Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection Process
2.4. Data Extraction and Synthesis
2.5. Critical Reading and Level of Evidence
2.6. Data Analysis
3. Results
3.1. Search Results
3.2. Study and Participant Characteristics
3.3. Burnout Syndrome and Sleep Problems in Nurses
3.4. Sociodemographic Variables and Probability of Suffering from Burnout and Sleep Disorders
3.5. Sleep Problems, Burnout Syndrome and the Organization of Nursing Work
3.6. Other Risk Factors: Work Environment, Workplace Violence and Psychological Factors
3.7. Psychological Interventions to Improve Sleep and Burnout
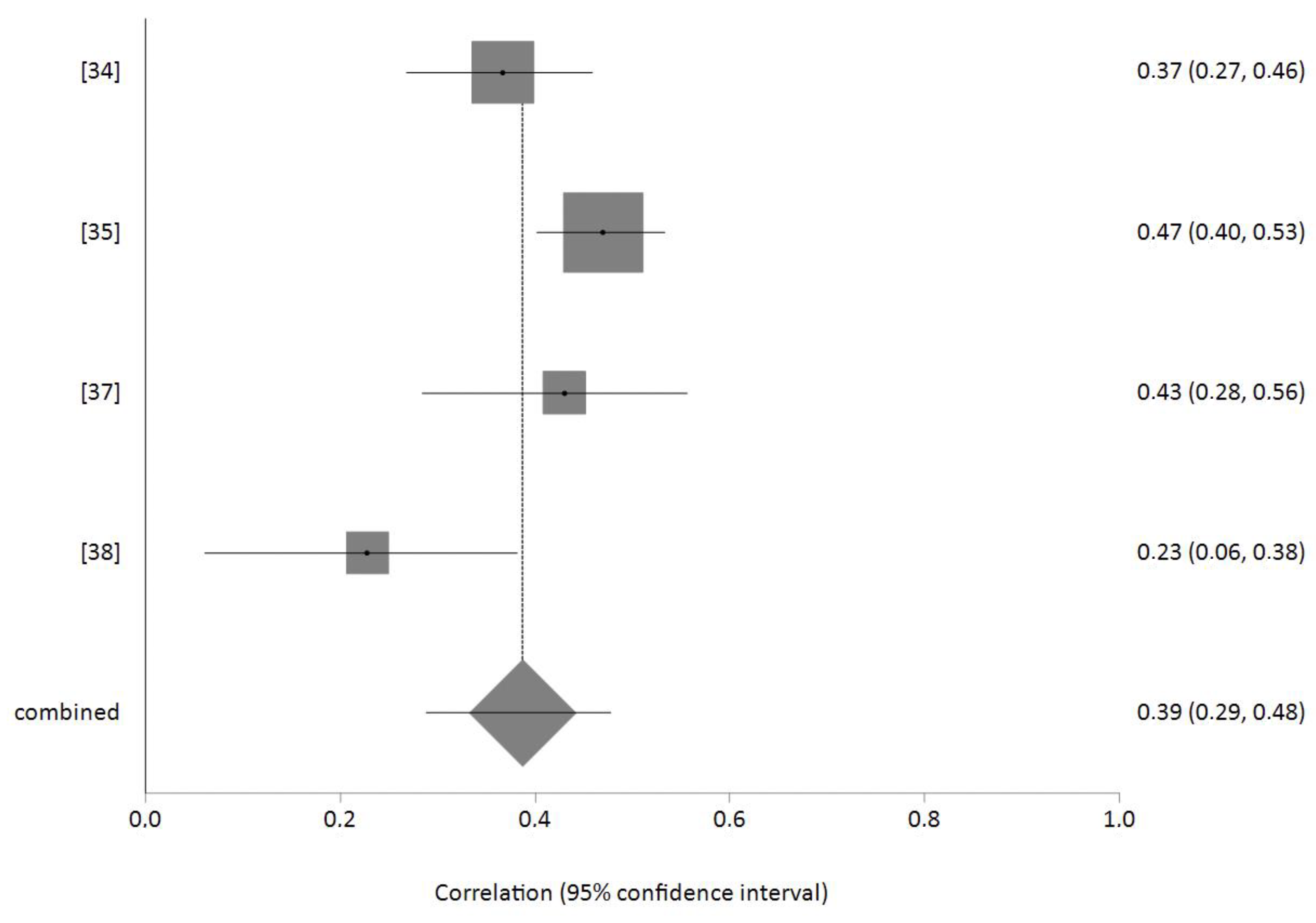
3.8. Meta-Analysis of the Relationship between Burnout and Sleep Problems
4. Discussion
Implications for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bradley, H.B. Community-based treatment for young adult offenders. Crime Delinq. 1969, 15, 359–370. [Google Scholar] [CrossRef]
- Freudenberger, H.J. Staff burn-out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1981. [Google Scholar]
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory, 2nd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1986. [Google Scholar]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. The Maslach Burnout Inventory, 3rd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- De la Fuente, G.A.C.; Vargas, C.; San Luis, C.; García, I.; Cañadas, G.R.; de la Fuente, E.I. Risk factors and prevalence of burnout syndrome in the nursing profession. Int. J. Nurs. Stud. 2015, 52, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Molina-Praena, J.; Ramírez-Baena, L.; Gómez-Urquiza, J.L.; Cañadas, G.R.; de la Fuente, E.I.; Cañadas-De la Fuente, G.A. Levels of burnout and risk factors in medical area nurses: A meta-analytic study. Int. J. Environ. Res. 2018, 15, 2800. [Google Scholar] [CrossRef] [PubMed]
- Parada, M.E.; Moreno, R.; Mejías, M.Z.; Rivas, F.A.; Rivas, F.F.; Cerrada, S.J.; Rivas, P.F. Job satisfaction and burnout syndrome in the nursing staff of the Instituto Autónomo Hospital Universitario Los Andes, Mérida, Venezuela. Rev. Fac. Nac. 2005, 23, 33–45. [Google Scholar]
- Gómez-Urquiza, J.L.; Monsalve-Reyes, C.S.; San Luis-Costas, C.; Fernández-Castillo, R.; Aguayo-Estremera, R.; Cañadas-de la Fuente, G.A. Factores de riesgo y niveles de burnout en enfermeras de atención primaria: Una revisión sistemática. Aten. Primaria 2017, 49, 77–85. [Google Scholar] [CrossRef]
- Gallagher, R.M.; Gormley, D.K. Perceptions of stress, burnout, and support systems in pediatric bone marrow transplantation nursing. Clin. J. Oncol. Nurs. 2009, 13, 681–685. [Google Scholar] [CrossRef]
- Karasek, R.; Theorell, T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life; Basic Books: New York, NY, USA, 1990. [Google Scholar]
