An Ecological Analysis of Hospitalization Patterns for Diseases of the Nervous System in England and Wales over the Last 20 Years
Abstract
:1. Introduction
2. Methods
2.1. Study Sources and the Population
2.2. Statistical Analysis
3. Results
3.1. Admission Rates Stratified by Gender
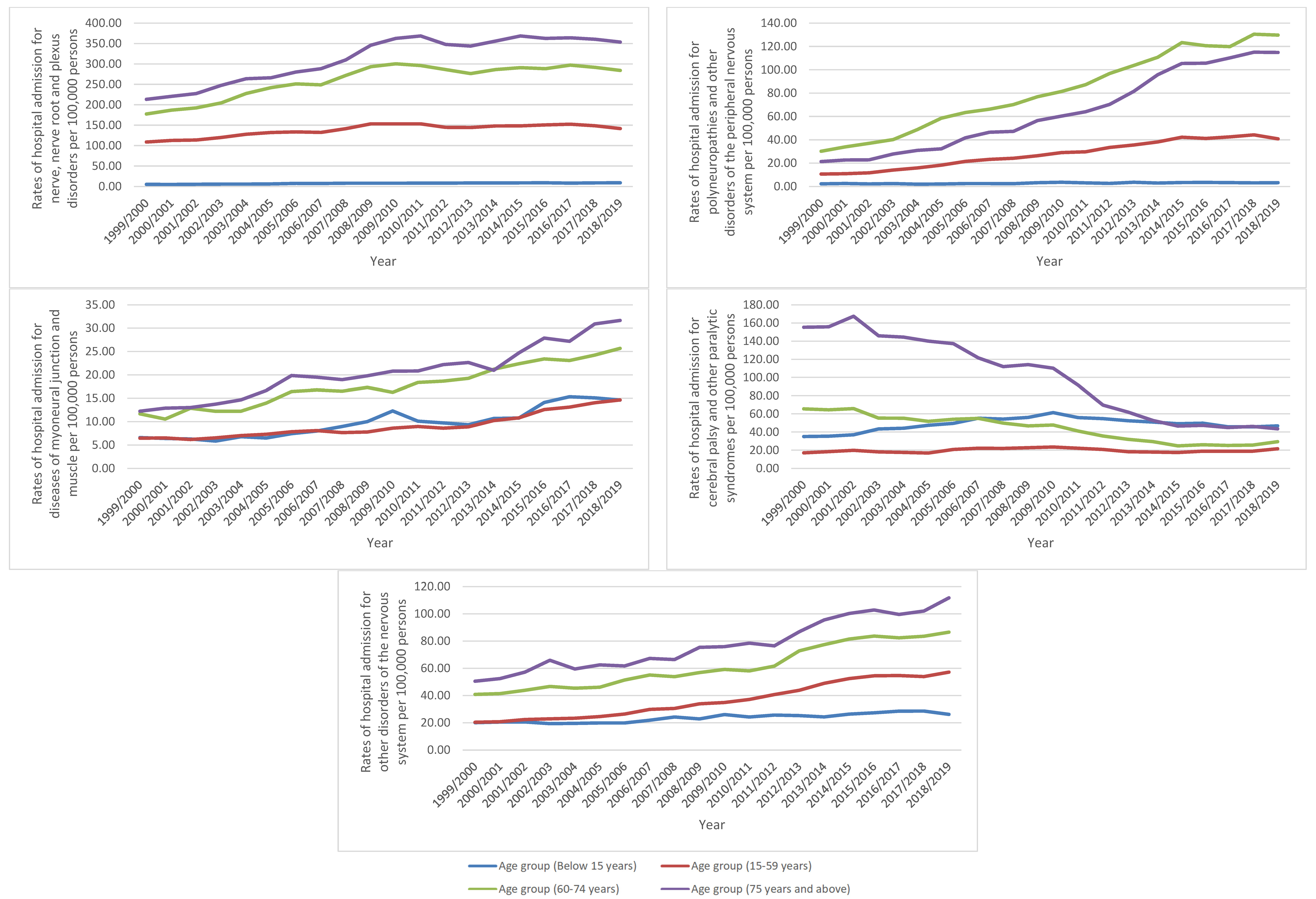
3.2. Admission Rates Stratified by Age Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. Neurol. 2017, 16, 877–897. [Google Scholar] [CrossRef]
- GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. Neurol. 2019, 18, 459–480. [Google Scholar]
- ICD10Data.com. 2021 ICD-10-CM Codes. Available online: https://www.icd10data.com/ICD10CM/Codes (accessed on 19 April 2022).
