Comprehending Nutrition and Lifestyle Behaviors of People with Metabolic Syndrome: A Focus Group Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Respondents
2.3. Focus Group Discussions
2.4. Analyses
3. Results
3.1. Characteristics of Study Respondents
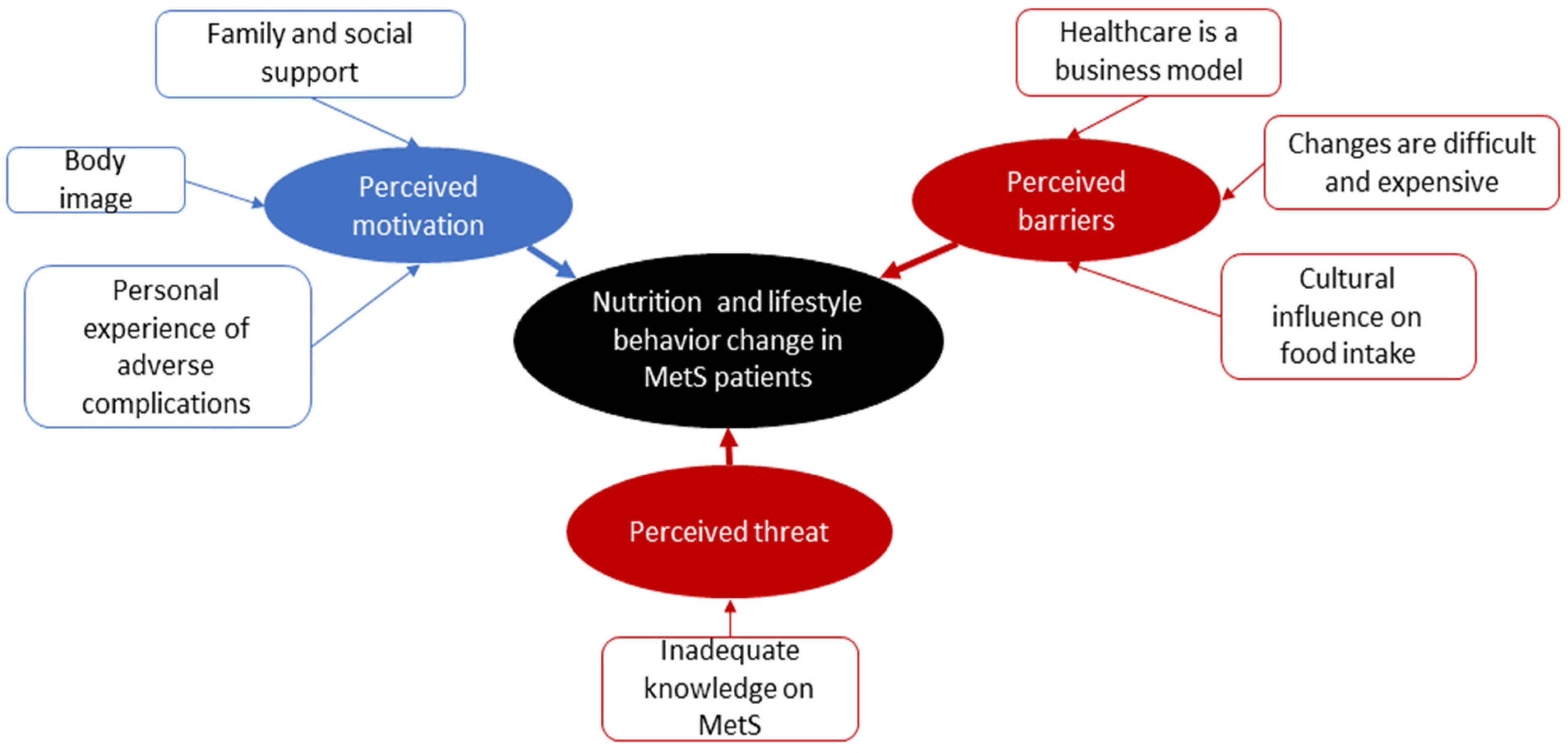
3.2. Themes
3.2.1. Perceived Motivation to Adopt Healthy Nutrition and Lifestyle Behaviors
3.2.2. Perceived Barriers toward Healthy Nutrition and Lifestyle Behaviors
3.2.3. Perceived Threat towards the Adoption of Healthy Nutrition and Lifestyle Behaviors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martin, C.A.; Gowda, U.; Smith, B.J.; Renzaho, A.M.N. Systematic review of the effect of lifestyle interventions on the components of the metabolic syndrome in South Asian migrants. J. Immigr. Minority Health 2018, 20, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Nyenwe, E.A.; Dagogo-Jack, S. Metabolic syndrome, prediabetes and the science of primary prevention. Minerva Endocrinol. 2011, 36, 129–145. [Google Scholar] [PubMed]
- Isomaa, B. A major health hazard: The metabolic syndrome. Life Sci. 2003, 73, 2395–2411. [Google Scholar] [CrossRef]
- Lim, K.G.; Cheah, W.K. A review of metabolic syndrome research in Malaysia. Med. J. Malays. 2016, 71 (Suppl. S1), 20–28. [Google Scholar]
- Rampal, S.; Mahadeva, S.; Guallar, E.; Bulgiba, A.; Mohamed, R.; Rahmat, R.; Arif, M.T.; Rampal, L. Ethnic differences in the prevalence of metabolic syndrome: Results from a multi-ethnic population-based survey in Malaysia. PLoS ONE 2012, 7, e46365. [Google Scholar] [CrossRef]
- Tan, A.K.G.; Dunn, R.A.; Yen, S.T. Ethnic disparities in metabolic syndrome in Malaysia: An analysis by risk factors. Metab. Syndr. Relat. Disord. 2011, 9, 441–451. [Google Scholar] [CrossRef]
- Iqbal, S.P.; Ramadas, A.; Fatt, Q.K.; Shin, H.L.; Onn, W.Y.; Kadir, K.A. Relationship of sociodemographic and lifestyle factors and diet habits with metabolic syndrome (MetS) among three ethnic groups of the Malaysian population. PLoS ONE 2020, 15, e0224054. [Google Scholar] [CrossRef]
- Marks, D.F. The quest for meaningful theory in health psychology. J. Health Psychol. 2008, 13, 977–981. [Google Scholar] [CrossRef]
- Coleman, M.T.; Pasternak, R.H. Effective strategies for behavior change. Prim. Care Clin. Off. Pract. 2012, 39, 281–305. [Google Scholar] [CrossRef]
- Bully, P.; Sánchez, T.; Zabaleta-del-Olmo, E.; Pombo, H.; Grandes, G. Evidence from interventions based on theoretical models for lifestyle modification (physical activity, diet, alcohol and tobacco use) in primary care settings: A systematic review. Prev. Med. 2015, 76, S76–S93. [Google Scholar] [CrossRef]
- Finfgeld, D.L.; Wongvatunyu, S.; Conn, V.S.; Grando, V.T.; Russell, C.L. Health belief model and reversal theory: A comparative analysis. J. Adv. Nurs. 2003, 43, 288–297. [Google Scholar] [CrossRef]
