Readiness of Mozambique Health Facilities to Address Undernutrition and Diarrhea in Children under Five: Indicators from 2018 and 2021 Survey Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Collection
2.1.1. Service Availability and Readiness Assessment (SARA), 2018
2.1.2. Nutrition Service Assessment (NSA) in Three Provinces of Mozambique, 2021
2.2. Study Design and Population
2.2.1. Service Availability and Readiness Assessment—SARA, 2018
2.2.2. Nutrition Service Assessment—NSA, 2021
2.3. Data Analysis
2.4. Statistical Analysis
3. Results
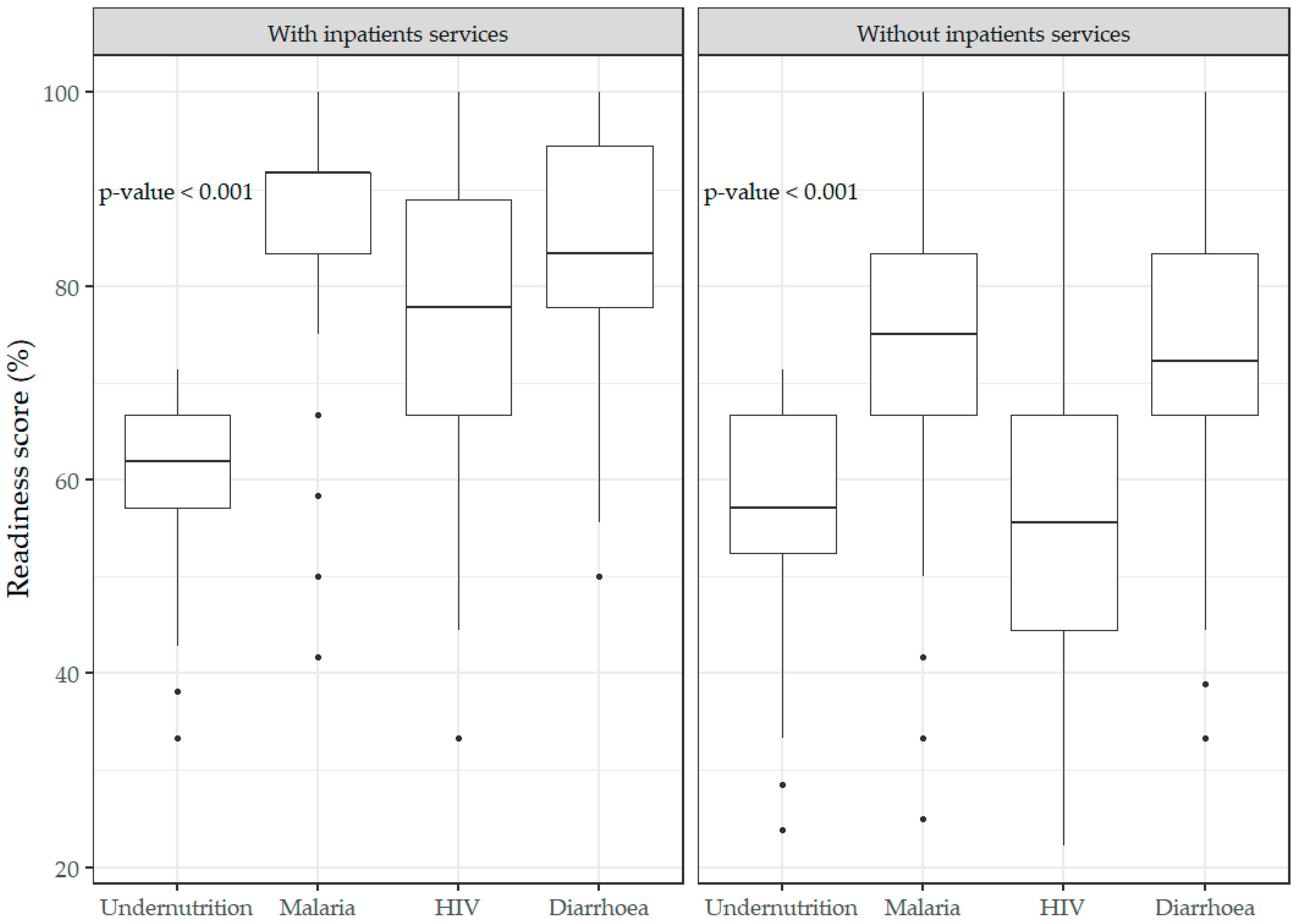
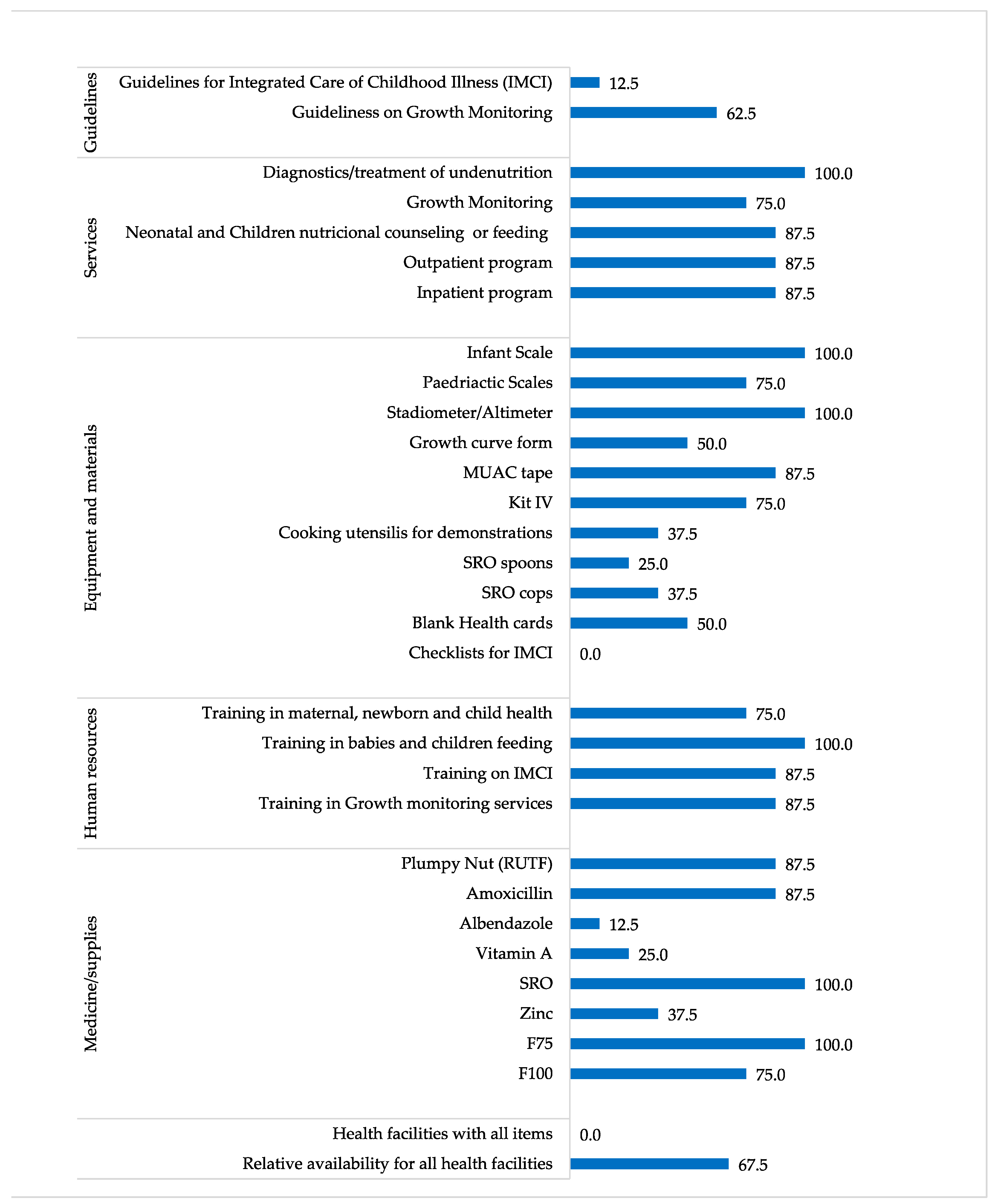
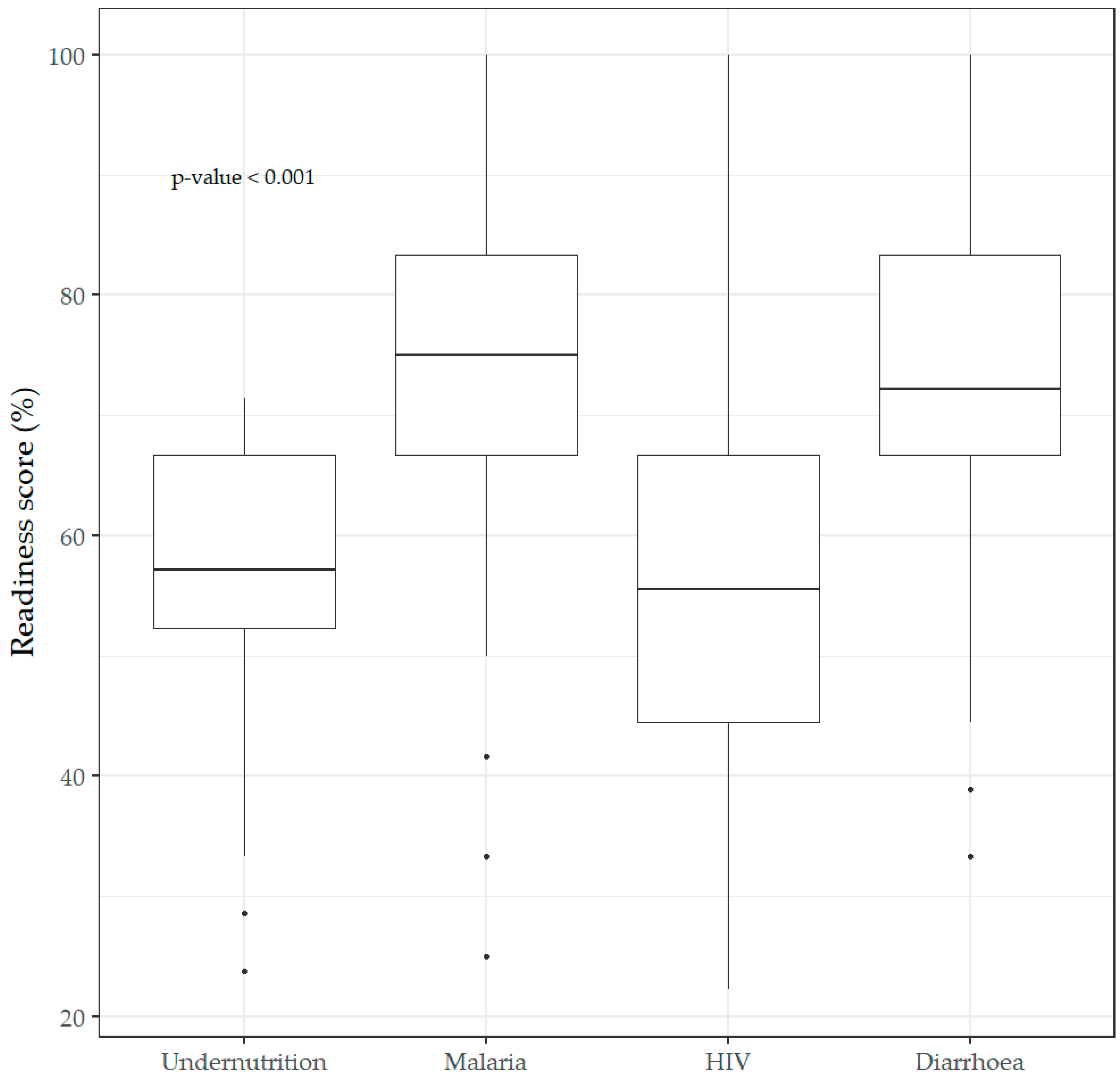
3.1. Service Availability and Readiness Assessment—SARA, 2018
3.1.1. Availability and Readiness
3.1.2. Quantile Regression Model Estimates for Readiness
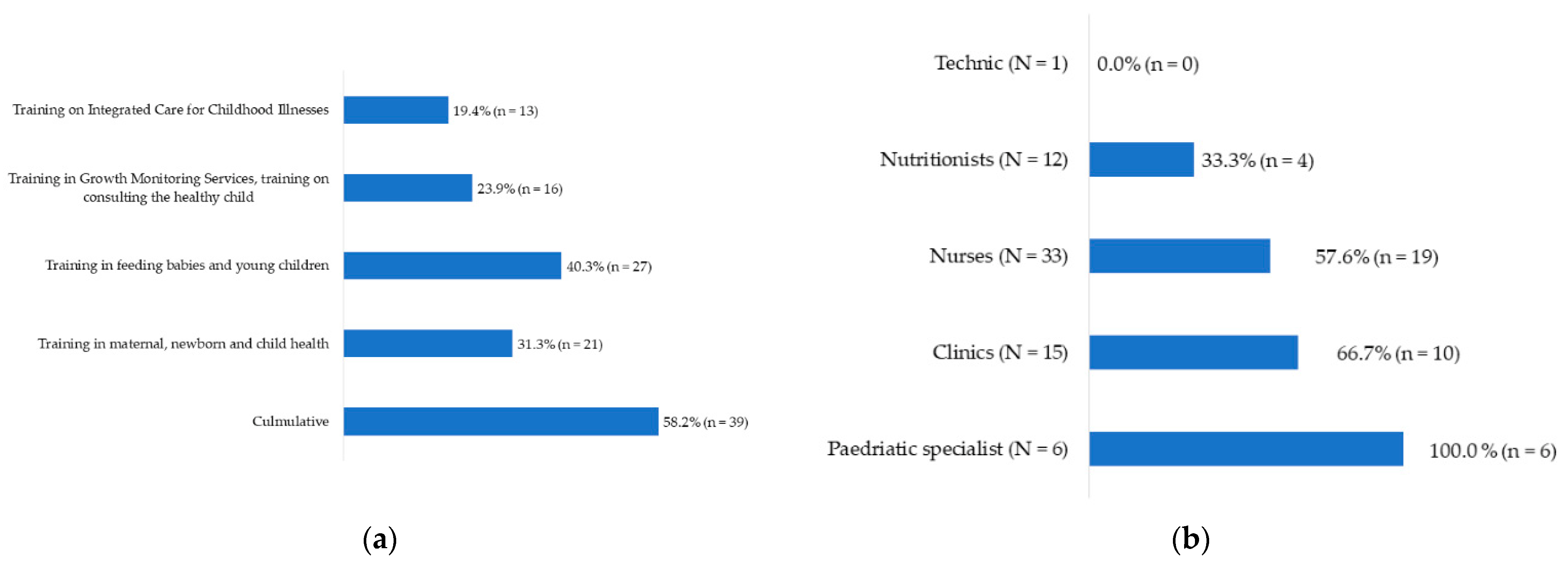
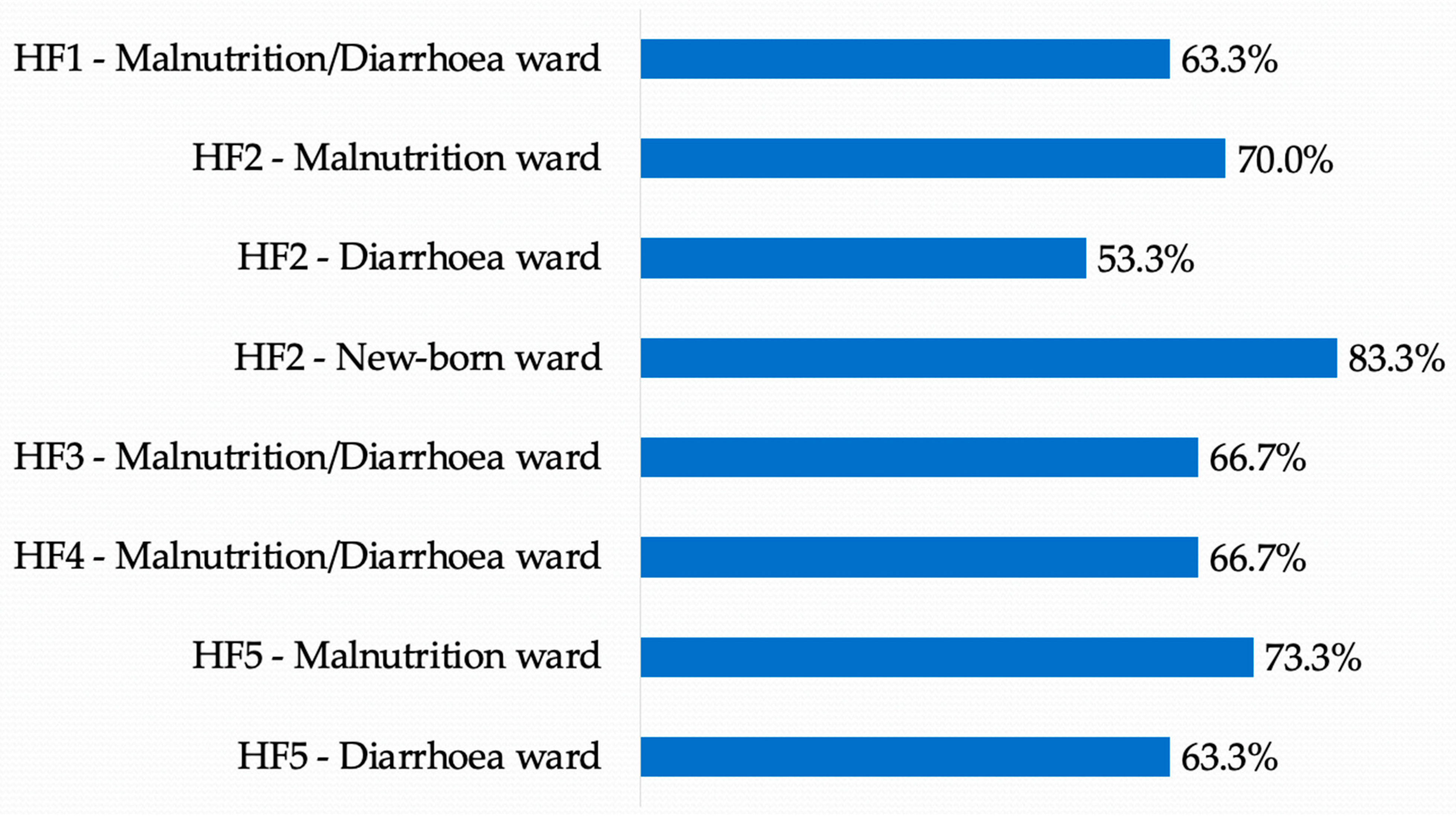
3.2. Nutrition Service Assessment: NSA, 2021
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
Appendix C
| Readiness Type | N | Min | Q1 | Median | Q3 | Max |
|---|---|---|---|---|---|---|
| Overall readiness | ||||||
| Undernutrition | 1295 | 23.8 | 52.4 | 57.1 | 66.7 | 71.4 |
| Malaria | 1214 | 25.0 | 66.7 | 75.0 | 83.3 | 100.0 |
| HIV | 1301 | 22.2 | 44.4 | 55.6 | 66.7 | 100.0 |
| Diarrhea | 1295 | 33.3 | 66.7 | 72.2 | 83.3 | 100.0 |
| Readiness for health facilities in rural areas | ||||||
| Undernutrition | 1123 | 23.8 | 52.4 | 57.1 | 66.7 | 71.4 |
| Malaria | 1057 | 25.0 | 66.7 | 75.0 | 83.3 | 100.0 |
| HIV | 1124 | 22.2 | 44.4 | 55.6 | 66.7 | 100.0 |
| Diarrhea | 1123 | 33.3 | 66.7 | 72.2 | 83.3 | 100.0 |
| Readiness for health facilities in urban areas | ||||||
