Italian Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in an Undergraduate Healthcare Student Context
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Description of the Version of RIPLS Adopted in This Study
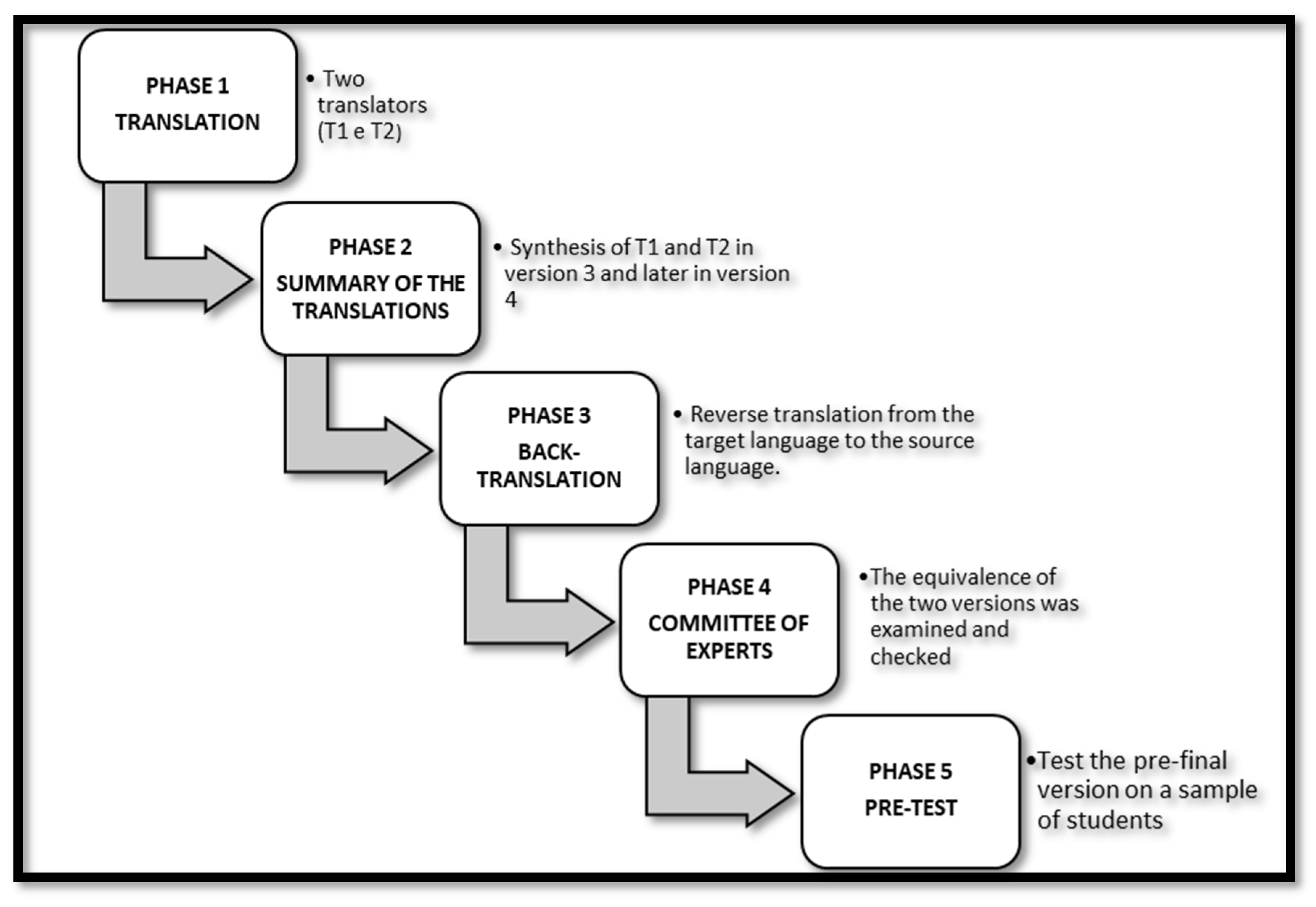
2.3. Phase One: Translation and Cross-Cultural Adaptation of the RIPLS
2.4. Phase Two: Data Collection Procedure
2.5. Data Analysis
2.6. Ethical Consideration
3. Results
3.1. Descriptive Characteristics of the Sample
3.2. Preliminary Item Analysis
3.3. Exploratory Factor Analysis
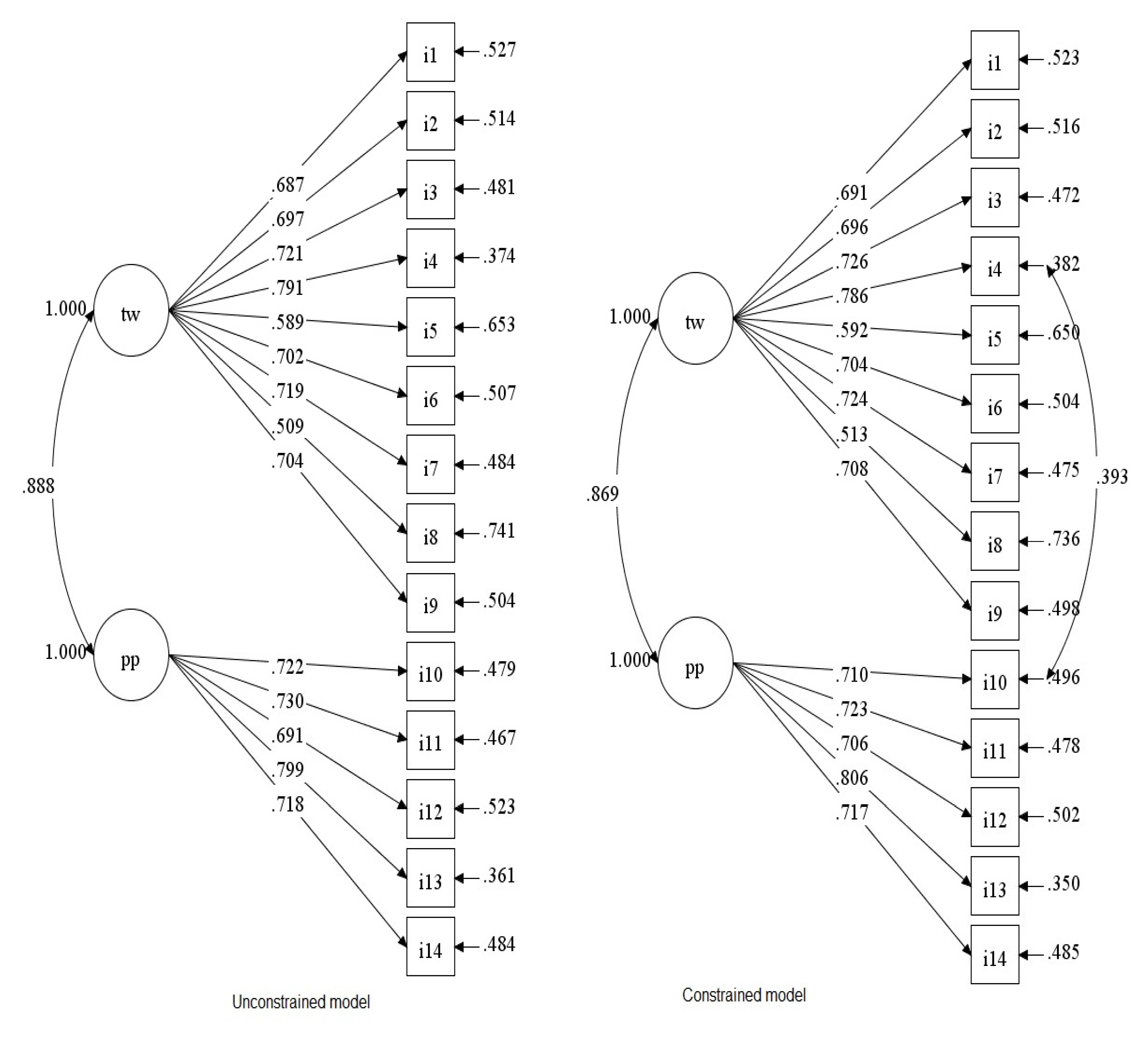
3.4. Confirmatory Factor Analysis
3.5. Reliability of the Italian RIPLS
4. Discussion
5. Conclusions and Future Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oishi, A.; Haruta, J.; Yoshimi, K.; Goto, M.; Yoshida, K.; Yoshimoto, H. Cross-Cultural Adaptation of the Professional Version of the Readiness for Interprofessional Learning Scale (RIPLS) in Japanese. J. Interprof. Care 2017, 31, 85–90. [Google Scholar] [CrossRef] [PubMed]
- WHO Framework for Action on Interprofessional Education & Collaborative Practice. Available online: https://www.who.int/publications-detail-redirect/framework-for-action-on-interprofessional-education-collaborative-practice (accessed on 24 August 2022).
