Obstructive Sleep Apnea and Adherence to Continuous Positive Airway Pressure (CPAP) Treatment: Let’s Talk about Partners!
Abstract
1. Introduction
2. Materials and Methods
2.1. Identifying the Research Questions
- Is partner involvement effective in CPAP management of someone with OSA?
- What strategies are implemented by couples to improve quality of life?
2.2. Identifying Relevant Studies
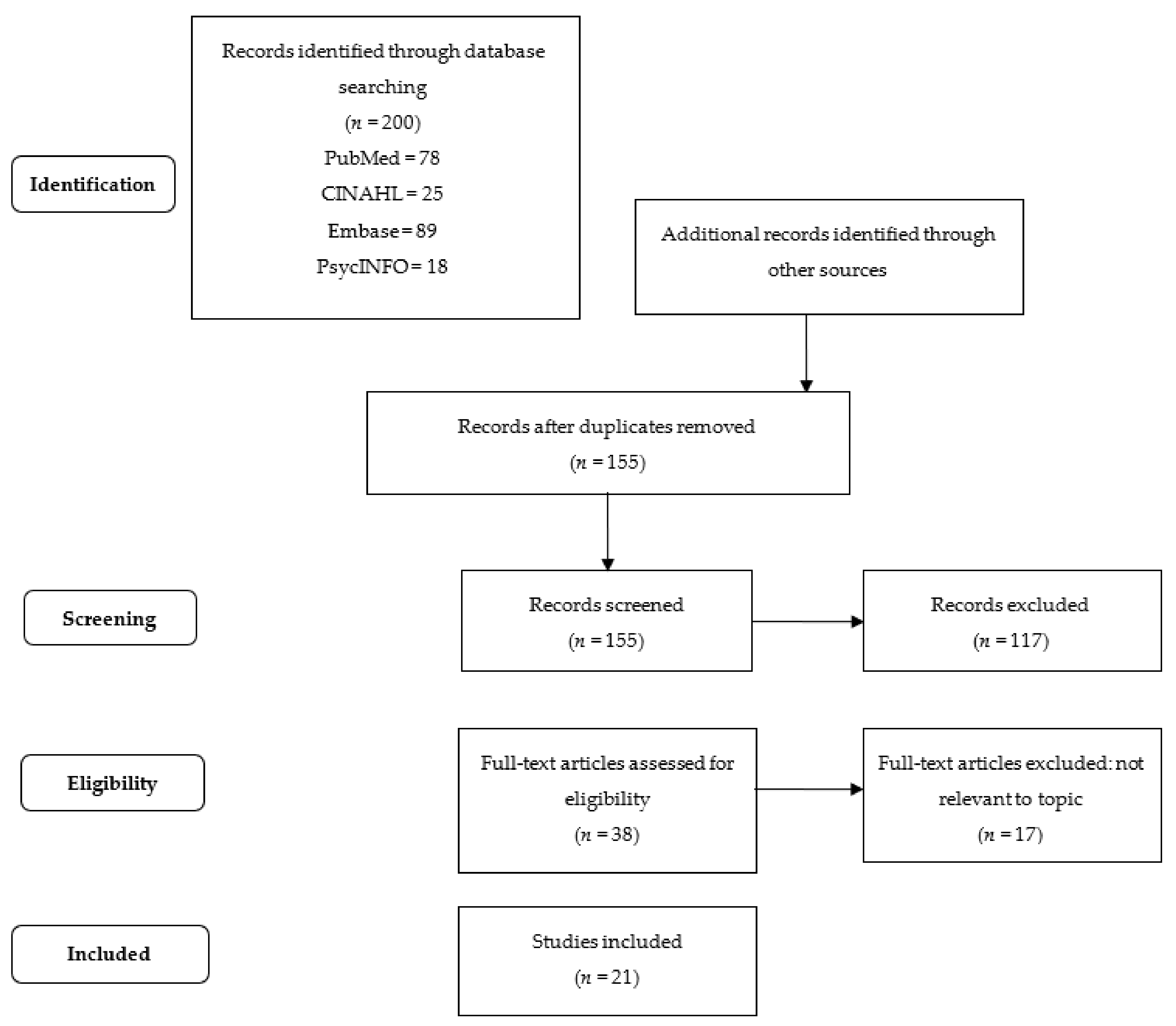
2.3. Selecting Relevant Studies
2.4. Extracting Collected Data
2.5. Reporting Results
3. Results
3.1. Partner’s Engagement
3.2. Anxiety and Depressive Symptoms
3.3. Daytime Sleepiness and Sleep Quality
3.4. Quality of Sexual Life and Marital Relationship
3.5. Encouraging Empowerment
3.6. Facilitators to CPAP Treatment
3.7. Barriers to CPAP Treatment
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Somers, V.K.; White, D.P.; Amin, R.; Abraham, W.T.; Costa, F.; Culebras, A.; Daniels, S.; Floras, J.S.; Hunt, C.E.; Olson, L.J.; et al. Sleep Apnea and Cardiovascular Disease. J. Am. Coll. Cardiol. 2008, 52, 686–717. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased Prevalence of Sleep-Disordered Breathing in Adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining Phenotypic Causes of Obstructive Sleep Apnea. Identification of Novel Therapeutic Targets. Am. J. Respir. Crit. Care Med. 2013, 188, 996–1004. [Google Scholar] [CrossRef]
- Pini, L.; Magri, R.; Perger, E.; Levi, G.; Zambelli, L.; Giordani, J.; Ciarfaglia, M.; Tantucci, C. Phenotyping OSAH patients during wakefulness. Sleep Breath. 2022. [Google Scholar] [CrossRef]
- Perger, E.; Mattaliano, P.; Lombardi, C. Menopause and Sleep Apnea. Maturitas 2019, 124, 35–38. [Google Scholar] [CrossRef]
- Kirkness, J.P. Obesity-related Ventilatory Phenotypes of Sleep-disordered Breathing. Am. J. Respir. Crit. Care Med. 2014, 190, 853–854. [Google Scholar] [CrossRef]
- Edwards, B.A.; Wellman, A.; Sands, S.A.; Owens, R.L.; Eckert, D.J.; White, D.P.; Malhotra, A. Obstructive Sleep Apnea in Older Adults is a Distinctly Different Physiological Phenotype. Sleep 2014, 37, 1227–1236A. [Google Scholar] [CrossRef]
- Lin, C.H.; Perger, E.; Lyons, O.D. Obstructive sleep apnea and chronic kidney disease. Curr. Opin. Pulm. Med. 2018, 24, 549–554. [Google Scholar] [CrossRef]
- Lyons, O.D.; Inami, T.; Perger, E.; Yadollahi, A.; Chan, C.T.; Bradley, T.D. The effect of fluid overload on sleep apnoea severity in haemodialysis patients. Eur. Respir. J. 2017, 49, 1601789. [Google Scholar] [CrossRef]
- Perger, E.; Blaise, S.; Vermorel, C.; Boge, G.; Pepin, J.L.; Redolfi, S.; Bosson, J.L. Subjects with venous insufficiency have high risk of obstructive sleep apnea in relationship to fluid shift. Sleep Med. 2020, 72, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Arredondo, E.; Udeani, G.; Panahi, L.; Taweesedt, P.T.; Surani, S. Obstructive Sleep Apnea in Adults: What Primary Care Physicians Need to Know. Medicina 2022, 33, e17843. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Kang, R.; Zhao, S.; Zhang, T.; Zhu, W.; Li, E.; Li, F.; Wan, S.; Zhao, Z. Sexual Dysfunction in Patients with Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. J. Sex. Med. 2015, 12, 1992–2003. [Google Scholar] [CrossRef] [PubMed]
- Perger, E.; Soranna, D.; Pengo, M.; Meriggi, P.; Lombardi, C.; Parati, G. Sleep-disordered Breathing among Hospitalized Patients with COVID-19. Am. J. Respir. Crit. Care Med. 2021, 203, 239–241. [Google Scholar] [CrossRef] [PubMed]
- Hoyos, C.M.; Drager, L.F.; Patel, S.R. OSA and cardiometabolic risk: What’s the bottom line? Respirology 2017, 22, 420–429. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Punjabi, N.M. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 2020, 323, 1389–1400. [Google Scholar] [CrossRef]
- Pavwoski, P.; Shelgikar, A.V. Treatment options for obstructive sleep apnea. Neurol. Clin. Pract. 2017, 7, 77–85. [Google Scholar] [CrossRef]
- Perger, E.; Jutant, E.M.; Redolfi, S. Targeting volume overload and overnight rostral fluid shift: A new perspective to treat sleep apnea. Sleep Med. Rev. 2018, 42, 160–170. [Google Scholar] [CrossRef]
- Perger, E.; Taranto-Montemurro, L. Upper airway muscles: Influence on obstructive sleep apnoea pathophysiology and pharmacological and technical treatment options. Curr. Opin. Pulm. Med. 2021, 27, 505–513. [Google Scholar] [CrossRef]
- Taranto-Montemurro, L.; Messineo, L.; Sands, S.A.; Azarbarzin, A.; Marques, M.; Edwards, B.A.; Eckert, D.J.; White, D.P.; Wellman, A. Targeting Endotypic Traits with Medications for the Pharmacological Treatment of Obstructive Sleep Apnea. A Review of the Current Literature. J. Clin. Med. 2019, 8, 1846. [Google Scholar] [CrossRef]
- Perger, E.; Montemurro, L.T.; Rosa, D.; Vicini, S.; Marconi, M.; Zanotti, L.; Meriggi, P.; Azarbarzin, A.; Sands, S.A.; Wellman, A.; et al. Reboxetine plus Oxybutynin for Obstructed Sleep Apnea Treatment A 1-week Randomized, Placebo-controlled, Double-Blind Crossover Trial. Chest 2022, 1, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Taranto-Montemurro, L.; Messineo, L.; Sands, S.A.; Azarbarzin, A.; Marques, M.; Edwards, B.A.; Eckert, D.J.; White, D.P.; Wellman, A. The Combination of Atomoxetine and Oxybutynin Greatly Reduces Obstructive Sleep Apnea Severity. A Randomized, Placebo-controlled, Double-Blind Crossover Trial. Am. J. Respir. Crit. Care Med. 2019, 199, 1267–1276. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.N.S.; Olomu, A.B.; Bottu, S.; Roller, M.R.; Smith, R.C. Semistructured Motivational Interviews of Patients and Caregivers to Improve CPAP Adherence: A Qualitative Analysis. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2019, 15, 1721–1730. [Google Scholar] [CrossRef]
- Collen, J.; Lettieri, C.; Kelly, W.; Roop, S. Clinical and Polysomnographic Predictors of Short-Term Continuous Positive Airway Pressure Compliance. Chest 2009, 135, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Budhiraja, R.; Parthasarathy, S.; Drake, C.L.; Roth, T.; Sharief, I.; Budhiraja, P.; Saunders, V.; Hudgel, D.W. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep 2007, 30, 320–324. [Google Scholar] [PubMed]
- Weaver, T.E.; Sawyer, A.M. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: Implications for future interventions. Indian J. Med. Res. 2010, 131, 245–258. [Google Scholar]
- Weaver, T.E.; Maislin, G.; Dinges, D.F.; Bloxham, T.; George, C.F.P.; Greenberg, H.; Kader, G.; Mahowald, M.; Younger, J.; Pack, A.I. Relationship Between Hours of CPAP Use and Achieving Normal Levels of Sleepiness and Daily Functioning. Sleep 2007, 30, 711–719. [Google Scholar] [CrossRef]
- Gagnadoux, F.; Vaillant, M.; Goupil, F.; Pigeanne, T.; Chollet, S.; Masson, P.; Humeau, M.P.; Bizieux-Thaminy, A.; Meslier, N. Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS ONE 2011, 6, e22503. [Google Scholar] [CrossRef]