| Undernutrition | 172 | 33.3 | 52.4 | 61.9 | 66.7 | 71.4 |
| Malaria | 157 | 41.7 | 75.0 | 83.3 | 91.7 | 100.0 |
| HIV | 177 | 22.2 | 55.6 | 66.7 | 77.8 | 100.0 |
| Diarrhea | 172 | 38.9 | 72.2 | 77.8 | 84.7 | 100.0 |
| Readiness for health facilities with inpatient services | ||||||
| Undernutrition | 174 | 33.3 | 57.1 | 61.9 | 66.7 | 71.4 |
| Malaria | 183 | 41.7 | 83.3 | 91.7 | 91.7 | 100.0 |
| HIV | 187 | 33.3 | 66.7 | 77.8 | 88.9 | 100.0 |
| Diarrhea | 174 | 50.0 | 77.8 | 83.3 | 94.4 | 100.0 |
| Readiness for health facilities without inpatient services | ||||||
| Undernutrition | 1121 | 23.8 | 52.4 | 57.1 | 66.7 | 71.4 |
| Malaria | 1031 | 25.0 | 66.7 | 75.0 | 83.3 | 100.0 |
| HIV | 1114 | 22.2 | 44.4 | 55.6 | 66.7 | 100.0 |
| Diarrhea | 1121 | 33.3 | 66.7 | 72.2 | 83.3 | 100.0 |
Appendix D
| Variables | p-Value | cOR 1 (IC 2 95%) | p-Value | aOR 3 (IC 2 95%) |
|---|---|---|---|---|
| Third quantile regression model estimates for diarrhea readiness | ||||
| Type of area | <0.001 | 0.337 | ||
| Urban | 1 | 1 | ||
| Rural | 0.946 (0.910–0.983) | 0.992 (0.976–1.008) | ||
| Type of health facility | <0.001 | 0.001 | ||
| With inpatient services | 1 | 1 | ||
| Without inpatient services | 0.895 (0.878–0.912) | 0.972 (0.955–0.988) | ||
| Readiness for undernutrition | <0.001 | 3.211 (3.211–3.211) | <0.001 | 2.559 (2.391–2.738) |
| Readiness for malaria | <0.001 | 1.560 (1.457–1.670) | <0.001 | 1.185 (1.126–1.248) |
| Readiness for HIV | <0.001 | 1.649 (1.576–1.725) | 0.027 | 1.059 (1.007–1.113) |
| Third quantile regression model estimates for undernutrition readiness | ||||
| Type of area | 1.000 | 0.001 | ||
| Urban | 1 | 1 | ||
