Polycystic Ovary Syndrome (PCOS) and Non-Suicidal Self-Injury (NSSI): A Community-Based Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
2.2.1. Demographics
2.2.2. Difficulties in Emotion Regulation Scale (DERS)
2.2.3. Ruminative Responses Scale (RRS)
2.2.4. Deliberate Self-Harm Inventory Self-Injurious (DSHI)
2.2.5. Suicide Behaviors Questionnaire-Revised (SBQ-R)
2.3. Procedure
2.4. Analysis
3. Results
3.1. Preliminary Analyses
3.2. Prevalence
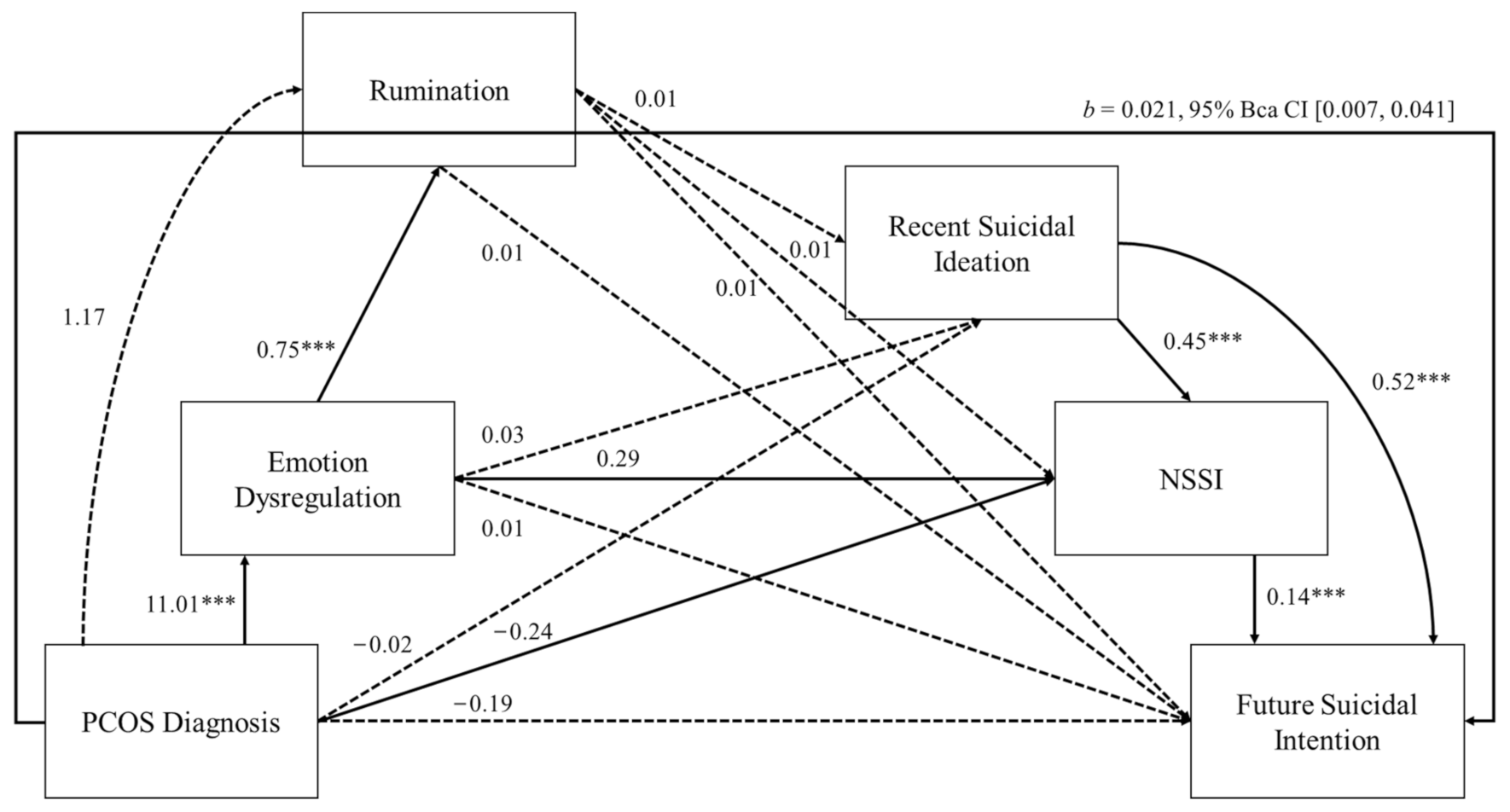
3.3. Correlations and Serial Mediation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goodman, N.F.; Cobin, R.H.; Futterweit, W.; Glueck, J.S.; Legro, R.S.; Carmina, E.; American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Androgen Excess and PCOS Society (AES). American association of clinical endocrinologists, American college of endocrinology, and Androgen excess and PCOS society disease state clinical review: Guide to the best practices in the evaluation and treatment of polycystic ovary syndrome—Part 1. Endocr. Pract. 2015, 21, 1291–1300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.J.; Ullah, A.; Basit, S. Genetic basis of polycystic ovary syndrome (PCOS): Current perspectives. Appl. Clin. Genet. 2019, 12, 249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, S. Polycystic ovary syndrome (PCOS), an inflammatory, systemic, lifestyle endocrinopathy. J. Steroid. Biochem. Mol. Biol. 2018, 182, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Marsh, C.A.; Berent-Spillson, A.; Love, T.; Persad, C.C.; Pop-Busui, R.; Zubieta, J.K.; Smith, Y.R. Functional neuroimaging of emotional processing in women with polycystic ovary syndrome: A case-control pilot study. Fertil. Steril. 2013, 100, 200–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scaruffi, E.; Franzoi, I.G.; Civilotti, C.; Guglielmucci, F.; La Marca, L.; Tomelini, M.; Veglia, F.; Granieri, A. Body image, personality profiles and alexithymia in patients with polycystic ovary syndrome (PCOS). J. Psychosom. Obstet. Gynaecol. 2019, 40, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Barry, J.A.; Kuczmierczyk, A.R.; Hardiman, P.J. Anxiety and depression in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2011, 26, 2442–2451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooney, L.G.; Dokras, A. Depression and anxiety in polycystic ovary syndrome: Etiology and Treatment. Curr. Psychiatry Rep. 2017, 19, 83. [Google Scholar] [CrossRef] [PubMed]
- Cooney, L.G.; Lee, I.; Sammel, M.D.; Dokras, A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2017, 32, 1075–1091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deeks, A.A.; Gibson-Helm, M.E.; Teede, H.J. Anxiety and depression in polycystic ovary syndrome: A comprehensive investigation. Fertil. Steril. 2010, 93, 2421–2423. [Google Scholar] [CrossRef]
