Medicinal Treatment of Elderly Psoriasis Patients before and after Entering a Nursing Home
Abstract
:1. Introduction
2. Material and Methods
2.1. Database and Study Cohort
2.2. Psoriasis
2.3. Severe Psoriasis
2.4. Prescription Prevalence
2.5. Statistical Analyses
3. Results
3.1. Baseline
3.2. Prescription Prevalence
3.3. Psoriasis Relevant Therapy
3.4. Systemic Therapies in Psoriasis
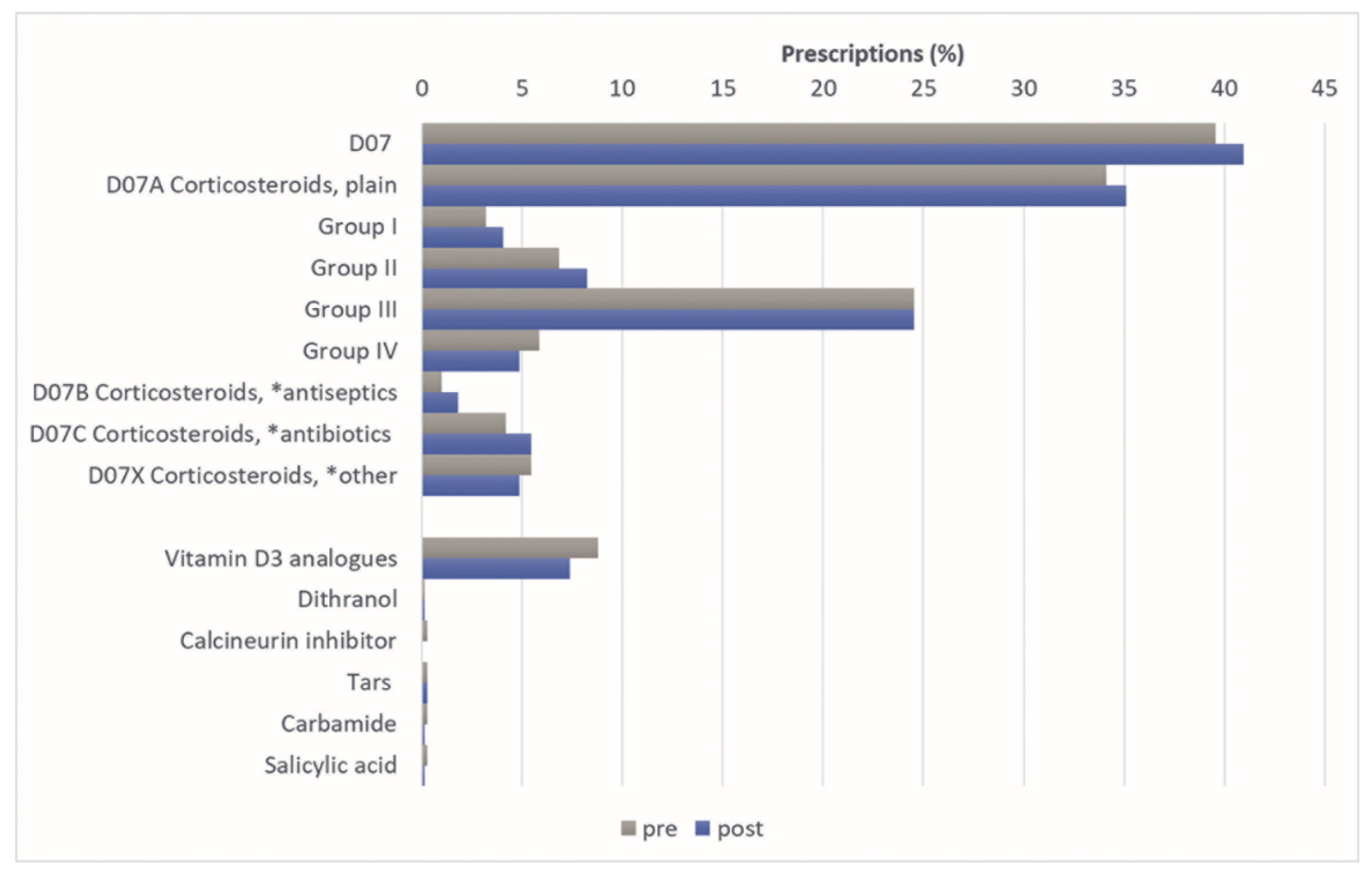
3.5. Topical Therapy
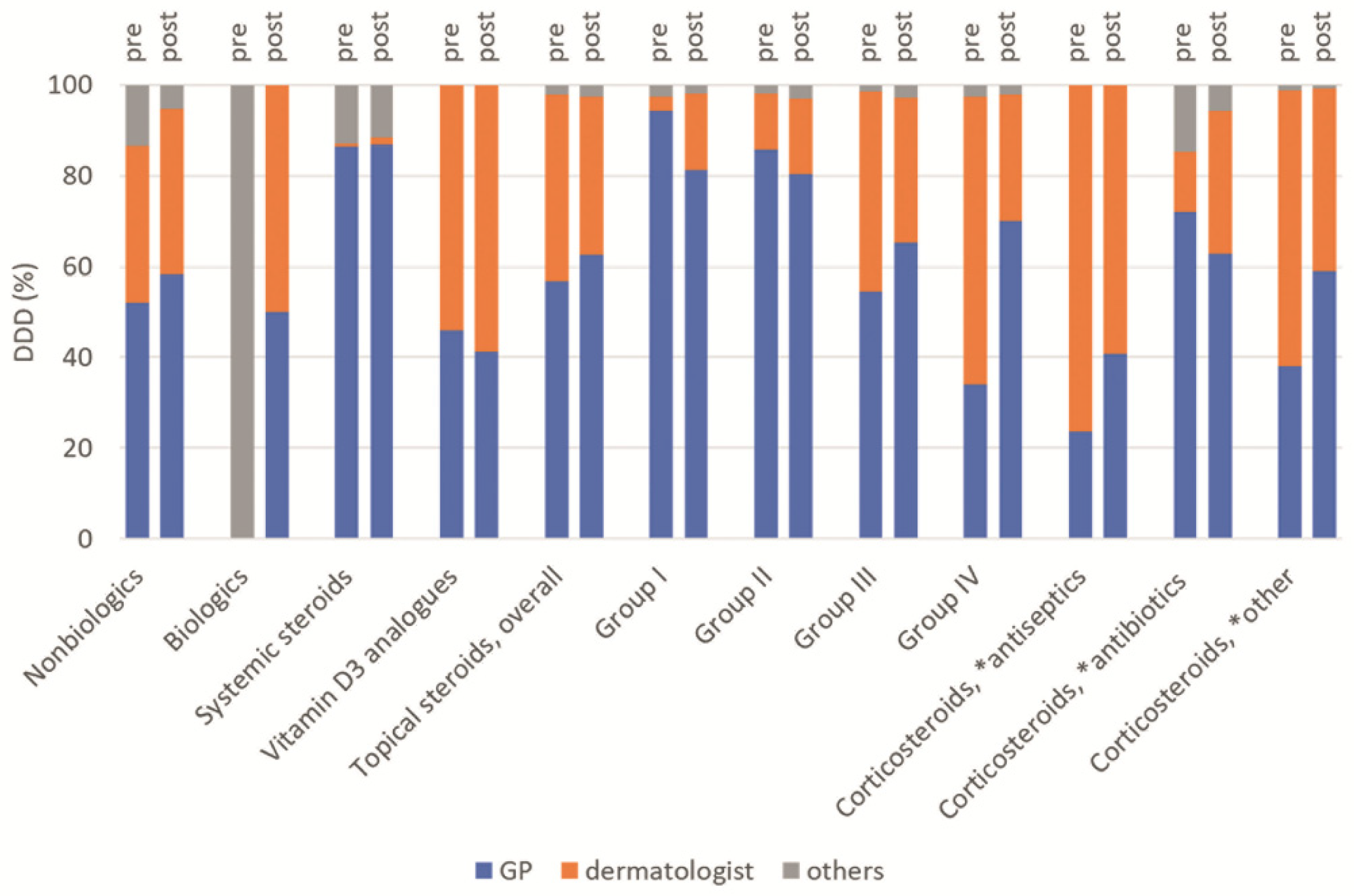
3.6. Prescribing Specialist Group
4. Discussion
4.1. Drug Supply of Patients with Psoriasis
4.2. Treatment of Psoriasis
4.3. Systemic Therapies
4.4. Topical Therapies
4.5. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Augustin, M.; Krüger, K.; Radtke, M.A.; Schwippl, I.; Reich, K. Disease severity, quality of life and health care in plaque-type psoriasis: A multicenter cross-sectional study in Germany. Dermatology 2008, 216, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Dalgard, F.J.; Gieler, U.; Tomas-Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.E.; Misery, L.; Szabo, C.; Linder, D.; Sampogna, F.; et al. The psychological burden of skin diseases: A cross-sectional multicenter study among dermatological out-patients in 13 European countries. J. Investig. Dermatol. 2015, 135, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Enamandram, M.; Kimball, A.B. Psoriasis epidemiology: The interplay of genes and the environment. J. Investig. Dermatol. 2013, 133, 287–289. [Google Scholar] [CrossRef]
- Sampogna, F.; Tabolli, S.; Mastroeni, S.; Di Pietro, C.; Fortes, C.; Abeni, D. Quality of life impairment and psychological distress in elderly patients with psoriasis. Dermatology 2007, 215, 341–347. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Report on Psoriasis. Available online: https://apps.who.int/iris/handle/10665/204417 (accessed on 2 September 2022).
- Reich, K. The concept of psoriasis as a systemic inflammation: Implications for disease management. J. Eur. Acad. Dermatol. Venereol. 2012, 26 (Suppl. 2), 3–11. [Google Scholar] [CrossRef] [PubMed]
- Philipp, S.; Simon, M. Ätiologie und Oathogenese—Die Psoriasis hat viele Gesichter. Ges. Komment. 2014, 55, 4–8. [Google Scholar]
- AWMF—Abeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften. S3—Leitlinie zur Therapie der Psoriasis Vulgaris. Available online: https://www.awmf.org/uploads/tx_szleitlinien/013-001l_S3_Therapie_Psoriasis-vulgaris_2017-12.pdf (accessed on 17 September 2020).