| Rural | 1.000 (0.983–1.017) | 1.020 (1.008–1.032) | ||
| Type of health facility | 1.000 | <0.001 | ||
| With inpatient services | 1 | 1 | ||
| Without inpatient services | 1.000 (0.984–1.017) | 1.040 (1.027–1.053) | ||
| Readiness for diarrhea | <0.001 | 1.845 (1.772–1.920) | <0.001 | 1.831 (1.757–1.909) |
| Readiness for malaria | - | 1.000 (1.000–1.000) | <0.001 | 0.874 (0.841–0.908) |
| Readiness for HIV | <0.001 | 1.331 (1.280–1.383) | <0.001 | 1.163 (1.123–1.205) |
Appendix E
Appendix F
Appendix G

References
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-Quality Health Systems in the Sustainable Development Goals Era: Time for a Revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Everybody’s Business—Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Kruk, M.E.; Gage, A.D.; Joseph, N.T.; Danaei, G.; García-Saisó, S.; Salomon, J.A. Mortality Due to Low-Quality Health Systems in the Universal Health Coverage Era: A Systematic Analysis of Amenable Deaths in 137 Countries. Lancet 2018, 392, 2203–2212. [Google Scholar] [CrossRef] [Green Version]
- Paulson, K.R.; Kamath, A.M.; Alam, T.; Bienhoff, K.; Abady, G.G.; Abbas, J.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abd-Elsalam, S.M.; et al. Global, Regional, and National Progress towards Sustainable Development Goal 3.2 for Neonatal and Child Health: All-Cause and Cause-Specific Mortality Findings from the Global Burden of Disease Study 2019. Lancet 2021, 398, 870–905. [Google Scholar] [CrossRef]
- Acácio, S.; Mandomando, I.; Nhampossa, T.; Quintó, L.; Vubil, D.; Sacoor, C.; Kotloff, K.; Farag, T.; Nasrin, D.; Macete, E.; et al. Risk Factors for Death among Children 0–59 Months of Age with Moderate-to-Severe Diarrhea in Manhiça District, Southern Mozambique. BMC Infect. Dis. 2019, 19, 322. [Google Scholar] [CrossRef]