- Dellafiore, F.; Caruso, R.; Conte, G.; Grugnetti, A.M.; Bellani, S.; Arrigoni, C. Individual-Level Determinants of Interprofessional Team Collaboration in Healthcare. J. Interprof. Care 2019, 33, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Bridges, D.R.; Davidson, R.A.; Odegard, P.S.; Maki, I.V.; Tomkowiak, J. Interprofessional Collaboration: Three Best Practice Models of Interprofessional Education. Med. Educ. Online 2011, 16, 6035. [Google Scholar] [CrossRef] [PubMed]
- Caruso, R.; Magon, A.; Dellafiore, F.; Griffini, S.; Milani, L.; Stievano, A.; Orchard, C.A. Italian Version of the Assessment of Interprofessional Team Collaboration Scale II (I-AITCS II): A Multiphase Study of Validity and Reliability amongst Healthcare Providers. Med. Lav. 2018, 109, 316–324. [Google Scholar] [CrossRef]
- Aston, S.J.; Rheault, W.; Arenson, C.; Tappert, S.K.; Stoecker, J.; Orzoff, J.; Galitski, H.; Mackintosh, S. Interprofessional Education: A Review and Analysis of Programs from Three Academic Health Centers. Acad. Med. 2012, 87, 949–955. [Google Scholar] [CrossRef]
- Carroll, J.S.; Edmondson, A.C. Leading Organisational Learning in Health Care. Qual. Saf. Health Care 2002, 11, 51–56. [Google Scholar] [CrossRef]
- Lie, D.A.; Forest, C.P.; Kysh, L.; Sinclair, L. Interprofessional Education and Practice Guide No. 5: Interprofessional Teaching for Prequalification Students in Clinical Settings. J. Interprof. Care 2016, 30, 324–330. [Google Scholar] [CrossRef]
- Cobianchi, L.; Dal Mas, F.; Massaro, M.; Fugazzola, P.; Coccolini, F.; Kluger, Y.; Leppäniemi, A.; Moore, E.E.; Sartelli, M.; Angelos, P.; et al. Team Dynamics in Emergency Surgery Teams: Results from a First International Survey. World J. Emerg. Surg. 2021, 16, 47. [Google Scholar] [CrossRef]
- Busari, J.; Moll, F.; Duits, A. Understanding the Impact of Interprofessional Collaboration on the Quality of Care: A Case Report from a Small-Scale Resource Limited Health Care Environment. JMDH 2017, 10, 227–234. [Google Scholar] [CrossRef]
- Li, Z.; Sun, Y.; Zhang, Y. Adaptation and Reliability of the Readiness for Inter-Professional Learning Scale (RIPLS) in the Chinese Health Care Students Setting. BMC Med. Educ. 2018, 18, 309. [Google Scholar] [CrossRef]
- Milutinović, D.; Lovrić, R.; Simin, D. Interprofessional Education and Collaborative Practice: Psychometric Analysis of the Readiness for Interprofessional Learning Scale in Undergraduate Serbian Healthcare Student Context. Nurse Educ. Today 2018, 65, 74–80. [Google Scholar] [CrossRef]
- Brock, D.; Abu-Rish, E.; Chiu, C.-R.; Hammer, D.; Wilson, S.; Vorvick, L.; Blondon, K.; Schaad, D.; Liner, D.; Zierler, B. Interprofessional Education in Team Communication: Working Together to Improve Patient Safety. BMJ Qual. Saf. 2013, 22, 414–423. [Google Scholar] [CrossRef]
- Eddy, K.; Jordan, Z.; Stephenson, M. Health Professionals’ Experience of Teamwork Education in Acute Hospital Settings: A Systematic Review of Qualitative Literature. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 96–137. [Google Scholar] [CrossRef]
- Parsell, G.; Bligh, J. The Development of a Questionnaire to Assess the Readiness of Health Care Students for Interprofessional Learning (RIPLS). Med. Educ. 1999, 33, 95–100. [Google Scholar] [CrossRef]
- Reid, R.; Bruce, D.; Allstaff, K.; McLernon, D. Validating the Readiness for Interprofessional Learning Scale (RIPLS) in the Postgraduate Context: Are Health Care Professionals Ready for IPL? Med. Educ. 2006, 40, 415–422. [Google Scholar] [CrossRef]