- Adriaenssens, J.; Hamelink, A.; van Bogaert, P. Predictors of occupational stress and well-being in first-line nurse managers: A cross-sectional survey study. Int. J. Nurs. Stud. 2017, 73, 85–92. [Google Scholar] [CrossRef]
- Hsieh, M.L.; Li, Y.M.; Chang, E.T.; Lai, H.L.; Wang, W.H.; Wang, S.C. Sleep disorder in Taiwanese nurses: A random sample survey. Nurs. Health Sci. 2011, 13, 468–474. [Google Scholar] [CrossRef]
- Huang, C.L.C.; Wu, M.P.; Ho, C.; Wang, J.J. Risks of treated anxiety, depression, and insomnia among nurses: A nationwide longitudinal cohort study. PLoS ONE 2018, 13, e0204224. [Google Scholar] [CrossRef]
- Yazdanshenas, M.; Kavian, M.; Ahmadloo, M.; Jarchi, A.; Golchin, S.; Latifi, S.; Hossein, S.A.; Ghajarzadeh, M. The association between life satisfaction and the extent of depression, anxiety and stress among Iranian nurses: A multicenter survey. Iran J. Psychiatry 2016, 11, 120–127. [Google Scholar]
- Jacobsen, H.B.; Reme, S.E.; Sembajwe, G.; Hopcia, K.; Stoddard, A.M.; Kenwood, C.; Buxton, O.M. Work- family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace Health Saf. 2014, 62, 282–291. [Google Scholar]
- Geiger-Brown, J.; Rogers, V.E.; Trinkoff, A.M.; Kane, R.L.; Bausell, R.B.; Scharf, S.M. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol. Int. 2012, 29, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Sarrais, F.; de Castro, P. El insomnio. An. Sist. Sanit. Navar. 2007, 30, 121–134. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, A.M.; Vega-Escaño, J. Abordaje del insomnio en salud laboral. Enferm. Trab. 2019, 9, 11–20. [Google Scholar]
- Stewart, N.H.; Arora, V.M. The impact of sleep and circadian disorders on physician burnout. Chest 2019, 156, 1022–1030. [Google Scholar] [CrossRef]
- Bautista, S.; Balanza, J.; Torres, L. Trastornos del Sueño. In Guía de Manejo de los Trastornos Mentales; Chamorro, L., Ed.; Ars Medica: Barcelona, Spain, 2004; pp. 141–158. [Google Scholar]
- Kemper, K.J.; Mo, X.; Khayat, R. Are mindfulness and self-compassion associated with sleep and resilience in health professionals? J. Altern. Complement. Med. 2015, 21, 496–503. [Google Scholar] [CrossRef]
- Zhang, Y.; Duffy, J.F.; Ronan, E. Do sleep disturbances mediate the association between work-family conflict and depressive symptoms among nurses? A cross-sectional study. J. Psychiatr. Ment. Health Nurs. 2017, 24, 620–628. [Google Scholar] [CrossRef]
- Eanes, L. CE: The potential effects of sleep loss on a nurse’s health. Am. J. Nurs. Sci. 2015, 115, 34–40. [Google Scholar] [CrossRef]
