Healthcare Avoidance before and during the COVID-19 Pandemic among Australian Youth: A Longitudinal Study
Abstract
:1. Introduction
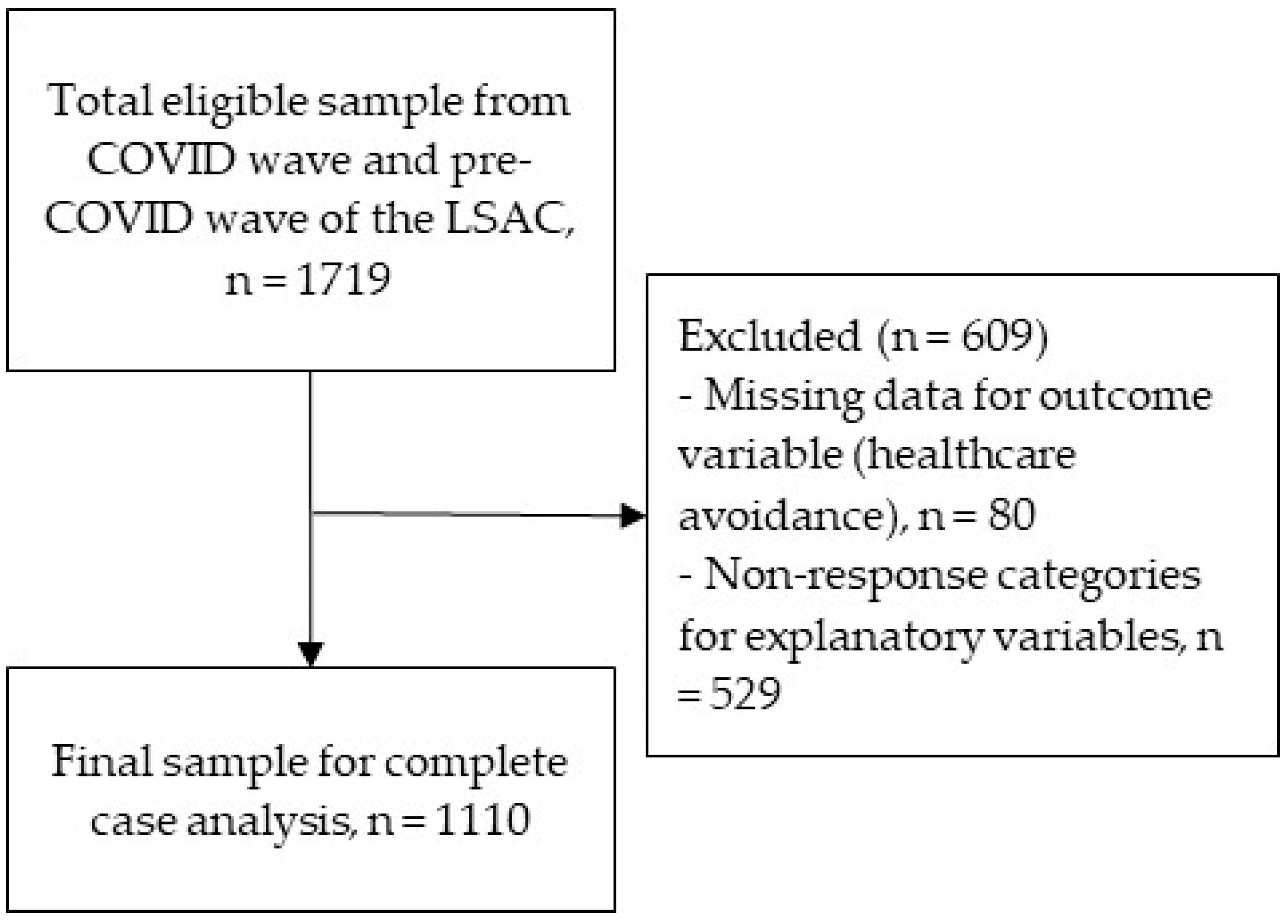
2. Methods
2.1. Data Source
2.2. Measures
2.3. Statistical Analysis
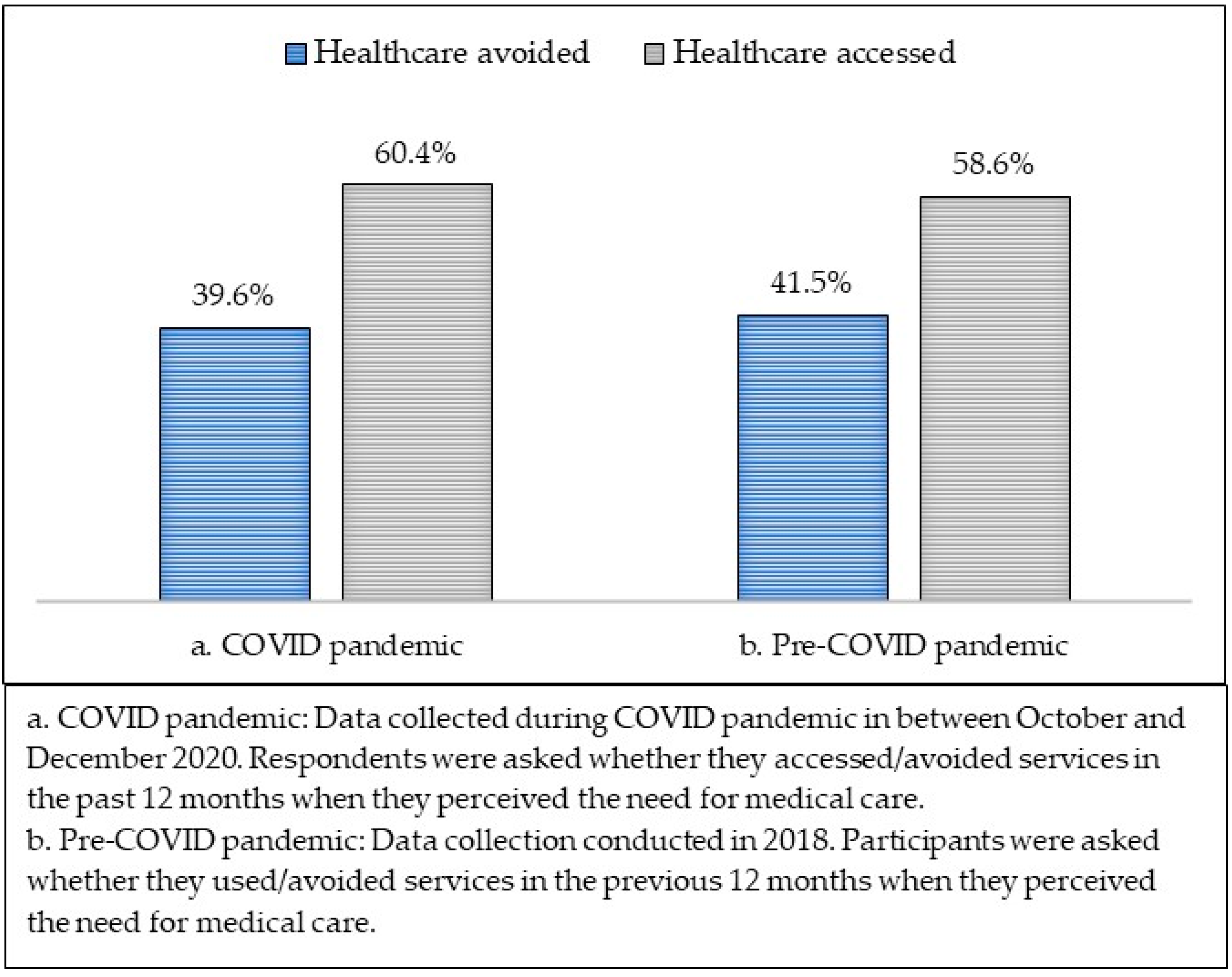
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Organization for Economic Cooperation and Development. Health at a Glance: Europe 2020: State of Health in the EU Cycle; Organisation for Economic Co-operation and Development OECD: Paris, France, 2020. [Google Scholar]
- World Health Organization. Health at a Glance: Asia/Pacific 2020 Measuring Progress towards Universal Health Coverage: Measuring Progress towards Universal Health Coverage; OECD Publishing: Paris, France, 2020. [Google Scholar]
- Zhang, H.; Guo, L.-W.; Gao, Y.-Y.; Yao, H.; Xie, Z.-K.; Zhang, W.-X. The impact of the COVID-19 pandemic on pediatric clinical practice in Wenzhou, China: A retrospective study. Front. Pediatr. 2020, 8, 585629. [Google Scholar] [CrossRef] [PubMed]
- Keyes, D.; Hardin, B.; Sweeney, B.; Shedden, K. Change in urban and non-urban pattern of ED use during the COVID-19 pandemic in 28 Michigan hospitals: An observational study. BMJ Open 2021, 11, e043024. [Google Scholar] [CrossRef] [PubMed]
- Dopfer, C.; Wetzke, M.; Zychlinsky Scharff, A.; Mueller, F.; Dressler, F.; Baumann, U.; Sasse, M.; Hansen, G.; Jablonka, A.; Happle, C. COVID-19 related reduction in pediatric emergency healthcare utilization—A concerning trend. BMC Pediatr. 2020, 20, 427. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.; Woolfenden, S.; Pengilly, S.; Breen, C.; Cohn, R.; Biviano, L.; Johns, A.; Worth, A.; Lamb, R.; Lingam, R.; et al. COVID-19 pandemic: The impact on vulnerable children and young people in Australia. J. Pediatr. Child Health 2020, 56, 1851–1855. [Google Scholar] [CrossRef]