- Thannhauser, J.; Russell-Mayhew, S.; Scott, C. Measures of Interprofessional Education and Collaboration. J. Interprof. Care 2010, 24, 336–349. [Google Scholar] [CrossRef]
- Peduzzi, M.; Norman, I.; Coster, S.; Meireles, E. Cross-Cultural Adaptation of the Readiness for Interprofessional Learning Scale in Brazil. Rev. Esc. Enferm. USP 2015, 49, 7–15. [Google Scholar] [CrossRef]
- El-Zubeir, M.; Rizk, D.E.E.; Al-Khalil, R.K. Are Senior UAE Medical and Nursing Students Ready for Interprofessional Learning? Validating the RIPL Scale in a Middle Eastern Context. J. Interprof. Care 2006, 20, 619–632. [Google Scholar] [CrossRef]
- McFadyen, A.K.; Webster, V.; Strachan, K.; Figgins, E.; Brown, H.; McKechnie, J. The Readiness for Interprofessional Learning Scale: A Possible More Stable Sub-Scale Model for the Original Version of RIPLS. J. Interprof. Care 2005, 19, 595–603. [Google Scholar] [CrossRef]
- Cloutier, J.; Lafrance, J.; Michallet, B.; Marcoux, L.; Cloutier, F. French Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in a Canadian Undergraduate Healthcare Student Context. J. Interprof. Care 2015, 29, 150–155. [Google Scholar] [CrossRef]
- Mahler, C.; Giesler, M.; Stock, C.; Krisam, J.; Karstens, S.; Szecsenyi, J.; Krug, K. Confirmatory Factor Analysis of the German Readiness for Interprofessional Learning Scale (RIPLS-D). J. Interprof. Care 2016, 30, 381–384. [Google Scholar] [CrossRef]
- Lauffs, M.; Ponzer, S.; Saboonchi, F.; Lonka, K.; Hylin, U.; Mattiasson, A.C. Cross-Cultural Adaptation of the Swedish Version of Readiness for Interprofessional Learning Scale (RIPLS). Med. Educ. 2008, 42, 405–411. [Google Scholar] [CrossRef]
- Ergönül, E.; Başkurt, F.; Yilmaz, N.D.; Başkurt, Z.; Aşci, H.; Koç, Ş.; Temel, U.B. Reliability and Validity of the Readiness for Interprofessional Learning Scale (RIPLS) in Turkish Speaking Health Care Students. Acta Med. Mediterr. 2018, 34, 797–803. [Google Scholar] [CrossRef]
- Parsell, G.; Stewart, A.; Bligh, J. Testing the Validity of the Readiness for Interprofessional Learning Scale (RIPLS). In Proceedings of the 8th Ottawa International Conference, Ottawa, ON, Canada, 7–9 October 1998. [Google Scholar]
- Tamura, Y.; Seki, K.; Usami, M.; Taku, S.; Bontje, P.; Ando, H.; Taru, C.; Ishikawa, Y. Cultural Adaptation and Validating a Japanese Version of the Readiness for Interprofessional Learning Scale (RIPLS). J. Interprof. Care 2012, 26, 56–63. [Google Scholar] [CrossRef]
- Tyastuti, D.; Onishi, H.; Ekayanti, F.; Kitamura, K. Psychometric Item Analysis and Validation of the Indonesian Version of the Readiness for Interprofessional Learning Scale (RIPLS). J. Interprof. Care 2014, 28, 426–432. [Google Scholar] [CrossRef]
- Pype, P.; Deveugele, M. Dutch Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in a Primary Healthcare Context. Eur. J. Gen. Pract. 2016, 22, 225–231. [Google Scholar] [CrossRef]
- Nørgaard, B.; Draborg, E.; Sørensen, J. Adaptation and Reliability of the Readiness for Inter-Professional Learning Scale in a Danish Student and Health Professional Setting. BMC Med. Educ. 2016, 16, 60. [Google Scholar] [CrossRef] [PubMed]