- Augustin, M.; Mrowietz, U.; Luck-Sikorski, C.; von Kiedrowski, R.; Schlette, S.; Radtke, M.A.; John, S.M.; Zink, A.; Suthakharan, N.; Sommer, R. Translating the WHA resolution in a member state: Towards a German programme on ‘Destigmatization’ for individuals with visible chronic skin diseases. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 2202–2208. [Google Scholar] [CrossRef]
- Augustin, M.; Spehr, C.; Radtke, M.A.; Boehncke, W.-H.; Luger, T.; Mrowietz, U.; Reusch, M.; Strömer, K.; Wozel, G.; von Kiedrowski, R.; et al. German psoriasis registry PsoBest: Objectives, methodology and baseline data. J. Dtsch. Dermatol. Ges. 2014, 12, 48–57. [Google Scholar] [CrossRef]
- Grozdev, I.S.; van Voorhees, A.S.; Gottlieb, A.B.; Hsu, S.; Lebwohl, M.G.; Bebo, B.F.; Korman, N.J. Psoriasis in the elderly: From the Medical Board of the National Psoriasis Foundation. J. Am. Acad. Dermatol. 2011, 65, 537–545. [Google Scholar] [CrossRef]
- Smith, E.S.; Fleischer, A.B.; Feldman, S.R. Demographics of aging and skin disease. Clin. Geriatr. Med. 2001, 17, 631–641. [Google Scholar] [CrossRef]
- Phan, C.; Sigal, M.-L.; Estève, E.; Reguiai, Z.; Barthélémy, H.; Beneton, N.; Maccari, F.; Lahfa, M.; Thomas-Beaulieu, D.; Le Guyadec, T.; et al. Psoriasis in the elderly: Epidemiological and clinical aspects, and evaluation of patients with very late onset psoriasis. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Kratzsch, D.; Treudler, R. Dermatologic therapy in geriatric patients. J. Dtsch. Dermatol. Ges. 2014, 12, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Makrantonaki, E.; Liakou, A.I.; Eckardt, R.; Zens, M.; Steinhagen-Thiessen, E.; Zouboulis, C.C. Hauterkrankungen beim geriatrischen Patienten. Epidemiologische Daten. Hautarzt 2012, 63, 938–946. [Google Scholar] [CrossRef]
- Di Lernia, V.; Goldust, M. An overview of the efficacy and safety of systemic treatments for psoriasis in the elderly. Expert Opin. Biol. Ther. 2018, 18, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Lé, A.M.; Torres, T. New Topical Therapies for Psoriasis. Am. J. Clin. Dermatol. 2022, 23, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Busse, R.; Blümel, M.; World Health Organization. Germany: Health System Review; World Health Organization: Geneva, Switzerland, 2014; Volume 16, 296p. [Google Scholar]