- Luyster, F.S.; Aloia, M.S.; Buysse, D.J.; Dunbar-Jacob, J.; Martire, L.M.; Sereika, S.M.; Strollo, P.J. A Couples-Oriented Intervention for Positive Airway Pressure Therapy Adherence: A Pilot Study of Obstructive Sleep Apnea Patients and Their Partners. Behav. Sleep Med. 2019, 17, 561–572. [Google Scholar] [CrossRef]
- Phillips, C.L.; Grunstein, R.R.; Darendeliler, M.A.; Mihailidou, A.S.; Srinivasan, V.K.; Yee, B.J.; Marks, G.B.; Cistulli, P.A. Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2013, 187, 879–887. [Google Scholar] [CrossRef]
- Lynch, S.; Blase, A.; Wimms, A.; Erikli, L.; Benjafield, A.; Kelly, C.; Willes, L. Retrospective descriptive study of CPAP adherence associated with use of the ResMed myAir application; ResMed Ltd.: Sydney, Australia, 2015; Volume 10, pp. 1–6. [Google Scholar]
- Chou, M.S.H.; Ting, N.C.H.; El-Turk, N.; Harrington, Z.; Dobler, C.C. Treatment burden experienced by patients with obstructive sleep apnoea using continuous positive airway pressure therapy. PLoS ONE 2021, 16, e0252915. [Google Scholar] [CrossRef] [PubMed]
- Labarca, G.; Schmidt, A.; Dreyse, J.; Jorquera, J.; Barbe, F. Telemedicine interventions for CPAP adherence in obstructive sleep apnea patients: Systematic review and meta-analysis. Sleep Med. Rev. 2021, 60, 101543. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Giron, M.; Bonsignore, M.R.; Montserrat, J.M. New organisation for follow-up and assessment of treatment efficacy in sleep apnoea. Eur. Respir. Rev. an Off. J. Eur. Respir. Soc. 2019, 28, 190059. [Google Scholar] [CrossRef] [PubMed]
- Rapelli, G.; Pietrabissa, G.; Manzoni, G.M.; Bastoni, I.; Scarpina, F.; Tovaglieri, I.; Perger, E.; Garbarino, S.; Fanari, P.; Lombardi, C.; et al. Improving CPAP Adherence in Adults with Obstructive Sleep Apnea Syndrome: A Scoping Review of Motivational Interventions. Front. Psychol. 2021, 12, 705364. [Google Scholar] [CrossRef]
- Ye, L.; Antonelli, M.T.; Willis, D.G.; Kayser, K.; Malhotra, A.; Patel, S.R. Couples’ experiences with continuous positive airway pressure treatment: A dyadic perspective. Sleep Health 2017, 3, 362–367. [Google Scholar] [CrossRef]
- Luyster, F.S. Impact of Obstructive Sleep Apnea and Its Treatments on Partners: A Literature Review. J. Clin. Sleep Med. 2017, 13, 467–477. [Google Scholar] [CrossRef]
- Luyster, F.S.; Dunbar-Jacob, J.; Aloia, M.S.; Martire, L.M.; Buysse, D.J.; Strollo, P.J. Patient and Partner Experiences with Obstructive Sleep Apnea and CPAP Treatment: A Qualitative Analysis. Behav. Sleep Med. 2016, 14, 67–84. [Google Scholar] [CrossRef]
- Pucciarelli, G.; Buck, H.G.; Barbaranelli, C.; Savini, S.; Simeone, S.; Juarez-Vela, R.; Alvaro, R.; Vellone, E. Psychometric Characteristics of the Mutuality Scale in Stroke Patients and Caregivers. Gerontologist 2016, 56, e89–e98. [Google Scholar] [CrossRef]
- Dellafiore, F.; Buck, H.G.; Pucciarelli, G.; Barbaranelli, C.; Paturzo, M.; Alvaro, R.; Vellone, E. Psychometric characteristics of the mutuality scale in heart failure patients and caregivers. Heart Lung. 2018, 47, 553–561. [Google Scholar] [CrossRef]
- Dellafiore, F.; Rosa, D.; Pittella, F.; Caruso, M.P.; Allemano, M.; Caruso, R. The impact of type 2 diabetes diagnosis on married couples. J. Diabetes Nurs. 2018, 22, 1–5. [Google Scholar]
- Cilluffo, S.; Bassola, B.; Lusignani, M. Mutuality in Motor Neuron Disease: A Mixed-Method Study. J. Neurosci. Nurs. J. Am. Assoc. Neurosci. Nurses. 2021, 53, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Villa, G.; Mannarini, M.; Della Giovanna, G.; Marzo, E.; Manara, D.F.; Vellone, E. A literature review about self-care on ostomy patients and their caregivers. Int. J. Urol. Nurs. 2019, 13, 75–80. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Baron, K.G.; Smith, T.W.; Berg, C.A.; Czajkowski, L.A.; Gunn, H.; Jones, C.R. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep Breath. 2011, 15, 525–534. [Google Scholar] [CrossRef]
- Petersen, M.; Kristensen, E.; Berg, S.; Giraldi, A.; Midgren, B. Sexual Function in Female Patients with Obstructive Sleep Apnea. J. Sex. Med. 2011, 8, 2560–2568. [Google Scholar] [CrossRef]
- Baron, K.G.; Gunn, H.E.; Czajkowski, L.A.; Smith, T.W.; Jones, C.R. Spousal involvement in CPAP: Does pressure help? J. Clin. Sleep Med. 2012, 8, 147–153. [Google Scholar] [CrossRef][Green Version]
- Elfström, M.; Karlsson, S.; Nilsen, P.; Fridlund, B.; Svanborg, E.; Broström, A. Decisive situations affecting partners’ support to continuous positive airway pressure-treated patients with obstructive sleep apnea syndrome: A critical incident technique analysis of the initial treatment phase. J. Cardiovasc. Nurs. 2012, 27, 228–239. [Google Scholar] [CrossRef]
- Henry, D.; Rosenthal, L. “Listening for his breath:” The significance of gender and partner reporting on the diagnosis, management, and treatment of obstructive sleep apnea. Soc. Sci. Med. 2013, 79, 48–56. [Google Scholar] [CrossRef]
- Petersen, M.; Kristensen, E.; Berg, S.; Midgren, B. Sexual function in male patients with obstructive sleep apnoea after 1 year of CPAP treatment. Clin. Respir. J. 2013, 7, 214–219. [Google Scholar] [CrossRef]
- Acar, M.; Kaya, C.; Catli, T.; Hancı, D.; Bolluk, O.; Aydin, Y. Effects of nasal continuous positive airway pressure therapy on partners’ sexual lives. Eur. Arch. Otorhinolaryngol. 2016, 273, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Baron, K.G.; Gunn, H.E.; Wolfe, L.F.; Zee, P.C. Relationships and CPAP adherence among women with obstructive sleep apnea. Sleep Sci. Pract. 2017, 1, 22. [Google Scholar] [CrossRef]
- Tramonti, F.; Maestri, M.; Carnicelli, L.; Fava, G.; Lombardi, V.; Rossi, M.; Fabbrini, M.; Di Coscio, E.; Iacopini, E.; Bonanni, E. Relationship quality of persons with obstructive sleep Apnoea syndrome. Psychol. Health Med. 2017, 22, 896–901. [Google Scholar] [CrossRef]
- Batool-Anwar, S.; Baldwin, C.; Fass, S.; Quan, S. Role of spousal involvement in continuous positive airway pressure (CPAP) adherence in patients with obstructive sleep apnea (OSA). Southwest J. Pulm. Crit. Care. 2017, 14, 213–227. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.; Campbell, A.; Mather, S.; Neill, A. From diagnosis to long-term management: The experiences of older New Zealanders with obstructive sleep apnoea. J. Prim. Health Care. 2018, 10, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Jara, S.M.; Hopp, M.L.; Weaver, E.M. Association of continuous positive airway pressure treatment with sexual quality of life in patients with sleep apnea follow-up study of a randomized clinical trial. JAMA Otolaryngol.-Head Neck Surg. 2018, 144, 587–593. [Google Scholar] [CrossRef]
- Ward, K.; Gott, M.; Hoare, K. Becoming a team: Findings from a grounded theory study about living with CPAP. Collegian 2018, 25, 81–88. [Google Scholar] [CrossRef]