- Ataollahi, M.; Amini, M.; Delavari, S.; Bazrafkan, L.; Jafari, P. Reliability and Validity of the Persian Version of Readiness for Inter-Professional Learning Scale. Int. J. Med. Educ. 2019, 10, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Torsvik, M.; Johnsen, H.C.; Lillebo, B.; Reinaas, L.O.; Vaag, J.R. Has “The Ceiling” Rendered the Readiness for Interprofessional Learning Scale (RIPLS) Outdated? J. Multidiscip. Healthc. 2021, 14, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Villagrán, I.; Jeldez, P.; Calvo, F.; Fuentes, J.; Moya, J.; Barañao, P.; Irarrázabal, L.; Rojas, N.; Soto, P.; Barja, S.; et al. Spanish Version of the Readiness for Interprofessional Learning Scale (RIPLS) in an Undergraduate Health Sciences Student Context. J. Interprof. Care 2022, 36, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Watkins, M.W. Exploratory Factor Analysis: A Guide to Best Practice. J. Black Psychol. 2018, 44, 219–246. [Google Scholar] [CrossRef]
- Rozental, A.; Kottorp, A.; Boettcher, J.; Andersson, G.; Carlbring, P. Negative Effects of Psychological Treatments: An Exploratory Factor Analysis of the Negative Effects Questionnaire for Monitoring and Reporting Adverse and Unwanted Events. PLoS ONE 2016, 11, e0157503. [Google Scholar] [CrossRef]
- Hinkin, T.R. A Review of Scale Development Practices in the Study of Organizations. J. Manag. 1995, 21, 967–988. [Google Scholar] [CrossRef]
- Cristobal, E.; Flavián, C.; Guinalíu, M. Perceived E-service Quality (PeSQ): Measurement Validation and Effects on Consumer Satisfaction and Web Site Loyalty. Manag. Serv. Qual. Int. J. 2007, 17, 317–340. [Google Scholar] [CrossRef]
- Sunderland, K.M.; Beaton, D.; Fraser, J.; Kwan, D.; McLaughlin, P.M.; Montero-Odasso, M.; Peltsch, A.J.; Pieruccini-Faria, F.; Sahlas, D.J.; Swartz, R.H.; et al. The Utility of Multivariate Outlier Detection Techniques for Data Quality Evaluation in Large Studies: An Application within the ONDRI Project. BMC Med. Res. Methodol. 2019, 19, 102. [Google Scholar] [CrossRef]
- Siegel, A.F. Practical Business Statistics, 6th ed.; Academic Press: Burlington, MA, USA, 2012; ISBN 978-0-12-385208-3. [Google Scholar]
- Arbuckle, J.L. IBM® SPSS® AmosTM 25 User’s Guide; SPSS Inc.: Chicago, IL, USA, 2019; p. 720. [Google Scholar]
- Basto, M.; Pereira, J.M. An SPSS R-Menu for Ordinal Factor Analysis. J. Stat. Softw. 2012, 46, 1–29. [Google Scholar] [CrossRef]
- Hair, J.F. (Ed.) Multivariate Data Analysis, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2010; ISBN 978-0-13-813263-7. [Google Scholar]
- Lim, S.; Jahng, S. Determining the Number of Factors Using Parallel Analysis and Its Recent Variants. Psychol. Methods 2019, 24, 452–467. [Google Scholar] [CrossRef]
- O’Connor, B.P. SPSS and SAS Programs for Addressing Interdependence and Basic Levels-of-Analysis Issues in Psychological Data. Behav. Res. Methods Instrum. Comput. 2004, 36, 17–28. [Google Scholar] [CrossRef]
- Auerswald, M.; Moshagen, M. How to Determine the Number of Factors to Retain in Exploratory Factor Analysis: A Comparison of Extraction Methods under Realistic Conditions. Psychol. Methods 2019, 24, 468–491. [Google Scholar] [CrossRef]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the Use of Exploratory Factor Analysis in Psychological Research. Psychol. Methods 1999, 4, 272–299. [Google Scholar] [CrossRef]
- Kim, H.; Ku, B.; Kim, J.Y.; Park, Y.-J.; Park, Y.-B. Confirmatory and Exploratory Factor Analysis for Validating the Phlegm Pattern Questionnaire for Healthy Subjects. Evid.-Based Complement. Altern. Med. 2016, 2016, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, T.A. Using the Modification Index and Standardized Expected Parameter Change for Model Modification. J. Exp. Educ. 2012, 80, 26–44. [Google Scholar] [CrossRef]
- Guillemin, F.; Bombardier, C.; Beaton, D. Cross-Cultural Adaptation of Health-Related Quality of Life Measures: Literature Review and Proposed Guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef]