- Boehncke, W.-H. Systemic Inflammation and Cardiovascular Comorbidity in Psoriasis Patients: Causes and Consequences. Front. Immunol. 2018, 9, 579. [Google Scholar] [CrossRef] [PubMed]
- Saß, A.-C.; Wurm, S.; Ziese, T. 2 Alter = Krankheit? Gesundheitszustand und Gesundheitsentwicklung. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Gesundheitszustand-Relevantes-Verhalten/Publikationen/Downloads-Gesundheitszustand/gesundheit-krankheit-im-alter-5230003099004.pdf?__blob=publicationFile (accessed on 24 March 2022).
- WHO Collaborating Centre for Drug Statistics Methodology. Dermatologicals. Available online: https://www.whocc.no/atc_ddd_index/?code=D&showdescription=no (accessed on 17 August 2022).
- Swart, E.; Gothe, H.; Geyer, S.; Jaunzeme, J.; Maier, B.; Grobe, T.G.; Ihle, P. Gute Praxis Sekundärdatenanalyse (GPS): Leitlinien und Empfehlungen. Gesundheitswesen 2015, 77, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Petersen, J.; Garbe, C.; Wolf, S.; Stephan, B.; Augustin, M.; Hagenström, K. Ärztliche Versorgung älterer Psoriasiserkrankter vor und nach Pflegeheimeintritt: Eine retrospektive Krankenkassendatenanalyse. Z. Gerontol. Geriatr. 2022. [Google Scholar] [CrossRef]
- Kühn, F. Die Demografische Entwicklung in Deutschland. Available online: https://www.bpb.de/ajax/183654?type=pdf (accessed on 28 February 2021).
- Robert Koch-Institut. Gesundheit in Deutschland: Welche Auswirkungen Hat der Demografische Wandel auf Gesundheit und Gesundheitsversorgung? Available online: https://www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsGiD/2015/09_gesundheit_in_deutschland.html (accessed on 24 March 2022).
- Kottner, J.; Rahn, Y.; Blume-Peytavi, U.; Lahmann, N. Skin care practice in German nursing homes: A German-wide cross-sectional study. J. Dtsch. Dermatol. Ges. 2013, 11, 329–336. [Google Scholar] [CrossRef]
- Kamel, J.G.; Yamauchi, P.S. Managing Mild-to-Moderate Psoriasis in Elderly Patients: Role of Topical Treatments. Drugs Aging 2017, 34, 583–588. [Google Scholar] [CrossRef]
