Fetal Fibronectin and Cervical Length as Predictors of Spontaneous Onset of Labour and Delivery in Term Pregnancies
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Henderson, J.; Redshaw, M. Sociodemographic differences in women’s experience of early labour care: A mixed methods study. BMJ Open 2017, 7, e016351. [Google Scholar] [CrossRef] [PubMed]
- Sarah Beake, R.M.; Chang, Y.S.; Helen Cheyne, R.M.; Spiby, H.; RM, J.S.; Bick, D. Experiences of early labour management from perspectives of women, labour companions and health professionals: A systematic review of qualitative evidence. Midwifery 2018, 57, 69–84. [Google Scholar]
- Lalonde, A.B.; Butt, C.; Bucio, A. Maternal health in Canadian Aboriginal communities: Challenges and opportunities. J. Obstet. Gynaecol. Can. 2009, 31, 956–962. [Google Scholar] [CrossRef]
- Tess, B.H.; Glenister, H.M.; Rodrigues, L.C.; Wagner, M.B. Incidence of hospital-acquired infection and length of hospital stay. Eur. J. Clin. Microbiol. Infect. Dis. 1993, 12, 81–86. [Google Scholar] [CrossRef]
- Jia, H.; Li, L.; Li, W.; Hou, T.; Ma, H.; Yang, Y.; Wu, A.; Liu, Y.; Wen, J.; Yang, H.; et al. Impact of Healthcare-Associated Infections on Length of Stay: A Study in 68 Hospitals in China. Biomed Res. Int. 2019, 2019, 2590563. [Google Scholar] [CrossRef]
- Faltin-Traub, E.F.; Boulvain, M.; Faltin, D.L.; Extermann, P.; Irion, O. Reliability of the Bishop score before labour induction at term. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 112, 178–181. [Google Scholar] [CrossRef]
- Wormer, K.C.; Williford, A.E. Bishop Score. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2019. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470368/ (accessed on 10 April 2022).
- Bolt, L.A.; Chandiramani, M.; De Greeff, A.; Seed, P.T.; Kurtzman, J.; Shennan, A.H. The value of combined cervical length measurement and fetal fibronectin testing to predict spontaneous preterm birth in asymptomatic high-risk women. J. Matern. Fetal Neonatal Med. 2011, 24, 928–932. [Google Scholar] [CrossRef]
- Stock, S.J.; Horne, M.; Bruijn, M.; White, H.; Boyd, K.A.; Heggie, R.; Wotherspoon, L.; Aucott, L.; Morris, R.K.; Dorling, J.; et al. Development and validation of a risk prediction model of preterm birth for women with preterm labour symptoms (the QUIDS study): A prospective cohort study and individual participant data meta-analysis. PLoS Med. 2021, 18, e1003686. [Google Scholar] [CrossRef]