- Núñez, A.; Sreeganga, S.D.; Ramaprasad, A. Access to Healthcare during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2980. [Google Scholar] [CrossRef]
- Sifris, R.; Penovic, T. Barriers to abortion access in Australia before and during the COVID-19 pandemic. In Women’s Studies International Forum; Pergamon: Oxford, UK, 2021; p. 102470. [Google Scholar]
- Fisk, M.; Livingstone, A.; Pit, S.W. Telehealth in the context of COVID-19: Changing perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 2020, 22, e19264. [Google Scholar] [CrossRef]
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Soares, P.; Leite, A.; Esteves, S.; Gama, A.; Laires, P.A.; Moniz, M.; Pedro, A.R.; Santos, C.M.; Goes, A.R.; Nunes, C. Factors Associated with the Patient’s Decision to Avoid Healthcare during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 13239. [Google Scholar] [CrossRef]
- Byrne, S.K. Healthcare avoidance: A critical review. Holist. Nurs. Pract. 2008, 22, 280–292. [Google Scholar] [CrossRef]
- Lee, M.; You, M. Avoidance of healthcare utilization in South Korea during the coronavirus disease 2019 (COVID-19) pandemic. Int. J. Environ. Res. Public Health 2021, 18, 4363. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Kennedy, J.L.; Wiley, J.F.; Facer-Childs, E.R.; Robbins, R.; Barger, L.K.; Czeisler, C.A.; Rajaratnam, S.M.; Howard, M.E. Delay or avoidance of routine, urgent and emergency medical care due to concerns about COVID-19 in a region with low COVID-19 prevalence: Victoria, Australia. Respirology 2021, 26, 707. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Marynak, K.; Clarke, K.E.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1250. [Google Scholar] [CrossRef] [PubMed]
