Sides of a Single Coin: A Determinant of Antioxidant System or a Factor in Metabolic Syndrome. J. Clin. Diagn. Res. 2016, 10, OC27–OC31. [Google Scholar] [CrossRef]
- Lee, B.J. Association of depressive disorder with biochemical and anthropometric indices in adult men and women. Sci. Rep. 2021, 11, 13596. [Google Scholar] [CrossRef]
- Kriaucioniene, V.; Bagdonaviciene, L.; Rodríguez-Pérez, C.; Petkeviciene, J. Associations between Changes in Health Behaviours and Body Weight during the COVID-19 Quarantine in Lithuania: The Lithuanian COVIDiet Study. Nutrients 2020, 12, 3119. [Google Scholar] [CrossRef]
- Sacks, D.; Baxter, B.; Campbell, B.C.V.; Carpenter, J.S.; Cognard, C.; Dippel, D.; Eesa, M.; Fischer, U.; Hausegger, K.; Hirsch, J.A.; et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar] [CrossRef]
- Guglielmi, V.; Colangeli, L.; Scipione, V.; Ballacci, S.; Di Stefano, M.; Hauser, L.; Bisogno, M.C.; D’Adamo, M.; Medda, E.; Sbraccia, P. Inflammation, underweight, malignancy and a marked catabolic state as predictors for worse outcomes in COVID-19 patients with moderate-to-severe disease admitted to Internal Medicine Unit. PLoS ONE 2022, 17, e0268432. [Google Scholar] [CrossRef]
- Brenner, B.M.; Rector, O.F. The Kidney; WB Saunders Co.: Philadelphia, PA, USA, 1976. [Google Scholar]
- Cabrerizo, S.; Cuadras, D.; Gomez-Busto, F.; Artaza-Artabe, I.; Marín-Ciancas, F.; Malafarina, V. Serum albumin and health in older people: Review and meta analysis. Maturitas 2015, 81, 17–27. [Google Scholar] [CrossRef]
- Silva-Fhon, J.R.; Rojas-Huayta, V.M.; Aparco-Balboa, J.P.; Céspedes-Panduro, B.; Partezani-Rodrigues, R.A. Sarcopenia and blood albumin: A systematic review with meta-analysis. Biomedica 2021, 41, 590–603. [Google Scholar] [CrossRef]
- Picca, A.; Coelho-Junior, H.J.; Calvani, R.; Marzetti, E.; Vetrano, D.L. Biomarkers shared by frailty and sarcopenia in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 73, 101530. [Google Scholar] [CrossRef] [PubMed]
- Stam, S.P.; Eisenga, M.F.; Gomes-Neto, A.W.; van Londen, M.; de Meijer, V.E.; van Beek, A.P.; Gansevoort, R.T.; Bakker, S.J. Muscle mass determined from urinary creatinine excretion rate, and muscle performance in renal transplant recipients. J. Cachex Sarcopenia Muscle 2019, 10, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Dowling, T.C.; Wang, E.-S.; Ferrucci, L.; Sorkin, J.D. Glomerular Filtration Rate Equations Overestimate Creatinine Clearance in Older Individuals Enrolled in the Baltimore Longitudinal Study on Aging: Impact on Renal Drug Dosing. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2013, 33, 912–921. [Google Scholar] [CrossRef] [PubMed]
- Flamant, M.; Haymann, J.-P.; Vidal-Petiot, E.; Letavernier, E.; Clerici, C.; Boffa, J.-J.; Vrtovsnik, F. GFR Estimation Using the Cockcroft-Gault, MDRD Study, and CKD-EPI Equations in the Elderly. Am. J. Kidney Dis. 2012, 60, 847–849. [Google Scholar] [CrossRef] [PubMed]
- Manini, T.M.; Clark, B.C. Dynapenia and Aging: An Update. J. Gerontol. Biol. Sci. Med. Sci. 2011, 67, 28–40. [Google Scholar] [CrossRef]
- Swedko, P.J.; Clark, H.D.; Paramsothy, K.; Akbari, A. Serum Creatinine Is an Inadequate Screening Test for Renal Failure in Elderly Patients. Arch. Intern. Med. 2003, 163, 356–360. [Google Scholar] [CrossRef]
- Moore, B.; Bemben, D.A.; Lein, D.H.; Bemben, M.G.; Singh, H. Fat mass is negatively associated with muscle strength and jump test performance. J. Frailty Aging 2020, 9, 214–218. [Google Scholar] [CrossRef]