- Gentina, T.; Bailly, S.; Jounieaux, F.; Verkindre, C.; Broussier, P.M.; Guffroy, D.; Prigent, A.; Gres, J.J.; Kabbani, J.; Kedziora, L.; et al. Marital quality, partner’s engagement and continuous positive airway pressure adherence in obstructive sleep apnea. Sleep Med. 2019, 55, 56–61. [Google Scholar] [CrossRef]
- Adams, G.C.; Skomro, R.; Wrath, A.J.; Le, T.; McWilliams, L.A.; Fenton, M.E. The relationship between attachment, treatment compliance and treatment outcomes in patients with obstructive sleep apnea. J. Psychosom. Res. 2020, 137, 110196. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Linee guida per il reporting di revisioni sistematiche e meta-analisi: Il PRISMA Statement. Evidence 2015, 7, e1000114. [Google Scholar]
- Baron, C.E.; Smith, T.W.; Baucom, B.R.; Uchino, B.N.; Williams, P.G.; Sundar, K.M.; Czajkowski, L. Relationship partner social behavior and continuous positive airway pressure adherence: The role of autonomy support. Health Psychol. 2020, 39, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Chasens, E.R.; Ratcliffe, S.J.; Weaver, T.E. Development of the FOSQ-10: A short version of the Functional Outcomes of Sleep Questionnaire. Sleep 2009, 32, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Pépin, J.L.; Krieger, J.; Rodenstein, D.; Cornette, A.; Sforza, E.; Delguste, P.; Deschaux, C.; Grillier, V.; Lévy, P. Effective compliance during the first 3 months of continuous positive airway pressure. A European prospective study of 121 patients. Am. J. Respir. Crit. Care Med. 1999, 160, 1124–1129. [Google Scholar] [CrossRef]
- Marcomini, I.; Destrebecq, A.; Rosa, D.; Terzoni, S. Self-reported skills for ensuring patient safety and quality of care among Italian nursing students: A descriptive cross-sectional study. Int. J. Health Promot. Educ. 2021, 60, 67–78. [Google Scholar] [CrossRef]
- Dellafiore, F.; Rosa, D.; Udugampolage, N.S.; Villa, G.; Albanesi, B. Professional values and nursing self-efficacy in the Italian context. Correlational descriptive study. Scand. J. Caring Sci. 2022, 36, 142–149. [Google Scholar] [CrossRef]
- Gobbi, P.; Castoldi, M.G.; Alagna, R.A.; Brunoldi, A.; Pari, C.; Gallo, A.; Magri, M.; Marioni, L.; Muttillo, G.; Passoni, C.; et al. Validity of the Italian Code of Ethics for everyday nursing practice. Nurs. Ethics. 2018, 25, 906–917. [Google Scholar] [CrossRef]
| Database | Query |
|---|---|
| PubMed (1) | (“Sleep Apnea, Obstructive” [Mesh] OR “Sleep Apnea, Obstructive” [text word] OR Sleep Apnea, Obstructive OR “Apneas, Obstructive Sleep” [text word] OR “Obstructive Sleep Apneas” [text word] OR Sleep Apneas, Obstructive OR “Sleep Apneas, Obstructive” [text word] OR Sleep Apneas, Obstructive OR “Obstructive Sleep Apnea Syndrome” [text word] OR Obstructive Sleep Apnea Syndrome OR “Obstructive Sleep Apnea” [text word] OR Obstructive Sleep Apnea OR “OSAHS” [text word] OR OSAHS OR “Syndrome, Sleep Apnea, Obstructive” [text word] OR Syndrome, Sleep Apnea, Obstructive OR “Sleep Apnea Syndrome, Obstructive” [text word] OR Sleep Apnea Syndrome, Obstructive OR “Apnea, Obstructive Sleep” [text word] OR Apnea, Obstructive Sleep OR “Sleep Apnea Hypopnea Syndrome” [text word] OR Sleep Apnea Hypopnea Syndrome OR “Syndrome, Obstructive Sleep Apnea” [text word] OR Syndrome, Obstructive Sleep Apnea OR “Upper Airway Resistance Sleep Apnea Syndrome”[text word] OR Upper Airway Resistance Sleep Apnea Syndrome OR “Syndrome, Upper Airway Resistance, Sleep Apnea” [text word] OR Syndrome, Upper Airway Resistance, Sleep Apnea) AND (“Continuous Positive Airway Pressure”[Mesh] OR “Continuous Positive Airway Pressure”[text word] OR Continuous Positive Airway Pressure OR “CPAP Ventilation” [text word] OR CPAP Ventilation OR “Ventilation, CPAP” [text word] OR Ventilation, CPAP OR “Nasal Continuous Positive Airway Pressure” [text word] OR Nasal Continuous Positive Airway Pressure OR “nCPAP Ventilation” [text word] OR nCPAP Ventilation OR “Ventilation, nCPAP” [text word] OR Ventilation, nCPAP OR “Airway Pressure Release Ventilation” [text word] OR Airway Pressure Release Ventilation OR “APRV Ventilation Mode” [text word] OR APRV Ventilation Mode OR “APRV Ventilation Modes” [text word] OR APRV Ventilation Modes OR “Ventilation Mode, APRV” [text word] OR Ventilation Mode, APRV OR “Ventilation Modes, APRV” [text word] OR Ventilation Modes, APRV) AND (“Treatment Adherence and Compliance” [Mesh] OR “Treatment Adherence and Compliance” [text word] OR Treatment Adherence and Compliance OR “Therapeutic Adherence and Compliance” [text word] OR Therapeutic Adherence and Compliance OR “Treatment Adherence” [text word] OR Treatment Adherence OR “Adherence, Treatment” [text word] OR Adherence, Treatment OR “Therapeutic Adherence” [text word] OR Therapeutic Adherence OR “Adherence, Therapeutic” [text word] OR Adherence, Therapeutic) AND (“Spouses” [Mesh] OR “Spouses” [text word] OR Spouses OR “Spouse” [text word] OR Spouse OR “Married Persons” [text word] OR Married Persons OR “Married Person” [text word] OR Married Person OR “Person, Married” [text word] OR Person, Married OR “Persons, Married” [text word] OR Persons, Married OR “Husbands” [text word] OR Husbands OR “Husband” [text word] OR Husband OR “Domestic Partners” [text word] OR domestic partners OR “Domestic Partner” [text word] OR Domestic Partner OR “Partner, Domestic” [text word] OR Partner, Domestic OR “Partners, Domestic” [text word] OR Partners, Domestic OR “Spousal Notification” [text word] OR Spousal Notification OR “Notification, Spousal” [text word] OR Notification, Spousal OR “Wives” [text word] OR Wives OR “Wife” [text word] OR Wife OR “Spousal involvement” [text word] OR Spousal involvement) |
| PubMed (2) | (((caregiv* [TIAB] OR “CARE GIVER*” [Title/Abstract] OR SPOUS* [Title/Abstract] OR HUSBAND* [Title/Abstract] OR WIFE [Title/Abstract] OR WIVES [TIAB] OR MARITAL [TIAB] OR PARTNER* [Title/Abstract] OR COUPLE [TIAB] OR COUPLES [TIAB]) AND (CPAPS [TIAB] OR CPAP [Title/Abstract] OR “Continuous Positive Airway Pressure” [Title/Abstract] OR Ncpap [Title/Abstract] OR “Airway Pressure Release Ventilation” [Title/Abstract])) AND (“Obstructive Sleep Apnea*” [Title/Abstract] OR “Obstructive Sleep ApnOea*” [TIAB] OR OSAHS [Title/Abstract] OR “Obesity Hypoventilation Syndrome*” [TIAB] OR “Sleep Apnea Hypopnea Syndrome” [Title/Abstract] OR “Sleep Apnoea Hypopnea Syndrome” [TIAB] OR “Upper Airway Resistance Sleep Apnea Syndrome” [Title/Abstract] OR OSA [Title/Abstract] OR OSAS [Title/Abstract])) OR (((“Sleep Apnea, Obstructive” [Mesh]) AND (“Continuous Positive Airway Pressure” [Mesh])) AND ((“Caregivers” [Mesh]) OR “Spouses” [Mesh])) AND (y_10 [Filter]) |