- INS; ICF. Inquérito Nacional Sobre Indicadores de Malária Em Moçambique 2018; Instituto Nacional de Saúde: Maputo, Mozambique; Rockville, MD, USA, 2019.
- INS; INE; ICF. Inquérito Nacional de Prevalência, Riscos Comportamentais e Informação Sobre o HIV e SIDA Em Moçambique 2009; ICF Macro: Calverton, MD, USA, 2010. [Google Scholar]
- Tickell, K.D.; Pavlinac, P.B.; John-Stewart, G.C.; Denno, D.M.; Richardson, B.A.; Naulikha, J.M.; Kirera, R.K.; Swierczewski, B.E.; Singa, B.O.; Walson, J.L. Impact of Childhood Nutritional Status on Pathogen Prevalence and Severity of Acute Diarrhea. Am. J. Trop. Med. Hyg. 2017, 97, 1337–1344. [Google Scholar] [CrossRef] [Green Version]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and Child Undernutrition and Overweight in Low-Income and Middle-Income Countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Black, R.; Fontaine, O.; Lamberti, L.; Bhan, M.; Huicho, L.; El Arifeen, S.; Masanja, H.; Walker, C.F.; Mengestu, T.K.; Pearson, L.; et al. Drivers of the Reduction in Childhood Diarrhea Mortality 1980–2015 and Interventions to Eliminate Preventable Diarrhea Deaths by 2030. J. Glob. Health 2019, 9, 020801. [Google Scholar] [CrossRef]
- Micha, R.; Mannar, V.; Afshin, A.; Allemandi, L.; Baker, P.; Battersby, J.; Bhutta, Z.; Chen, K.; Corvalan, C.; Di Cesare, M.; et al. 2020 Global Nutrition Report: Action on Equity to End Malnutrition. Available online: https://globalnutritionreport.org/reports/2020-global-nutrition-report/ (accessed on 25 January 2021).