- Zhang, C.; Tait, C.; Minacapelli, C.D.; Bhurwal, A.; Gupta, K.; Amin, R.; Rustgi, V.K. The role of race, sex and age in circadian disruption and metabolic disorders. Gastro Hep Adv. 2022, 1, 471–479. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, 105906. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, 160. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Iniciative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- des Jarlais, D.C.; Lyles, C.; Crepaz, N. Trend Group: Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. Am. J. Public. Health 2004, 94, 361–366. [Google Scholar] [CrossRef]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. Explanation of the 2011 Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence (Background Document). Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 30 October 2021).
- Ekstedt, M.; Söderström, M.; Akerstedt, T. Sleep physiology in recovery from burnout. Biol. Psychol. 2009, 82, 267–273. [Google Scholar] [CrossRef]
- Morimoto, H.; Tanaka, H.; Ohkubo, R.; Mimura, M.; Ooe, N.; Ichikawa, A.; Yukitoshi, H. Self-help therapy for sleep problems in hospital nurses in Japan: A controlled pilot study. Sleep Biol. Rhythm. 2015, 14, 177–185. [Google Scholar] [CrossRef][Green Version]
- Bagheri, M.; Ebrahimi, M.H.; Khanjani, N.; Biganeh, J.; Mohammadi, S.; Abdolahfard, M. The effects of amplitude and stability of circadian rhythm and occupational stress on burnout syndrome and job dissatisfaction among irregular shift working nurses. J. Clin. Nurs. 2019, 28, 1868–1878. [Google Scholar] [CrossRef]
- Giorgi, F.; Mattei, A.; Notarnicola, I.; Petrucci, C.; Lancia, L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. J. Adv. Nurs. 2018, 74, 698–708. [Google Scholar] [CrossRef]
- Havaei, F.; Astivia, O.L.; MacPhee, M. The impact of workplace violence on medical-surgical nurses’ health outcome: A moderated mediation model of work environment conditions and burnout using secondary data. Int. J. Nurs. Stud. 2020, 109, 103666. [Google Scholar] [CrossRef]
- Iskera-Golec, I.; Folkard, S.; Marek, T.; Noworol, C. Health, well-being and burnout of ICU nurses on 12- and 8-h shifts. Work Stress 1996, 10, 251–256. [Google Scholar] [CrossRef]
- Kim, S.J.; Na, H. A study of the relationships between compassion fatigue, compassion satisfaction, depression, anxiety, and sleep disorders among oncology nurses. Asian Oncol. Nurs. 2017, 2, 116–123. [Google Scholar] [CrossRef]
- Lu, J.L. Multiple interactions of hazard exposures, role stressors and situational factors, and burnout among nurses. Int. J. Occup. Saf. Ergon. 2007, 13, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Casbas, M.T.; Alonso-Poncelas, E.; Gómez-García, T.; Martínez-Madrid, M.J.; Escobar-Aguilar, G. Percepción sobre la calidad de los cuidados, entorno laboral y características del sueño de las enfermeras que trabajan en el Sistema Nacional de Salud. Enferm. Clin. 2018, 28, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Schult, T.M.; Mohr, D.C.; Osatuke, K. Examining burnout profiles in relation to health and well-being in the Veterans Health Administration employee population. Stress Health 2018, 34, 490–499. [Google Scholar] [CrossRef]