| CINAHL | ((MH “Sleep Apnea, Obstructive”) OR TI (“Obstructive Sleep Apneas” OR “Sleep Apnoea Hypopnea Syndrome” OR “Obstructive Sleep ApnOea*” OR OSAHS OR “Sleep Apnea Hypopnea Syndrome” OR “Upper Airway Resistance Sleep Apnea Syndrome” OR OSA OR OSAS OR “Obesity Hypoventilation Syndrome*”) OR AB (“Sleep Apnoea Hypopnea Syndrome” OR “Obstructive Sleep ApnOea*” OR “Obstructive Sleep Apneas” OR OSAHS OR “Sleep Apnea Hypopnea Syndrome” OR “Upper Airway Resistance Sleep Apnea Syndrome” OR OSA OR OSAS OR “Obesity Hypoventilation Syndrome*”) AND (MH “Caregivers”) OR (MH “Spouses”) OR TI (caregiv* “CARE GIVER*” OR SPOUS* OR HUSBAND* OR WIFE OR WIVES OR PARTNER* OR MARITAL OR COUPLE OR COUPLES) OR (caregiv* “CARE GIVER*” OR SPOUS* OR HUSBAND* OR WIFE OR WIVES OR PARTNER* OR MARITAL OR COUPLE OR CUOPLES) AND (MH “Continuous Positive Airway Pressure”) OR TI (CPAP OR CPAPS OR “Continuous Positive Airway Pressure” OR Ncpap or “Airway Pressure Release Ventilation”) OR AB (CPAP OR CPAPS OR “Continuous Positive Airway Pressure” OR Ncpap or “Airway Pressure Release Ventilation”)) |
| Embase | (((‘continuous positive airway pressure’/exp OR ‘cpap device’/exp) OR (cpap:ti,ab,kw OR cpaps:ti,ab,kw OR ‘continuous positive airway pressure’:ti,ab,kw OR ncpap:ti,ab,kw OR ‘airway pressure release ventilation’:ti,ab,kw)) AND (‘sleep disordered breathing’/exp OR (‘obstructive sleep apneas’:ti,ab,kw OR osahs:ti,ab,kw OR ‘sleep apnea hypopnea syndrome’:ti,ab,kw OR ‘upper airway resistance sleep apnea syndrome’:ti,ab,kw OR osa:ti,ab,kw OR osas:ti,ab,kw OR ‘obesity hypoventilation syndrome*’:ti,ab,kw OR ‘sleep apnoea hypopnea syndrome’:ti,ab,kw OR ‘obstructive sleep apnoea*’:ti,ab,kw)) AND ((‘caregiver’/exp OR ‘spouse’/exp) OR (‘caregiv* care giver*’:ti,ab,kw OR spous*:ti,ab,kw OR husband*:ti,ab,kw OR wife:ti,ab,kw OR wives:ti,ab,kw OR partner*:ti,ab,kw OR marital:ti,ab,kw OR couple:ti,ab,kw OR couples:ti,ab,kw)) AND (2011–2021)/py) AND (‘article’/it OR ‘article in press’/it OR ‘chapter’/it OR ‘conference paper’/it OR ‘review’/it) |
| PsycINFO |
|
| Author/ Year | Aim | Study Design, Sample | Tools and Strategies | Results | Conclusion |
|---|---|---|---|---|---|
| Baron et al., 2011 [46] | To determine the effects of spouse involvement on CPAP adherence and response to treatment problems in male patients with OSA. | Quantitative observational study. Sample 31 males. Inclusion criteria: age < 65 years; cohabitants > 1 year; new diagnosis of OSA; never used CPAP. Exclusion criteria: chronic obstructive pulmonary disease; oxygen therapy; congestive heart failure; cardiomyopathy; psychosis. Study length: 3 months. | Daily questionnaire to be completed by the patient in the evening before going to bed, without the help of the wife, to study the bidirectional relationship between spouse involvement and nocturnal CPAP adherence. Patients rate the wife’s behaviors on a scale: pressure to use the device, cooperation, and support. Severity of illness → AHI; quality of relationship → QRI | 94% report emotional support from their spouse; 77% report being helped with CPAP management; 63% report that their partner reminded them to perform the treatment. The presence of emotional support is associated with cooperation in treatment management (p = 0.06). Spousal support increases after nights with reduced adherence to therapy (p < 0.05). Couples with a positive relationship have higher treatment adherence and cooperation (p < 0.05). Wife pressure to use CPAP is negatively correlated with objective adherence at 3 months. | Emotional and practical involvement of the spouse improves the patient’s approach and adherence to treatment. High levels of relational conflict may interfere with collaboration. |
| Gagnadoux et al., 2011 [28] | To assess the impact of socioeconomic factors on long-term treatment adherence, patient characteristics, and OSA prior to initiation of CPAP therapy. | Multicentre prospective cohort study. Samples: 1141 (674 CPAP adherent, 467 non adherent). Inclusion criteria: age > 18 years; CPAP treatment. Exclusion criteria: patients with mental retardation; patients unable to give informed consent; unable to read and/or speak French; with neuromuscular diseases. Study length: 6 months. | CPAP pre-treatment: health education by a specialist nurse. Tools: Subjective daytime sleepiness → ESS; depressive symptoms → Pichot scale, SES (self-administered questionnaires). One week later, telephone calls were made by the nurse. Follow-up: 3, 6 months. Daily use of CPAP, recorded via device memory card. | Non-adherence is associated with: working patients, non-cohabiting, normal weight, mild to moderate OSA, and smokers (p = 0.051). CPAP adherence is associated with four variables: AHI (p = 0.003); BMI (for BMI ≥ 25 and <30 kg/m², p = 0.01; for BMI ≥ 30 kg/m², p = 0.01); employment status (p = 0.007); married marital status (p = 0.01). Depressive symptoms and daytime sleepiness does not show a statistically significant difference in the non-adherent group (p = 0.18 for Pichot; p = 0.85 for ESS). | Adherence to CPAP influenced by: partner’s post-treatment sleep quality and quality of life. Patients who live alone and/or work are at higher risk of non-adherence. |
| Petersen et al., 2011 [47] | To investigate the effects after 1 year of CPAP treatment on difficulties, discomfort, and sexual dysfunction in female patients with OSA | Quantitative observational study. Sample: 92 female patients. Inclusion criteria: diagnosis of OSA; CPAP treatment; age > 18 years; ability to read and write in Danish. Exclusion criteria: sleep disorders; psychiatric comorbidity. Study length: 1 year. | The sample responded to mailed questionnaires and to the 1 year follow-up in CPAP treatment. Tools: sexual performance for women with partner → FSFI; sexual difficulties → FSDS; sexual difficulties → MFSD; life as a whole, family life, relationship with partner, and sexual life → LiSat-11; daytime sleepiness →ESS. | The FSFI results show no significant improvements for any of the items: desire (p = 0.69); arousal (p = 0.97); lubrication (p = 0.85); orgasm (p = 0.90); satisfaction (p = 0.96); pain (p = 0.94); total score (p = 0.89). FSDS results show no significant improvement (p = 0.06). MSFD results show a reduction in sexual difficulties in the older age group (≥45 years) (p = 0.06) compared to the younger (<45 years) (p = 0.63). The LiSat-11 results do not show significant improvements for any of the parameters: life as a whole (p = 0.59); family life (p = 0.73); relationship with partner (p = 1.00); sex life (p = 0.92). The results of the ESS scale show a significant improvement after 1 year of CPAP treatment (p < 0.001). | CPAP treatment does not adversely affect family or partner relationships. Sharing this information with patients can be important when starting treatment. |