- Solanke, F.; Easton, S.; Selby, A.; James, D.; Roberts, G. Impact of COVID-19 pandemic on emergency department attendances for young people. Arch. Dis. Child. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Collyer, T.A.; Athanasopoulos, G.; Srikanth, V.; Tiruvoipati, R.; Matthews, C.; McInnes, N.; Menon, S.; Dowling, J.; Braun, G.; Krivitsky, T.A.; et al. Impact of COVID-19 lockdowns on hospital presentations and admissions in the context of low community transmission: Evidence from time series analysis in Melbourne, Australia. J. Epidemiol. Community Health 2021, 76, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Nassar, N.; Shrapnel, J.; Perkes, I.; Hodgins, M.; O’Leary, F.; Trudgett, C.; Eapen, V.; Woolfenden, S.; Knight, K. The impact of the COVID-19 pandemic on paediatric health service use within one year after the first pandemic outbreak in New South Wales Australia—A time series analysis. Lancet Reg. Health-West. Pac. 2021, 19, 100311. [Google Scholar] [CrossRef] [PubMed]
- Donato, R.; Scotton, R. The Australian Health Care System; Routledge: Abingdon-on-Thames, UK, 2020. [Google Scholar]
- Malik, A.; Lenzen, M.; McAlister, S.; McGain, F. The carbon footprint of Australian health care. Lancet Planet. Health 2018, 2, e27–e35. [Google Scholar] [CrossRef] [Green Version]
- Australian Government Department of Health. Coronavirus (COVID-19) Case Numbers and Statistics. Available online: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-case-numbers-and-statistics (accessed on 7 March 2022).
- Tiller, E.; Fildes, J.; Hall, S. Mission Australia Youth Survey Report 2020; Mission Australia: Sydney, Australia, 2020. [Google Scholar]
- Australian Institute of Health Welfare. COVID-19 and the Impact on Young People. Available online: https://www.aihw.gov.au/reports/children-youth/covid-19-and-young-people (accessed on 7 March 2022).
- Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings. Available online: https://www.abs.gov.au/statistics/health/health-services/patient-experiences-australia-summary-findings/latest-release (accessed on 7 March 2022).