- Fuchs, I.B.; Henrich, W.; Osthues, K.; Dudenhausen, J.W. Sonographic cervical length in singleton pregnancies with intact membranes presenting with threatened preterm labor. Ultrasound Obstet. Gynecol. 2004, 24, 554–557. [Google Scholar] [CrossRef]
- Foster, C.; Shennan, A.H. Fetal fibronectin as a biomarker of preterm labor: A review of the literature and advances in its clinical use. Biomark. Med. 2014, 8, 471–484. [Google Scholar] [CrossRef]
- Berghella, V.; Hayes, E.; Visintine, J.; Baxter, J.K. Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database Syst. Rev. 2008, 2008, CD006843. [Google Scholar] [CrossRef] [PubMed]
- Ruma, M.S.; Banker, W.M. Availability and use of fetal fibronectin testing and transvaginal ultrasound for preterm labor evaluation in the United States. J. Matern. Fetal Neonatal Med. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Holzer, I.; Koch-Trappel, M.; Leitich, H.; Meyer, E.L.; Farr, A.; Helmer, H. The fetal fibronectin test is superior to cervical length measurement in predicting preterm birth in twin pregnancies: A retrospective observational study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 247, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Ahner, R.; Egarter, C.; Kiss, H.; Heinzl, K.; Zeillinger, R.; Schatten, C.; Dormeier, A.; Husslein, P. Fetal fibronectin as a selection criterion for induction of term labor. Am. J. Obstet. Gynecol. 1995, 173, 1513–1517. [Google Scholar] [CrossRef]
- Ahner, R.; Kub-Csizi, P.; Heinzl, H.; Bikas, D.; Rabl, M.; Wagenbichler, P.; Husslein, P. The fast-reacting fetal fibronectin test: A screening method for better prediction of the time of delivery. Am. J. Obstet. Gynecol. 1997, 177, 1478–1482. [Google Scholar] [CrossRef]
- Kiss, H.; Ahner, R.; Hohlagschwandtner, M.; Leitich, H.; Husslein, P. Fetal fibronectin as a predictor of term labor: A literature review. Acta Obstet. Gynecol. Scand. 2000, 79, 3–7. [Google Scholar] [CrossRef]
- Lockwood, C.J.; Moscarelli, R.D.; Wein, R.; Lynch, L.; Lapinski, R.H.; Ghidini, A. Low concentrations of vaginal fetal fibronectin as a predictor of deliveries occurring after 41 weeks. Am. J. Obstet. Gynecol. 1994, 171, 1–4. [Google Scholar] [CrossRef]
- Luton, D.; Guibourdenche, J.; Sibony, O.; Braig, S.; Benzakine, Y.; Oury, J.-F.; Porquet, D.; Blot, P. Fetal fibronectin in the cervical secretion predicts accurately the onset of labor at term. Eur. J. Obstet. Gynecol. Reprod. Biol. 1997, 74, 161–164. [Google Scholar] [CrossRef]