| Baron et al., 2012 [48] | To assess spouse involvement in CPAP treatment of the person with OSA, and its association with adherence to therapy. | Longitudinal observational study. Sample: 23 male. Inclusion criteria: age 18–65 years; male gender; diagnosis of OSA; married or cohabiting with a partner ≥1 year; CPAP treatment. Exclusion criteria: CPAP use by spouse; chronic obstructive pulmonary disease; oxygen therapy; conditions such as: heart failure, cardiomyopathy, psychosis; use of other concomitant treatments for OSA. Length of treatment: 3 months. | Demographic questionnaire completed by patients, prior to CPAP treatment. Partner involvement assessed with questionnaires 7–10 days post treatment start. Tools: Assessing spousal support for CPAP support → Actions Scale-C32, 1 week after treatment start and after 3 months. | At 3 month follow-up, N = 14 Spousal involvement is rated positively by 83% of the patients, with a mean rating of 2.3. A total of 57%, with a mean rating of 1.9, also report negative behaviour. Spousal involvement increases at follow-up, although not significantly (p = 0.07). Adherence to therapy at 3 months improves, and is statistically significantly (p = 0.002). | Involvement of the spouse, especially if positive and supportive, in CPAP treatment in male patients with OSA increases adherence to therapy from the start of treatment to 3 months. |
| Elfström, et al., 2012 [49] | To explore and describe the factors that influence partner support in patients with OSA and how they manage these situations during the initial phase of CPAP treatment. | Exploratory qualitative study. Sample: 25 partners of OSA patients treated with CPAP (18 females and 7 males). Inclusion criteria: Age > 18 years. Exclusion criteria: Patient or partner with a life-threatening illness; diagnosis of a severe psychiatric illness; diagnosis of dementia; difficulty in reading or speaking Swedish. | Semi-structured interviews, lasting from 12 to 60 min, were administered to the partners. Interviews were based on three open-ended questions, asking for a description of: a situation that facilitated treatment support; a situation that worsened the support; the management of these situations. | Five negative factors emerge: adverse effects, limited effect, practical and psychosocial problems, and inappropriate initial routine. Four positive factors emerge: effective treatment, improvement, motivation, and support. Three behaviors influence the partners’ support in using the device: complete freedom (patient autonomy), shared management (supportive behaviour), and substitution (supervision and control). | The presence of the partner on the first days of treatment is a positive predictor of treatment adherence. |
| Henry & Rosenthal, 2013 [50] | To illustrate the significance of the role and relationship with the partner in OSA patients, to diagnose, manage, and set up treatment. | Mixed method. Samples: 24 (12 patients and 12 partners) | Twenty-four semi-structured, qualitative–quantitative interviews were conducted. | A total of 10 patients (83%) report that the symptoms of OSA were identified by their partners: “my husband used to wake me up and say: Hey, you’re not breathing”. Male snoring is often considered “normal” compared to female snoring. Snoring is often mocked by the spouse in contrast to apnea. Patients often associate daytime symptoms with the disease. For 50% of the sample, body weight is the main cause of the problem. The willingness to tackle the problem is delayed. Love–hate relationship with CPAP. Three partners complain about the noise or intrusiveness of the machine, even though they are in favor of the treatment; three spouses, on the other hand, report relaxing because they no longer have to control their partner’s breathing. | It is found that the role of the spouse is crucial in shaping problem identification, perception, help-seeking, and evaluation of the effectiveness of CPAP treatment in patients with OSA. |
| Petersen et al., 2013 [51] | To investigate the impact, after 1 year of CPAP treatment, on sexuality in male patients diagnosed with OSA. | Quantitative observational study. Sample: 146 patients. Inclusion criteria: diagnosis of OSA; CPAP therapy; age > 18 years; ability to read and write in Danish. Length of study: 1 year. | Tools: Life satisfaction → LiSat-11; sexual function → FSFI; daytime sleepiness → ESS. | The LiSat-11 questionnaire shows that sex life significantly improves after 1 year with CPAP treatment (p < 0.05), while family life and relationship with the partner does not change significantly (p > 0.05). All four items of the BSFI change in a statistically significant way: erection (p < 0.05); ejaculation (p < 0.01); desire (p < 0.001); evaluation of problems (p < 0.001). ESS improves significantly after 1 year of CPAP treatment (p < 0.0001). | Significant improvement in sex life and performance in male patients with OSA after 1 year of CPAP treatment. |
| Acar et al., 2016 [52] | Assessing sexual performance in partners before and after CPAP therapy in men with OSA. | Prospective study. Sample: 31 male patients. Patient inclusion criteria: Age > 18 years; AHI ≥ 25; CPAP therapy; BMI ≤ 40 kg/m²; normal uro-andrological examination. Patient exclusion criteria: nitrate treatment and erectile dysfunction (ED) treatment; non-heterosexual relationship; altered hormonal status; diagnosis of: hypertension, diabetes mellitus, peripheral neuropathic disease, or prostate cancer; renal transplantation; aortic aneurysm; spinal cord injury; endocrine disorders, and chronic and acute psychiatric disorders; penile deformities; alcohol abuse; psychotropic drugs; chronic diseases and cardiovascular diseases; and metabolic disorders and neurological disorders. Partner inclusion criteria: age > 18 years; normal urogynecological examination; Partner exclusion criteria: history of alcohol or other substance abuse; severe cardiac or pulmonary disease; uncontrolled hypertension, diabetes mellitus, thyroid disease; history of medication use with sexual side effects; severe pelvic organ prolapse. Length of study: 3 months. | Patients and their partners completed questionnaires separately before CPAP treatment and at 12 weeks, without sharing results. CPAP use was assessed through the device’s internal memory device. Tools: patient sexual function → IIEF; female partner sexual function → FSFI; depression → BDI. | Based on the IIEF questionnaire, all aspects of male sexual functioning improve significantly after CPAP therapy (p < 0.01). An improvement in FSFI post-treatment is also observed in partners (p < 0.001). Assessment of BDI in women at 12 weeks improves statistically significantly (p < 0.01). | CPAP therapy led to improvements in all aspects of male sexual performance. In partners, it was assessed that sexual performance may be unsatisfactory at the diagnosis of spouse OSA, but improves with CPAP treatment. In addition to improving quality of life in men with OSA receiving CPAP treatment, BDI results indicate that the emotional benefits of treatment also extend to the psychological state of the partner. |