- Dokras, A.; Stener-Victorin, E.; Yildiz, B.O.; Li, R.; Ottey, S.; Shah, D.; Teede, H. Androgen Excess-Polycystic Ovary Syndrome Society: Position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertil. Steril. 2018, 109, 888–899. [Google Scholar] [CrossRef]
- Damone, A.L.; Joham, A.E.; Loxton, D.; Earnest, A.; Teede, H. Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychol. Med. 2019, 49, 1510–1520. [Google Scholar] [CrossRef]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J. International PCOS Network Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. 2018, 33, 1602–1618. [Google Scholar] [CrossRef] [Green Version]
- Hart, R.; Doherty, D.A. The potential implications of a PCOS diagnosis on a woman’s long-term health using data linkage. J. Clin. Endocrinol. Metab. 2015, 100, 911–919. [Google Scholar] [CrossRef]
- Williams, S.; Sheffield, D.; Knibb, R.C. ‘Everything’s from the inside out with PCOS’: Exploring women’s experiences of living with polycystic ovary syndrome and co-morbidities through Skype™ interviews. Health Psychol. Open 2015, 28, 2055102915603051. [Google Scholar] [CrossRef] [Green Version]
- Kjaer, T.; Jensen, A.; Dalton, S.; Johansen, C.; Schmiedel, S.; Kjaer, S. Suicide in Danish women evaluated for fertility problems. Hum. Reprod. 2011, 26, 2401–2407. [Google Scholar] [CrossRef] [Green Version]
- Shani, C.; Yelena, S.; Reut, B.; Adrian, S.; Sami, H. Suicidal risk among infertile women undergoing in-vitro fertilization: Incidence and risk factors. Psychiatry Res. 2016, 240, 53–59. [Google Scholar] [CrossRef]
- Shah, K.; Kulkarni, R.; Singh, R.; Pannu, H.S.; Kamrai, D. Role of Bupropion and Naltrexone in Managing Depression With Polycystic Ovary Syndrome: A Case Report and Literature Review. Cureus 2020, 12. [Google Scholar] [CrossRef]
- Månsson, M.; Holte, J.; Landin-Wilhelmsen, K.; Dahlgren, E.; Johansson, A.; Landén, M. Women with polycystic ovary syndrome are often depressed or anxious—A case control study. Psychoneuroendocrinology 2008, 33, 1132–1138. [Google Scholar] [CrossRef]
- Cesta, C.E.; Månsson, M.; Palm, C.; Lichtenstein, P.; Iliadou, A.N.; Landén, M. Polycystic ovary syndrome and psychiatric disorders: Co-morbidity and heritability in a nationwide Swedish cohort. Psychoneuroendocrinology 2016, 73, 196–203. [Google Scholar] [CrossRef] [Green Version]
- Hawton, K.; Zahl, D.; Wetherall, R. Suicide following deliberate self-harm: Long-term follow-up of patients who presented to a general hospital. BJPsych 2003, 182, 537–542. [Google Scholar] [CrossRef] [Green Version]
- Klonsky, E.D.; May, A.M. Differentiating suicide attempters from suicide ideators: A critical frontier for suicidology research. Suicide Life Threat. Behav. 2014, 44, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; Saffer, B.Y.; Bryan, C.J. Ideation-to-action theories of suicide: A conceptual and empirical update. Curr. Opin. Psychol. 