- Rumbold, A.; Kruske, S.; Boyle, J.; Weckert, R.; Putland, S.; Giles, L.; Barclay, L.; Kildea, S. Can the fetal fibronectin test be used by remote dwelling pregnant women to predict the onset of labour at term and delay transfer for birth in regional settings? Rural Remote Health 2013, 13, 2126. [Google Scholar] [CrossRef]
- Deshpande, S.N.; van Asselt, A.D.; Tomini, F.; Armstrong, N.; Allen, A.; Noake, C.; Khan, K.; Severens, J.L.; Kleijnen, J.; Westwood, M.E. Rapid fetal fibronectin testing to predict preterm birth in women with symptoms of premature labour: A systematic review and cost analysis. Health Technol. Assess. 2013, 17, 1–138. [Google Scholar] [CrossRef]
- Giles, W.; Bisits, A.; Knox, M.; Madsen, G.; Smith, R. The effect of fetal fibronectin testing on admissions to a tertiary maternal-fetal medicine unit and cost savings. Am. J. Obstet. Gynecol. 2000, 182, 439–442. [Google Scholar] [CrossRef]
- Katsura, D.; Tsuji, S.; Hayashi, K.; Tokoro, S.; Yamada, K.; Suzuki, K.; Kimura, F.; Murakami, T. Predictive factors of labour onset using ultrasonography. J. Obstet. Gynaecol. 2021, 41, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.T.V.; Lau, K.W.; Hui, W.; Lau, C.H.; Leung, W.C.; Lau, W.L. Sonographic measurement of cervical length and head perineum distance before labor to predict time of delivery. J. Matern. Fetal Neonatal Med. 2021, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Mukherji, J.; Bhadra, A.; Ghosh, S.K.; Hazra, A.; Anant, M.; Bhattacharya, S.K.; Das, B.; Banu, S. Cervical length measurement in nulliparous women at term by ultrasound & its relationship to spontaneous onset of labour. Indian J. Med. Res. 2017, 146, 498–504. [Google Scholar] [PubMed]
- Mouw, R.J.; Egberts, J.; van Roosmalen, J.J.; Kragt, H. High cervical fetal-fibronectin concentrations and birth within 3 days in pregnancies of 41 weeks or more. N. Engl. J. Med. 1995, 332, 1105. [Google Scholar] [CrossRef] [PubMed]
- Healey, G.K.; Macdonald, W.A.; Grzybowski, S.; Nevin, R.; Kornelsen, J.; Hogg, W.E. Exploring fetal fibronectin testing as a predictor of labour onset: In parturient women from isolated communities. Can. Fam. Physician 2018, 64, e108–e114. [Google Scholar] [PubMed]
- Walke, S.; Deshpande, B.; Patankar, A. Assessment of transvaginal ultrasound measurement of cervical length for prediction of spontaneous onset of labor at term. Indian J. Obstet. Gynecol. Res. 2020, 7, 421–425. [Google Scholar] [CrossRef]