- Blakemore, S.-J.; Mills, K.L. Is adolescence a sensitive period for sociocultural processing? Annu. Rev. Psychol. 2014, 65, 187–207. [Google Scholar] [CrossRef] [PubMed]
- Australian Health Ministers’ Advisory Council. National Strategic Framework for Chronic Conditions; Australian Government: Canberra, Australia, 2017. [Google Scholar]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. Am. J. Transplant. 2020, 20, 2612–2617. [Google Scholar] [CrossRef]
- Jenner, R.; Walker, A.; Isba, R. Kids are back in town: The return of high demand for paediatric emergency care. Arch. Dis. Child. 2022, 107, 204–205. [Google Scholar] [CrossRef]
- AIHW. The First Year of COVID-19 in Australia: Direct and Indirect Health Effects; AIHW: Canberra, Australia, 2021. [Google Scholar]
- Jessup, R.L.; Bramston, C.; Beauchamp, A.; Gust, A.; Cvetanovska, N.; Cao, Y.; Haywood, C.; Conilione, P.; Tacey, M.; Copnell, B. Impact of COVID-19 on emergency department attendance in an Australia hospital: A parallel convergent mixed methods study. BMJ Open 2021, 11, e049222. [Google Scholar] [CrossRef]
- Li, S.H.; Beames, J.R.; Newby, J.M.; Maston, K.; Christensen, H.; Werner-Seidler, A. The impact of COVID-19 on the lives and mental health of Australian adolescents. Eur. Child Adolesc. Psychiatry 2021, 1–13. [Google Scholar] [CrossRef]
- Alvarez, E.; Lavis, J.N.; Brouwers, M.; Schwartz, L. Developing a workbook to support the contextualisation of global health systems guidance: A case study identifying steps and critical factors for success in this process at WHO. Health Res. Policy Syst. 2018, 16, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobs, B.; Ir, P.; Bigdeli, M.; Annear, P.L.; Van Damme, W. Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012, 27, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Uneke, C.J.; Langlois, E.V.; Uro-Chukwu, H.C.; Chukwu, J.; Ghaffar, A. Fostering access to and use of contextualised knowledge to support health policy-making: Lessons from the Policy Information Platform in Nigeria. Health Res. Policy Syst. 2019, 17, 38. [Google Scholar] [CrossRef]
- Bekele, B.B.; Alhaffar, B.A.; Wasnik, R.N.; Sándor, J. The Effect of the COVID-19 Pandemic on the Social Inequalities of Health Care Use in Hungary: A Nationally Representative Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2258. [Google Scholar] [CrossRef]
- Burch, A.E. Factors responsible for healthcare avoidance among rural adults in the Eastern Region of North Carolina. J. Community Health 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Splinter, M.J.; Velek, P.; Ikram, M.K.; Kieboom, B.C.; Peeters, R.P.; Bindels, P.J.; Ikram, M.A.; Wolters, F.J.; Leening, M.J.; de Schepper, E.I. Prevalence and determinants of healthcare avoidance during the COVID-19 pandemic: A population-based cross-sectional study. PLoS Med. 2021, 18, e1003854. [Google Scholar] [CrossRef] [PubMed]
- Mohal, J.; Lansangan, C.; Gasser, C.; Taylor, T.; Renda, J.; Jessup, K.; Daraganova, G. Growing Up in Australia: The Longitudinal Study of Australian Children—Data User Guide, Release 9C1; Australian Institute of Family Studies: Melbourne, Australia, 2021. [Google Scholar]
- Soloff, C.; Lawrence, D.; Johnstone, R. Sample Design; Australian Institute of Family Studies: Melbourne, Australia, 2005. [Google Scholar]
- Burnett, A.J.; Lamb, K.E.; Spence, A.C.; Lacy, K.E.; Worsley, A. Parenting style as a predictor of dietary score change in children from 4 to 14 years of age. Findings from the Longitudinal Study of Australian Children. Public Health Nutr. 2021, 24, 6058–6066. [Google Scholar] [CrossRef]
- Zhuchkova, S.; Rotmistrov, A. How to choose an approach to handling missing categorical data:(un) expected findings from a simulated statistical experiment. Qual. Quant. 2021, 56, 1–22. [Google Scholar] [CrossRef]