2017, 22, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.R.; Selby, E.A.; Joiner, T.E. The interpersonal theory of suicide. Psychol. Rev. 2010, 117, 575–600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fadoir, N.A.; Lutz-Zois, C.J.; Goodnight, J.A. Psychopathy and suicide: The mediating effects of emotional and behavioural dysregulation. Pers. Individ. Differ. 2019, 142, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Hare, R.D.; Neumann, C.S. Psychopathy as a clinical and empirical construct. Annu. Rev. Clin. Psychol. 2008, 4, 217–246. [Google Scholar] [CrossRef] [Green Version]
- Gross, J.J.; John, O.P. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 2003, 85, 348. [Google Scholar] [CrossRef]
- Johnson, D.P.; Whisman, M.A. Gender differences in rumination: A meta-analysis. Pers. Individ. Differ. 2013, 55, 367–374. [Google Scholar] [CrossRef] [Green Version]
- Fowler, C.H.; Miernicki, M.E.; Rudolph, K.D.; Telzer, E.H. Disrupted amygdala-prefrontal connectivity during emotion regulation links stress-reactive rumination and adolescent depressive symptoms. Dev. Cog. Neurosci. 2017, 27, 99–106. [Google Scholar] [CrossRef]
- Selby, E.A.; Anestis, M.D.; Joiner, T.E. Understanding the relationship between emotional and behavioral dysregulation: Emotional cascades. Behav. Res. Ther. 2008, 46, 593–611. [Google Scholar] [CrossRef]
- Nock, M.K. Why do people hurt themselves? New insights into the nature and functions of self-injury. Curr. Dir. Psychol. Sci. 2009, 18, 78–83. [Google Scholar] [CrossRef] [Green Version]
- Klonsky, E.D.; May, A.M.; Glenn, C.R. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J. Abnorm. Psychol. 2013, 122, 231. [Google Scholar] [CrossRef] [Green Version]
- Joiner, T.E.; Ribeiro, J.D.; Silva, C. Nonsuicidal self-injury, suicidal behavior, and their co-occurrence as viewed through the lens of the interpersonal theory of suicide. Curr. Dir. Psychol. Sci. 2012, 21, 342–347. [Google Scholar] [CrossRef]
- Volk, F.; Thomas, J.; Sosin, L.; Jacob, V.; Moen, C. Religiosity, developmental context, and sexual shame in pornography users: A serial mediation model. Sex. Addict. Compulsivity 2016, 23, 244–259. [Google Scholar] [CrossRef]
- Peer, E.; Brandimarte, L.; Samat, S.; Acquisti, A. Beyond the Turk: Alternative platforms for crowdsourcing behavioral research. J. Exp. Soc. Psychol. 2017, 70, 153–163. [Google Scholar] [CrossRef] [Green Version]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Treynor, W.; Gonzalez, R.; Nolen-Hoeksema, S. Rumination reconsidered: A psychometric analysis. Cognit. Ther. Res. 2003, 27, 247–259. [Google Scholar] [CrossRef]
- Gratz, K.L. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. J. Psychopathol. Behav. Assess. 2001, 23, 253–263. [Google Scholar] [CrossRef]
- Osman, A.; Bagge, C.L.; Gutierrez, P.M.; Konick, L.C.; Kopper, B.A.; Barrios, F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment 2001, 8, 443–454. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Rudd, M.D. Fluid vulnerability theory: A cognitive approach to understanding the process of acute and chronic suicide risk. In Cognition and Suicide: Theory, Research, and Therapy; Ellis, T.E., Ed.; American Psychological Association: Washington, DC, USA, 2006; pp. 355–368. [Google Scholar] [CrossRef]