- Wilson, W.; Raj, J.P.; Narayan, G.; Ghiya, M.; Murty, S.; Joseph, B. Quantifying Burnout among Emergency Medicine Professionals. J. Emerg. Trauma Shock 2017, 10, 199–204. [Google Scholar] [CrossRef]
- Zencirci, A.D.; Arslan, S. Morning-evening type and burnout level as factors influencing sleep quality of shift nurses: A questionnaire study. Croat. Med. J. 2011, 52, 527–537. [Google Scholar] [CrossRef]
- Alba-Martín, R. Burnout in nursing: Prevalence and related factors in a hospital environment. Rev. Cient. Soc. Esp. Enferm. Neurol. 2015, 41, 9–14. [Google Scholar]
- Blanca-Gutiérrez, J.J.; Arias-Herrera, A. Síndrome de burnout en personal de enfermería: Asociación con estresores del entorno hospitalario, Andalucía, España. Enferm. Univ. 2018, 15, 30–44. [Google Scholar] [CrossRef]
- Gómez, M.C.; Álamo, M.C.; Amador, M.; Ceacero, F.; Mayor, A.; Muñoz, A.; Izquierdo, M. Estudio de seguimiento del desgaste profesional en relación con factores organizativos en el personal de enfermería de medicina interna. Med. Segur. Trab. 2009, 55, 52–62. [Google Scholar]
- Paris, L. Estrategias de afrontamiento del estrés asistencial y satisfacción laboral-personal en médicos y enfermeros. Rev. Interam. Psicol. Ocup. 2007, 26, 7–21. [Google Scholar]
- Camerino, D.; Sandri, M.; Sartori, S.; Conway, P.M.; Campanini, P.; Costa, G. Shiftwork, work-family conflict among italian nurses and prevention efficacy. Chronobiol. Int. 2010, 27, 1105–1123. [Google Scholar] [CrossRef] [PubMed]
- Estryn-Behar, M.; Fry, C.; Guetarni, K.; Machet, G.; Doppia, M.A.; Lassaunière, J.M.; Muster, D.; Pelloux, P.; Prudhomme, C. Work week duration, work-family balance and difficulties encountered by female and male physicians: Results from the French SESMAT study. Work 2011, 40, 83–100. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, A.M.; Awadalla, N.J.; Alsaleem, S.A.; Alsamghan, A.S.; Alsaleem, M.A. Burnout syndrome among emergency physicians and nurses in Abha and Khamis Mushait Cities, Aseer Region, Southwestern Saudi Arabia. Sci. World J. 2019, 2019, 4515972. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.H.; Jiang, C.Q.; Lam, T.H. The relationship between occupational stress, burnout, and turnover intention among managerial staff from a Sino-Japanese joint venture in Guangzhou. J. Occup. Health 2013, 55, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Ríos, M.I.; Godoy, C.; Peñalver, F.; Alonso, A.R.; López, F.; López, A.; Garnés, S.; Salmerón, E.; López, M.D.; Ruiz, R.; et al. Estudio comparativo del burnout en personal de enfermería de Cuidados Intensivos y Urgencias. Enferm. Intensiva 2008, 19, 2–13. [Google Scholar] [CrossRef]
- Nogareda, C.; Nogareda, S. NTP 455. Trabajo a Turnos y Nocturnos: Aspectos Organizativos [Ministerio de Trabajo y Asuntos Sociales, España Web Site]. Available online: https://www.insst.es/documents///ntp_455.pdf/–21f3–419a-b356–1f2ddb9e2766 (accessed on 20 October 2021).