- Liu, X.; Hao, Q.; Yue, J.; Hou, L.; Xia, X.; Zhao, W.; Zhang, Y.; Ge, M.; Ge, N.; Dong, B. Sarcopenia, Obesity and Sarcopenia Obesity in Comparison: Prevalence, Metabolic Profile, and Key Differences: Results from WCHAT Study. J. Nutr. Health Aging 2020, 24, 429–437. [Google Scholar] [CrossRef]
- Máximo, R.D.O.; de Oliveira, D.C.; Ramirez, P.C.; Luiz, M.M.; de Souza, A.F.; Delinocente, M.L.B.; Steptoe, A.; de Oliveira, C.; Alexandre, T.D.S. Combination of dynapenia and abdominal obesity affects long-term physical performance trajectories in older adults: Sex differences. Am. J. Clin. Nutr. 2022, 115, 1290–1299. [Google Scholar] [CrossRef]
- Bevilacqua, G.; Jameson, K.A.; Zhang, J.; Bloom, I.; Ward, K.A.; Cooper, C.; Dennison, E.M. The association between social isolation and musculoskeletal health in older community-dwelling adults: Findings from the Hertfordshire Cohort Study. Qual. Life Res. 2021, 30, 1913–1924. [Google Scholar] [CrossRef]
- Merchant, R.A.; Liu, S.G.; Lim, J.Y.; Fu, X.; Chan, Y.H. Factors associated with social isolation in community-dwelling older adults: A cross-sectional study. Qual. Life Res. 2020, 29, 2375–2381. [Google Scholar] [CrossRef] [PubMed]
- Imamura, K.; Kamide, N.; Ando, M.; Sato, H.; Sakamoto, M.; Shiba, Y. Social isolation is associated with future decline of physical performance in community-dwelling older adults: A 1-year longitudinal study. Aging Clin. Exp. Res. 2022, 34, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Greco, G.I.; Noale, M.; Trevisan, C.; Zatti, G.; Pozza, M.D.; Lazzarin, M.; Haxhiaj, L.; Ramon, R.; Imoscopi, A.; Bellon, S.; et al. Increase in Frailty in Nursing Home Survivors of Coronavirus Disease 2019: Comparison With Noninfected Residents. J. Am. Med Dir. Assoc. 2021, 22, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Westerterp, K.R. Changes in physical activity over the lifespan: Impact on body composition and sarcopenic obesity. Obes. Rev. 2018, 19 (Suppl. 1), 8–13. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, K.E.; Guo, W.; Cairns, B.J.; Armstrong, M.E.; Key, T.J. Association between physical activity and body fat percentage, with adjustment for BMI: A large cross-sectional analysis of UK Biobank. BMJ Open 2017, 7, e011843. [Google Scholar] [CrossRef] [Green Version]
| Variable | Older Women (n = 30) | ||
|---|---|---|---|
| Before (Pre) | After (Post) | p-Value | |
| Age (year) | 73.7 ± 6.2 | 74.7 ± 6.2 | ns |
| Weight (kg) | 60.9 ± 12.9 | 61.1 ± 13.1 | ns |
| Height (m) | 1.53 ± 0.07 | 1.53 ± 0.07 | ns |
| BMI (kg/m2) | 25.8 ± 4.4 | 25.9 ± 4.6 | ns |
| Variable | Older Women (n = 30) | ||
|---|---|---|---|
| Before (Pre) | After (Post) | p-Value | |
| GS, m/s | 3.2 ± 0.5 | 4.2 ± 1.2 | 0.0129 |
| TUGT, s | 6.8 ± 0.8 | 7.6 ± 1.1 | 0.0012 |
| HG, in kgf | 23.5 ± 3.7 | 21.9 ± 3.9 | 0.0151 |
| Parameters | Pre | Parameters | Post | ||
|---|---|---|---|---|---|
| Anthropometric X Metabolic | rho-value | p-value | Anthropometric X Metabolic | rho-value | p-value |
| Body weight X BMI | 0.909 | <0.0001 | Body weight X BMI | 0.917 | <0.0001 |
| Body weight X ECC | 0.595 | 0.0007 | Body weight X ECC | 0.614 | 0.0003 |
| BMI X ECC | 0.467 | 0.0106 | BMI X ECC | 0.540 | 0,0021 |
| Total cholesterol X LDL | 0.988 | <0.0001 | Total cholesterol X LDL | 0.991 | <0.0001 |
| Creatinine X ECC | −0.594 | 0.0005 | Creatinine X ECC | −0.479 | 0.0073 |
| Creatinine X Urea | 0.692 | <0.0001 | Body weight X Urea | 0.360 | 0.0491 |
