Variation in Hemodynamic Characteristics during Periodontal Crown-Lengthening Surgical Procedure: An Uncontrolled Cohort Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Silvestre, F.-J.; Salvador-Martínez, I.; Bautista, D.; Silvestre-Rangil, J. Clinical study of hemodynamic changes during extraction in controlled hypertensive patients. Med. Oral Patol. Oral Cir. Bucal. 2011, 16, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Moore, P.A.; Doll, B.; Delie, R.A.; Hersh, E.V.; Korostoff, J.; Johnson, S.; Goodson, J.M.; Halem, S.; Palys, M.; Leonel, J.S. Hemostatic and anesthetic efficacy of 4% articaine HCl with 1:200,000 epinephrine and 4% articaine HCl with 1: 100,000 epinephrine when administered intraorally for periodontal surgery. J. Periodontol. 2007, 78, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Fukayama, H.; Yagiela, J.A. Monitoring of vital signs during dental care. Int. Dent. J. 2006, 56, 102–108. [Google Scholar] [CrossRef] [PubMed]
- D’Eramo, E.M.; Bookless, S.J.; Howard, J.B. Adverse events with outpatient anesthesia in Massachusetts. J. Oral Maxillofac. Surg. 2003, 61, 793–800. [Google Scholar] [CrossRef]
- D’Eramo, E.M. Mortality and morbidity with outpatient anesthesia: The Massachusetts experience. J. Oral Maxillofac. Surg. 1999, 57, 531–536. [Google Scholar] [CrossRef]
- D’Eramo, E.M.; Bontempi, W.J.; Howard, J.B. Anesthesia morbidity and mortality experience among Massachusetts oral and maxillofacial surgeons. J. Oral Maxillofac. Surg. 2008, 66, 2421–2433. [Google Scholar] [CrossRef]
- Tomlin, P.J. Death in outpatient dental anaesthetic practice. Anaesthesia 1974, 29, 551–570. [Google Scholar] [CrossRef]
- Silvestre, F.; Verdú, M.; Sanchís, J.; Grau, D.; Peñarrocha, M. Effects of vasoconstrictors in dentistry upon systolic and diastolic arterial pressure. Med. Oral Patol. Oral Cir.Bucal. 2001, 6, 57–63. [Google Scholar]
- Brand, H.; Gortzak, R.T. Different types of dental tre. Int. Dent. J. 1995, 45, 45–48. [Google Scholar]
- Agras, S.; Sylvester, D.; Oliveau, D. The epidemiology of common fears and phobia. Compr. Psychiatry 1969, 10, 151–156. [Google Scholar] [CrossRef]