- Hughes, R.A.; Heron, J.; Sterne, J.A.; Tilling, K. Accounting for missing data in statistical analyses: Multiple imputation is not always the answer. Int. J. Epidemiol. 2019, 48, 1294–1304. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Codony, M.; Alonso, J.; Almansa, J.; Bernert, S.; De Girolamo, G.; De Graaf, R.; Haro, J.M.; Kovess, V.; Vilagut, G.; Kessler, R.C. Perceived need for mental health care and service use among adults in Western Europe: Results of the ESEMeD project. Psychiatr. Serv. 2009, 60, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Mojtabai, R.; Olfson, M.; Mechanic, D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch. Gen. Psychiatry 2002, 59, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.E.; Lawrence, D.; Hafekost, J.; Saw, S.; Buckingham, W.J.; Sawyer, M.; Ainley, J.; Zubrick, S.R. Service use by Australian children for emotional and behavioural problems: Findings from the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Aust. N. Z. J. Psychiatry 2016, 50, 887–898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, S.E.; Lawrence, D.; Sawyer, M.; Zubrick, S.R. Mental disorders in Australian 4- to 17-year olds: Parent-reported need for help. Aust. N. Z. J. Psychiatry 2018, 52, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Vu, X.-B.B.; Biswas, R.K.; Khanam, R.; Rahman, M. Mental health service use in Australia: The role of family structure and socio-economic status. Child. Youth Serv. Rev. 2018, 93, 378–389. [Google Scholar] [CrossRef] [Green Version]
- Stobart, A.; Duckett, S. Australia’s Response to COVID-19. Health Econ. Policy Law 2022, 17, 95–106. [Google Scholar] [CrossRef]
- Siette, J.; Seaman, K.; Dodds, L.; Ludlow, K.; Johnco, C.; Wuthrich, V.; Earl, J.K.; Dawes, P.; Strutt, P.; Westbrook, J.I. A national survey on COVID-19 second-wave lockdowns on older adults’ mental wellbeing, health-seeking behaviours and social outcomes across Australia. BMC Geriatr. 2021, 21, 400. [Google Scholar] [CrossRef]
- O’Sullivan, D.; Rahamathulla, M.; Pawar, M. The impact and implications of COVID-19: An Australian perspective. Int. J. Community Soc. Dev. 2020, 2, 134–151. [Google Scholar] [CrossRef]
- Gilkey, M.B.; Kong, W.Y.; Huang, Q.; Grabert, B.K.; Thompson, P.; Brewer, N.T. Using Telehealth to Deliver Primary Care to Adolescents during and after the COVID-19 Pandemic: National Survey Study of US Primary Care Professionals. J. Med. Internet Res. 2021, 23, e31240. [Google Scholar] [CrossRef]
- Reitzle, L.; Schmidt, C.; Färber, F.; Huebl, L.; Wieler, L.H.; Ziese, T.; Heidemann, C. Perceived access to health care services and relevance of telemedicine during the COVID-19 pandemic in Germany. Int. J. Environ. Res. Public Health 2021, 18, 7661. [Google Scholar] [CrossRef]
- Saunders, N.; Guttmann, A.; Brownell, M.; Cohen, E.; Fu, L.; Guan, J.; Sarkar, J.; Mahar, A.; Gandhi, S.; Fiksenbaum, L. Pediatric primary care in Ontario and Manitoba after the onset of the COVID-19 pandemic: A population-based study. Can. Med. Assoc. Open Access J. 2021, 9, E1149–E1158. [Google Scholar] [CrossRef] [PubMed]
- Ganson, K.T.; Weiser, S.D.; Tsai, A.C.; Nagata, J.M. Associations between anxiety and depression symptoms and medical care avoidance during COVID-19. J. Gen. Intern. Med. 2020, 35, 3406–3408. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A.; Braunack-Mayer, A.; Wittert, G. What do we know about men’s help-seeking and health service use? Med. J. Aust. 2006, 184, 81–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santomauro, D.F.; Herrera, A.M.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Frederiksen, B.; Ranji, U.; Salganicoff, A.; Long, M. Women’s Experiences with Health Care during the COVID-19 Pandemic: Findings from the KFF Women’s Health Survey; Kaiser Family Foundation: San Francisco, CA, USA, 2021. [Google Scholar]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. The COVID-19 response must be disability inclusive. Lancet Public Health 2020, 5, e257. [Google Scholar] [CrossRef] [Green Version]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef] [Green Version]
- Radez, J.; Reardon, T.; Creswell, C.; Lawrence, P.J.; Evdoka-Burton, G.; Waite, P. Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. Eur. Child Adolesc. Psychiatry 2021, 30, 183–211. [Google Scholar] [CrossRef] [Green Version]
- Van Dyke, N. Young People’s Experiences with Health Services; Commissioner for Children and Young People: Perth, WA, USA, 2013. [Google Scholar]
- Australian Bureau of Statistics. Migration, Australia; Australian Bureau of Statistics: Canberra, Australia, 2021. [Google Scholar]
- AIHW. Rural & Remote Health; Australian Institute of Health and Welfare; Australian Government: Canberra, Australia, 2020.