- Takeshita, J.; Gelfand, J.M.; Li, P.; Pinto, L.; Yu, X.; Rao, P.; Viswanathan, H.N.; Doshi, J.A. Psoriasis in the US Medicare Population: Prevalence, Treatment, and Factors Associated with Biologic Use. J. Investig. Dermatol. 2015, 135, 2955–2963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, F.; Meinecke, P.; Freitag, M.H.; Glaeske, G.; Schulze, J.; Schmiemann, G. Who gets dipyrone (metamizole) in Germany? Prescribing by age, sex and region. J. Clin. Pharm. Ther. 2015, 40, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Schulze, J.; Freitag, M.H.; Glaeske, G.; Schmiemann, G.; Hoffmann, F. Schmerzmittelversorgung von Pflegeheimbewohnern mit und ohne Krebserkrankung. Am häufigsten mit Metamizol. Schmerz 2015, 29, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Balato, N.; Patruno, C.; Napolitano, M.; Patrì, A.; Ayala, F.; Scarpa, R. Managing moderate-to-severe psoriasis in the elderly. Drugs Aging 2014, 31, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Kostović, K.; Žužul, K.; Čeović, R.; Bukvić Mokos, Z. Psoriasis in the mature patient: Therapeutic approach in the era of biologics. Clin. Dermatol. 2018, 36, 222–230. [Google Scholar] [CrossRef]
- Di Caprio, R.; Caiazzo, G.; Cacciapuoti, S.; Fabbrocini, G.; Scala, E.; Balato, A. Safety concerns with current treatments for psoriasis in the elderly. Expert Opin. Drug Saf. 2020, 19, 523–531. [Google Scholar] [CrossRef]
- Tatu, A.L.; Elisei, A.M.; Chioncel, V.; Miulescu, M.; Nwabudike, L.C. Immunologic adverse reactions of β-blockers and the skin. Exp. Ther. Med. 2019, 18, 955–959. [Google Scholar] [CrossRef]
- Parslew, R.; Traulsen, J. Efficacy and local safety of a calcipotriol/ betamethasone dipropionate ointment in elderly patients with psoriasis vulgaris. Eur. J. Dermatol. 2005, 15, 37–39. [Google Scholar]
- Zhang, P.; Wu, M.X. A clinical review of phototherapy for psoriasis. Lasers Med. Sci. 2018, 33, 173–180. [Google Scholar] [CrossRef]
- Augustin, M.; Glaeske, G.; Schäfer, I.; Rustenbach, S.J.; Hoer, A.; Radtke, M.A. Processes of psoriasis health care in Germany--long-term analysis of data from the statutory health insurances. J. Dtsch. Dermatol. Ges. 2012, 10, 648–655. [Google Scholar] [CrossRef]
| ICD-10 Diagnosis | Term |
|---|---|
| L40 | Psoriasis |
| L40.0 | Psoriasis vulgaris |
| L40.1 | Generalized pustular psoriasis |
| L40.2 | Acrodermatitis continua |
| L40.3 | Pustulosis palmaris et plantaris |
| L40.4 | Guttate psoriasis |
| L40.5 | Psoriatic arthritis (PsA) |
| L40.8 | Psoriasis, unspecified |
| L40.9 | Other psoriasis |
| ATC Information | Active Ingredients |
|---|---|
| Biological systemic medication | |
| L04AB04 | Adalimumab |
| L04AB02 | Infliximab |
| L04AC05 | Ustekinumab |
