Prevalence and Risk Factors of Depression between Patients with Parkinson’s Disease and Their Caregivers: A One-Year Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedure
2.3. Statistical Analyses
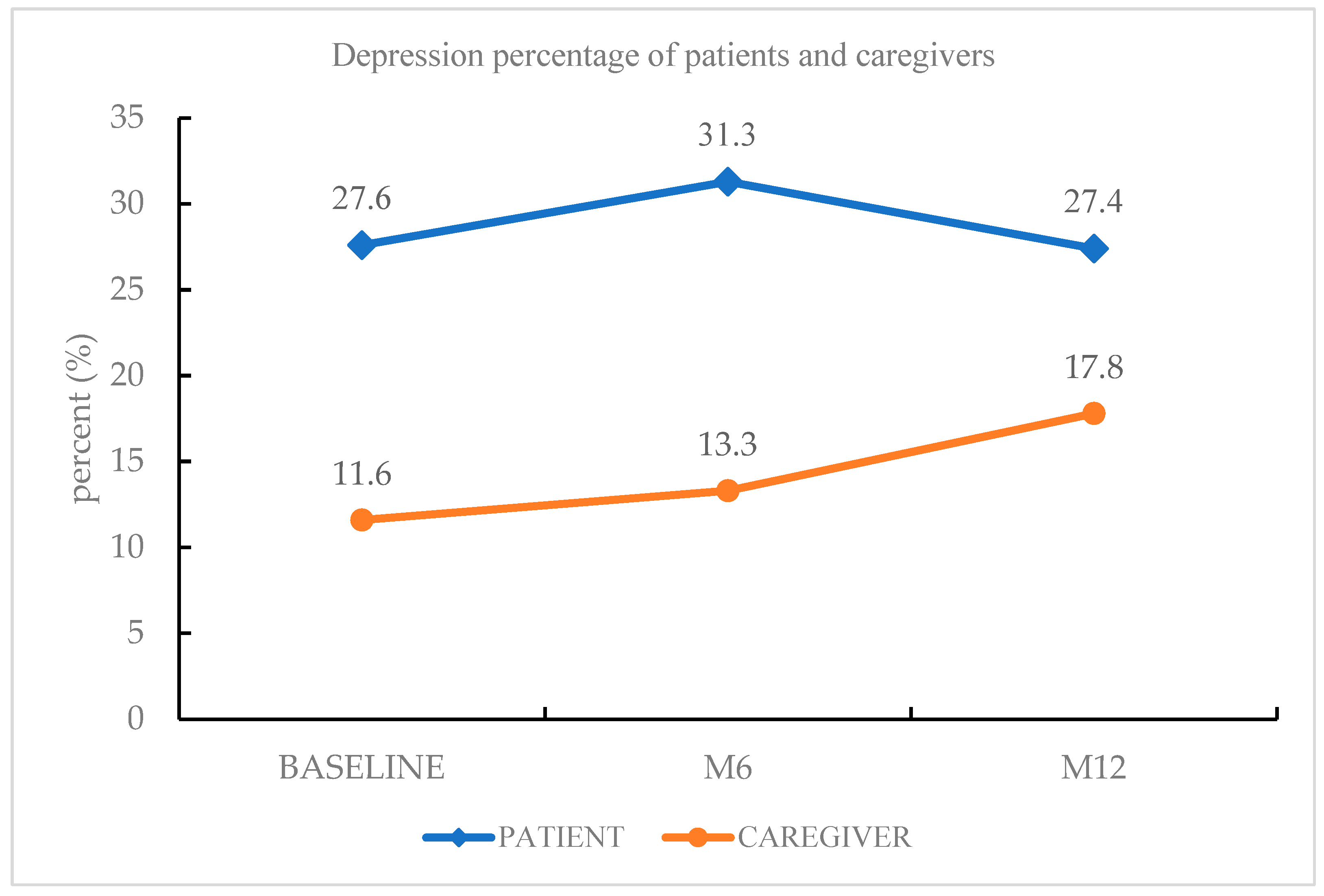
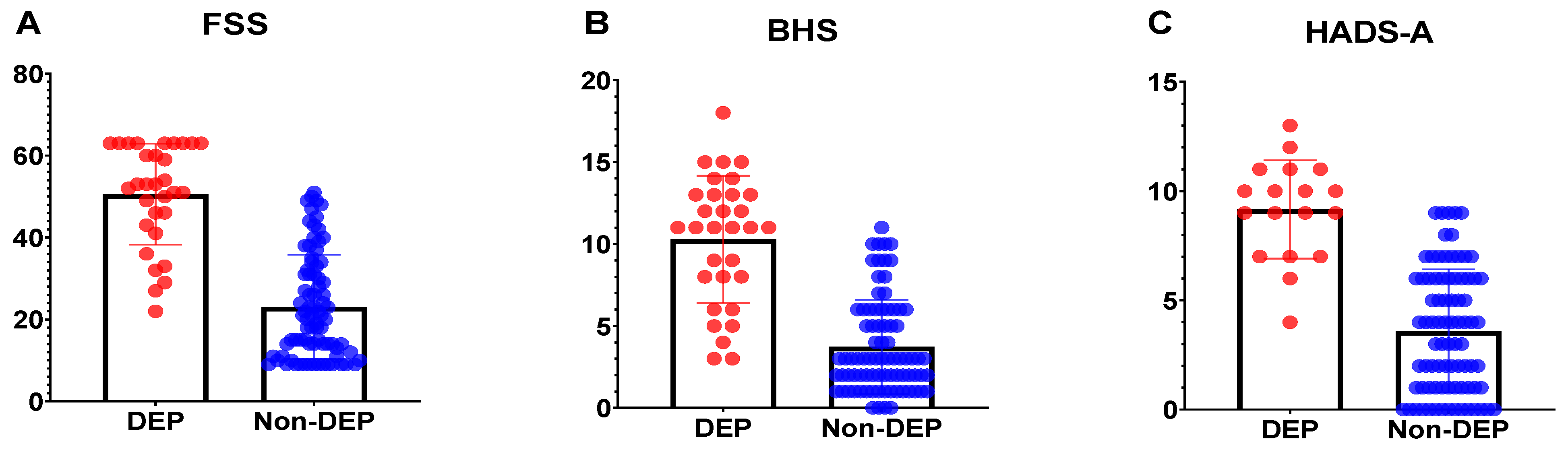
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pringsheim, T.; Jette, N.; Frolkis, A.; Steeves, T.D. The prevalence of Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014, 29, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Müller, B.; Assmus, J.; Herlofson, K.; Larsen, J.P.; Tysnes, O.B. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Relat. Disord. 2013, 19, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Yu, S.; Hu, Y.H.; Li, C.Y.; Artaud, F.; Carcaillon-Bentata, L.; Elbaz, A.; Lee, P.C. Risk of Suicide Among Patients with Parkinson Disease. JAMA Psychiatry 2021, 78, 293–301. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2013. [Google Scholar]
- Liu, Y.; Wang, J. Validity of the Patient Health Questionnaire-9 for DSM-IV major depressive disorder in a sample of Canadian working population. J. Affect. Disord. 2015, 187, 122–126. [Google Scholar] [CrossRef]
- Linden, W.; Vodermaier, A.; MacKenzie, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef]
- Bomasang-Layno, E.; Fadlon, I.; Murray, A.N.; Himelhoch, S. Antidepressive treatments for Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism Relat. Disord. 2015, 21, 833–842; discussion 833. [Google Scholar] [CrossRef] [Green Version]
- Reijnders, J.S.; Ehrt, U.; Weber, W.E.; Aarsland, D.; Leentjens, A.F. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov. Disord. 2008, 23, 183–189. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.-S.; Lin, P.-Y.; Chien, C.-Y.; Fang, F.-M.; Chiu, N.-M.; Hung, C.-F.; Lee, Y.; Chong, M.-Y. Anxiety and depression in patients with head and neck cancer: 6-month follow-up study. Neuropsychiatr. Dis. Treat. 2016, 12, 1029–1036. [Google Scholar] [CrossRef] [Green Version]
- Pontone, G.M.; Bakker, C.C.; Chen, S.; Mari, Z.; Marsh, L.; Rabins, P.V.; Williams, J.R.; Bassett, S.S. The longitudinal impact of depression on disability in Parkinson disease. Int. J. Geriatr. Psychiatry 2016, 31, 458–465. [Google Scholar] [CrossRef]
- Yapici Eser, H.; Bora, H.A.; Kuruoğlu, A. Depression and Parkinson disease: Prevalence, temporal relationship, and determinants. Turk. J. Med. Sci. 2017, 47, 499–503. [Google Scholar] [CrossRef]