- Chen, S.-H.; Chen, S.-C.; Lai, Y.-P.; Chen, P.-H.; Huang, T.-Y.; Lin, C.-C.; Yeh, K.-Y. Correlates between health beliefs and health-promoting lifestyle profiles in the development of metabolic syndrome in Taiwan. Asia Pac. J. Public Health 2019, 31, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.W.S.; Chair, S.Y.; Lee, F.K. Factors associated with health-promoting behavior of people with or at high risk of metabolic syndrome: Based on the Health Belief Model. Appl. Nurs. Res. 2015, 28, 197–201. [Google Scholar] [CrossRef]
- Park, Y.; Kim, D. Health Belief Model-based needs assessment for development of a metabolic syndrome risk reduction program for Korean male blue-collar workers in small-sized companies. Korean J. Occup. Health Nurs. 2018, 27, 235–246. [Google Scholar] [CrossRef]
- Hirakawa, Y.; Chiang, C.; Yasuda, U.M.; Aoyama, A. Health-related behavior of the people who neglect the specific health guidance for metabolic syndrome control. Nagoya J. Med. Sci. 2019, 81, 199–205. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Wong, L.P. Focus group discussion: A tool for health and medical research. Singap. Med. J. 2008, 49, 256–261. [Google Scholar]
- Roden, J. Validating the revised Health Belief Model for young families: Implications for nurses’ health promotion practice. Nurs. Health Sci. 2004, 6, 247–259. [Google Scholar] [CrossRef]
- Onwuegbuzie, A.J.; Dickinson, W.B.; Leech, N.L.; Zoran, A.G. A qualitative framework for collecting and analyzing data in focus group research. Intl. J. Qual. Methods 2009, 8, 1–21. [Google Scholar] [CrossRef]
- National Coordinating Committee of Food and Nutrition (NCCFN). Malaysian Dietary Guidelines; Ministry of Health: Kuala Lumpur, Malaysia, 2010. [Google Scholar]
- Bredland, E.L.; Söderström, S.; Vik, K. Challenges and motivators to physical activity faced by retired men when ageing: A qualitative study. BMC Public Health 2018, 18, 627. [Google Scholar] [CrossRef]
- Chen, W.C.; Lin, C.C. Constructing a peer-led self-management program for elderly patients with metabolic syndrome. J. Nurs. 2017, 64, 111–119. [Google Scholar] [CrossRef]
- Gardiner, S.; Glogowska, M.; Stoddart, C.; Pendlebury, S.; Lasserson, D.; Jackson, D. Older people’s experiences of falling and perceived risk of falls in the community: A narrative synthesis of qualitative research. Int. J. Older People Nurs. 2017, 12, e12151. [Google Scholar] [CrossRef] [PubMed]
- Wray, F.; Clarke, D. Longer-term needs of stroke survivors with communication difficulties living in the community: A systematic review and thematic synthesis of qualitative studies. BMJ Open 2017, 7, e017944. [Google Scholar] [CrossRef] [PubMed]
- Pindus, D.M.; Mullis, R.; Lim, L.; Wellwood, I.; Rundell, A.V.; Abd Aziz, N.A.; Mant, J. Stroke survivors’ and informal caregivers’ experiences of primary care and community healthcare services—A systematic review and meta-ethnography. PLoS ONE 2018, 13, e0192533. [Google Scholar] [CrossRef]
- Reid, C.; Seymour, J.; Jones, C. A thematic synthesis of the experiences of adults living with hemodialysis. Clin. J. Am. Soc. Nephrol. 2016, 11, 1206–1218. [Google Scholar] [CrossRef]
- Sulaiman, N.D.; Furler, J.S.; Hadj, E.J.; Corbett, H.M.; Young, D.Y.L. Stress, culture and ‘home’: Social context in Turkish and Arabic-speaking Australians’ views of diabetes prevention. Health Promot. J. Aust. 2007, 18, 63–68. [Google Scholar] [CrossRef]