| Creatinine X HDL | −0.362 | 0.0489 | HDL X Triglycerides | −0.551 | 0.0016 |
| Creatinine X Albumin | −0.371 | 0.0432 | Urea X Triglycerides | −0.430 | 0.0175 |
| Albumin X Total protein | 0.376 | 0.0401 | Urea X TG/HDL ratio | −0.413 | 0.0220 |
| Albumin X ECC | 0.397 | 0.0295 | |||
| HDL X Urea | −0.430 | 0.0175 | |||
| Anthropometric X Metabolic X Physical test | rho-value | p-value | Anthropometric X Metabolic X Physical test | rho-value | p-value |
| Body weight X TUGT | 0.581 | 0.0009 | Body weight X TUGT | 0.469 | 0.0136 |
| BMI X TUGT | 0.536 | 0.0027 | BMI X TUGT | 0.566 | 0.0020 |
| Albumin X GS | −0.411 | 0.0237 | Body weight X HG | 0.390 | 0.0328 |
| Albumin X TUGT | −0.397 | 0.0298 | BMI X HG | 0.433 | 0.0167 |
| Creatinine X GS | 0,.13 | 0.0231 | ECC X TUGT | 0.433 | 0.0239 |
| Urea X HG | −0.406 | 0.0286 | |||
| Physical tests | rho-value | p-value | Physical tests | rho-value | p-value |
| GS X TUGT | 0.386 | 0.0346 | GS X TUGT | 0.451 | 0.0180 |
| Variables | Age-Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| Older Women (n = 30) | ||||||||
| Pre-COVID-19 Pandemic | Post-COVID-19 Pandemic | |||||||
| β−Value | 95% CI | p-Value | R2 | β−Value | 95% CI | p-Value | R2 | |
| TG/HDL ratio | 0.009 | 0.002 to 0.017 | 0.0163 | 0.834 | 0.014 | 0.0014 to 0.026 | 0.032 | 0.906 |
| Creatinine (mg/dL) | −0.011 | −0.017 to −0.0045 | 0.003 | 0.785 | −0.0128 | −0.019 to −0.007 | 0.0006 | 0.815 |
| ECC (mL/min) | −1.139 | −1.499 to −0.780 | <0.0001 | 0.517 | −0.9887 | −1.310 to −0.667 | <0.0001 | 0.686 |
| TUGT (s) | ns | ns | ns | Ns | 0.2432 | 0.104 to 0.383 | 0.003 | 0.858 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cezário, K.; Santos, C.A.F.d.; Filho, C.d.M.A.; Amirato, G.R.; Paixão, V.d.; Almeida, E.B.; Amaral, J.B.d.; Caldo-Silva, A.; Pimenta, N.; Sampaio, A.R.; et al. Older Women Who Practiced Physical Exercises before the COVID-19 Pandemic Present Metabolic Alterations and Worsened Functional Physical Capacity after One Year of Social Isolation. Healthcare 2022, 10, 1736. https://doi.org/10.3390/healthcare10091736
Cezário K, Santos CAFd, Filho CdMA, Amirato GR, Paixão Vd, Almeida EB, Amaral JBd, Caldo-Silva A, Pimenta N, Sampaio AR, et al. Older Women Who Practiced Physical Exercises before the COVID-19 Pandemic Present Metabolic Alterations and Worsened Functional Physical Capacity after One Year of Social Isolation. Healthcare. 2022; 10(9):1736. https://doi.org/10.3390/healthcare10091736
Chicago/Turabian StyleCezário, Kizzy, Carlos André Freitas dos Santos, Clineu de Mello Almada Filho, Gislene Rocha Amirato, Vitória da Paixão, Ewin Barbosa Almeida, Jônatas Bussador do Amaral, Adriana Caldo-Silva, Nuno Pimenta, António Rodrigues Sampaio, and et al. 2022. "Older Women Who Practiced Physical Exercises before the COVID-19 Pandemic Present Metabolic Alterations and Worsened Functional Physical Capacity after One Year of Social Isolation" Healthcare 10, no. 9: 1736. https://doi.org/10.3390/healthcare10091736
APA StyleCezário, K., Santos, C. A. F. d., Filho, C. d. M. A., Amirato, G. R., Paixão, V. d., Almeida, E. B., Amaral, J. B. d., Caldo-Silva, A., Pimenta, N., Sampaio, A. R., Teques, P., Rodrigues, F. M., França, C. N., & Bachi, A. L. L. (2022). Older Women Who Practiced Physical Exercises before the COVID-19 Pandemic Present Metabolic Alterations and Worsened Functional Physical Capacity after One Year of Social Isolation. Healthcare, 10(9), 1736. https://doi.org/10.3390/healthcare10091736