- Leentjens, A.F.; Moonen, A.J.; Dujardin, K.; Marsh, L.; Martinez-Martin, P.; Richard, I.H.; Starkstein, S.E.; Köhler, S. Modeling depression in Parkinson disease: Disease-specific and nonspecific risk factors. Neurology 2013, 81, 1036–1043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Becker, C.; Brobert, G.P.; Johansson, S.; Jick, S.S.; Meier, C.R. Risk of incident depression in patients with Parkinson disease in the UK. Eur. J. Neurol. 2011, 18, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Dissanayaka, N.N.; Sellbach, A.; Silburn, P.A.; O’Sullivan, J.D.; Marsh, R.; Mellick, G.D. Factors associated with depression in Parkinson’s disease. J. Affect. Disord. 2011, 132, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Violante, M.; Cervantes-Arriaga, A.; Berlanga-Flores, C.; Ruiz-Chow, A. Prevalence and determinants of depression in Mexican patients with Parkinson’s disease. Clin. Neurol. Neurosurg. 2012, 114, 1293–1296. [Google Scholar] [CrossRef]
- Genç, F.; Yuksel, B.; Tokuc, F.E.U. Caregiver Burden and Quality of Life in Early and Late Stages of Idiopathic Parkinson’s Disease. Psychiatry Investig. 2019, 16, 285–291. [Google Scholar] [CrossRef]
- Carod-Artal, F.J.; Mesquita, H.M.; Ziomkowski, S.; Martinez-Martin, P. Burden and health-related quality of life among caregivers of Brazilian Parkinson’s disease patients. Parkinsonism Relat. Disord. 2013, 19, 943–948. [Google Scholar] [CrossRef]
- Meara, J.; Mitchelmore, E.; Hobson, P. Use of the GDS-15 geriatric depression scale as a screening instrument for depressive symptomatology in patients with Parkinson’s disease and their carers in the community. Age Ageing 1999, 28, 35–38. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.; Chiou, Y.-J.; Hung, C.-F.; Chang, Y.-Y.; Chen, Y.-F.; Lin, T.-K.; Wang, L.-J. Prevalence and Associated Factors of Depressive Disorder in Caregivers of Individuals with Parkinson Disease. J. Geriatr. Psychiatry Neurol. 2020, 34, 418–425. [Google Scholar] [CrossRef]
- Fernandez, H.H.; Tabamo, R.E.; David, R.R.; Friedman, J.H. Predictors of depressive symptoms among spouse caregivers in Parkinson’s disease. Mov. Disord. 2001, 16, 1123–1125. [Google Scholar] [CrossRef]
- Covinsky, K.E.; Newcomer, R.; Fox, P.; Wood, J.; Sands, L.; Dane, K.; Yaffe, K. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. J. Gen. Intern. Med. 2003, 18, 1006–1014. [Google Scholar] [CrossRef] [Green Version]