- Cañadas-de la Fuente, G.A.; Albendín-García, L.; de la Fuente, E.I.; San Luis, C.; Gómez-Urquiza, J.L.; Cañadas, G.R. Síndrome de burnout en profesionales de enfermería que realizan jornada física complementaria en servicios de cuidados críticos y urgencias. Rev. Esp. Salud Publica 2016, 90, e1–e9. [Google Scholar] [PubMed]
- Bonet-Porqueras, R.; Moliné-Pallarés, A.; Olona-Cabases, M.; Gil-Mateu, E.; Bonet-Notario, P.; Les-Morell, E.; Iza-Maiza, M.; Bonet-Porqueras, M. Turno nocturno: Un factor de riesgo en la salud y calidad de vida del personal de enfermería. Enferm. Clin. 2009, 19, 76–82. [Google Scholar] [CrossRef]
- García, A. Enfermería y turno de noche: Trabajar contra corriente. Inferm. Ponent 2003, 8, 1–7. [Google Scholar]
- Chiu, H.Y.; Tsai, P.S. The impact of various work schedules on sleep complaints and minor accidents during work or leisure time: Evidence from a national survey. J. Occup. Environ. Med. 2013, 55, 325–330. [Google Scholar] [CrossRef]
- Deschamps, A.; Olivares, S.B.; de la Rosa, K.L.; Asunsolo, A. Influencia de los turnos de trabajo y las guardias nocturnas en la aparición del Síndrome de Burnout en médicos y enfermeras. Med. Segur. Trab. 2011, 57, 224–241. [Google Scholar] [CrossRef][Green Version]
- Palermo, T.A.C.; Rotenberg, L.; Zeitoune, R.C.G.; Silva-Costa, A.; Souto, E.P.; Griep, R.H. Siesta durante la guardia nocturna y la recuperación tras el trabajo entre enfermeros de hospitales. Rev. Lat. Am. Enferm. 2015, 23, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Poursadeghiyan, M.; Moghimian, M.; Nabiamjad, R.; Baneshi, M.M.; Yari, A.; Noroozi, M.; Hami, M.; Khammar, A.; Farrokhi, M. Effects on job stress on Iranian clinical nurses. Ann. Trop. Med. Public Health 2017, 10, 985–988. [Google Scholar] [CrossRef]
- Adriaenssens, J.; de Gucht, V.; Maes, S. The impact of traumatic events on emergency room nurses: Findings from a questionnaire survey. Int. J. Nurs. Stud. 2012, 49, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Roche, M.A.; Diers, D.; Duffield, C.; Catling-Paull, C. Violence toward nurses, the work environment, and patient outcomes. J. Nurs. Scholarsh. 2010, 42, 13–22. [Google Scholar] [CrossRef]
- Díaz-Ramiro, E.M.; Rubio-Valdehita, S.; López-Núñez, M.I.; Aparicio-García, M.E. Los hábitos de sueño como predictores de la salud psicológica en profesionales sanitarios. An. Psicol. 2020, 36, 242–246. [Google Scholar] [CrossRef]
- de la Fuente-Solana, E.I.; Gómez-Urquiza, J.L.; Cañadas, G.R.; Albendín-García, L.; Ortega-Campos, E.; Cañadas-de la Fuente, G.A. Burnout and its relationship with personality factors in oncology nurses. Eur. J. Oncol. Nurs. 2017, 30, 91–96. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Funderburk, J.; Bishop, T.M.; Crean, H.F. Brief cognitive behavioral therapy for insomnia delivered to depressed veterans receiving primary care services: A pilot study. J. Affect. Disord. 2017, 217, 105–111. [Google Scholar] [CrossRef]
- Huang, C.Y.; Chang, E.T.; Lai, H.L. Comparing the effects of music and exercise with music for older adults with insomnia. Appl. Nurs. Res. 2016, 32, 104–110. [Google Scholar] [CrossRef]
- Shatté, A.; Perlman, A.; Smith, B.; Lynch, W.D. The positive effect of resilience on stress and business outcomes in difficult work environments. J. Occup. Environ. Med. 2017, 59, 135–140. [Google Scholar] [CrossRef]

| Author, Publication Year, Country | Study Type | Sample (n) | Instrument for Burnout Measurement and Sleep Disturbance | Aim | Mean ± SD | Main Results | LE/GR |
|---|---|---|---|---|---|---|---|
| Bagheri et al. [33] Iran | Cross-sectional | n = 684 Female 575 (84%) Age group 30–40: 285 (41%) | MBI CTI | To investigate the relation between the circadian rhythm amplitude and stability, and occupational stress with Burnout Syndrome and Job Dissatisfaction among shift working nurses. | Circadian rhythm Amplitude: Vigorous: 513 (75.2%) Languid: 169 (24.8%) Stability: Rigid 523 (76.7%) Flexible 159 (23.3%) MBI (Low/moderate/high) EE: 178 (26.1%)/240 (35.2%)/264 (38.7%) DE 308 (45.1%)/167 (24.5%)/207 (30.4%) PA 345 (50.6%)/169 (24.8%)/168 (24.6%) Global: 43 (6.3%)/542 (79.5%)/97 (14.2%) |