- Richardson, M. Beyond restoration: Considering emotion regulation in natural well-being. Ecopsychology 2019, 11, 123–129. [Google Scholar] [CrossRef]
- Guendelman, S.; Medeiros, S.; Rampes, H. Mindfulness and emotion regulation: Insights from neurobiological, psychological, and clinical studies. Front. Psychol. 2017, 8, 220. [Google Scholar] [CrossRef] [PubMed]
| MPCOS− (SD) | MPCOS+ (SD) | t | p | 95% CI | d | |
|---|---|---|---|---|---|---|
| Age | 33.65 (11.38) | 31.01 (6.33) | 2.33 | 0.02 | (0.415, 4.859) | 0.29 |
| Education | 2.73 (0.90) | 2.51 (0.97) | 2.196 | 0.03 | (0.023, 4.19) | 0.24 |
| Emotion Dysregulation | 37.50 (15.54) | 50.18 (16.77 | −7.25 | <0.001 | (−16.120, −9.244) | 0.78 |
| Rumination | 46.38 (14.28) | 56.98 (13.94) | −6.78 | <0.001 | (−13.670, −7.527) | 0.75 |
| Recent suicidal ideation | 0.65 (1.04) | 1.15 (1.16) | −4.21 | <0.001 | (−0.730, −0.266) | 0.45 |
| NSSI | 1.19 (1.69) | 1.57 (1.70) | −2.04 | 0.04 | (−0.746, −0.013) | 0.22 |
| Future suicidal intention | 1.00 (1.19) | 1.33 (1.45) | −2.33 | 0.02 | (−0.598, −0.051) | 0.25 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. PCOS | - | 0.335 *** | 0.316 *** | 0.202 *** | 0.099 * | 0.113 * |
| 2. Emotion Dysregulation | - | - | 0.853 *** | 0.583 *** | 0.475 *** | 0.500 *** |
| 3. Rumination | - | - | - | 0.527 *** | 0.418 *** | 0.471 *** |
| 4. Recent suicidal ideation | - | - | - | 0.459 *** | 0.624 *** | |
| 5. NSSI | - | - | - | - | - | 0.457 *** |
| 6. Future suicidal intention | - | - | - | - | - | - |
| M(SD) | - | 40.92 (16.84) | 49.25 (14.93) | 0.79 (1.09) | 1.29 (1.70) | 1.09 (1.27) |
| z-Skewness | - | 3.31 | 1.94 | 11.11 | 11.79 | 9.59 |
| z-Kurtosis | - | −3.70 | −2.65 | 3.68 | 5.94 | 6.22 |
| a | - | 0.95 | 0.96 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Williams, S.; Fido, D.; Sheffield, D. Polycystic Ovary Syndrome (PCOS) and Non-Suicidal Self-Injury (NSSI): A Community-Based Study. Healthcare 2022, 10, 1118. https://doi.org/10.3390/healthcare10061118
Williams S, Fido D, Sheffield D. Polycystic Ovary Syndrome (PCOS) and Non-Suicidal Self-Injury (NSSI): A Community-Based Study. Healthcare. 2022; 10(6):1118. https://doi.org/10.3390/healthcare10061118
Chicago/Turabian StyleWilliams, Sophie, Dean Fido, and David Sheffield. 2022. "Polycystic Ovary Syndrome (PCOS) and Non-Suicidal Self-Injury (NSSI): A Community-Based Study" Healthcare 10, no. 6: 1118. https://doi.org/10.3390/healthcare10061118
APA StyleWilliams, S., Fido, D., & Sheffield, D. (2022). Polycystic Ovary Syndrome (PCOS) and Non-Suicidal Self-Injury (NSSI): A Community-Based Study. Healthcare, 10(6), 1118. https://doi.org/10.3390/healthcare10061118