- Berggren, U.; Meynert, G. Dental fear and avoidance: Causes, symptoms, and consequences. J. Am. Dent. Assoc. 1984, 109, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Kleinknecht, R.A.; Klepac, R.K.; Alexander, L.D. Origins and characteristics of fear of dentistry. J. Am. Dent. Assoc. 1973, 86, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.E.; Dorman, M.L.; Moore, P.A.; Girdler, N.M. Pain control and anxiety management for periodontal therapies. Periodontol 2000 2008, 46, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Grisolia, B.M.; Dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef]
- Said, O.B.; Razumova, S.; Velichko, E.; Tikhonova, S.; Barakat, H. Evaluation of the changes of salivary pH among dental students depending on their anxiety level. Eur. J. Dent. 2020, 14, 605–612. [Google Scholar] [CrossRef]
- Gaffar, B.O.; Alagl, A.S.; Al-Ansari, A.A. The prevalence, causes, and relativity of dental anxiety in adult patients to irregular dental visits. Saudi. Med. J. 2014, 35, 598–603. [Google Scholar]
- Jeddy, N.; Nithya, S.; Radhika, T.; Jeddy, N. Dental anxiety and influencing factors: A cross-sectional questionnaire-based survey. Indian J. Dent. Res. 2018, 29, 10–15. [Google Scholar]
- Gadve, V.R.; Shenoi, R.; Vats, V.; Shrivastava, A. Evaluation of anxiety, pain, and hemodynamic changes during surgical removal of lower third molar under local anesthesia. Ann. Maxillofac. Surg. 2018, 8, 247–253. [Google Scholar] [CrossRef]
- Moaddabi, A.; Hasheminia, D.; Bagheri, S.; Soltani, P.; Patini, R. Effect of opaque eye coverage on anxiety in candidates for surgical removal of impacted third molars: A randomized clinical trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 267–272. [Google Scholar] [CrossRef]
- Patini, R.; Staderini, E.; Cantiani, M.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Dental anaesthesia for children–effects of a computer-controlled delivery system on pain and heart rate: A randomised clinical trial. Br. J. Oral Maxillofac. Surg. 2018, 56, 744–749. [Google Scholar] [CrossRef]
- Matsumura, K.; Miura, K.; Takata, Y.; Kurokawa, H.; Kajiyama, M.; Abe, I.; Fujishima, M. Changes in blood pressure and heart rate variability during dental surgery. Am. J. Hypertens. 1998, 11, 1376–1380. [Google Scholar] [CrossRef]
- Bayat, M.; Zaeri, F.; Sadatnia, F. Comparison of O2 saturation, heart and respiratory rate following injection of vasoconstrictor containing anesthetic (lidocaine 2%) and without vasoconstrictor anesthetic (Mepivacaine). Int J. Dent. Med. 2005, 18, 45–50. [Google Scholar]