About 15% of the nurses suffered from high levels of burnout syndrome. Psychological demand and workplace support were significant predictors of BS and JD. Male nurses reported lower BS and higher JD. Irregular shift working schedule was also related to significantly higher odds of BS and JD. Nurses classified as languid experienced significantly more BS and JD than vigorous nurses. | 2 b/B |
| Ekstedt et al. [31] Norway | Quasi-experimental | n = 39 CG: n = 16 12 women, Mean age 43 IG: n = 23 16 women, Mean age 44 | SMBQ SQI | To investigate the role of sleep physiology in recovery from burnout. Intervention: IG underwent a multi-modal rehabilitation program, based on accepted Cognitive Behavioral Therapeutic methods with the aim of reducing stress. | SMBQ (l–7 = high) (Mean ± SD) Baseline CG: 1.7 ± 0.2 IG: 5.7 ± 0.2 Follow up CG: 1.8 ± 0.3 IG: 3.5 ± 0.3 SQI (l–6 = good) (Mean ± SD) Baseline CG: 5.0 ± 0.1 IG: 2.8 ± 0.2 Follow-up CG: 4.9 ± 0.1 IG: 4.3 ± 0.1 | The intervention resulted in a strong improvement of sleep physiology, with recovery from burnout and a relation between improved sleep and a reduction in fatigue. It is suggested that impaired sleep continuity may be part of the fatigue component of burnout. | 2 a/B |
| Giorgi et al. [34] Italy | Cross-sectional | n = 315 Female 67% Age group 41–50: 48% | CBI PSQI | To investigate the relationship between sleep disorders, burnout and job performance in a shift-work population of nurses. | Impaired sleep quality 164 nurses (52.1%) Presence of burnout: 99 nurses (31.4%) | Female gender and personal burn- out were significantly associated with impaired sleep quality, and there was a significant linear association between the quality of sleep and burnout (q = 0.367; p < 0.001). Sleep disturbance, daytime dysfunction and subjective sleep quality showed a significant positive correlation with the mean values of the total burnout score and its relative dimensions and was predominantly correlated with personal burnout. | 2 b/B |
| Havaei et al. [35] Canada | Cross-sectional | n = 537 Female n = 506 (95%) Mean age 39 | MBI-HSS CCHS | To examine whether work environment conditions moderate the mediating effect that burnout has on the relationship between workplace violence and musculoskeletal injuries, sleep disturbances/insomnia and anxiety disorders. | Mean sleep disturbances/insomnia (Range 0–6) 3.3 ± 1.9 EE (range punctuation 0–54) 28.2 ± 13.3 | Burnout mediated the relationship between workplace violence and sleep. In healthier work environments, workplace violence was more strongly related to increased reports of burnout and sleep disturbances compared to less healthy work environments. | 2 b/B |
| Iskera-Golec et al. [36] Poland | Cross-sectional | n = 126 Group of nurses 12 h shift: n = 96 Mean age: 25 Group of nurses 8 h shift: n = 30 Mean age 26 | MBI ESS PSQI | To compare measures of health, sleep, psychological and social wellbeing, job satisfaction and burnout of ICU nurses on 12-h and 8-h shifts. | MBI dimensions 8 h/12 h shifts EE (0–54 punctuation): 16.80/21.37 DE (0–30 punctuation): 9.27/7.43 PA (0–48 punctuation): 31.00/28.39 Sleep measures 8 h/12 h shifts General sleep disturbance (4–20 punctuation): 10.00/12.50 Tired after sleep (4–20 punctuation) 11.38/13.36 Premature awakening (4–20 punctuation) 10.33/9.28 Difficulties in falling asleep (4–20 punctuation): 9.35/8.72 Average length of sleep (h): 5.43/6.11 Ratio of average length of sleep to length of sleep declared as sufficient: 0.62/0.84 | The 12 h shift nurses showed worse indices of health, well-being and burnout than the 8 h shift nurses. It is suggested that this may be associated with their longer daily exposure to the stress of work. | 2 b/B |