- WHO; UNICEF; World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2019; p. 16. [Google Scholar]
- MISAU; INE; ICF. Inquérito de Indicadores de Imunização, Malária e HIV/SIDA Em Moçambique (IMASIDA) 2015; ICF International: Lexington, KY, USA, 2018. [Google Scholar]
- WHO. Prevalence of Stunting among Children Under-Five Years of Age (Height-for-Age <-2SD of the Median) (SDG 2.2.1). Available online: https://www.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/mca/prevalence-of-stunting-among-children-under-five-years-of-age-(height-for-age--2sd-of-the-median) (accessed on 28 January 2021).
- WHO. Prevalence of Wasting among Children Under-Five Years of Age (Weight-for-Height <-2SD of the Median). Available online: https://www.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/mca/prevalence-of-wasting-among-children-under-five-years-of-age-(weight-for-height--2sd-of-the-median) (accessed on 28 January 2021).
- WHO. Prevalence of Underweight among Children Under-Five Years of Age (Weight-for-Age <-2SD of the Median). Available online: https://www.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/mca/prevalence-of-underweight-among-children-under-five-years-of-age-(weight-for-age--2sd-of-the-median) (accessed on 28 January 2021).
- Sambo, J.; Cassocera, M.; Chissaque, A.; Bauhofer, A.F.L.; Roucher, C.; Chilaúle, J.; Cossa-Moiane, I.; Guimarães, E.L.; Manhique-Coutinho, L.; Anapakala, E.; et al. Characterizing Undernourished Children Under-Five Years Old with Diarrhoea in Mozambique: A Hospital Based Cross-Sectional Study, 2015–2019. Nutrients 2022, 14, 1164. [Google Scholar] [CrossRef]
- Brown, K.H. Diarrhea and Malnutrition. J. Nutr. 2003, 133, 328s–332s. [Google Scholar] [CrossRef] [Green Version]
- Murarkar, S.; Gothankar, J.; Doke, P.; Pore, P.; Lalwani, S.; Dhumale, G.; Quraishi, S.; Patil, R.; Waghachavare, V.; Dhobale, R.; et al. Prevalence and Determinants of Undernutrition among Under-Five Children Residing in Urban Slums and Rural Area, Maharashtra, India: A Community-Based Cross-Sectional Study. BMC Public Health 2020, 20, 1559. [Google Scholar] [CrossRef]
- Black, R.E.; Brown, K.H.; Becker, S. Malnutrition Is a Determining Factor in Diarrheal Duration, but Not Incidence, among Young Children in a Longitudinal Study in Rural Bangladesh. Am. J. Clin. Nutr. 1984, 39, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Schorling, J.B.; Mcauliffe, J.F.; De Souza, M.A.; Guerrant, R.L. Malnutrition Is Associated with Increased Diarrhoea Incidence and Duration among Children in an Urban Brazilian Slum. Int. J. Epidemiol. 1990, 19, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Tette, E.M.A.; Sifah, E.K.; Nartey, E.T. Factors Affecting Malnutrition in Children and the Uptake of Interventions to Prevent the Condition. BMC Pediatr. 2015, 15, 189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Correia, M.I.T.D.; Hegazi, R.A.; Higashiguchi, T.; Michel, J.-P.; Reddy, B.R.; Tappenden, K.A.; Uyar, M.; Muscaritoli, M. Evidence-Based Recommendations for Addressing Malnutrition in Health Care: An Updated Strategy from the FeedM.E. Global Study Group. J. Am. Med. Direct. Assoc. 2014, 15, 544–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barker, L.; Gout, B.; Crowe, T. Hospital Malnutrition: Prevalence, Identification and Impact on Patients and the Healthcare System. Int. J. Environ. Res. Public Health 2011, 8, 514–527. [Google Scholar] [CrossRef] [Green Version]
- Travis, P.; Bennett, S.; Haines, A.; Pang, T.; Bhutta, Z.; Hyder, A.A.; Pielemeier, N.R.; Mills, A.; Evans, T. Overcoming Health-Systems Constraints to Achieve the Millennium Development Goals. Lancet 2004, 364, 900–906. [Google Scholar] [CrossRef]
- Donabedian, A. The Quality of Care: How Can It Be Assessed? JAMA 1988, 260, 1743–1748. [Google Scholar] [CrossRef]
- Leslie, H.H.; Spiegelman, D.; Zhou, X.; Kruk, M.E. Service Readiness of Health Facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull. World Health Organ. 2017, 95, 738–748. [Google Scholar] [CrossRef]
- Roberton, T.; Carter, E.D.; Chou, V.B.; Stegmuller, A.R.; Jackson, B.D.; Tam, Y.; Sawadogo-Lewis, T.; Walker, N. Early Estimates of the Indirect Effects of the COVID-19 Pandemic on Maternal and Child Mortality in Low-Income and Middle-Income Countries: A Modelling Study. Lancet Glob. Health 2020, 8, e901–e908. [Google Scholar] [CrossRef]
- Billah, S.M.; Saha, K.K.; Khan, A.N.S.; Chowdhury, A.H.; Garnett, S.P.; Arifeen, S.E.; Menon, P. Quality of Nutrition Services in Primary Health Care Facilities: Implications for Integrating Nutrition into the Health System in Bangladesh. PLoS ONE 2017, 12, e0178121. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Service Availability and Readiness Assessment (SARA): An Annual Monitoring System for Service Delivery: Reference Manual; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Hampshire, R.D.; Aguayo, V.M.; Harouna, H.; Roley, J.A.; Tarini, A.; Baker, S.K. Delivery of Nutrition Services in Health Systems in Sub-Saharan Africa: Opportunities in Burkina Faso, Mozambique and Niger. Public Health Nutr. 2004, 7, 1047–1053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PEPFAR: President’s Emergency Program for AIDS Relief. Partnership to Fight HIV/AIDS in Mozambique; U.S. Embassy Maputo: Maputo, Mozambique, 2022.