| Variables | Description |
|---|---|
| Outcome variable | |
| Avoidance of healthcare | The main outcome variable of the study was avoidance of healthcare among those who perceived the need, assessed by asking the cohort “In the last 12 months, has there been any time when you thought you should get medical care, but you didn’t?”. The response categories were ‘Yes’ (coded as 1) and ‘No’ (coded as 0). This is to note that the question was not very sensitive as the LSAC database did not allow us to ascertain how hard or how many times the respondents tried to get access, or how many times they failed to obtain access to services; instead, it provided the list of causes for avoiding the services when the respondents perceived the need. |
| Exposure variables | |
| Age | Considered as a continuous variable |
| Sex | Dichotomized into two categories: ‘Male’ (coded as 0) and ‘Female’ (coded as 1) |
| Country of birth | Classified as ‘Overseas’ (coded as 0) and ‘Australian’ (coded as 1) |
| Residential state | Categorized into four: ‘Others’ (coded as 0), ‘New South Wales’ (coded as 1), ‘Victoria’ (coded as 2), and ‘Queensland’ (coded as 3). |
| Remoteness | According to the Australian Bureau of Statistics (ABS) from the Census of Population and Housing 2016, remoteness areas divide Australia into 5 categories of remoteness based on the relative availability of services—major cities, inner regional, outer regional, remote, and very remote. In this study, we created a binary variable ‘Remoteness’ from the responses. ‘Major cities’ were coded as ‘1′, while ‘inner regional’, ‘outer regional’, ‘remote’, and ‘very remote’ were combined to classify as ‘regional/remote’ (coded as 0). |
| Education | The education of the participants was dichotomized into two categories: ‘Technical/Others’ (coded as 0) and ‘University/Tertiary’ (coded as 1) |
| Employment | The employment status of the respondents was dichotomized into two categories: ‘Unemployed’ (coded as 0) and ‘Employed’ (coded as 1). |
| Living with parents | Dichotomized into two categories: ‘No’ (coded as 0) and ‘Yes’ (coded as 1). |
| Family cohesion | Cohesion is the ability of family members to get along with each other. Categorized into two: ‘Poor’ (coded as 0) and ‘Strong’ (coded as 1). |
| Ongoing medical conditions | Whether the participant has any of the following ongoing medical conditions: eczema, hay fever, allergies, musculoskeletal problems, ADHD, anxiety, depression, autism, diabetes, asthma, palpitations, congenital heart disease, seizures/epilepsy, wheezing, chronic fatigue, or Disability. The response categories for each condition were ‘Yes/No’. From the responses for each of the categories, we created a new binary variable, termed ‘Any medical conditions’ and coded 1 for ‘Yes’ and 0 for ‘No’. |
| Psychological distress | Psychological distress was measured using the Kessler Psychological Distress Scale (K10) and categorized based on the K10 scale summed score. For analytical purposes, psychological distress was categorized into three levels: ‘low’ (coded as 0), ‘moderate’ (coded as 1), and ‘high’ (coded as 2) |
| COVID-19 tested | Whether the respondent tested for COVID-19 or not. The response categories were ‘Yes’ (coded as 1) and ‘No’ (coded as 0). Note that only the Polymerase chain reaction (PCR) testing method was used by the Australian Government until November 2021. |
| Physical activity during lockdown * | Whether the study participant performed physical activities during the coronavirus restriction period or not. Responses were ‘Yes’ (coded as 1) and ‘No’ (coded as 0). |
| Employment status in lockdown | The employment status of the respondents during lockdown was dichotomized into two categories: ‘Yes’ (coded as 1) and ‘No’ (coded as 0). |
| Coronavirus supplement during lockdown | Whether the respondent received any financial support (e.g., Youth Allowance, JobSeeker, or JobKeeper) from the Australian Government during the 1st lockdown due to the COVID-19 pandemic in Australia. Responses were ‘Yes’ (coded as 1) and ‘No’ (coded as 0). |