- World Health Organization. Neurological Disorders: Public Health Challenges. Available online: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=198:2008-trastornos-neurologicos&Itemid=40615&lang=en#:~:text=Neurological%20disorders%3A%20public%20health%20challenges%20describes%20and%20discusses,disorders%2C%20Parkinson%27s%20disease%2C%20stroke%20and%20traumatic%20brain%20injuries (accessed on 19 April 2022).
- Hou, Y.; Dan, X.; Babbar, M.; Wei, Y.; Hasselbalch, S.G.; Croteau, D.L.; Bohr, V.A. Ageing as a risk factor for neurodegenerative disease. Nat. Rev. Neurol. 2019, 15, 565–581. [Google Scholar] [PubMed]
- Prince, M.; Guerchet, M.; Prina, M. The Global Impact of Dementia 2013–2050. Available online: https://www.alzint.org/u/2020/08/GlobalImpactDementia2013.pdf (accessed on 19 April 2022).
- Wimo, A.; Jönsson, L.; Bond, J.; Prince, M.; Winblad, B. Alzheimer Disease International. The worldwide economic impact of dementia 2010. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2013, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Health and Social Care Information Centre (HSCIC). Hospital Episode Statistics. Available online: http://http//content.digital.nhs.uk/hes (accessed on 19 April 2022).
- NHS Wales Informatics Service. Annual PEDW Data Tables. Available online: http://www.infoandstats.wales.nhs.uk/page.cfm?pid=41010&orgid=869 (accessed on 19 April 2022).
- Office for National Statistics (ONS). Population Estimates. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed on 19 April 2022).
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the- (accessed on 19 April 2022).
- ICD10 Codes. Diseases of the Nervous System G00-G99, ICD-10-CM Codes. Available online: https://www.icd10data.com/ICD10CM/Codes/G00-G99 (accessed on 19 April 2022).
- National Institute for Neurological Disorders and Stroke. Transient Ischemic Attack. Available online: https://www.ninds.nih.gov/health-information/disorders/transient-ischemic-attack (accessed on 24 August 2022).
- Johnston, S.C.; Rothwell, P.M.; Nguyen-Huynh, M.N.; Giles, M.F.; Elkins, J.S.; Bernstein, A.L.; Sidney, S. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 2007, 369, 283–292. [Google Scholar] [CrossRef]
- Béjot, Y.; Yaffe, K. Ageing Population: A Neurological Challenge. Neuroepidemiology 2019, 52, 76–77. [Google Scholar] [CrossRef] [PubMed]
- Béjot, Y.; Bailly, H.; Graber, M.; Garnier, L.; Laville, A.; Dubourget, L.; Mielle, N.; Chevalier, C.; Durier, J.; Giroud, M. Impact of the Ageing Population on the Burden of Stroke: The Dijon Stroke Registry. Neuroepidemiology 2019, 52, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Beghi, E.; Giussani, G. Aging and the Epidemiology of Epilepsy. Neuroepidemiology 2018, 51, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Bell, G.S.; Neligan, A.; Sander, J.W. An unknown quantity—The worldwide prevalence of epilepsy. Epilepsia 2014, 55, 958–962. [Google Scholar] [CrossRef] [PubMed]