- Tolaymat, L.L.; Gonzalez-Quintero, V.H.; Sanchez-Ramos, L.; Kaunitz, A.; Wludyka, P.; O’Sullivan, M.J.; Martin, D. Cervical length and the risk of spontaneous labor at term. J. Perinatol. 2007, 27, 749–753. [Google Scholar] [CrossRef][Green Version]
- Strobel, E.; Sladkevicius, P.; Rovas, L.; Smet, F.D.; Karlsson, E.D.; Valentin, L. Bishop score and ultrasound assessment of the cervix for prediction of time to onset of labor and time to delivery in prolonged pregnancy. Ultrasound Obstet. Gynecol. 2006, 28, 298–305. [Google Scholar] [CrossRef]
- Hoogeveen, M.M.; Stoutenbeek, P.; Visser, G.H.A. Methods of sonographic cervical length measurement in pregnancy: A review of the literature. J. Matern. Fetal Neonatal Med. 2006, 19, 755–762. [Google Scholar] [CrossRef]
- van Baaren, G.J.; Vis, J.Y.; Wilms, F.F.; Oudijk, M.A.; Kwee, A.; Porath, M.M.; Oei, G.; Scheepers, H.C.J.; Spaanderman, M.E.A.; Bloemenkamp, K.W.M.; et al. Predictive value of cervical length measurement and fibronectin testing in threatened pre-term labor. Obstet. Gynecol. 2014, 123, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, E.; Akmal, S.; Geerts, L.; Jeffery, B.; Nicolaides, K.H. Sono- graphic measurement of cervical length and fetal fibronectin testing in threatened preterm labor. Ultrasound Obstet. Gynecol. 2006, 27, 368–372. [Google Scholar] [CrossRef] [PubMed]

| Demographic Characteristics at Baseline | Total Women (n = 268) |
|---|---|
| Maternal age (years) | 29.94 ± 5.857 |
| Age < 30 years | 116 (43.3%) |
| Age ≥ 30 years | 152 (56.7%) |
| Place of living | |
| Urban | 92 (34.3%) |
| Rural | 176 (65.7%) |
| Parity | |
| Nulliparous | 76 (28.4%) |
| Multiparous | 192 (71.6%) |
| Gestational age at admission (days) | 269.00 ± 7.397 |
| Gestational age at delivery (days) | 275.81 ± 6.760 |
| Previous deliveries | 192 (71.6%) |
| Vaginal deliveries | 136 (70.8%) |
| Caesarean section | 56 (29.2%) |
| Mode of delivery | |
| Vaginal delivery | 164 (61.2%) |
| Caesarean section | 104 (38.8%) |
| Number of days from admission to delivery | 6.93 ± 3.689 |
| Cervical length at admission (mm) | 31.54 ± 7.334 |
| Delivery within 5 days after admission | 92 (34.3%) |
| Factor | Delivery within 5 Days after Admission | Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 92) | No (n = 176) | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Positive fFN assessment at admission | 60 (65.2%) | 8 (4.5%) | 39,375 | 17,188; 90,202 | 0.000 | 49,879 | 16,896; 147,251 | 0.000 |