- U.S. President’s Malaria Initiative. Mozambique Malaria Operational Plan FY 2022; USAID: Rockville, MD, USA, 2022.
- INS; OMS. SARA 2018: INVENTÁRIO NACIONAL; OMS em África: Brazzaville, Congo, 2020. [Google Scholar]
- O’Neill, K.; Takane, M.; Sheffel, A.; Abou-Zahr, C.; Boerma, T. Monitoring Service Delivery for Universal Health Coverage: The Service Availability and Readiness Assessment. Bull. World Health Organ. 2013, 91, 923–931. [Google Scholar] [CrossRef] [PubMed]
- El Haj, H.; Lamrini, M.; Rais, N. Quality of Care between Donabedian Model and ISO9001V2008. Int. J. Qual. Res. 2013, 7, 17–30. [Google Scholar]
- Berwick, D.; Fox, D.M. “Evaluating the Quality of Medical Care”: Donabedian’s Classic Article 50 Years Later. Milbank Q. 2016, 94, 237–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MISAU. Materiais de Apoio Ao Tratamento Da Desnutrição No Internamento (TDI); Ministério da Saúde: Maputo, Mozambique, 2015.
- Nilima, S.; Sen, K.K.; Zahura, F.T.; Bari, W. Prevalence and Determinants of Readiness of Health Facilities for Quality Antenatal Care Services in Bangladesh. Res. Sq. 2021. in review. [Google Scholar]
- Galarza, C.E.; Zhang, P.; Lachos, V.H. Logistic Quantile Regression for Bounded Outcomes Using a Family of Heavy-Tailed Distributions. Sankhya B 2021, 83, 325–349. [Google Scholar] [CrossRef]
- Adebisi, Y.A.; Alaran, A.; Badmos, A.; Bamisaiye, A.O.; Emmanuella, N.; Etukakpan, A.U.; Oladunjoye, I.O.; Oluwaseyifunmi, O.; Musa, S.K.; Akinmuleya, T.; et al. How West African Countries Prioritize Health. Trop. Med. Health 2021, 49, 87. [Google Scholar] [CrossRef]
- Adebisi, Y.A.; Umah, J.O.; Olaoye, O.C.; Alaran, A.J.; Sina-Odunsi, A.B.; Iii, D.E.L.-P. Assessment of Health Budgetary Allocation and Expenditure Toward Achieving Universal Health Coverage in Nigeria. J. Health Rep. Technol. 2020, 6, e102552. [Google Scholar] [CrossRef]
- Banda, K.; Chilengi-Sakala, S.; Chunga, C.C.; Solomon, H.; Chalwe, V.; Nkaama, J.M.; Leonard, C.; Bobo, M.; Aongola, A.; Biemba, G. Towards Universal Coverage for Nutrition Services in Children under Five Years-A Descriptive Analysis of the Capacity of Level One Hospitals to Provide Nutrition Services in Five Provinces of Zambia. PLoS ONE 2020, 15, e0232663. [Google Scholar] [CrossRef]
- Acharya, K.; Thapa, R.; Bhattarai, N.; Bam, K.; Shrestha, B. Availability and Readiness to Provide Sexually Transmitted Infections and HIV Testing and Counselling Services in Nepal: Evidence from Comprehensive Health Facility Survey. BMJ Open 2020, 10, e040918. [Google Scholar] [CrossRef]
- Bintabara, D.; Nakamura, K.; Seino, K. Determinants of Facility Readiness for Integration of Family Planning with HIV Testing and Counseling Services: Evidence from the Tanzania Service Provision Assessment Survey, 2014–2015. BMC Health Serv. Res. 2017, 17, 844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mills, A. Health Care Systems in Low- and Middle-Income Countries. N. Engl. J. Med. 2014, 370, 552–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wanzira, H.; Muyinda, R.; Lochoro, P.; Putoto, G.; Segafredo, G.; Wamani, H.; Lazzerini, M. Quality of Care for Children with Acute Malnutrition at Health Center Level in Uganda: A Cross Sectional Study in West Nile Region during the Refugee Crisis. BMC Health Serv. Res. 2018, 18, 561. [Google Scholar] [CrossRef]
- Winter, R.; Yourkavitch, J.; Wang, W.; Mallick, L. Assessment of Health Facility Capacity to Provide Newborn Care in Bangladesh, Haiti, Malawi, Senegal, and Tanzania. J. Glob. Health 2017, 7, 020509. [Google Scholar] [CrossRef] [PubMed]
- Millogo, O.; Doamba, J.E.O.; Sié, A.; Utzinger, J.; Vounatsou, P. Constructing a Malaria-Related Health Service Readiness Index and Assessing Its Association with Child Malaria Mortality: An Analysis of the Burkina Faso 2014 SARA Data. BMC Public Health 2021, 21, 20. [Google Scholar] [CrossRef]
- Mussa, A.H.; Pfeiffer, J.; Gloyd, S.S.; Sherr, K. Vertical Funding, Non-Governmental Organizations, and Health System Strengthening: Perspectives of Public Sector Health Workers in Mozambique. Hum. Resour. Health 2013, 11, 26. [Google Scholar] [CrossRef] [Green Version]
- MISAU. Plano Estratégico Do Sector Da Saúde—PESS 2014–2019; Ministério da Saúde: Maputo, Mozambique, 2013.
- MISAU. Plano Estratégico Da Malária 2012–2016; Ministério da Saúde: Maputo, Mozambique, 2012.
- MISAU. Plano Estratégico Da Malária 2017–2022; Ministério da Saúde: Maputo, Mozambique, 2017.
- De Maeseneer, J.; van Weel, C.; Egilman, D.; Mfenyana, K.; Kaufman, A.; Sewankambo, N. Strengthening Primary Care: Addressing the Disparity between Vertical and Horizontal Investment. Br. J. Gen. Pract. 2008, 58, 3–4. [Google Scholar] [CrossRef] [Green Version]
- Pfeiffer, J.; Montoya, P.; Baptista, A.J.; Karagianis, M.; Pugas, M.d.M.; Micek, M.; Johnson, W.; Sherr, K.; Gimbel, S.; Baird, S.; et al. Integration of HIV/AIDS Services into African Primary Health Care: Lessons Learned for Health System Strengthening in Mozambique—A Case Study. JIAS 2010, 13, 3. [Google Scholar] [CrossRef] [Green Version]
- England, R. The Dangers of Disease Specific Programmes for Developing Countries. BMJ 2007, 335, 565. [Google Scholar] [CrossRef] [Green Version]
- Correia, M.I.; Hegazi, R.A.; Graf, J.I.D.-P.; Gomez-Morales, G.; Gutiérrez, C.F.; Goldin, M.F.; Navas, A.; Espitia, O.L.P.; Tavares, G.M. Addressing Disease-Related Malnutrition in Healthcare: A Latin American Perspective. J. Parenter. Enter. Nutr. 2016, 40, 7. [Google Scholar] [CrossRef] [Green Version]
- MISAU. Multisectoral Action Plan for the Reduction of Chronic Undernutrition in Mozambique 2011–2015 (2020); USAID: Maputo, Mozambique, 2010.