| L04AC10 | Secukinumab |
| L04AB01 | Etanercept |
| Nonbiological systemic medication | |
| L04AA32 | Apremilast |
| L01BA01 | Methotrexate |
| M01CX01 | Methotrexate |
| L04AX03 | Methotrexate |
| L04AD01 | Ciclosporine |
| D05BB02 | Acitretin |
| D05BX20 | Alkyl esters of fumaric acid |
| D05BX01 | Fumaric acid |
| D05BX51 | Fumaric acid derivatives, combinations |
| ATC Information | Active Ingredient |
|---|---|
| Biological systemic drugs | |
| L04AB04 | Adalimumab |
| L04AB02 | Infliximab |
| L04AC05 | Ustekinumab |
| L04AC10 | Secukinumab |
| L04AB01 | Etanercept |
| Nonbiological systemic drugs | |
| L04AA32 | Apremilast |
| L01BA01 | Methotrexate |
| M01CX01 | Methotrexate |
| L04AX03 | Methotrexate |
| L04AD01 | Ciclosporine |
| D05BB02 | Acitretin |
| D05BX20 | Alkyl esters of fumaric acid |
| D05BX01 | Fumaric acid |
| D05BX51 | Fumaric acid derivatives, combinations |
| D05BA03 | Bergapten |
| D05BA02 | Methoxsalen |
| D05BA01 | Trioxysalen |
| Systemic steroids | |
| H02AB | Glucocorticoids |
| H02B | Corticosteroids for systemic use, combinations |
| ATC Information | Active Ingredient |
|---|---|
| Tars | |
| D05AA | Tars |
| Dithranol | |
| D05AC01 | Dithranol |
| D05AC51 | Dithranol, combinations |
| Psoralen | |
| D05AD01 | Trioxysalen |
| D05AD02 | Methoxsalen |
| Vitamin D3 analogues | |
| D05AX02 | Calcipotriol |
| D05AX03 | Calcitriol |
| D05AX04 | Tacalcitol |
| D05AX52, D05AX22 | Calcipotriol, combinations |
| Salicylic acid | |
| D05AX56 | Salicylic acid, combinations |
| D02AF | Salicylic acid preparations |
| Calcineurin inhibitors | |
| D11AH01 | Tacrolimus |
| D11AH02 | Pimecrolimus |
| D11AX14 (until 2010) | Tacrolimus |
| D11AX15 (until 2010) | Pimecrolimus |
| D07A—Corticosteroids, plain | |
| D07AA | Corticosteroids, weak (group I) |
| D07AB | Corticosteroids, moderately potent (group II) |
| D07AC | Corticosteroids, potent (group III) |
| D07AD | Corticosteroids, very potent (group IV) |
| D07B—Corticosteroids, combinations with antiseptics | |
| D07BA | Corticosteroids, weak, combinations with antiseptics |
| D07BB | Corticosteroids, moderately potent, combinations with antiseptics |
| D07BC | Corticosteroids, potent, combinations with antiseptics |
| D07BD | Corticosteroids, very potent, combinations with antiseptics |
| D07C—Corticosteroids, combinations with antibiotics | |