| Luyster et al., 2016 [38] | To explore the experiences and difficulties of patients and their partners with CPAP use. Identify an introductory CPAP coaching programme. | Qualitative study design with focus group. Sample: 26 (14 patients and 11 partners, of which 3 male and 8 female). Inclusion criteria: age > 21 for both patients and partners; OSA patients undergoing CPAP therapy; cohabiting for at least 1 year. | Eight focus groups were conducted. Patients and partners participated separately in a total of four groups (3–4 participants per group). Each of the focus groups lasted about 90 min. Half of the focus groups were conducted in person and half by telephone | Five themes are identified: knowledge of sleep apnea; effects of sleep apnea; effects of CPAP; barriers and facilitators to CPAP; ideas for a new user support programme. | The inclusion of the partner in CPAP treatment is identified as a key component of treatment adherence. The partner is a facilitator for device use and identification of strategies in the early phase of therapy. Both patients and their partners experience the disease negatively. The study suggests that the ways in which couples interact in the face of chronic illness evolve as the different stages of chronic illness occur. |
| Baron et al., 2017 [53] | Assessing the factors promoting CPAP adherence in women, and the change in the quality of the relationship with the partner. | Pre-post post-test study. Sample: 20 women (13 married/cohabiting and 7 unmarried/non-cohabiting) Inclusion criteria: age between 18 and 70 years; future treatment with CPAP for OSA. Exclusion criteria: diagnosis of chronic obstructive pulmonary disease; neurological disorders; oxygen therapy; future surgery (3 months); use of other treatments for OSA; dementia; inability to read or write English; unstable psychiatric disorders. Study length: 3 months. | Pre-treatment questionnaires were administered to participants. Adherence to CPAP was assessed at 12 weeks using the device memory. Tools: relationship quality → QRI; emotional support → QRI. One week after the start of CPAP, seven participants provided answers to open-ended questions about the effective and non-effective behaviors with which their partner was involved in therapy. | Higher CPAP adherence among married/cohabiting participants (p < 0.08). Relationship conflict was negatively associated with treatment adherence (p < 0.05). Greater ability to self-manage treatment reported by the unmarried (p < 0.05). Most (6 out of 7) of the participants reported support and encouragement from their spouse/partner. Favourable spouse attitudes: support, encouragement, humorism. Non-favourable attitudes: insistence/harassment, taunting. Participants did not demonstrate changes in the quality of the relationship. | This study assesses that a supportive relationship is important for women’s use of CPAP. Understanding the factors that influence CPAP therapy reduces the risk of non-adherence. |
| Tramonti et al., 2017 [54] | Assessing the quality of relationships in a sample of patients with OSA treated, or not treated, with CPAP. | Quantitative observational study. Sample: 87 (71 males and 16 females; 28 treated with CPAP and 59 untreated) Exclusion criteria: significant comorbidities; unstable medical conditions; shift work; not married; cohabitation < 1 year. Study duration: 6 months. | Tools: subjective daytime sleepiness → ESS; relationship quality → DAS. Adherence to treatment was assessed through the device’s internal memory device. | Treated patients have lower AHI and ESS scores than untreated patients (p = 0.46). Untreated patients show lower DAS scores in the items: affective expression and spousal support (p = 0.046). There are no differences between men and women in either group. Age and relationship duration are positively correlated with total DAS scores in the CPAP-treated group (p ≤ 0.01). | OSA symptoms have an impact on marital satisfaction and relationship quality. The relationship quality of CPAP-treated patients is better than that of untreated patients. Adequate CPAP treatment is important, not only for the clinical condition, but also for the improvement of quality of life. Lasting relationships can act as resources for adaptation to CPAP. |
| Batool-Anwar et al., 2017 [55] | Determine whether spousal involvement affects adherence to CPAP therapy, and how this association varies with gender. | Multicentre randomized double-blind study. Samples: 194 (84 sham CPAP, 110 CPAP). Inclusion criteria: Age ≥ 18 years; clinical diagnosis of OSA; AHI ≥ 10. Exclusion criteria: previous treatment for OSA with CPAP or surgery; oxygen saturation on baseline PSG < 75% by >10%; history of motor vehicle accident related to sleepiness in the last 12 months; presence of chronic diseases; hypnoinductive drugs; shift work. Study length: 3 years. | Patients were administered the 32-item DAS questionnaire assessing marital/affective relationships. CPAP use was recorded on the device’s memory card and analyzed. Long-term CPAP adherence was measured as self-reported at the time of DAS administration. Follow up: 6 months and 3 years. | After randomization at 6 months, CPAP adherence and spouse involvement emerges only in the CPAP group (p = 0.01). After gender stratification, the association between spousal involvement and CPAP adherence is limited to men only, in a statistically significant manner (p = 0.03). Spousal relationship quality is not associated with treatment adherence. At three years, spousal involvement in the CPAP group is not associated with treatment adherence (p = 0.13), even after stratification by gender. | Spousal involvement is important in determining CPAP adherence during the initial treatment period, but has no effect on long-term adherence. |