| The difficulty of life in lockdown | Addressing the question: How difficult was life during COVID-19 restrictions? Responses included from no problems/stresses to many problems/stresses. The responses were ‘less/no’ (coded as 0) and ‘few/many’ (coded as 1). |
| n | % | |
|---|---|---|
| Age 1 | Mean = 20.63, SD = ±0.49 | |
| Sex | ||
| Male | 459 | 41.4 |
| Female | 651 | 58.6 |
| Country of birth | ||
| Overseas | 56 | 5.0 |
| Australia | 1054 | 95.0 |
| Residential state | ||
| Others | 286 | 25.8 |
| NSW | 319 | 28.7 |
| VIC | 298 | 26.8 |
| QLD | 207 | 18.7 |
| Remoteness | ||
| Major cities | 849 | 76.5 |
| Regional/Remote | 261 | 23.5 |
| Education | ||
| Technical/Others | 405 | 36.5 |
| University/Tertiary | 705 | 63.5 |
| Employment | ||
| Unemployed | 248 | 22.3 |
| Employed | 862 | 77.7 |
| Living with parents | ||
| No | 316 | 28.5 |
| Yes | 794 | 71.5 |
| Family cohesion | ||
| Poor | 173 | 15.6 |
| Strong | 937 | 84.4 |
| IRSAD Quintiles | ||
| Q1 (0–20%)—Most disadvantaged | 288 | 26.0 |
| Q2 (20–40%) | 203 | 18.3 |
| Q3 (40–60%) | 268 | 24.1 |
| Q4 (60–80%) | 179 | 16.1 |
| Q5 (80–100%)—Most advantaged | 172 | 15.5 |
| Ongoing medical conditions | ||
| No | 422 | 38.0 |
| Yes | 688 | 62.0 |
| Psychological distress | ||
| Low | 344 | 31.0 |
| Moderate | 308 | 27.7 |
| High | 458 | 41.3 |
| Reasons * | COVID-19 Pandemic (n = 440) | Pre-COVID-19 Pandemic (n = 460) | |||
|---|---|---|---|---|---|
| n (%) | p-Value *** | n (%) | p-Value *** | ||
| 1 | Did not know who to go and see | 71 (16.1) | <0.001 | 47 (10.2) | <0.001 |
| 2 | Had no transportation | 18 (4.1) | <0.001 | 11 (2.4) | 0.088 |
| 3 | No one available to go along with | 16 (3.6) | <0.001 | 11 (2.4) | 0.026 |
| 4 | Difficult to make an appointment | 78 (17.7) | <0.001 | 51 (11.1) | <0.001 |
| 5 | Afraid of what doctors would say or do | 116 (26.4) | <0.001 | 84 (18.3) | <0.001 |
| 6 | Thought the problem would go away | 246 (55.9) | <0.001 | 164 (35.7) | <0.001 |
| 7 | Could not pay | 65 (14.8) | <0.001 | 47 (10.2) | <0.001 |
| 8 | The problem went away | 120 (27.3) | <0.001 | 82 (17.8) | <0.001 |
| 9 | Too embarrassed | 84 (19.1) | <0.001 | 59 (12.8) | <0.001 |
| 10 | Felt I would be discriminated against | 10 (2.3) | <0.001 | 8 (1.7) | 0.013 |
| 11 | Did not think they could help me | 78 (17.7) | <0.001 | 53 (11.5) | <0.001 |
| 12 | Services not available in my area | 14 (3.2) | <0.001 | 9 (2.0) | 0.081 |
| 13 | Others | 65 (14.8) | <0.001 | 44 (9.6) | <0.001 |
| During COVID-19 lockdown ** | <0.001 | ||||
| 14 | I did not want to visit the doctor during the coronavirus restriction period | 96 (21.8) | <0.001 | - | - |
| 15 | My doctor did not perform non-emergency appointments during the coronavirus restriction period | 15 (3.4) | <0.001 | - | - |
| 16 | Appointment cancelled or deferred indefinitely because of the coronavirus restriction period | 8 (1.8) | <0.001 | - | - |
| 17 | Isolating due to the coronavirus restrictions | 12 (2.7) | <0.001 | - | - |
| 18 | A telehealth appointment was the only option available | 37 (8.4) | <0.001 | - | - |
| COVID-19 Pandemic | Pre-COVID-19 Pandemic | |||||
|---|---|---|---|---|---|---|
| Service Avoided (n = 440) | Service Accessed (n = 670) | χ2 Tests (p-Value) | Service Avoided (n = 460) | Service Accessed (n = 650) | χ2 Tests (p-Value) | |
| Age | Mean = 20.64 (SD = 0.48) | Mean = 20.63 (SD = 0.48) | Mean = 20.63 (SD = 0.48) | Mean = 20.64 (SD = 0.48) | ||
| Sex | 8.18 (0.004 **) | 4.53 (0.033 *) | ||||
| Male | 159 (34.6) | 300 (65.4) | 173 (37.7) | 286 (62.3) | ||
| Female | 281 (43.2) | 370 (56.8) | 287 (44.1) | 364 (55.9) | ||
| Country of birth | 0.11 (0.737) | 1.37 (0.242) | ||||
| Overseas | 21 (37.5) | 35 (62.5) | 19 (33.9) | 37 (66.1) | ||
| Australia | 419 (39.8) | 635 (60.2) | 441 (41.8) | 613 (58.2) | ||
| Residential state | 1.15 (0.764) | 2.51 (0.472) | ||||
| Others | 118 (41.3) | 168 (58.7) | 110 (38.5) | 176 (61.5) | ||
| NSW | 121 (37.9) | 198 (62.1) | 136 (42.4) | 183 (57.4) | ||
| VIC | 115 (38.6) | 183 (61.4) | 132 (44.3) | 166 (55.7) | ||
| QLD | 86 (41.5) | 121 (58.5) | 82 (39.6) | 125 (60.4) | ||
| Remoteness | 0.25 (0.617) | 0.55 (0.458) | ||||
| Major cities | 340 (40.1) | 509 (59.9) | 357 (42.1) | 492 (57.9) | ||
| Regional/Remote | 100 (38.3) | 161 (61.7) | 103 (39.5) | 158 (60.5) | ||
| Education | 0.00 (0.953) | 0.61 (0.435) | ||||