| Kim & Na [37] Korea | Cross sectional | n = 140 Female 100% Mean age 30 | ProQOL PSQI | To identify the relationships between various factors, including compassion, fatigue, satisfaction, depression, anxiety and sleep disorders among oncology nurses. | Burnout (mean ± SD) (range 10–50) 30.53 ± 4.69 High group (range 56 ≤ T) 35 (25.0%) Medium group (44 ≤ T < 56) 73 (52.1%) Low group (T < 44) 32 (22.9%) Sleep disorder (range 0–21) 9.66 ± 3.18 |
Compassion fatigue is composed of secondary traumatic stress and burnout. The levels of compassion fatigue showed significant positive correlations with depression, anxiety and sleep disorder. | 2 b/B |
| Lu [38] Philippines | Cross-sectional | n = 135 Female 77% Mean Age 32 | MBI Questionnaire Data Health and Illness | To explore the interaction between situational factors (the role stressors, hazard exposure and personal factors) and development of burnout. | Sleep disturbances: 57 subjects (42.2%) experienced once a day. Spearman correlations between sleep disorder and burnout was 0.228, p = 0.08 | Regression showed factors associated with burnout were organizational role stress, hazard exposure, self-efficacy, age, number of working years, illness in the past 12 months, migraine, dizziness, sleep disorder, cough and colds, and diarrhea. | 2 b/B |
| Moreno-Casbas et al. [39] Spain | A multicenter, observational, and descriptive study | n = 635 Female: 551 (87%) Mean age: 41 | MBI MEQ ESS PSQI | To describe nurses’ perception in relation to the quality of care and their work environment. To explore nurses’ quality of sleep. To analyze the relationship between ward and work shift with nurses’ perception of their work environment, sleep quality and daytime drowsiness. | Burnout: High level, 86 nurses (15.4%) Low level 326 nurses 58.3% MBI scale high levels: EE 107 (17.8%) PA 148 (25%) DE 110 (18.4%) Epworth Scale: Excessive sleepiness 311(51.8%) Low sleepiness 166 (27.7%) Medium sleepiness 123(20.5%) PSQI (mean ± dt): Global score: 6.8 ± 3.387 Sleep quality: 1.35 ± 0.641 Sleep latency: 1.35 ± 0.957 Sleep duration: 0.76 ± 0.871 Sleep efficiency: 0.9 ± 1.026 Sleep disturbance 1.25 ± 0.481 Sleeping medication: 0.38 ± 0.827 Daytime disfunction: 0.72 ± 0.726 Sleepiness 0.72 ± 0.726 | 15.4% of the nurses had a high level of burnout, and 58.3% had low burnout. Sleep quality was 6.38 for nurses working day shifts, 6.78 for rotational shifts and 7.93 for night shifts. Significant differences were found between subjective sleep quality score, sleep duration, sleep disturbances and daytime dysfunction. | 2 b/B |
| Morimoto et al. [32] Japan | Quasi-experimental | n = 25 IG: 10 CG: 15 Female 22 (95%), Mean age 39 n = 84 (withdrew) | MBI (Japanese version) ESS (Japanese version) PSQI (Japanese version) | To examine the effectiveness of SHT in hospital nurses in Japan. Intervention: 90 min workshop covering sleep hygiene education and brief stress management. | PSQI (n = 84) Global score: 6.2 + −2.9 Sleep quality: 1.5 + −0.7 Sleep latency: 1.1 + 1.0 Sleep duration: 1.6 + −0.7 Sleep efficiency: 0.2 + −0.4 Sleep disturbance 0.7 + −0.5 Sleeping medication: 0.3 + −0.8 Daytime disfunction: 0.8 + −0.8 Sleepiness 8.8 + −4.5 MBI EE: 16.4 + 4.7 DE: 12.3 + −4.4 PA: 11.2 + −2.8 BASELINE (IG/CG) PSQI Global score: 6.5 ± 2.9/5.8 ± 3.3 Sleep quality: 1.3 ± 2.9/1.6 ± 3.3 Sleep latency: 1.5 ± 1.9/1.4 ± 2.2 Sleep duration: 1.9 ± 2.8/2.1 ± 3.3 Sleep efficiency: 0.0 ± 0.9/0.0 ± 1.1 Sleep disturbance 1.1 ± 2.4/0.9 ± 2.8 Sleeping medication: 0.0 ± 2.5/0.5 ± 3.0 Daytime disfunction: 1.1 ± 4.4/0.4 ± 5.1 Sleepiness 8.2 ± 8.9/8.9 ± 10.3 MBI EE: 15.6 ± 27.2/16.1 ± 31.7 DE: 12.6 ± 23.2/11.8 ± 27.0 PA: 14.6 ± 6.7/15.2 ± 7.8 FOLLOW UP (IG/CG) PSQI Global score: 5.3 ± 3.0/6.1 ± 3.4 Sleep quality: 1.2 ± 2.9/1.7 ± 3.3 Sleep latency: 1.3 ± 1.9/1.3 ± 2.2 Sleep duration: 1.8 ± 2.8/2.1 ± 3.3 Sleep efficiency: 0.0 ± 0.9/0.0 ± 1.1 Sleep disturbance 0.8 ± 2.4/0.8 ± 2.8 Sleeping medication: 0.0 ± 2.5/0.5 ± 3.0 Daytime disfunction: 0.7 ± 4.4/0.6 ± 5.1 Sleepiness 7.9 ± 8.9/8.1 ± 10.3 MBI EE: 15.0 ± 27.2/6.7 ± 31.7 DE: 12.7 ± 23.2/12.3 ± 27.0 PA: 13.0 ± 6.8/14.3 ± 7.8 | SHT improved subjective sleep quality (global PSQI scores). Participants with sleep problems at pre-test in the SHT group showed a significant reduction in sleep latency and sleep disturbance, which was not observed in the control group. No significant improvement was found in the SHT group for sleepiness. No significant improvement was observed in either group for depressive symptoms, burnout and quality of life. | 2 a/B |