- Givens, J.L.; Mezzacappa, C.; Heeren, T.; Yaffe, K.; Fredman, L. Depressive symptoms among dementia caregivers: Role of mediating factors. Am. J. Geriatr. Psychiatry 2013, 22, 481–488. [Google Scholar] [CrossRef] [Green Version]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Balker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33; quiz 4–57. [Google Scholar] [PubMed]
- Mendoza, T.R.; Wang, X.S.; Cleeland, C.S.; Morrissey, M.; Johnson, B.A.; Wendt, J.K.; Huber, S.L. The rapid assessment of fatigue severity in cancer patients: Use of the Brief Fatigue Inventory. Cancer 1999, 85, 1186–1196. [Google Scholar] [CrossRef]
- Jensen, M.P. The validity and reliability of pain measures in adults with cancer. J. Pain 2003, 4, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Brugha, T.; Bebbington, P.; Tennant, C.; Hurry, J. The List of Threatening Experiences: A subset of 12 life event categories with considerable long-term contextual threat. Psychol. Med. 1985, 15, 189–194. [Google Scholar] [CrossRef] [Green Version]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The Hopelessness Scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef]
- Rammstedt, B.; John, O.P. Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. J. Res. Pers. 2007, 41, 203–212. [Google Scholar] [CrossRef]
- Lee, Y.; Chiou, Y.J.; Hung, C.F.; Chang, Y.Y.; Chen, Y.F.; Lin, T.K.; Wang, L.J. A dyadic study of psychological well-being of individuals with Parkinson’s disease and their caregivers. Sci. Rep. 2021, 11, 957. [Google Scholar] [CrossRef]
- Saadat, P.; Faramarzi, M.; Salimkhani, F.; Khafri, S. Psychiatric Symptoms in Patients and Caregivers with Parkinson’s Disease. Oman Med. J. 2020, 35, e205. [Google Scholar] [CrossRef] [PubMed]
- First, M.; Spitzer, R.L.; Gibbon, M.L.; Williams, J. Structured clinical interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition; New York State Psychiatric Institute: New York, NY, USA, 2002. [Google Scholar]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Forjaz, M.J. Quality of life and burden in caregivers for patients with Parkinson’s disease: Concepts, assessment and related factors. Rev. Pharm. Outcomes Res. 2012, 12, 221–230. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, G.; Holton, A.R.; Hurren, K.; Watt, L.; Hassanyeh, F. Deliberate self harm-correlates of suicidal intent and severity of depression. Acta Psychiatr. Scand. 1987, 75, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lin, P.-Y.; Lin, M.-C.; Wang, C.-C.; Lu, H.-I.; Chen, Y.-C.; Chong, M.-Y.; Hung, C.-F. Morbidity and associated factors of depressive disorder in patients with lung cancer. Cancer Manag. Res. 2019, 11, 7587–7596. [Google Scholar] [CrossRef] [Green Version]
- Skorvanek, M.; Gdovinova, Z.; Rosenberger, J.; Ghorbani Saeedian, R.; Nagyova, I.; Groothoff, J.W.; Van Dijk, J.P. The associations between fatigue, apathy, and depression in Parkinson’s disease. Acta Neurol. Scand. 2015, 131, 80–87. [Google Scholar] [CrossRef]
- Zimmerman, M.; McDermut, W.; Mattia, J.I. Frequency of anxiety disorders in psychiatric outpatients with major depressive disorder. Am. J. Psychiatry 2000, 157, 1337–1340. [Google Scholar] [CrossRef]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Forjaz, M.J.; Frades-Payo, B.; Agüera-Ortiz, L.; Weintraub, D.; Riesco, A.; Kurtis, M.M.; Chaudhuri, K.R. Neuropsychiatric symptoms and caregiver’s burden in Parkinson’s disease. Parkinsonism Relat. Disord. 2015, 21, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Lageman, S.K.; Donovan, E.K.; Villaseñor, T.; Perrin, P.B. Exploration of Parkinson’s Disease Symptomatology Subtypes from the Caregiver Perspective: Implications for Caregiver Burden, Depression, and Anxiety. J. Geriatr. Psychiatry Neurol. 2021, 8919887211049146. [Google Scholar] [CrossRef]
- Chien, I.C.; Bih, S.H.; Chou, Y.J.; Lin, C.H.; Lee, W.G.; Chou, P. Trends in the use of psychotropic drugs in Taiwan: A population-based national health insurance study, 1997–2004. Psychiatr. Serv. 2007, 58, 554–557. [Google Scholar] [CrossRef]
| Patients | ||||||
|---|---|---|---|---|---|---|
| Depressive N (%), N = 31 | Non-Depressive N (%), N = 82 | Total N (%), N = 113 | z/χ2 | Cohen’s D/Phi | p | |
| Gender (%) | 1.64 | 0.12 | 0.20 | |||
| Male | 18 (58.1) | 58 (70.7) | 76 (67.3) | |||
| Female | 13 (41.9) | 24 (29.6) | 37 (33.0) | |||
| Age, years mean (s.d.) | 64.39 ± 8.47 | 65.79 ± 8.53 | 65.41 ± 8.50 | −0.64 | −0.16 | 0.52 |
| Age of onset | 55.90 ± 9.29 | 57.38 ± 10.95 | 56.97 ± 10.50 | −1.01 | −0.15 | 0.31 |
| Duration of PD | 8.45 ± 5.54 | 8.48 ± 5.49 | 8.47 ± 5.48 | −0.12 | −0.005 | 0.91 |