- Parsell, G.; Spalding, R.; Bligh, J. Shared Goals, Shared Learning: Evaluation of a Multiprofessional Course for Undergraduate Students. Med. Educ. 1998, 32, 304–311. [Google Scholar] [CrossRef]
- Khalili, H. Online Interprofessional Education during and Post the COVID-19 Pandemic: A Commentary. J. Interprof. Care 2020, 34, 687–690. [Google Scholar] [CrossRef]
- Zijlmans, E.A.O.; Tijmstra, J.; van der Ark, L.A.; Sijtsma, K. Item-Score Reliability as a Selection Tool in Test Construction. Front. Psychol. 2018, 9, 2298. [Google Scholar] [CrossRef] [Green Version]
| Studies | Number of Final Subscales | Number of Participants | Number of Final Items | Cronbach’s Alpha for the Entire Scale | Language Availability |
|---|---|---|---|---|---|
| Parsell, Stewart, Bligh (1998) [25] | 2 | 914 | 19 | - | English |
| Parsell & Bligh (1999) [15] | 3 | 120 | 19 | 0.90 | English |
| McFadyen et al. (2005) ª [20] | 4 | 308 | 19 | 0.84 | English |
| Reid et al. (2006) ᵇ [16] | 3 | 66 | 23 | 0.76 | English |
| El-Zubeir et al. (2006) ᵇ [19] | 3 | 178 | 20 | 0.61 | Arabic |
| Lauffs et al. (2008) [23] | 3 | 214 | 19 | - | Swedish |
| Tamura et al. (2012) ᵇ [26] | 3 | 132 | 19 | 0.74 | Japanese |
| Tyastuti, D. et al. (2014) [27] | 3 | 378 | 16 | 0.87 | Indonesian |
| Peduzzi, M. et al. (2015) [18] | 3 | 327 | 27 | - | Portuguese/Brazil |
| Cloutier, J. et al. (2015) [21] | 3 | 141 | 16 | 0.90 | French |
| Mahler, C. et al. (2016) [22] | 3 | 531 | 19 | - | German |
| Pype, P. et al. (2016) [28] | 3 | 510 | 23 | 0.88 | Dutch |
| Nørgaard, B. et al. (2016) [29] | 4 | 570 | 29 | - | Danish |
| Oishi, A. et al. (2017) [1] | 4 | 368 | 23 | 0.7 | Japanese |
| Ergonul, E. et al. (2018) [24] | 3 | 213 | 19 | 0.85 | Turkish |
| Li, Z. et al. (2018) [11] | 4 | 282 | 19 | 0.70 | Chinese |
| Milutinović, D. et al. (2018) [12] | 2 | 257 | 19 | 0.90 | Serbian |
| Ataollahi, M. et al. (2019) [30] | 4 | 200 | 19 | 0.94 | Persian |
| Torsvik et al. (2021) [31] | 4 | 307 | 19 | 0.85 | Norwegian |
| Villagrán, I et al. (2022) [32] | 3 | 407 | 24 | 0.86 | Spanish |
| Original Items | Translated Items |
|---|---|
| 1. Learning with other students and professionals will make me a more effective health and social care team member. | 1. Imparare con altri studenti/professionisti mi renderà un membro più efficace di una squadra di assistenza sanitaria e sociale. |
| 2. Patients would ultimately benefit if health and social care student professionals worked together. | 2. Alla fine i pazienti trarrebbero beneficio se gli studenti e i professionisti dell’assistenza sanitaria e sociale lavorassero insieme. |
| 3. Shared learning with other health and social care students professionals will increase the ability to understand clinical problems. | 3. L’apprendimento condiviso con altri studenti/professionisti della sanità e dell’assistenza sociale aumenterà le mie capacità di comprendere i problemi clinici. |
| 4. Communications skills should be learned with other health and social care students/professionals. | 4. Le capacità di comunicazione dovrebbero essere apprese con altri operatori sanitari e sociali. |
| 5. Teamworking skills are vital for all health and social care students/professionals to learn. | 5. Le capacità di lavorare in gruppo sono vitali per tutti gli studenti/professionisti dell’assistenza sanitaria e sociale per apprendere. |
| 6. Shared learning will help to understand my own professional limitations. | 6. L’apprendimento condiviso mi aiuterà a comprendere i miei limiti professionali. |