| Schult et al. [40] USA | Cross-sectional | n = 23,339 Female: 51,312 (61%) Age group: 50–59 y.o: 31% | MBI HSS Burnout profiles All employee survey: health promotion | To provide a population overview of burnout profiles by occupation in a healthcare sector employee population and to investigate how burnout profiles relate to self-reported health behaviors and chronic conditions. | Burnout profiles Engaged 43.8% Unfulfilled 21.3% Striving/overextended 11.0% Frustrated/burning up 14.7% Withdrawing/burned out 9.2% Sleep disorders OR = 1.98; 99% CI [1.85, 2.12] | Employees in the “frustrated/burning up” and “withdrawing/burned out” profiles had significantly increased odds of sleep disorders. 9.2% of the nurses had a withdrawing/burned out profile | 2 b/B |
| Wilson et al. [41] India | Cross-sectional | n = 51 Female: 71% Mean age: 28 | MBI Disturbed sleep | To measure the degree of burnout in doctors and nurses working in the emergency medicine department of four tertiary care teaching hospitals in South India. |
Moderate–severe burnout: EE 64.8% DP 71.4% PA 73.3% Disturbed sleep 31.4% | Degree of burnout among nurses was moderately high in the three components, and some of the identified predictors were criticism, disturbed sleep, short-tempered nature, fear of committing errors and witnessing death. | 2 b/B |
| Zencirci and Arslan [42] Turkey | Cross-sectional | n = 483 Female: 100% Mean age: 30 | MBI PSQI MEQ | To assess the relationship between sleep quality and demographic variables, morning–evening type and burnout in nurses who work shifts. | Mean PSQI value of nurses was 7.32 ± 3.42 PSQI value of 79.1% (n = 382) of nurses was ≥5. High EE (p < 0.001) and DP (p < 0.001), as well as PA decreased sleep quality (p = 0.001). | Most sociodemographic variables did not affect sleep quality. Participants with poor sleep quality had high burnout levels. Most nurses who belonged to a type that is neither morning nor evening had poor sleep quality. Nurses who experienced an incident worsening their sleep patterns (p < 0.001) and needlestick or sharp object injuries (p = 0.010) in the last month had poor sleep quality. The subjective sleep quality and sleep latency points of evening types within created models for the effect of burnout dimensions were high. | 2 b/B |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Membrive-Jiménez, M.J.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Velando-Soriano, A.; Ariza, T.; De la Fuente-Solana, E.I.; Cañadas-De la Fuente, G.A. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 954. https://doi.org/10.3390/healthcare10050954
Membrive-Jiménez MJ, Gómez-Urquiza JL, Suleiman-Martos N, Velando-Soriano A, Ariza T, De la Fuente-Solana EI, Cañadas-De la Fuente GA. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare. 2022; 10(5):954. https://doi.org/10.3390/healthcare10050954
Chicago/Turabian StyleMembrive-Jiménez, María José, José Luis Gómez-Urquiza, Nora Suleiman-Martos, Almudena Velando-Soriano, Tania Ariza, Emilia Inmaculada De la Fuente-Solana, and Guillermo A. Cañadas-De la Fuente. 2022. "Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis" Healthcare 10, no. 5: 954. https://doi.org/10.3390/healthcare10050954
APA StyleMembrive-Jiménez, M. J., Gómez-Urquiza, J. L., Suleiman-Martos, N., Velando-Soriano, A., Ariza, T., De la Fuente-Solana, E. I., & Cañadas-De la Fuente, G. A. (2022). Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare, 10(5), 954. https://doi.org/10.3390/healthcare10050954