| Years of education | 11.71 ± 4.64 | 10.66 ± 4.63 | 10.95 ± 4.63 | −1.34 | 0.23 | 0.18 |
| Education | 0.25 | 0.05 | 0.62 | |||
| Less than high school (<12) | 12 (38.7) | 36 (43.9) | 48 (42.5) | |||
| More than college (≥12) | 19 (61.3) | 46 (56.1) | 65 (57.5) | |||
| Marital status | 0.00 | 0.001 | 0.99 | |||
| Unmarried | 3 (9.7) | 8 (9.8) | 11 (9.7) | |||
| Married | 28 (90.3) | 74 (90.2) | 102 (90.3) | |||
| Unemployment | 24 (77.4) | 67 (81.7) | 91 (80.5) | 0.26 | 0.05 | 0.61 |
| Comorbid with other diseases | 18 (58.1) | 55 (67.1) | 73 (64.6) | 0.80 | −0.08 | 0.37 |
| Past psychiatric history | 3.87 | 0.19 | 0.049 | |||
| No psychiatric history | 23 (74.2) | 73 (89.0) | 95 (84.8) | |||
| Depressive disorder | 7 (22.6) | 3 (3.7) | 10 (8.8) | |||
| Anxiety disorder | 1 (3.2) | 3 (3.7) | 4 (3.5) | |||
| Insomnia | 2 (6.5) | 3 (3.7) | 5 (4.4) | |||
| Family psychiatric history | 3.04 | 0.03 | 0.39 | |||
| No psychiatric history | 29 (93.5) | 78 (95.1) | 107 (94.7) | |||
| Depressive disorder | 1 (3.2) | 3 (3.7) | 4 (3.5) | |||
| Anxiety disorder | 1 (3.2) | 1 (1.2) | 2 (1.8) | |||
| Family suicide history | 0 | 4 (4.9) | 4 (3.5) | 1.57 | −0.12 | 0.21 |
| Anxiolytics/Hypnotics use | 8 (25.8) | 24 (29.3) | 32 (28.3) | 0.13 | −0.03 | 0.72 |
| NPRS (range) | 3.68 (0–10) | 1.93 (0–8) | 2.41 (0–10) | −2.73 | 0.63 | 0.006 |
| HADS total scores | 18.81 ± 6.61 | 8.32 ± 4.95 | 11.19 ± 7.18 | −6.59 | 1.80 | <0.001 * |
| HADS-D | 10.16 ± 3.69 | 5.09 ± 3.17 | 6.48 ± 4.01 | −5.96 | 1.47 | <0.001 * |
| HADS-A | 8.65 ± 4.55 | 3.23 ± 2.60 | 4.72 ± 4.04 | −5.80 | 1.46 | <0.001 * |
| BHS | 10.29 ± 3.88 | 3.73 ± 2.87 | 5.53 ± 4.32 | −6.68 | 1.92 | <0.001 * |
| FSS | 50.55 ± 12.34 | 23.11 ± 12.71 | 30.64 ± 17.57 | −7.02 | 2.19 | <0.001 * |
| BFI-10 | ||||||
| Extraversion | 4.19 ± 2.23 | 4.74 ± 2.71 | 4.59 ± 2.59 | −0.78 | −0.22 | 0.44 |
| Agreeableness | 6.32 ± 1.47 | 7.00 ± 1.52 | 6.81 ± 1.53 | −2.03 | −0.45 | 0.042 |
| Conscientiousness | 7.97 ± 1.87 | 8.34 ± 1.96 | 8.24 ± 1.93 | −1.19 | −0.19 | 0.23 |
| Neuroticism | 7.29 ± 1.77 | 5.61 ± 1.75 | 6.07 ± 1.90 | −4.12 | 0.95 | <0.001 * |
| Openness | 7.00 ± 1.34 | 6.80 ± 1.44 | 6.86 ± 1.41 | −0.56 | 0.14 | 0.58 |
| LTEQ | 0.71 (0–3) | 0.34 (0–4) | 0.44 (0–4) | −1.94 | 0.42 | 0.052 |
| ADL scores | 88.55 ± 18.67 | 94.51 ± 15.55 | 92.88 ± 16.59 | −2.27 | −0.35 | 0.023 |
| Highly dependent | 2 (6.5) | 4 (4.9) | 6 (5.3) | |||