| Cervical length at admission (mm) ≤ 26 mm | 40 (43.5%) | 20 (11.4%) | 6.000 | 3.222; 11,173 | 0.000 | 3.343 | 1.199; 9.319 | 0.021 |
| Age > 32.5 | 48 (52.2%) | 32 (18.2%) | 4.909 | 2.803; 8.598 | 0.000 | 5.278 | 2.033; 13.698 | 0.001 |
| Age > 30.0 | 64 (69.6%) | 88 (50.0%) | 2.286 | 1.341; 3.897 | 0.002 | - | - | - |
| Nulliparous | 32 (34.8%) | 44 (25.0%) | - | - | 0.092 | - | - | - |
| Gestational age at admission (days) ≥ 275 | 52 (56.5%) | 16 (9.1%) | 13.000 | 6.727; 25.122 | 0.000 | 27.126 | 9.931; 74.097 | 0.000 |
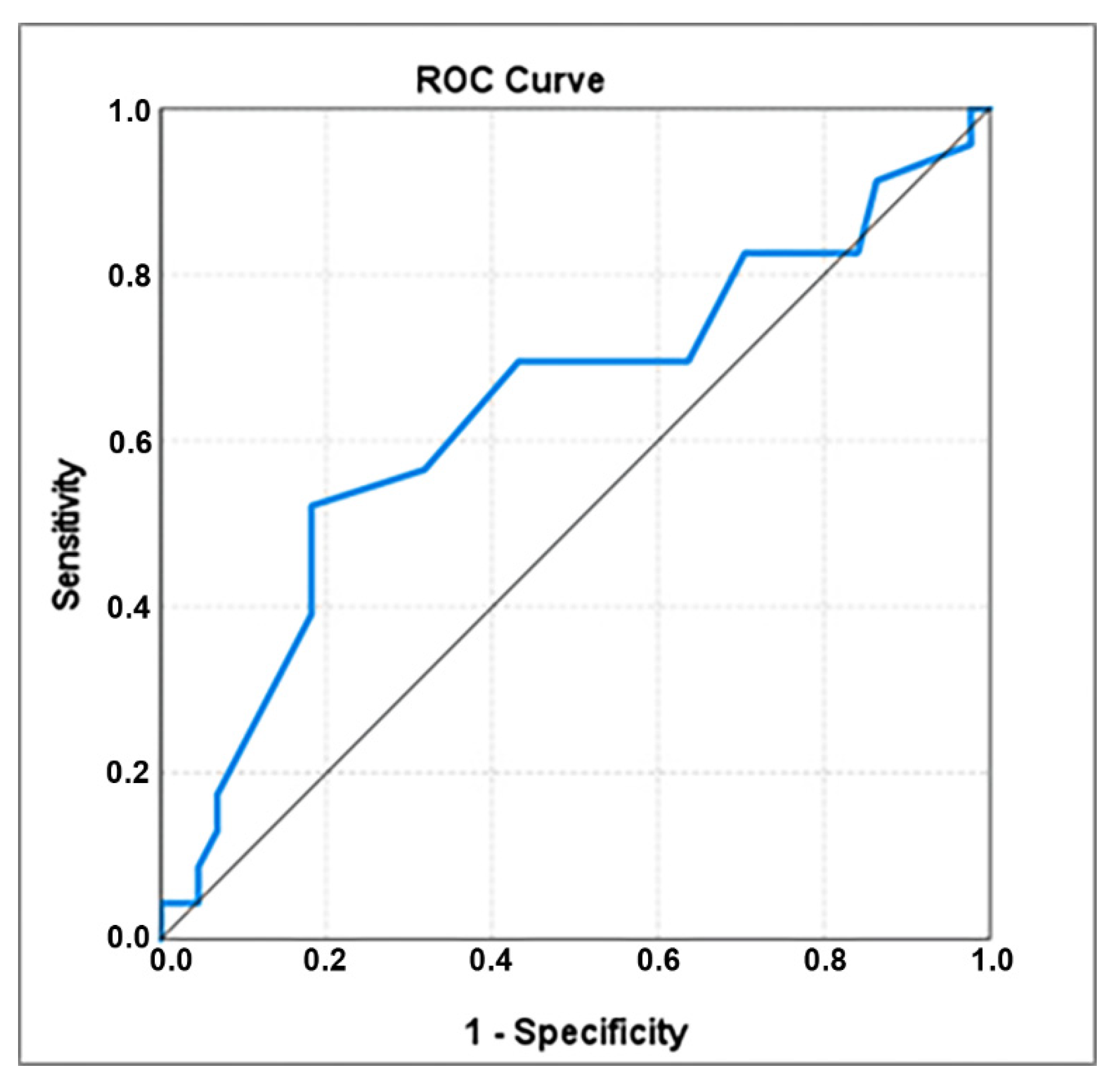
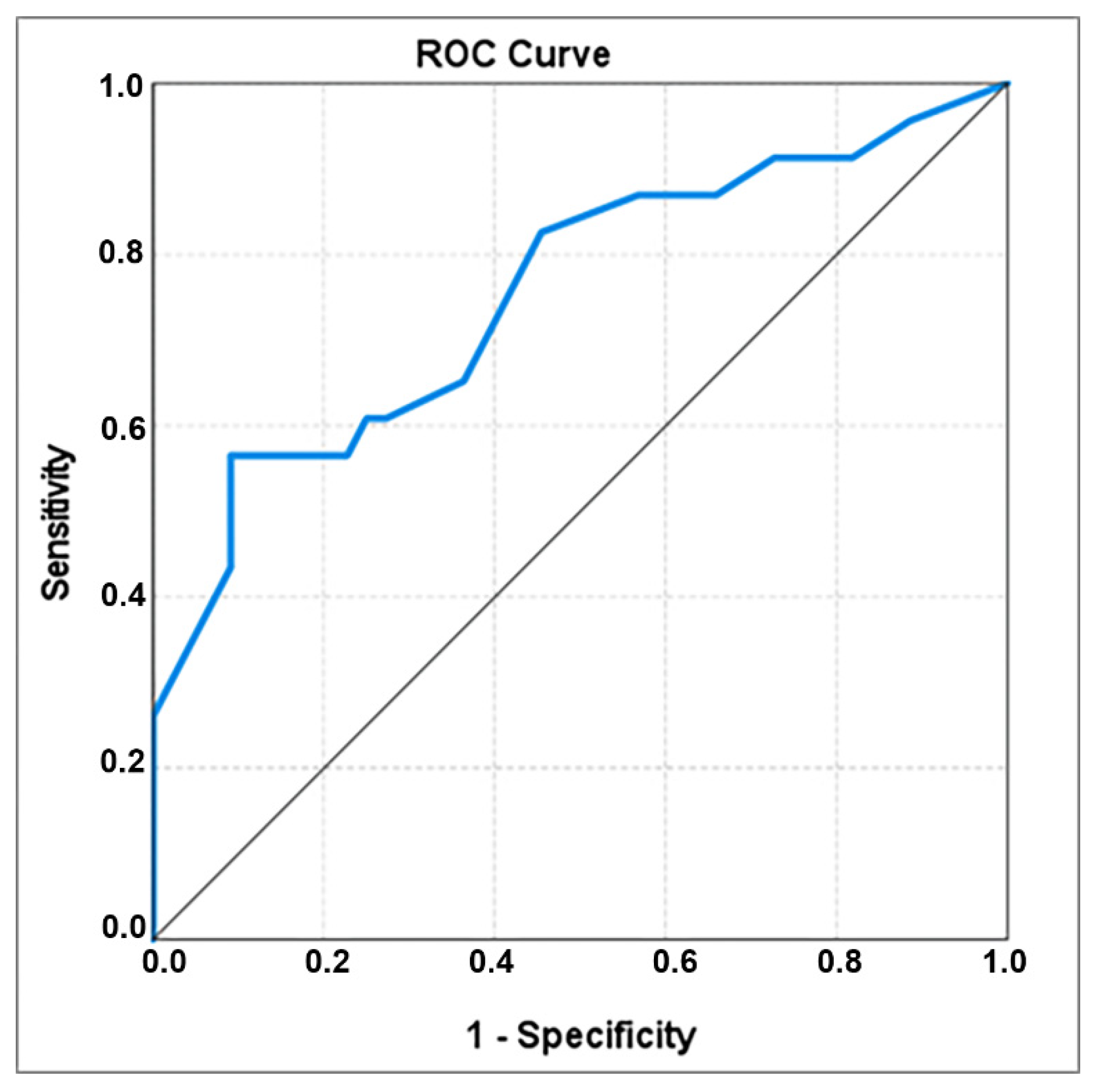
| Factor | Delivery within 5 Days after Admission | p-Value § | Cut-Off Value | Sensibility | Specificity | |
|---|---|---|---|---|---|---|
| Yes (n = 92) | No (n = 176) | |||||
| Cervical length at admission (mm) | 28.83 ± 8.274 | 32.95 ± 6.371 | 0.001 | 26 | 0.435 | 0.886 |
| Age | 31.48 ± 6.247 | 29.14 ± 5.491 | <0.001 | 32.5 | 0.552 | 0.818 |
| Gestational age at admission (days) | 273.52 ± 7.754 | 266.64 ± 5.987 | <0.001 | 274.5 | 0.565 | 0.909 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grab, D.; Doroftei, B.; Grigore, M.; Nicolaiciuc, O.S.; Anton, S.C.; Simionescu, G.; Maftei, R.; Bolota, M.; Ilea, C.; Costachescu, G.; et al. Fetal Fibronectin and Cervical Length as Predictors of Spontaneous Onset of Labour and Delivery in Term Pregnancies. Healthcare 2022, 10, 1349. https://doi.org/10.3390/healthcare10071349
Grab D, Doroftei B, Grigore M, Nicolaiciuc OS, Anton SC, Simionescu G, Maftei R, Bolota M, Ilea C, Costachescu G, et al. Fetal Fibronectin and Cervical Length as Predictors of Spontaneous Onset of Labour and Delivery in Term Pregnancies. Healthcare. 2022; 10(7):1349. https://doi.org/10.3390/healthcare10071349
Chicago/Turabian StyleGrab, Delia, Bogdan Doroftei, Mihaela Grigore, Ovidiu Sebastian Nicolaiciuc, Sorana Caterina Anton, Gabriela Simionescu, Radu Maftei, Maria Bolota, Ciprian Ilea, Gabriel Costachescu, and et al. 2022. "Fetal Fibronectin and Cervical Length as Predictors of Spontaneous Onset of Labour and Delivery in Term Pregnancies" Healthcare 10, no. 7: 1349. https://doi.org/10.3390/healthcare10071349
APA StyleGrab, D., Doroftei, B., Grigore, M., Nicolaiciuc, O. S., Anton, S. C., Simionescu, G., Maftei, R., Bolota, M., Ilea, C., Costachescu, G., & Anton, E. (2022). Fetal Fibronectin and Cervical Length as Predictors of Spontaneous Onset of Labour and Delivery in Term Pregnancies. Healthcare, 10(7), 1349. https://doi.org/10.3390/healthcare10071349