- Faraco, F.N.; Kawakami, P.Y.; Mestnik, M.J.; Ferrari, D.S.; Shibli, J.A. Effect of anesthetics containing lidocaine and epinephrine on cardiovascular changes during dental implant surgery. Oral Implantol. 2007, 33, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Jackson, E. Managing dental fears: A tentative code of practice. J. Oral Med. Oral Surg. 1974, 29, 96–101. [Google Scholar]
- Molin, C.; Seeman, K. Disproportionate dental anxiety clinical and nosological considerations. Acta Odontol. Scand. 1970, 28, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Gale, E.N. Fears of the dental situation. J. Dent. Res. 1972, 51, 964–966. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Matsumura, K.; Miura, K.; Kurokawa, H.; Abe, I.; Takata, Y. Cardiovascular and sympathetic responses to dental surgery with local anesthesia. Hypertens. Res. 2001, 24, 209–214. [Google Scholar] [CrossRef][Green Version]
- Miura, K.; Matsumura, K.; Nakamura, Y.; Kurokawa, H.; Kajiyama, M.; Takata, Y. Suppression of cardiac sympathetic nervous system during dental surgery in hypertensive patients. Hypertens. Res. 2000, 23, 207–212. [Google Scholar] [CrossRef][Green Version]
- Tsuchihashi, T.; Takata, Y.; Kurokawa, H.; Miura, K.; Maruoka, Y.; Kajiyama, M.; Fujishima, M. Blood pressure response during dental surgery. Hypertens. Res. 1996, 19, 189–194. [Google Scholar] [CrossRef]
- Satou, T.; Mukaida, T.; Abe, E.; Nozaka, K.; Amari, E. Blood pressure changes in children during minor oral surgery. ShoniShikagakuzasshi. Shoni Shikagaku Zasshi 1990, 28, 761–769. [Google Scholar]
- Meyer, F.-U. Haemodynamic changes under emotional stress following a minor surgical procedure under local anaesthesia. Int. J. Oral Maxillofac. Surg 1987, 16, 688–694. [Google Scholar] [CrossRef]
- Knoll-Kohler, E.; Frie, A.; Becker, J.; Ohlendorf, D. Changes in plasma epinephrine concentration after dental infiltration anesthesia with different doses of epinephrine. J. Dent. Res. 1989, 68, 1098–1101. [Google Scholar] [CrossRef] [PubMed]
- Salonen, M.; Forssell, H.; Scheinin, M. Local dental anaesthesia with lidocaine and adrenaline. Effects on plasma catecholamines, heart rate and blood pressure. Int. J. Oral Maxillofac. Surg. 1988, 17, 392–394. [Google Scholar] [CrossRef]
- Gedik, R.; Marakoglu, I.; Demirer, S. Blood pressure, heart rate and temperature variability during periodontal surgery. West Indian Med. J. 2005, 54, 329–333. [Google Scholar] [CrossRef]
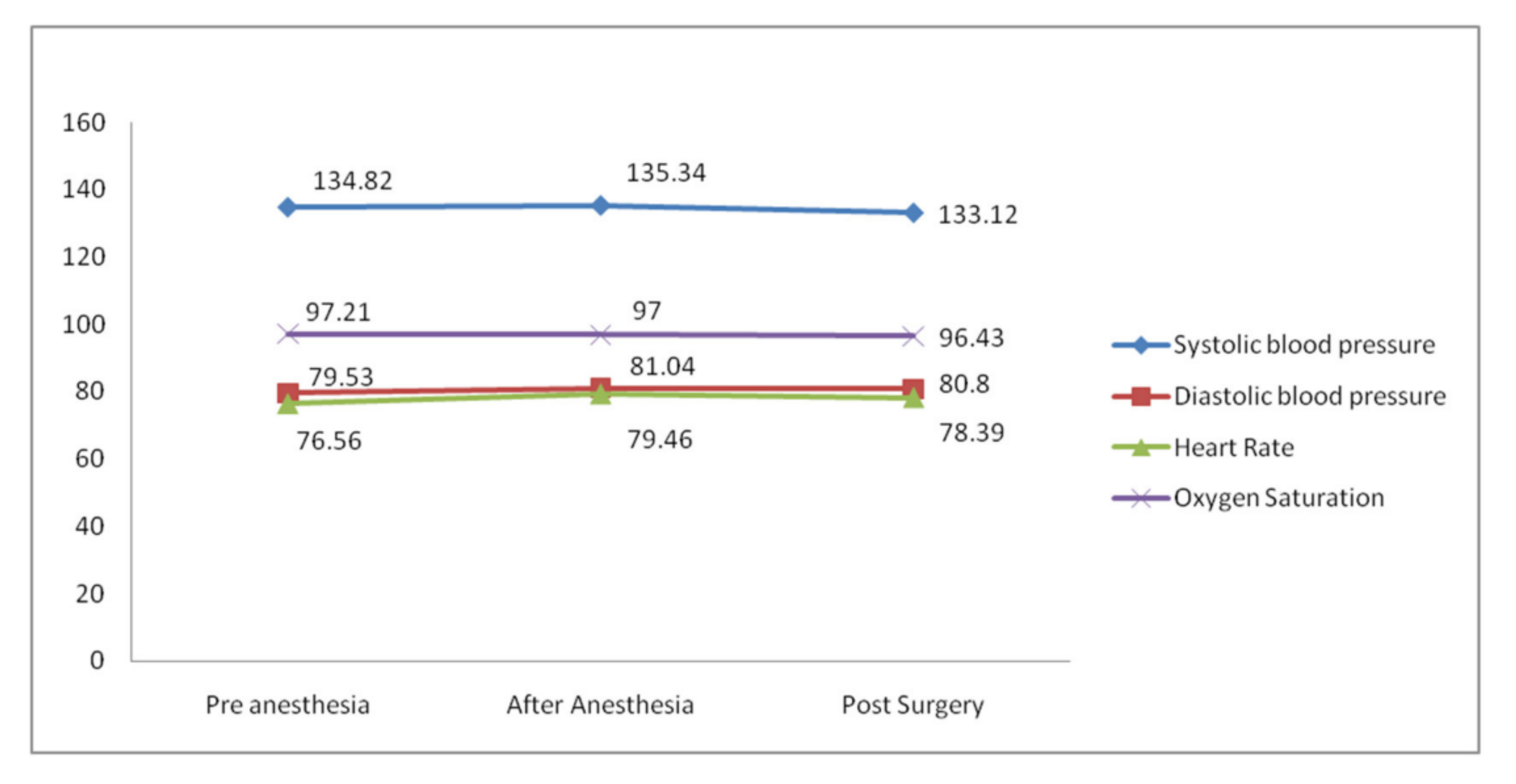