| Ye et al., 2017 [36] | Identifying aspects that promote and influence CPAP success in conjugate OSA patients. | Exploratory descriptive qualitative design. Sample: 20 couples Inclusion criteria: Age ≥ 18 years; OSA patient; CPAP; married/cohabiting for at least 1 year. Exclusion criteria: not cohabiting; working at night; not understanding English; partners of eligible patients should not have had OSA or been treated with CPAP. | Semi-structured interview of seven questions. The pairs were interviewed together. The interviews focused on the couples’ learning about CPAP management. The interviews lasted approximately 40–60 min, and were conducted in the field. | Sleep disruption and the patient’s health are the reasons why the partners encouraged the start of treatment. It is important that there is complicity in the couple. Couples report that CPAP improves sleep quality and couple’s life. Partners are aware that they are often the reason why their spouse initiates treatment. Both verbal and practical support from the partner in using CPAP was important. Limitations reported for the use of CPAP are: disruption of bedtime routines; decreased intimacy; patients’ concern for their image. | The role of partners is crucial in patients’ adherence to CPAP treatment, as they should not be seen as outsiders, but as integral to the success of the treatment. Partners can have both a positive and negative impact. Couples express the need to support each other and accept responsibility for each other’s wellbeing. Open, frequent, and supportive communication is necessary to facilitate adaptation. |
| Gibson et al., 2018 [56] | To explore the experience of older people (≥65 years) and their partners, living in the Greater Wellington region, regarding diagnosis and treatment for OSA with CPAP | Qualitative study with focus group. Samples: 25 (16 patients, 15 male and 1 female, and 9 spouses/partners). | Focus group (participants were divided into three groups). Breathing before the focus group. | The partners report the symptoms of OSA to the patient and remind them to perform the therapy. Symptoms are not noticed by most patients until treated with CPAP. The key issue for patients and partners is the noise associated with air leaks and CPAP equipment. Overall feedback from participants is positive about both the effect of CPAP and routine adoption of therapy. All participants report improved quality of life. | The key role of the partner in identifying the symptoms (and variation) of OSA, and in the correct use of devices, emerges. |
| Jara et al., 2018 [57] | Assessing the association of CPAP with sexual QoL for patients with OSA. | Prospective, observational cohort study. Samples: 182 (115 men and 67 women) Inclusion criteria: age 18–80 years; knowledge of the English language; CPAP therapy; ability to give informed consent; ability and willingness to understand the study protocol. Exclusion criteria: not having a telephone; previously diagnosed sleep disorder; intention to move during the study. CPAP treatment users were defined as those patients who used the CPAP treatment for more than 4 h per night; conversely, non-users were those who used the CPAP treatment for less than 30 min per night. Study length: 1 year. | Patients were met prior to initiation of CPAP treatment, and at 12 month follow-up. CPAP use was assessed via the device’s internal memory card. Tools: QoL change → SNORE-25. | The cohort is divided into 72 CPAP users and 110 non-users. Both groups show an improvement in QoL at 12 months (users: at baseline 1.2; SD = 1.1; and at follow-up 0.5; SD = 0.7). Men show no difference in improvement of QoL at 12 months between CPAP users and non-users (p > 0.05), in contrast to women who show a greater improvement of QoL at 12 months in CPAP users (p < 0.05). | CPAP users show an improvement in QoL compared to non-users. Among CPAP patients, women reveal a significant association between CPAP and QoL, in contrast to men. |
| Ward et al., 2018 [58] | Exploring experiences of living with CPAP therapy in accompanied persons with OSA. | Grounded theory study. Sample: 16 (9 men and 7 women) Exclusion criteria: age < 17 years; patients prescribed CPAP for other diseases. | Semi-structured interview conducted by telephone, with me, duration of 52 min. The interviews started with open questions to elicit information about the participant regarding CPAP. | Themes that emerged are: becoming a team that sleeps well, making choices about CPAP, and getting used to CPAP. “Becoming a team” explains how patients using CPAP see the role of their partners. Participants also report what contributions are made by family members and friends. Participants and their partners make changes in lifestyle habits to incorporate CPAP into daily life. The presence of family members is found to be the cause of the identification of the health problem (“for years and years, I didn’t see it as a big problem, because I never counted apneas”); they are also credited with the success of treatment adherence. | The study led to the construction of a theory based on negotiating the positive and negative aspects of CPAP, and the balance of living with it. Partners are an integral part of the CPAP process, and should be included in the pathway from diagnosis to treatment management at home. The active presence of partners promotes understanding of the pathology, purpose, and management of therapy. |
| Gentina et al., 2019 [59] | Assess spouse/partner involvement and relationship quality on CPAP adherence. | Multicentre prospective study. Samples = 290 (224 males and 66 females) Inclusion criteria: age >18 years; cohabitation > 1 year; newly diagnosed OSA, with no previous experience of CPAP use. Exclusion criteria: patients with neurocognitive disorders; patients with language fluency problems. A total of 72.4% of couples report sleeping in the same room. Length of study: 3 months. | Standardized 1 h educational programme, including 10 min videos on OSA, before starting treatment. At the beginning of treatment, patients assessed their marital relationship → QMI. After 45 days, patients completed a questionnaire to assess their partner’s commitment to CPAP. The following were assessed: pressure to use CPAP; emotional support; cooperation. | Partner involvement has a direct impact on QoL and adherence to therapy (p < 0.05). For patients with a high QMI, the relationship between partner involvement and adherence to therapy is statistically significant (p < 0.001). | Partner involvement and relationship quality have a significant impact on CPAP adherence and perceived quality of life, particularly in couples with a high QMI. |
| Khan et al., 2019 [23] | To identify OSA patients’ preferences, partners’ experiences, barriers and facilitators of CPAP adherence, and to assess understanding of the educational content provided, and satisfaction with the multidimensional intervention. | Randomized controlled clinical trial. Samples: 60 (28 treatment group, 32 control group). | Patients and partners participated in an information session on the use of the device. The experimental group underwent a further thirteen training sessions (60–90 min): interactive educational sessions; coaching; practical exercise with the device by a respiratory therapist; semi-structured motivational interview. The control group was observed over time. | Two positive and two negative emotional themes emerge. Sense of relief and desire to live long; fear and frustration. Part of the sample report that they started treatment prompted by their partner. Peer-coaching demonstrates the potential value of an emotionally supportive environment for treatment adherence. Adherence to treatment closely linked to the existence and quality of family ties | Patients’ and partners’ positive experiences with CPAP are enhanced by patient-centered education, and improved adherence to therapy. It is important to address the couple’s fears and concerns in order to optimize therapy. |