- Daivadanam, M.; Wahlström, R.; Ravindran, T.S.; Thankappan, K.; Ramanathan, M. Conceptual model for dietary behaviour change at household level: A ‘best-fit’ qualitative study using primary data. BMC Public Health 2014, 14, 574. [Google Scholar] [CrossRef]
- Whyte, J. The metabolic syndrome: Early clues, effective management. Consultant 2005, 45, 1195–1200. [Google Scholar]
- Azlan Mahadzir, M.D.; Quek, K.F.; Ramadas, A. Nutrition and lifestyle behavior peer support program for adults with metabolic syndrome: Outcomes and lessons learned from a feasibility trial. Nutrients 2020, 12, 1091. [Google Scholar] [CrossRef]
- Azlan Mahadzir, M.D.; Quek, K.F.; Ramadas, A. Process evaluation of a nutrition and lifestyle behavior peer support program for adults with metabolic syndrome. Int. J. Environ. Res. Public Health 2020, 17, 2641. [Google Scholar] [CrossRef]
- Noor, N.M.; Gandhi, A.D.; Ishak, I.; Wok, S. Development of indicators for family well-being in Malaysia. Soc. Indic. Res. 2014, 115, 279–318. [Google Scholar] [CrossRef]
- Embuldeniya, G.; Veinot, P.; Bell, E.; Bell, M.; Nyhof-Young, J.; Sale, J.E.M.; Britten, N. The experience and impact of chronic disease peer support interventions: A qualitative synthesis. Patient Educ. Couns. 2013, 92, 3–12. [Google Scholar] [CrossRef]
- Parry, M.; Watt-Watson, J. Peer support intervention trials for individuals with heart disease: A systematic review. Eur. J. Cardiovasc. Nurs. 2010, 9, 57–67. [Google Scholar] [CrossRef]
- Fisher, E.B.; Boothroyd, R.I.; Elstad, E.A.; Hays, L.; Henes, A.; Maslow, G.R.; Velicer, C. Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: Systematic reviews. Clin. Diabetes Endocrinol. 2017, 3, 4. [Google Scholar] [CrossRef]
- Bhan, N.; Madhira, P.; Muralidharan, A.; Kulkarni, B.; Murthy, G.V.S.; Basu, S.; Kinra, S. Health needs, access to healthcare, and perceptions of ageing in an urbanizing community in India: A qualitative study. BMC Geriatr. 2017, 17, 156. [Google Scholar] [CrossRef]
- Tan, N.C.; Cheah, S.L.; Teo, E.K. A qualitative study of health-seeking behavior of Hepatitis B carriers. Singap. Med. J. 2005, 46, 6–10. [Google Scholar]
- Wang, C.P.; Li, Y.; Wang, S. Health literacy evaluation index system for patients with metabolic syndrome from clinical perspective. Chin. Gernal Pract. 2016, 19, 1182–1187. [Google Scholar] [CrossRef]
- Enwald, H.; Hirvonen, N.; Huotari, M.L.; Korpelainen, R.; Pyky, R.; Savolainen, M.; Salonurmi, T.; Keränen, A.-M.; Jokelainen, T.; Niemelä, R. Everyday health information literacy among young men compared with adults with high risk for metabolic syndrome—A cross-sectional population-based study. J. Inf. Sci. 2015, 42, 344–355. [Google Scholar] [CrossRef]
- Solbrig, L.; Jones, R.; Kavanagh, D.; May, J.; Parkin, T.; Andrade, J. People trying to lose weight dislike calorie counting apps and want motivational support to help them achieve their goals. Internet Interv. 2017, 7, 23–31. [Google Scholar] [CrossRef]