- Arifeen, S.E.; Blum, L.S.; Hoque, D.M.E.; Chowdhury, E.K.; Khan, R.; Black, R.E.; Victora, C.G.; Bryce, J. Integrated Management of Childhood Illness (IMCI) in Bangladesh: Early Findings from a Cluster-Randomised Study. Lancet 2004, 364, 1595–1602. [Google Scholar] [CrossRef]
- Bintabara, D.; Ernest, A.; Mpondo, B. Health Facility Service Availability and Readiness to Provide Basic Emergency Obstetric and Newborn Care in a Low-Resource Setting: Evidence from a Tanzania National Survey. BMJ Open 2019, 9, e020608. [Google Scholar] [CrossRef] [PubMed]
- Abayneh, M.; Gebremedhin, T.; Dellie, E.; Tsehay, C.T.; Atnafu, A. Improving the Assessment and Classification of Sick Children According to the Integrated Management of Childhood Illness (IMCI) Protocol at Sanja Primary Hospital, Northwest Ethiopia: A Pre-Post Interventional Study. Int. J. Pediatr. 2020, 2020, e2501932. [Google Scholar] [CrossRef] [PubMed]
- Schellenberg, J.R.A.; Adam, T.; Mshinda, H.; Masanja, H.; Kabadi, G.; Mukasa, O.; John, T.; Charles, S.; Nathan, R.; Wilczynska, K.; et al. Effectiveness and Cost of Facility-Based Integrated Management of Childhood Illness (IMCI) in Tanzania. Lancet 2004, 364, 1583–1594. [Google Scholar] [CrossRef]
- Nimpagaritse, M.; Korachais, C.; Nsengiyumva, G.; Macq, J.; Meessen, B. Addressing Malnutrition among Children in Routine Care: How Is the Integrated Management of Childhood Illnesses Strategy Implemented at Health Centre Level in Burundi? BMC Nutr. 2019, 5, 22. [Google Scholar] [CrossRef] [Green Version]
- Chopra, M. Strategies to Improve Health Coverage and Narrow the Equity Gap in Child Survival, Health, and Nutrition. Lancet 2012, 380, 10. [Google Scholar] [CrossRef] [Green Version]
- Pelly, L.; Srivastava, K.; Singh, D.; Anis, P.; Mhadeshwar, V.B.; Kumar, R.; Crockett, M. Readiness to Provide Child Health Services in Rural Uttar Pradesh, India: Mapping, Monitoring and Ongoing Supportive Supervision. BMC Health Serv. Res. 2021, 21, 914. [Google Scholar] [CrossRef]
- Roberds, A.; Ferraro, E.; Luckhart, S.; Stewart, V.A. HIV-1 Impact on Malaria Transmission: A Complex and Relevant Global Health Concern. Front. Cell Infect. Microbiol. 2021, 11, 656938. [Google Scholar] [CrossRef]
- Anand, A.; Favero, R.; Dentinger, C.; Ralaivaomisa, A.; Ramamonjisoa, S.; Rabozakandraina, O.; Razafimandimby, E.; Razafindrakoto, J.; Wolf, K.; Steinhardt, L.; et al. Malaria Case Management and Elimination Readiness in Health Facilities of Five Districts of Madagascar in 2018. Malar. J. 2020, 19, 351. [Google Scholar] [CrossRef]
| Pillar | Indicators | Data Collection Method | Respondents |
|---|---|---|---|
| Structural Readiness | Human resources, Infrastructure (by interview and observation), Equipment (including observation), Screening for malnutrition in children with diarrhea as a routine, Clinical meetings to discuss child health management, Guidelines. | Structured questionnaire including a checklist Observation of the existence of functional equipment and materials. | Nurse in charge, nutritionist, and pharmacist. |
| Academic profile of health professionals, Experience, Training in the last two years, Supervisions. | Interview using a structured questionnaire. | All health professionals in the pediatric wards who are responsible for the care and monitoring of malnourished children were interviewed. |
| Variables | Diarrhea % (n/N) | Nutrition % (n/N) | Malaria % (n/N) | HIV % (n/N) |
|---|---|---|---|---|
| Guidelines | ||||
| Guidelines for the integrated care of childhood illness (IMCI) | 55.5 (867/1561) | 55.5 (867/1561) | - | 55.5 (867/1561) |
| Guidelines on growth monitoring | 53.1 (829/1561) | 53.1 (829/1561) | - | - |
| IMCI checklist | - | 55.9 (873/1561) | - | - |
| Malaria guidelines for diagnostics and treatment | - | - | 60.3 (939/1556) | - |
| Equipment | ||||
| Stadiometer/Altimeter | 100.0 (1423/1423) | 100.0 (1423/1423) | - | - |
| Growth curve form | - | 58.7 (916/1561) | - | - |
| Pediatric scale | 98.8 (1448/1466) | 98.8 (1448/1466) | 98.8 (1448/1466) | 98.8 (1448/1466) |
| MUAC tape | 93.2 (1455/1561) | 93.2 (1403/1498) | - | - |
| Thermometer | - | - | 98.8 (1328/1344) | - |
| Differential diagnosis | ||||
| HIV rapid test | 95.1 (1425/1498) | 95.1 (1425/1498) | - | 95.1 (1425/1498) |
| Malaria rapid test | 93.7 (1403/1498) | 93.7 (1403/1498) | - | - |
| Malaria rapid test or microscopy | - | - | 97.6 (1462/1498) | - |
| Blood collection on filter paper | - | - | - | 71.3 (1068/1498) |
| Medicine/supplies | ||||
| Oral rehydration salt | 97.6 (1492/1528) | 97.6 (1492/1528) | - | - |
| Zinc sulfate | 41.5 (634/1528) | 41.5 (634/1528) | - | - |
| Vitamin A | 91.5 (1398/1528) | 91.5 (1398/1528) | - | - |
| Amoxicillin | 85.7 (1309/1528) | 85.7 (1309/1528) | - | - |