| Moderate function | 29 (93.5) | 78 (95.1) | 107 (94.7) | |||
| CDRISC | 19.16 ± 7.52 | 32.51 ± 8.07 | 28.85 ± 9.90 | −6.26 | −1.71 | <0.001 * |
| Caregivers | ||||||
|---|---|---|---|---|---|---|
| Depressive N (%), N = 18 | Non-Depressive N (%), N = 83 | Total N (%), N = 101 | z/χ2 | Cohen’s D/Phi | p | |
| Gender (%) | 0.74 | 0.09 | 0.39 | |||
| Male | 4 (22.2) | 27 (32.5) | 31 (30.7) | |||
| Female | 14 (77.8) | 56 (67.5) | 70 (69.3) | |||
| Age, years mean (s.d.) | 60.44 ± 10.17 | 61.63 ± 10.83 | 61.42 ± 10.67 | −0.67 | −0.11 | 0.50 |
| Duration of caring | 7.89 ± 4.71 | 8.20±5.49 | 8.14 ± 5.34 | −0.09 | −0.06 | 0.93 |
| Years of education | 10.17 ± 4.58 | 11.43 ± 4.58 | 11.20 ± 4.58 | −1.06 | −0.28 | 0.29 |
| Education | 0.05 | −0.02 | 0.83 | |||
| Less than high school (<12) | 7 (38.9) | 30 (36.1) | 37 (36.6) | |||
| More than college (≥12) | 11 (61.1) | 53 (63.9) | 64 (63.4) | |||
| Marital status | 0.46 | 0.07 | 0.50 | |||
| Unmarried | 1 (5.6) | 9 (10.8) | 10 (9.9) | |||
| Married | 17 (94.4) | 74 (89.2) | 91 (90.1) | |||
| Unemployment | 14 (77.8) | 57 (69.9) | 72 (71.3) | 0.45 | −0.07 | 0.50 |
| Comorbid with other diseases | 10 (55.6) | 44 (53.0) | 54 (53.5) | 0.04 | 0.02 | 0.85 |
| Past psychiatric history | 7.85 | 0.28 | 0.005 | |||
| No psychiatric history | 13 (72.2) | 78 (94.0) | 91 (90.1) | |||
| Depressive disorder | 4 (22.2) | 1 (1.2) | 5 (5.0) | |||
| Anxiety disorder | 0 | 1 (1.2) | 1 (1.0) | |||
| Insomnia | 4 (22.2) | 2 (2.4) | 6 (5.9) | |||
| Suicide history | 1 (5.6) | 0 | 1 (1.0) | 4.66 | 0.22 | 0.031 |
| Family psychiatric history | 0.23 | −0.03 | 0.89 | |||
| No psychiatric history | 17 (94.4) | 77 (94.4) | 94 (93.1) | |||
| Depressive disorder | 1 (5.6) | 5 (6.0) | 6 (5.9) | |||
| Anxiety disorder | 0 | 1 (1.2) | 1 (1.0) | |||
| Family suicide history | 0 | 5 (5.0) | 5 (5.0) | 1.14 | −0.11 | 0.29 |
| Anxiolytics/Hypnotics use | 3 (16.7) | 9 (10.8) | 12 (11.9) | 0.48 | 0.07 | 0.49 |
| NPRS (range) | 2.33 (0–7) | 1.19 (0–10) | 1.40 (0–10) | −2.38 | 0.52 | 0.017 |
| HADS total scores | 19.00 ± 4.97 | 7.46 ± 4.96 | 9.51 ± 6.64 | −5.92 | 2.32 | <0.001 * |
| HADS-D | 9.83 ± 2.96 | 3.86 ± 2.88 | 4.92 ± 3.68 | −5.65 | 2.04 | <0.001 * |
| HADS-A | 9.17 ± 2.26 | 3.60 ± 2.82 | 4.59 ± 3.46 | −5.77 | 2.18 | <0.001 * |
| BHS | 7.61 ± 4.59 | 2.60 ± 2.56 | 3.50 ± 3.58 | −4.42 | 1.35 | <0.001 * |
| FSS | 32.39 ± 12.94 | 18.90 ± 8.70 | 21.31 ± 10.83 | −4.14 | 1.22 | <0.001 * |