| Parameters | Interval | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | T1 | 134.82 | 8.45 | 122.00 | 152.00 |
| T2 | 135.34 | 6.24 | 130.00 | 156.00 | |
| T3 | 133.12 | 4.89 | 128.00 | 150.00 | |
| Diastolic blood pressure (mmHg) | T1 | 79.53 | 9.32 | 64.00 | 92.00 |
| T2 | 81.04 | 7.01 | 70.00 | 98.00 | |
| T3 | 80.80 | 5.06 | 72.00 | 92.00 | |
| Heart Rate (BPM) | T1 | 76.56 | 7.11 | 67.00 | 88.00 |
| T2 | 79.46 | 8.18 | 67.00 | 99.00 | |
| T3 | 78.39 | 7.46 | 67.00 | 92.00 | |
| Oxygen Saturation (%) | T1 | 97.21 | 1.21 | 95.00 | 99.00 |
| T2 | 97.00 | 1.24 | 95.00 | 98.00 | |
| T3 | 96.43 | 1.18 | 95.00 | 98.00 |
| Parameters | Sum of Squares | Df | Mean Square | F | p |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 110.748 | 2 | 55.374 | 1.236 | 0.294 |
| Diastolic blood pressure (mmHg) | 54.049 | 2 | 27.024 | 0.501 | 0.607 |
| Heart Rate (BPM) | 176.602 | 2 | 88.301 | 1.528 | 0.221 |
| Oxygen Saturation (%) | 13.285 | 2 | 6.642 | 4.500 | 0.013 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, A.S.; Sharanesha, R.B.; Gufran, K.; Alqhtani, N.R.; Abushanan, A.; Alasqah, M.; Alsakr, A.M.; Alkharaan, H. Variation in Hemodynamic Characteristics during Periodontal Crown-Lengthening Surgical Procedure: An Uncontrolled Cohort Study. Healthcare 2022, 10, 919. https://doi.org/10.3390/healthcare10050919
Alqahtani AS, Sharanesha RB, Gufran K, Alqhtani NR, Abushanan A, Alasqah M, Alsakr AM, Alkharaan H. Variation in Hemodynamic Characteristics during Periodontal Crown-Lengthening Surgical Procedure: An Uncontrolled Cohort Study. Healthcare. 2022; 10(5):919. https://doi.org/10.3390/healthcare10050919
Chicago/Turabian StyleAlqahtani, Abdullah Saad, Rajashekhara Bhari Sharanesha, Khalid Gufran, Nasser Raqe Alqhtani, Alwaleed Abushanan, Mohammed Alasqah, Abdulaziz Mohammad Alsakr, and Hassan Alkharaan. 2022. "Variation in Hemodynamic Characteristics during Periodontal Crown-Lengthening Surgical Procedure: An Uncontrolled Cohort Study" Healthcare 10, no. 5: 919. https://doi.org/10.3390/healthcare10050919
APA StyleAlqahtani, A. S., Sharanesha, R. B., Gufran, K., Alqhtani, N. R., Abushanan, A., Alasqah, M., Alsakr, A. M., & Alkharaan, H. (2022). Variation in Hemodynamic Characteristics during Periodontal Crown-Lengthening Surgical Procedure: An Uncontrolled Cohort Study. Healthcare, 10(5), 919. https://doi.org/10.3390/healthcare10050919