| Technical/Others | 161 (39.8) | 244 (60.2) | 174 (42.9) | 231 (57.1) | ||
| University/Tertiary | 279 (39.6) | 426 (60.4) | 286 (40.6) | 419 (59.4) | ||
| Employment | 1.64 (0.200) | 0.03 (0.858) | ||||
| Unemployed | 107 (43.2) | 141 (56.9) | 104 (41.9) | 144 (58.1) | ||
| Employed | 333 (38.6) | 529 (61.4) | 356 (41.3) | 506 (58.7) | ||
| Living with parents | 3.49 (0.062) | 8.85 (0.003 **) | ||||
| No | 139 (44.0) | 177 (56.0) | 153 (48.4) | 163 (51.6) | ||
| Yes | 301 (37.9) | 493 (62.1) | 307 (38.7) | 487 (61.3) | ||
| Family cohesion | 18.49 (<0.001 ***) | 6.62 (0.010 **) | ||||
| Poor | 94 (54.3) | 79 (45.7) | 87 (50.3) | 86 (49.7) | ||
| Strong | 346 (36.9) | 591 (63.1) | 373 (39.8) | 564 (60.2) | ||
| IRSAD Quintiles | 6.26 (0.180) | 5.38 (0.250) | ||||
| Q1 (0–20%)—Most disadvantaged | 112 (38.9) | 176 (61.1) | 117 (40.6) | 171 (59.4) | ||
| Q2 (20–40%) | 82 (40.4) | 121 (59.6) | 81 (39.9) | 122 (60.1) | ||
| Q3 (40–60%) | 119 (44.4) | 149 (55.6) | 126 (47.0) | 142 (53.0) | ||
| Q4 (60–80%) | 71 (39.7) | 108 (60.3) | 73 (40.8) | 106 (59.2) | ||
| Q5 (80–100%)—Most advantaged | 56 (32.6) | 116 (67.4) | 63 (36.6) | 109 (63.4) | ||
| Ongoing medical conditions | 16.64 (<0.001 ***) | 11.38 (0.001 **) | ||||
| No | 135 (32.0) | 287 (68.0) | 148 (35.1) | 274 (64.9) | ||
| Yes | 305 (44.3) | 383 (55.7) | 312 (45.4) | 376 (54.7) | ||
| Psychological distress | 95.31 (<0.001 ***) | 38.59 (<0.001 ***) | ||||
| Low | 75 (21.8) | 269 (78.2) | 220 (33.7) | 432 (66.3) | ||
| Moderate | 111 (36.0) | 197 (64.0) | ||||
| High | 254 (55.5) | 204 (44.5) | 240 (52.4) | 218 (47.6) | ||
| COVID-19-tested | 0.03 (0.854) | |||||
| Yes | 129 (40.1) | 193 (59.9) | - | - | - | |
| No | 311 (39.5) | 477 (60.5) | ||||
| Physical activity during lockdown | 3.79 (0.050 *) | |||||
| No | 160 (43.7) | 206 (56.3) | - | - | - | |
| Yes | 280 (37.6) | 464 (62.4) | ||||
| Employment status during lockdown | 2.43 (0.119) | |||||
| Unemployed | 285 (38.1) | 464 (61.9) | - | - | - | |
| Employed | 155 (42.9) | 206 (57.1) | ||||
| Coronavirus supplement during lockdown | 1.45 (0.228) | |||||
| No | 266 (38.3) | 429 (61.7) | - | - | - | |
| Yes | 174 (41.9) | 241 (58.1) | ||||
| The difficulty of life during lockdown | 24.61 (<0.001 ***) | |||||
| Less or no | 318 (45.2) | 386 (54.8) | - | - | - | |
| Few to many | 122 (30.1) | 284 (69.9) | ||||
| Model I (COVID-19 Pandemic) aOR (95% CI) 1 | Model II (Pre-COVID-19) aOR (95% CI) | |
|---|---|---|
| Sex | ||
| Male | Ref. | Ref. |
| Female | 1.27 * (1.01, 1.65) | 1.11 (0.94, 1.32) |
| Living with parents | ||
| No | Ref. | Ref. |
| Yes | 0.93 (0.67, 1.31) | 0.73 (0.46, 1.16) |
| Family cohesion | ||
| Poor | Ref. | Ref. |
| Strong | 0.73 (0.51, 1.10) | 0.70 (0.38, 1.29) |
| Ongoing medical conditions | ||
| No | Ref. | Ref. |
| Yes | 1.38 * (1.13, 1.70) | 1.33 (0.91, 1.95) |
| Psychological distress | ||
| Low | Ref. | Ref. |
| Moderate | 2.06 ** (1.35, 3.18) | 1.72 *** (1.31, 2.26) |
| High | 4.77 *** (3.57, 6.37) | 2.97 *** (2.11, 4.16) |
| Physical activity during lockdown | ||
| No | Ref. | - |
| Yes | 0.85 (0.63, 1.16) | |
| Difficulties of life in lockdown | ||
| Less difficulty or no | Ref. | - |
| Few to many | 0.81 (0.65, 1.02) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Islam, M.I.; Freeman, J.; Chadwick, V.; Martiniuk, A. Healthcare Avoidance before and during the COVID-19 Pandemic among Australian Youth: A Longitudinal Study. Healthcare 2022, 10, 1261. https://doi.org/10.3390/healthcare10071261
Islam MI, Freeman J, Chadwick V, Martiniuk A. Healthcare Avoidance before and during the COVID-19 Pandemic among Australian Youth: A Longitudinal Study. Healthcare. 2022; 10(7):1261. https://doi.org/10.3390/healthcare10071261
Chicago/Turabian StyleIslam, Md Irteja, Joseph Freeman, Verity Chadwick, and Alexandra Martiniuk. 2022. "Healthcare Avoidance before and during the COVID-19 Pandemic among Australian Youth: A Longitudinal Study" Healthcare 10, no. 7: 1261. https://doi.org/10.3390/healthcare10071261
APA StyleIslam, M. I., Freeman, J., Chadwick, V., & Martiniuk, A. (2022). Healthcare Avoidance before and during the COVID-19 Pandemic among Australian Youth: A Longitudinal Study. Healthcare, 10(7), 1261. https://doi.org/10.3390/healthcare10071261