| BFI-10 | ||||||
| Extraversion | 6.00 ± 2.70 | 5.81 ± 2.41 | 5.84 ± 2.45 | −0.27 | 0.07 | 0.79 |
| Agreeableness | 6.17 ± 1.30 | 6.65 ± 1.56 | 6.56 ± 1.52 | −1.34 | −0.33 | 0.18 |
| Conscientiousness | 8.28 ± 1.36 | 8.16 ± 1.81 | 8.18 ± 1.73 | −0.17 | 0.07 | 0.88 |
| Neuroticism | 6.17 ± 1.58 | 4.90 ± 1.58 | 5.13 ± 1.65 | −2.54 | 0.80 | 0.011 |
| Openness | 6.39 ± 1.09 | 6.42 ± 1.42 | 6.42 ± 1.37 | −0.04 | −0.02 | 0.97 |
| LTEQ | 1.83 (0–3) | 0.37 (0–15) | 0.63 (0–15) | −2.58 | 0.57 | 0.01 |
| CDRISC | 24.06 ± 8.08 | 32.23 ± 7.20 | 30.77 ± 7.97 | −3.78 | −1.07 | <0.001 * |
| Item | β | S.E. | Wald | Odds Ratio | C.I. | p |
|---|---|---|---|---|---|---|
| FSS | 0.09 | 0.03 | 7.98 | 1.09 | 1.03–1.16 | 0.005 * |
| BHS | 0.36 | 0.11 | 9.95 | 1.43 | 1.15–1.79 | 0.002 * |
| Item | β | S.E. | Wald | Odds Ratio | C.I. | p |
|---|---|---|---|---|---|---|
| BHS | 0.23 | 0.14 | 2.68 | 1.25 | 0.96–1.64 | 0.101 |
| CDRISC | 0.04 | 0.06 | 0.39 | 1.04 | 0.92–1.17 | 0.532 |
| FSS | 0.07 | 0.04 | 2.55 | 1.07 | 0.99–1.16 | 0.111 |
| HADS-A | 0.55 | 0.25 | 4.75 | 1.73 | 1.26–2.82 | 0.029 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.; Chang, Y.-Y.; Chen, Y.-F.; Lin, T.-K.; Hung, C.-F.; Chiou, Y.-J.; Wang, L.-J. Prevalence and Risk Factors of Depression between Patients with Parkinson’s Disease and Their Caregivers: A One-Year Prospective Study. Healthcare 2022, 10, 1305. https://doi.org/10.3390/healthcare10071305
Lee Y, Chang Y-Y, Chen Y-F, Lin T-K, Hung C-F, Chiou Y-J, Wang L-J. Prevalence and Risk Factors of Depression between Patients with Parkinson’s Disease and Their Caregivers: A One-Year Prospective Study. Healthcare. 2022; 10(7):1305. https://doi.org/10.3390/healthcare10071305
Chicago/Turabian StyleLee, Yu, Yung-Yee Chang, Ying-Fa Chen, Tsu-Kung Lin, Chi-Fa Hung, Yu-Jie Chiou, and Liang-Jen Wang. 2022. "Prevalence and Risk Factors of Depression between Patients with Parkinson’s Disease and Their Caregivers: A One-Year Prospective Study" Healthcare 10, no. 7: 1305. https://doi.org/10.3390/healthcare10071305
APA StyleLee, Y., Chang, Y.-Y., Chen, Y.-F., Lin, T.-K., Hung, C.-F., Chiou, Y.-J., & Wang, L.-J. (2022). Prevalence and Risk Factors of Depression between Patients with Parkinson’s Disease and Their Caregivers: A One-Year Prospective Study. Healthcare, 10(7), 1305. https://doi.org/10.3390/healthcare10071305