| 7. Learning between health and social care students before qualification and for professionals after qualification would improve working relationships after qualification/collaborative practice. | 7. L’apprendimento tra gli studenti dell’assistenza sanitaria e sociale, prima e dopo la qualifica professionale, migliorerebbe i rapporti di lavoro e la pratica collaborativa. |
| 8. Shared learning will help me think positively about other health and social care professionals. | 8. L’apprendimento condiviso mi aiuterà a pensare positivamente verso gli altri professionisti sanitari e sociali. |
| 9. For small group learning to work, students/professionals need to respect and trust each other. | 9. Per imparare a lavorare in piccoli gruppi, studenti e professionisti devono rispettarsi e fidarsi l’uno dell’altro. |
| 10. I do not want to waste time learning with other health and social care students/professionals. | 10. Non voglio perdere tempo a imparare con altri studenti e professionisti sanitari e sociali. |
| 11. It is not necessary for undergraduate/postgraduate health and social care students/professionals to learn together. | 11. Non è necessario che gli studenti laureati e post laureati nell’assistenza sanitaria e sociale apprendano insieme. |
| 12. Clinical problem solving can only be learnt effectively with students/professionals from my own school/organization. | 12. La risoluzione dei problemi clinici può essere appresa efficacemente solo con studenti/professionisti della mia scuola/organizzazione. |
| 13. Shared learning with other health and social care professionals will help me to communicate better with patients and other professionals. | 13. L’apprendimento condiviso con altri professionisti sanitari e sociali mi aiuterà a comunicare meglio con i pazienti e gli altri professionisti. |
| 14. I would welcome the opportunity to work on small group projects with other health and social care students/professionals. | 14. Gradirei l’opportunità di lavorare su progetti in piccoli gruppi con altri studenti di assistenza sanitaria e sociale. |
| 15. I would welcome the opportunity to share some generic lectures, tutorials or workshops with other health and social care students/professionals. | 15. Gradirei l’opportunità di condividere alcune lezioni di base, tutorial o seminari con altri studenti/professionisti dell’assistenza sanitaria e sociale. |
| 16. Shared learning and practice will help me clarify the nature of patients’ or clients’ problems. | 16. L’apprendimento e la pratica condivisi mi aiuteranno a chiarire la natura dei problemi dei pazienti. |
| 17. Shared learning before and after qualification will help me become a better team worker. | 17. L’apprendimento condiviso prima e dopo la qualifica professionale mi aiuterà a diventare un miglior collaboratore. |
| 18. I am unsure what my professional role will be/is. | 18. Non sono sicuro di quale sia/sarà il mio ruolo di professionista. |
| 19. I have to acquire much more knowledge and skill than other students/professionals in my own faculty/organization. | 19. Devo acquisire molte più conoscenze e abilità rispetto ad altri studenti/professionisti nella mia facoltà/organizzazione. |
| Tot (n = 414) | EFA (n = 207) | CFA (n = 207) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Disciplines | ||||||
| Physiotherapy | 219 | 52.9 | 29 | 14.0 | 190 | 91.8 |
| Nursing | 34 | 8.2 | 17 | 8.2 | 17 | 8.2 |
| Medicine | 120 | 29.0 | 120 | 58.0 | - | - |