- Hemminki, K.; Li, X.; Sundquist, K. Familial risks for nerve, nerve root and plexus disorders in siblings based on hospitalisations in Sweden. J. Epidemiol. Community Health 2007, 61, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.D.; Rudolfer, S.M. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991–2001. J. Neurol. Neurosurg. Psychiatry 2003, 74, 1674–1679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gelfman, R.; Melton, L.J., 3rd; Yawn, B.P.; Wollan, P.C.; Amadio, P.C.; Stevens, J.C. Long-term trends in carpal tunnel syndrome. Neurology 2009, 72, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Latinovic, R.; Gulliford, M.C.; Hughes, R.A. Incidence of common compressive neuropathies in primary care. J. Neurol. Neurosurg. Psychiatry 2006, 77, 263–265. [Google Scholar] [PubMed]
- Ogden, C.L.; Carroll, M.D.; Curtin, L.R.; McDowell, M.A.; Tabak, C.J.; Flegal, K.M. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006, 295, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Village, J.; Rempel, D.; Teschke, K. Musculoskeletal disorders of the upper extremity associated with computer work: A systematic review. Occup. Ergon. 2005, 5, 205–218. [Google Scholar] [CrossRef]
- Public Health England. Multiple Sclerosis: Prevalence, Incidence and Smoking Status-Data Briefing. Available online: https://www.gov.uk/government/publications/multiple-sclerosis-prevalence-incidence-and-smoking-status/multiple-sclerosis-prevalence-incidence-and-smoking-status-data-briefing (accessed on 19 April 2022).
- Manouchehrinia, A.; Hedström, A.K.; Alfredsson, L.; Olsson, T.; Hillert, J.; Ramanujam, R. Association of Pre-Disease Body Mass Index With Multiple Sclerosis Prognosis. Front. Neurol. 2018, 9, 232. [Google Scholar] [PubMed]
- Olsson, T.; Barcellos, L.F.; Alfredsson, L. Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nat. Rev. Neurol. 2017, 13, 25–36. [Google Scholar] [CrossRef] [PubMed]
- G7 Academics’ Joint Statement. The Challenges of Neurodegenerative Diseases in Aging Population. Available online: https://royalsociety.org/-/media/about-us/international/g-science-statements/2017-may-aging-population.pdf?la=en-GB&hash=C665B04DAB77DE2C053D8F51E61E4379 (accessed on 19 April 2022).
- World Health Organization. Dementia: A Public Health Priority, World Health Organization—Alzheimer’s Disease International. Available online: http://www.who.int/mental_health/publications/dementia_report_2012/en/ (accessed on 19 April 2022).
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Lopez, A.D.; World Health, O.; World, B. Harvard School of Public Health. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020: Summary; Murray, C.J.L., Lopez, A.D., Eds.; World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- Stump, E. WHO report: Millions have neurological disorders worldwide. Neurol. Today 2007, 7, 25. [Google Scholar] [CrossRef]


| ICD Code | Description | Number of Admissions | Percentage from Total Number of Admissions |
|---|---|---|---|
| G00–G09 | Inflammatory diseases of the central nervous system | 168,074 | 2.3% |
| G10–G14 | Systemic atrophies primarily affecting the central nervous system | 110,205 | 1.5% |
| G20–G26 | Extrapyramidal and movement disorders | 387,080 | 5.2% |
| G30–G32 | Other degenerative diseases of the nervous system | 276,408 | 3.7% |
| G35–G37 | Demyelinating diseases of the central nervous system | 688,479 | 9.3% |
| G40–G47 | Episodic and paroxysmal disorders | 2,757,086 | 37.4% |