| D07CA | Corticosteroids, weak, combinations with antibiotics |
| D07CB | Corticosteroids, moderately potent, combinations with antibiotics |
| D07CC | Corticosteroids, potent, combinations with antibiotics |
| D07CD | Corticosteroids, very potent, combinations with antibiotics |
| D07X—Corticosteroids, other combinations | |
| D07XA | Corticosteroids, weak, other combinations |
| D07XB | Corticosteroids, moderately potent, other combinations |
| D07XC | Corticosteroids, potent, other combinations |
| D07XD | Corticosteroids, very potent, other combinations |
| 12 Months Pre NHA * | 12 Months Post NHA | |
|---|---|---|
| Mean age at NH entry, years (SD) | 83.3 (7.5) | 84.3 (7.5) |
| Age groups, in years, n (%) | ||
| 65–74 | 109 (15.2) | |
| 75–84 | 251 (35.0) | |
| 85+ | 358 (50.0) | |
| Sex, n (%) | ||
| Male | 171 (23.8) | |
| Female | 547 (76.2) | |
| Care level, n (%) | ||
| 0/1 | 456 (63.5) | |
| 2 | 231 (32.2) | |
| 3 | 31 (4.3) | |
| Severity of disease, n (%) | ||
| Mild | 694 (96.7) | 699 (97.4) |
| Moderate to severe | 24 (3.3) | 19 (2.6) |
| Prevalence of psoriasis-related comorbidities, n (%) | ||
| Diabetes mellitus | 277 (38.6) | 258 (35.9) |
| Obesity | 120 (16.7) | 82 (11.4) |
| Hypertension | 612 (85.2) | 571 (79.5) |
| Ischemic heart disease | 268 (37.3) | 226 (31.5) |
| Osteoporosis | 240 (33.4) | 213 (29.7) |
| Depression | 293 (40.8) | 248 (34.5) |
| Cataract | 214 (29.8) | 184 (25.6) |
| Pruritus | 51 (7.1) | 64 (8.9) |
| Dementia | 382 (53.2) | 441 (61.4) |
| 12 Months Pre NHA * | 12 Months Post NHA | |||||
|---|---|---|---|---|---|---|
| ATC Code | Agent | Frequency, n (%) | ATC Code | Agent | Frequency, n (%) | |
| 1 | N02BB02 | Metamizole natrium | 1601 (5.7) | N02BB02 | Metamizole natrium | 2688 (8.1) |
| 2 | C03CA04 | Torasemide | 962 (3.4) | A02BC02 | Pantoprazole | 1332 (4.0) |
| 3 | A02BC02 | Pantoprazole | 847 (3.0) | C03CA04 | Torasemide | 1277 (3.8) |
| 4 | C09AA05 | Ramipril | 724 (2.6) | C09AA05 | Ramipril | 834 (2.5) |
| 5 | C07AB02 | Metoprolol | 702 (2.5) | C07AB02 | Metoprolol | 713 (2.1) |
| 12 Months Pre NHA * | 12 Months Post NHA | p-Value | |
|---|---|---|---|
| People with psoriasis with at least one drug prescription, n (%) | 715 (99.6%) | 718 (100%) | 0.2482 |
| Number of drug prescriptions, n (mean; SD) | 27,936 (39.1; 0.9) | 33,301 (46.4; 22.8) | <0.0001 |
| Prescriptions for different agents, n (SD) | 14.3 (6.5) | 13.2 (5.6) | <0.0001 |