- Narayanan, P.; Meng, O.L.; Mahanim, O. Do the prevalence and components of metabolic syndrome differ among different ethnic groups? A cross-sectional study among obese Malaysian adolescents. Metab. Syndr. Relat. Disord. 2011, 9, 389–395. [Google Scholar] [CrossRef]
- Clarke, V.A.; Lovegrove, H.; Williams, A.; Machperson, M. Unrealistic optimism and the Health Belief Model. J. Behav. Med. 2000, 23, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Kudo, Y.; Okada, M.; Tsunoda, M.; Satoh, T.; Aizawa, Y. A lifestyle to prevent or combat the metabolic syndrome among Japanese workers: Analyses using the Health Belief Model and the multidimensional health locus of control. Ind. Health 2011, 49, 365–373. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Azlan Mahadzir, M.D.; Quek, K.F.; Ramadas, A. Group-based lifestyle intervention strategies for metabolic syndrome: A scoping review and strategic framework for future research. Medicina 2021, 57, 1169. [Google Scholar] [CrossRef] [PubMed]
- Fereday, J.; Muir-Cochrane, E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int. J. Qual. Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Michie, S.; Crey, R.N.; Johnston, M.; Rothman, A.J.; de Bruin, M.; Kelly, M.P.; Connell, L.E. From theory-inspired to theory-based interventions: A protocol for developing and testing methodology for linking behaviour change techniques to theoretical mechanism of action. Ann. Behav. Med. 2018, 52, 501–512. [Google Scholar] [CrossRef]
- Johnson, M.J.; May, C.R. Promoting professional behaviour change in healthcare: What intervention work, and why a theory-led overview of systematic review. BMJ Open 2015, 5, e008592. [Google Scholar] [CrossRef]
| Characteristics | Mean (SD) | n (%) | |
|---|---|---|---|
| Age | 51.0 (10.3) | ||
| Sex | Male | 6 (28.6) | |
| Female | 15 (71.4) | ||
| Marital status | Single | 1 (3.4) | |
| Married | 15 (71.4) | ||
| Widowed/separated | 5 (23.8) | ||
| Education level | Secondary | 5 (23.8) | |
| Tertiary | 16 (76.2) | ||
| Occupation | Employed/self-employed | 15 (71.4) | |
| Unemployed | 1 (4.7) | ||
| Retired | 5 (23.8) | ||
| Personal income (MYR) | <2000 | 3 (14.3) | |
| 2000–3999 | 5 (23.8) | ||
| 4000–5999 | 5 (23.8) | ||
| >6000 | 8 (38.1) | ||
| Metabolic risk factors | Abdominal obesity | 21 (100.0) | |
| Hypertension | 21 (100.0) | ||
| Diabetes | 19 (90.5) | ||
| Dyslipidemia | 7 (33.3) | ||
| Hypertriglyceridemia | 9 (42.9) |
| Themes | Example of Responses |
|---|---|
| Body image | “You can eat all the pills, but you will see the difference only once you sweat and eat better”. “The tummy has become large until I feel tired carrying it”. “I only started exercising when my dermatologist said it helps get rid of my wrinkles”. |
| Personal experience of Adverse complication | “I’ve made up in my mind, but I’m not ready to go yet as I am not sure how to start.” |
| “A couple of years ago, my father had a stroke at 59 years old—could not move, could not eat, could not do anything, and depend on us (the children)...it really started all of us thinking and decided to change. Whatever goes inside my husband’s and my children’s mouths are taken care of. It will be too late when we get a stroke. Why want to trouble everyone around us because of our bad habits…” | |