| Cotrimoxazole | 88.1 (1346/1528) | 88.1 (1346/1528) | - | - |
| Albendazole/Metronidazole * | 91.0 (1390/1528) | 97.2 (1485/1528) | - | - |
| Coarten (artemeter and lumefantrina) | - | - | 93.3 (1421/1523) | - |
| Injectable or rectal artesunate | - | - | 58.8 (896/1523) | - |
| Quinine | - | - | 62.4 (951/1523) | - |
| Paracetamol or Ibuprofen | - | - | 88.9 (1359/1528) | - |
| Nevirapine syrup (NVP) or Lopinavir (LVP) + Ritonavir (RTV) | - | - | - | 95.6 (821/859) |
| Zitovudina (AZT) or Abacavir (ABC) | - | - | - | 42.9 (600/1399) |
| Lamivudine (3TC) | - | - | - | 7.4 (104/1399) |
| Human resources and training | ||||
| Training on IMCI in the last two years | 46.1 (720/1561) | 46.1 (720/1561) | ||
| Training in growth monitoring services in the last two years | 35.0 (546/1561) | 35.0 (546/1561) | - | - |
| General clinicians | 7.2 (113/1561) | 7.2 (113/1561) | 7.2 (113/1561) | 7.2 (113/1561) |
| General nurses | 50.9 (795/1561) | 50.9 (795/1561) | 59.2 (924/1561) | - |
| Nutritionists | - | 8.8 (117/1330) | - | - |
| Maternal and child health nurses | 87.4 (1365/1561) | 87.4 (1365/1561) | - | 87.4 (1365/1561) |
| Medical technicians | - | - | 55.1 (860/1561) | 55.1 (860/1561) |
| Overall items’ relative availability | 73.0 | 68.6 | 72.3 | 58.0 |
| Health facilities with all items | 1.2 (15/1295) | 0.0 (0/1295) | 4.0 (48/1214) | 0.6 (8/1301) |
| Variables | p-Value | cOR 1 (CI 2 95%) | p-Value | aOR 3 (CI 2 95%) |
|---|---|---|---|---|
| Median quantile regression model estimates for diarrhea readiness | ||||
| Type of area | <0.001 | 0.495 | ||
| Urban | 1 | 1 | ||
| Rural | 0.946 (0.919–0.974) | 0.995 (0.981–1.010) | ||
| Type of health facility | <0.001 | <0.001 | ||
| With inpatient services | 1 | 1 | ||
| Without inpatient services | 0.895 (0.869–0.921) | 0.965 (0.951–0.980) | ||
| Readiness for undernutrition | <0.001 | 3.211 (3.046–3.385) | <0.001 | 2.597 (2.447–2.758) |
| Readiness for malaria | <0.001 | 1.560 (1.446–1.683) | <0.001 | 1.199 (1.146–1.255) |
| Readiness for HIV | <0.001 | 1.649 (1.542–1.763) | 0.045 | 1.047 (1.001–1.094) |
| Median quantile regression model estimates for undernutrition readiness | ||||
| Type of area | <0.001 | 0.087 | ||
| Urban | 1 | 1 | ||
| Rural | 0.953 (0.930–0.977) | 1.010 (0.999–1.021) | ||
| Type of health facility | <0.001 | <0.001 | ||
| With inpatient services | 1 | 1 | ||
| Without inpatient services | 0.953 (0.930–0.977) | 1.029 (1.018–1.041) | ||
| Readiness for diarrhea | <0.001 | 1.902 (1.837–1.970) | <0.001 | 1.985 (1.911–2.062) |
| Readiness for malaria | <0.001 | 1.331 (1.247–1.420) | <0.001 | 0.892 (0.861–0.924) |
| Readiness for HIV | <0.001 | 1.535 (1.449–1.626) | <0.001 | 1.089 (1.054–1.126) |
| n (%) | |
|---|---|
| Number of health professionals by health facility (HF) | |
| HF2 | 24 (35.8) |
| HF5 | 14 (20.9) |
| HF1 | 12 (17.9) |
| HF4 | 9 (13.4) |
| HF3 | 8 (11.9) |
| Roles of the health professionals | |
| Nurse | 33 (49.3) |
| Generalist medical doctor | 15 (22.4) |
| Nutritionist | 12 (17.9) |
| Pediatrician | 6 (9.0) |
| Technician (preventive medicine) | 1 (1.5) |
| Years of work by HF | Median (IQ), min–max |
| HF2 | 3.0 (1.75–7.25), 0–30 |
| HF5 | 2.5 (2.0–6.5), 0–16 |
| HF1 | 3.5 (1.0–6.75), 0–12 |
| HF4 | 8.0 (3.0–15.0), 0–16 |
| HF3 | 3.5 (1.5–5.25), 0–20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sambo, J.; Bauhofer, A.F.L.; Boene, S.S.; Djedje, M.; Júnior, A.; Pilale, A.; Gonçalves, L.; Deus, N.d.; Chicumbe, S. Readiness of Mozambique Health Facilities to Address Undernutrition and Diarrhea in Children under Five: Indicators from 2018 and 2021 Survey Data. Healthcare 2022, 10, 1200. https://doi.org/10.3390/healthcare10071200
Sambo J, Bauhofer AFL, Boene SS, Djedje M, Júnior A, Pilale A, Gonçalves L, Deus Nd, Chicumbe S. Readiness of Mozambique Health Facilities to Address Undernutrition and Diarrhea in Children under Five: Indicators from 2018 and 2021 Survey Data. Healthcare. 2022; 10(7):1200. https://doi.org/10.3390/healthcare10071200
Chicago/Turabian StyleSambo, Júlia, Adilson Fernando Loforte Bauhofer, Simone S. Boene, Marlene Djedje, António Júnior, Adalgisa Pilale, Luzia Gonçalves, Nilsa de Deus, and Sérgio Chicumbe. 2022. "Readiness of Mozambique Health Facilities to Address Undernutrition and Diarrhea in Children under Five: Indicators from 2018 and 2021 Survey Data" Healthcare 10, no. 7: 1200. https://doi.org/10.3390/healthcare10071200
APA StyleSambo, J., Bauhofer, A. F. L., Boene, S. S., Djedje, M., Júnior, A., Pilale, A., Gonçalves, L., Deus, N. d., & Chicumbe, S. (2022). Readiness of Mozambique Health Facilities to Address Undernutrition and Diarrhea in Children under Five: Indicators from 2018 and 2021 Survey Data. Healthcare, 10(7), 1200. https://doi.org/10.3390/healthcare10071200