| Dentistry | 41 | 9.9 | 41 | 19.8 | - | - |
| Sex | ||||||
| Females | 240 | 58.0 | 147 | 71.0 | 93 | 44.9 |
| Males | 174 | 42.0 | 60 | 29.0 | 114 | 55.1 |
| Age | ||||||
| Years (Mean; standard deviation) | 24.37 | 4.23 | 25.1 | 4.06 | 23.64 | 4.28 |
| 1° Item Analysis | 2° Item Analysis | |||
|---|---|---|---|---|
| Corrected Item-Total Correlation | Cronbach’s Alpha if Item Deleted | Corrected Item-Total Correlation | Cronbach’s Alpha if Item Deleted | |
| RIPS1 | 0.578 | 0.798 | 0.602 | 0.907 |
| RIPS2 | 0.528 | 0.799 | 0.586 | 0.907 |
| RIPS3 | 0.580 | 0.797 | 0.604 | 0.907 |
| RIPS4 | 0.536 | 0.798 | 0.576 | 0.908 |
| RIPS5 | 0.608 | 0.794 | 0.627 | 0.906 |
| RIPS6 | 0.570 | 0.795 | 0.608 | 0.907 |
| RIPS7 | 0.691 | 0.790 | 0.731 | 0.902 |
| RIPS8 | 0.612 | 0.792 | 0.691 | 0.903 |
| RIPS9 | 0.538 | 0.799 | 0.549 | 0.909 |
| RIPS10 | 0.149 | 0.824 | ||
| RIPS11 | 0.197 | 0.820 | ||
| RIPS12 | 0.021 | 0.835 | ||
| RIPS13 | 0.618 | 0.793 | 0.641 | 0.905 |
| RIPS14 | 0.545 | 0.797 | 0.602 | 0.907 |
| RIPS15 | 0.561 | 0.796 | 0.587 | 0.907 |
| RIPS16 | 0.570 | 0.797 | 0.608 | 0.906 |
| RIPS17 | 0.680 | 0.792 | 0.712 | 0.903 |
| RIPS18 | −0.130 | 0.843 | ||
| RIPS19 | 0.164 | 0.820 | ||
| New Item Scale | Former Item Scale | Factor 1 | Factor 2 | Communalities | Cronbach’s Alpha | |
|---|---|---|---|---|---|---|
| Factor 1-Teamwork & collaboration | I-RIPLS 1 | RIPLS1 | 0.722 | −0.089 | 0.584 | 0.883 |
| I-RIPLS 2 | RIPLS5 | 0.756 | −0.087 | 0.537 | ||
| I-RIPLS 3 | RIPLS6 | 0.614 | 0.002 | 0.519 | ||
| I-RIPLS 4 | RIPLS7 | 0.782 | 0.016 | 0.622 | ||
| I-RIPLS 5 | RIPLS2 | 0.462 | 0.243 | 0.465 | ||
| I-RIPLS 6 | RIPLS8 | 0.67 | 0.117 | 0.565 | ||
| I-RIPLS 7 | RIPLS3 | 0.415 | 0.195 | 0.476 | ||
| I-RIPLS 8 | RIPLS9 | 0.623 | 0.040 | 0.405 | ||
| I-RIPLS 9 | RIPLS4 | 0.331 | 0.236 | 0.425 | ||
| Factor 2-Positive Professional Identity, Roles and Responsibility | I-RIPLS 10 | RIPLS15 | −0.008 | 0.661 | 0.654 | 0.818 |
| I-RIPLS 11 | RIPLS14 | −0.108 | 0.773 | 0.632 | ||
| I-RIPLS 12 | RIPLS16 | −0.032 | 0.760 | 0.608 | ||
| I-RIPLS 13 | RIPLS17 | 0.182 | 0.621 | 0.645 | ||
| I-RIPLS 14 | RIPLS13 | 0.270 | 0.418 | 0.515 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spada, F.; Caruso, R.; De Maria, M.; Karma, E.; Oseku, A.; Pata, X.; Prendi, E.; Rocco, G.; Notarnicola, I.; Stievano, A. Italian Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in an Undergraduate Healthcare Student Context. Healthcare 2022, 10, 1698. https://doi.org/10.3390/healthcare10091698
Spada F, Caruso R, De Maria M, Karma E, Oseku A, Pata X, Prendi E, Rocco G, Notarnicola I, Stievano A. Italian Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in an Undergraduate Healthcare Student Context. Healthcare. 2022; 10(9):1698. https://doi.org/10.3390/healthcare10091698
Chicago/Turabian StyleSpada, Florian, Rosario Caruso, Maddalena De Maria, Emiljan Karma, Aisel Oseku, Xhesika Pata, Emanuela Prendi, Gennaro Rocco, Ippolito Notarnicola, and Alessandro Stievano. 2022. "Italian Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in an Undergraduate Healthcare Student Context" Healthcare 10, no. 9: 1698. https://doi.org/10.3390/healthcare10091698
APA StyleSpada, F., Caruso, R., De Maria, M., Karma, E., Oseku, A., Pata, X., Prendi, E., Rocco, G., Notarnicola, I., & Stievano, A. (2022). Italian Translation and Validation of the Readiness for Interprofessional Learning Scale (RIPLS) in an Undergraduate Healthcare Student Context. Healthcare, 10(9), 1698. https://doi.org/10.3390/healthcare10091698