| Family and social support | “I think that means a lot when you got somebody else in the house that’s take care of food and drinks and conscious about food every day”. “I always join my neighbor to walk around the neighborhood. Usually, we will do it in a group. I feel very moved to go for a walk. My wife and kids are together too. On weekends, we usually have a barbeque get-together. That kind of support makes me feel better about myself.” “My husband is a jealous type. If he does not like it, you better not do it. Like walking and all, he can never see me doing it. Because when I do it, and he is lazy, he feels intimidated.” |
| Themes | Example of Responses |
|---|---|
| Healthcare as a business model | “I always heard ‘you are what you eat’, but doctors are busy prescribing medications only.” “…sometimes when the doctors prescribed too many medications, they act as they work for the pharmacy.” “I think doctors give too much medication until five or six different medicines will cancel out something.” |
| Difficult and expensive nutrition and lifestyle behavior changes | “I bought all the weight loss vitamins (supplements) for nearly 10,000 (MYR), it feels slimmer for a while, but after a year, I feel my body expands.” “Once you have been off a diet and go back, it’s just harder to go back.” “Health needs discipline. That is why a lot of successful people have a healthy life. They have the discipline to be healthy.” |
| Cultural influence on food intake | “We as Malaysians can never stop eating rice. Make rice healthy and then only tell us to diet.” “We are told what to eat since we are kids. If you are Chinese, you will eat more soup and not eat at night. It’s different from Indian, Malay and any other race in Malaysia.” |
| Themes | Example of Responses |
|---|---|
| Inadequate knowledge of metabolic syndrome | “We only know about diabetes, high blood pressure, and high blood cholesterol”. “We were only told to eat properly, exercise, and eat our medication. Metabolic syndrome is new. If you said it’s the big tummy problem, that’s what I call fat.” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahadzir, M.D.A.; Quek, K.F.; Ramadas, A. Comprehending Nutrition and Lifestyle Behaviors of People with Metabolic Syndrome: A Focus Group Study. Healthcare 2022, 10, 1653. https://doi.org/10.3390/healthcare10091653
Mahadzir MDA, Quek KF, Ramadas A. Comprehending Nutrition and Lifestyle Behaviors of People with Metabolic Syndrome: A Focus Group Study. Healthcare. 2022; 10(9):1653. https://doi.org/10.3390/healthcare10091653
Chicago/Turabian StyleMahadzir, Muhammad Daniel Azlan, Kia Fatt Quek, and Amutha Ramadas. 2022. "Comprehending Nutrition and Lifestyle Behaviors of People with Metabolic Syndrome: A Focus Group Study" Healthcare 10, no. 9: 1653. https://doi.org/10.3390/healthcare10091653
APA StyleMahadzir, M. D. A., Quek, K. F., & Ramadas, A. (2022). Comprehending Nutrition and Lifestyle Behaviors of People with Metabolic Syndrome: A Focus Group Study. Healthcare, 10(9), 1653. https://doi.org/10.3390/healthcare10091653