| People with psoriasis with at least one prescription for a psoriasis-related therapy, n (%) | 386 (53.8%) | 382 (53.2%) | 0.7995 |
| 12 Months Pre NHA * | 12 Months Post NHA | p-Value | |
|---|---|---|---|
| Systemic drugs (without steroids), people with psoriasis with at least one prescription, n (%) | 19 (2.6) | 15 (2.1) | 0.2482 |
| DDD, n (mean, SD) | 3003.1 (Ø 158.1; ±12.6) | 2992.4 (Ø 199.5; ±103.5) | 0.9874 |
| Biological drugs, n (%) | 2 (0.3) | 2 (0.3) | - |
| DDD (mean, SD) | 542.9 (Ø 271.4; ±101.0) | 685.7 (Ø 342.9; ±0.002) | 0.3282 |
| Nonbiological drugs, n (%) | 17 (2.4) | 13 (1.8) | 0.2482 |
| DDD (mean, SD) | 2460.3 (Ø 144.7; ±124.2) | 2306.7 (Ø 177.4; ±92.6) | 0.8230 |
| Systemic steroids, n (%) | 126 (17.5) | 102 (13.8) | 0.0097 |
| DDD (mean, SD) | 22,702.4 (Ø180.2; ±178.8) | 21,618.7 (Ø 212.0; ±219.1) | 0.6423 |
| Stratified analysis of systemic steroids | |||
| Age in years, n (%) | |||
| 65–74 | 18 (16.5) | 14 (12.8) | 0.2059 |
| 75–84 | 58 (23.1) | 42 (16.7) | 0.0077 |
| 85+ | 50 (14.0) | 46 (12.8) | 0.5271 |
| Sex, n (%) | |||
| Male | 22 (12.9) | 15 (8.8) | 0.0522 |
| Female | 104 (19.0) | 87 (15.9) | 0.0466 |
| Level of care, n (%) | |||
| 0/1 | 79 (17.3) | 66 (14.5) | 0.0687 |
| 2 | 42 (18.2) | 31 (13.4) | 0.0482 |
| 3 | 5 (16.1) | 5 (16.1) | 1.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petersen, J.; Garbe, C.; Wolf, S.; Stephan, B.; Augustin, M.; Hagenström, K. Medicinal Treatment of Elderly Psoriasis Patients before and after Entering a Nursing Home. Healthcare 2022, 10, 1730. https://doi.org/10.3390/healthcare10091730
Petersen J, Garbe C, Wolf S, Stephan B, Augustin M, Hagenström K. Medicinal Treatment of Elderly Psoriasis Patients before and after Entering a Nursing Home. Healthcare. 2022; 10(9):1730. https://doi.org/10.3390/healthcare10091730
Chicago/Turabian StylePetersen, Jana, Claudia Garbe, Sandra Wolf, Brigitte Stephan, Matthias Augustin, and Kristina Hagenström. 2022. "Medicinal Treatment of Elderly Psoriasis Patients before and after Entering a Nursing Home" Healthcare 10, no. 9: 1730. https://doi.org/10.3390/healthcare10091730
APA StylePetersen, J., Garbe, C., Wolf, S., Stephan, B., Augustin, M., & Hagenström, K. (2022). Medicinal Treatment of Elderly Psoriasis Patients before and after Entering a Nursing Home. Healthcare, 10(9), 1730. https://doi.org/10.3390/healthcare10091730