| G50–G59 | Nerve, nerve root, and plexus disorders | 1,632,271 | 22.1% |
| G60–G65 | Polyneuropathies and other disorders of the peripheral nervous system | 385,998 | 5.2% |
| G70–G73 | Diseases of myoneural junction and muscle | 128,052 | 1.7% |
| G80–G83 | Cerebral palsy and other paralytic syndromes | 382,065 | 5.2% |
| G89–G99 | Other disorders of the nervous system | 465,232 | 6.3% |
| Diseases | Rate of Diseases in 1999 per 100,000 Persons (95% CI) | Rate of Diseases in 2019 per 100,000 Persons (95% CI) | Percentage Change from 1999–2019 | p-Value |
|---|---|---|---|---|
| Inflammatory diseases of the central nervous system | 9.11 (8.85–9.37) | 23.17 (22.79–23.56) | 154.4% | p ≤ 0.001 |
| Systemic atrophies primarily affecting the central nervous system | 8.26 (8.01–8.51) | 12.01 (11.73–12.29) | 45.4% | p ≤ 0.01 |
| Extrapyramidal and movement disorders | 30.01 (29.54–30.48) | 43.80 (43.27–44.33) | 46.0% | p ≤ 0.01 |
| Other degenerative diseases of the nervous system | 24.52 (24.10–24.95) | 26.95 (26.53–27.37) | 9.9% | p ≤ 0.05 |
| Demyelinating diseases of the central nervous system | 35.69 (35.18–36.21) | 92.90 (92.13–93.68) | 160.3% | p ≤ 0.001 |
| Episodic and paroxysmal disorders | 177.81 (176.67–178.96) | 302.59 (301.19–303.99) | 70.2% | p ≤ 0.01 |
| Nerve, nerve root, and plexus disorders | 106.25 (105.36–107.13) | 158.49 (157.48–159.51) | 49.2% | p ≤ 0.01 |
| Polyneuropathies and other disorders of the peripheral nervous system | 12.50 (12.20–12.81) | 54.48 (53.88–55.07) | 335.6% | p ≤ 0.001 |
| Diseases of myoneural junction and muscle | 7.62 (7.38–7.86) | 17.95 (17.61–18.29) | 135.5% | p ≤ 0.001 |
| Cerebral palsy and other paralytic syndromes | 37.30 (36.78–37.83) | 29.44 (29.01–29.88) | −21.1% | p ≤ 0.05 |
| Other disorders of the nervous system | 25.37 (24.94–25.80) | 61.58 (60.95–62.21) | 142.7% | p ≤ 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naser, A.Y.; Dahmash, E.Z.; Al-Daghastani, T.; Alwafi, H.; Abu Hamdah, S.; Alsairafi, Z.K.; Alsaleh, F.M. An Ecological Analysis of Hospitalization Patterns for Diseases of the Nervous System in England and Wales over the Last 20 Years. Healthcare 2022, 10, 1670. https://doi.org/10.3390/healthcare10091670
Naser AY, Dahmash EZ, Al-Daghastani T, Alwafi H, Abu Hamdah S, Alsairafi ZK, Alsaleh FM. An Ecological Analysis of Hospitalization Patterns for Diseases of the Nervous System in England and Wales over the Last 20 Years. Healthcare. 2022; 10(9):1670. https://doi.org/10.3390/healthcare10091670
Chicago/Turabian StyleNaser, Abdallah Y., Eman Zmaily Dahmash, Tamara Al-Daghastani, Hassan Alwafi, Sawsan Abu Hamdah, Zahra K. Alsairafi, and Fatemah M. Alsaleh. 2022. "An Ecological Analysis of Hospitalization Patterns for Diseases of the Nervous System in England and Wales over the Last 20 Years" Healthcare 10, no. 9: 1670. https://doi.org/10.3390/healthcare10091670
APA StyleNaser, A. Y., Dahmash, E. Z., Al-Daghastani, T., Alwafi, H., Abu Hamdah, S., Alsairafi, Z. K., & Alsaleh, F. M. (2022). An Ecological Analysis of Hospitalization Patterns for Diseases of the Nervous System in England and Wales over the Last 20 Years. Healthcare, 10(9), 1670. https://doi.org/10.3390/healthcare10091670