| Luyster et al., 2019 [29] | Assessing the acceptability, feasibility, and preliminary effectiveness of a CES intervention for CPAP adherence. | Observational quantitative pilot study Sample: 30 (patients/partners) Inclusion criteria: age > 18 years; diagnosis of OSA; CPAP treatment; mothers or cohabitation with partner; English reading and writing skills. Exclusion criteria: previous CPAP treatment. Length of the study: 3 months. | Random assignment to three groups: CES, PES, and UC. CPAP adherence assessed by memory device at 1 week, 1 month, and 3 months. Tools: daytime sleepiness → ESS; sleep quality → PSQI; impact of sleepiness on life activities →FOSQ-10. | CES: increased adherence to CPAP (1.4 h from 1 week to 1 month; decrease of 1.6 h from 1 to 3 months). In the three groups, improvements are observed at 3 months for ESS, PSQI, and FOSQ-10. Specifically for the CES group, PSQI: at baseline 8.4 (SD = 2.5), and at 3 months 5.0 (SD = 3.4); EES: at baseline 9.0 (SD = 6.9), and at 3 months 4.2 (SD = 0.8); FOSQ-10: at baseline 16.6 (SD = 2.6), and at 3 months 17.9 (SD = 0.9). The partners also report improved values on all three scales from baseline to 3 months. | An educational and supportive intervention aimed at new CPAP users and their partners is feasible and beneficial. Improvements in sleep quality, daytime sleepiness, and daytime function are evident for both patients and partners in the CES group. In the CES group, there is an increase in CPAP use in the first month, and a decrease at 3 months. The authors recommend further educational sessions. All partners report that the intervention helped them to support the patient in using the CPAP. This involvement may decrease with time. |
| Adams et al., 2020 [60] | Explore the role of two important interpersonal descriptors (attachment and relationship satisfaction) on treatment initiation and CPAP compliance. The benefit of CPAP treatment on sleep measures and psychological functioning is also examined. | Observational study pre-test post-test. Sample: N = 83 (T1) (69 women and 14 men), after 3 months (T2) N = 31 Inclusion criteria: age 18–65 years; diagnosis of OSA; living with partner for six months. Exclusion criteria: other sleep disorders; hypnoinductive therapy at the time of assessment; substance abuse; oxygen therapy; recent hospitalization; history of heart failure, chronic pain, chronic obstructive pulmonary disease, psychosis, or bipolar disorder. | Tools: adherence to therapy → ECR; sleep quality → PSQI; daytime sleepiness → ESS; depressive symptoms and anxiety symptoms → PHQ-9 and GAD-7; relationship satisfaction → CSI-16 Adherence to CPAP treatment was recorded on a memory card in the CPAP machines (between T1 and T2). | There is no significant difference in the perception of anxiety between those who started the treatment prompted by their partner or autonomously (p = 0.049), and those who decided in agreement with their partner or autonomously (p = 0.04). Adherence to CPAP increases at T2, associated with increased use of the device (p = 0.02). Between T1 and T2, improved sleep quality and reduced levels of depression (p < 0.001) and anxiety (p < 0.001). No statistically significant difference between T1 and T2 in CSI (p = 0.26) | The use of CPAP makes a significant difference in the treatment of sleep, a reduction in depression and anxiety at 1 month after treatment, but these are not sustained after 3 months of treatment. The study does not provide relevant information with respect to the improvement in the quality of the couple’s relationship 3 months after the start of treatment. The authors suggest including the partner in CPAP education and management. |
| Baron et al., 2020 [53] | Examining patients’ perceptions of partner support on CPAP adherence. | Quantitative observational study. Sample: 92 patients Inclusion criteria: OSA diagnosis; cohabitation > 1 year; no CPAP use. Exclusion criteria: treatment for OSA other than CPAP; chronic obstructive pulmonary disease; oxygen therapy; congestive heart failure; cardiomyopathy; psychosis; non-native English speaker. Study length: 2 months. | Completion of online questionnaires at 14 and 60 days after CPAP initiation: support for perceived partner autonomy and response to CPAP. Adherence to CPAP was assessed through the device memory. Tools: autonomy support → IOCQ; perceived partner participation → Likert scale. | Average daily increase in CPAP use (p < 0.001). A significant improvement in perceived partner support is observed at 14 and 60 days (p = 0.046; p = 0.001). The association between partner autonomy support and CPAP use is re-evaluated at 1, 14, 30, 46, and 60 days: day 1: p = 0.546; day 14: p = 0.046; day 30: p = 0.001; day 46: p < 0.001; day 60: p = 0.001. | Positive and/or negative spousal attitudes discriminate against CPAP adherence. Perceived autonomy is observed to be associated with CPAP adherence, with patients reporting higher levels of partner support being more likely to adhere to treatment. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa, D.; Amigoni, C.; Rimoldi, E.; Ripa, P.; Ligorio, A.; Fracchiolla, M.; Lombardi, C.; Parati, G.; Perger, E. Obstructive Sleep Apnea and Adherence to Continuous Positive Airway Pressure (CPAP) Treatment: Let’s Talk about Partners! Healthcare 2022, 10, 943. https://doi.org/10.3390/healthcare10050943
Rosa D, Amigoni C, Rimoldi E, Ripa P, Ligorio A, Fracchiolla M, Lombardi C, Parati G, Perger E. Obstructive Sleep Apnea and Adherence to Continuous Positive Airway Pressure (CPAP) Treatment: Let’s Talk about Partners! Healthcare. 2022; 10(5):943. https://doi.org/10.3390/healthcare10050943
Chicago/Turabian StyleRosa, Debora, Carla Amigoni, Elisa Rimoldi, Paola Ripa, Antonella Ligorio, Miriam Fracchiolla, Carolina Lombardi, Gianfranco Parati, and Elisa Perger. 2022. "Obstructive Sleep Apnea and Adherence to Continuous Positive Airway Pressure (CPAP) Treatment: Let’s Talk about Partners!" Healthcare 10, no. 5: 943. https://doi.org/10.3390/healthcare10050943
APA StyleRosa, D., Amigoni, C., Rimoldi, E., Ripa, P., Ligorio, A., Fracchiolla, M., Lombardi, C., Parati, G., & Perger, E. (2022). Obstructive Sleep Apnea and Adherence to Continuous Positive Airway Pressure (CPAP) Treatment: Let’s Talk about Partners! Healthcare, 10(5), 943. https://doi.org/10.3390/healthcare10050943






