Abstract
Falling birth rates and rising life expectancy are leading to global aging. The proportional increase in older people can be observed in almost all countries and regions worldwide. As a result, more people spend their later years in nursing homes. In homes where person-centered care is implemented, residents report greater satisfaction and quality of life. This approach is based on the wishes and needs of the residents. Therefore, the purpose of this scoping review is to explore the wishes and needs of nursing home residents. A scoping review of the literature was conducted in which 12 databases were systematically searched for relevant articles according to PRISMA-ScR guidelines. Both quantitative and qualitative study designs were considered. A total of 51 articles met the inclusion criteria. Included articles were subjected to thematic analysis and synthesis to categorize findings into themes. The analysis identified 12 themes to which the wishes and needs were assigned: (1) Activities, leisure, and daily routine; (2) Autonomy, independence, choice, and control; (3) Death, dying, and end-of-life; (4) Economics; (5) Environment, structural conditions, meals, and food; (6) Health condition; (7) Medication, care, treatment, and hygiene; (8) Peer relationship, company, and social contact; (9) Privacy; (10) Psychological and emotional aspects, security, and safety; (11) Religion, spirituality; and (12) Sexuality. Nursing home residents are not a homogeneous group. Accordingly, a wide range of needs and wishes are reported in the literature, assigned to various topics. This underscores the need for tailored and person-centered approaches to ensure long-term well-being and quality of life in the nursing home care setting.
1. Introduction
Declines in fertility rates and increases in life expectancy are leading to global population aging. The proportional growth of older people in almost all countries and regions worldwide supports this premise [1]. This demographic change is considered one of the most significant social transformations of the 21st century by the United Nations [1].
In parallel, the number of older people in need of care is also increasing. In Germany, for instance, more than 800,000 people were receiving full inpatient care in a nursing home (NH) at the end of 2019 [2]. These trends bring forth the projection that by 2030 there will be a demand for 1.3 million NH places [3].
Quality of care and residents’ quality of life is still suboptimal in some NHs. Efforts are being made to implement a culture change to improve the quality of the homes [4]. This change is intended to shift away from a focus on physical care and a standardized approach to person-centered and individualized care. The person-centered approach is holistic and views residents as individuals. Respectful discourse with the resident is fundamental to promote care oriented to resident needs and values [4,5].
In NHs where person-centered care is implemented, residents are more satisfied with the quality of care and service. Life satisfaction, overall satisfaction, and quality of life are also higher among residents of homes with person-centered care [6,7]. Implementation of person-centered care for NH residents requires a foundation built on the recognition of their wishes and needs. Thus, fulfilled wishes and needs lead to greater life satisfaction [8]. Consequently, identifying and addressing these can improve quality of life and care for NH residents. Therefore, the purpose of this scoping review is to provide an empirical overview of the range of wishes and needs of NH residents. Previous reviews have already assessed the wishes and needs of older people. However, these have focused either on people receiving home care [9] or exclusively on NH residents with dementia [10,11].
2. Methods
We conducted the present review in accordance with the framework proposed by Peters et al. from the Joanna Briggs Institute (JBI) [12]. The framework includes the following nine steps:
(1) Defining and aligning the objective and question; (2) Developing and aligning the inclusion and exclusion criteria with the objective and question; (3) Describing the planned approach to evidence searching, selection, data extraction, and presentation of the evidence; (4) Searching for the evidence; (5) Selecting the evidence; (6) Extracting the evidence; (7) Analyzing of the evidence; (8) Presenting the results; and (9) Summarizing the evidence in relation to the purpose of the review, making conclusions, and noting any implications of the findings.
We registered the protocol for the study in advance on the Center for Open Science (OSF) in October 2020 [13]. The review process was conducted and the findings were documented and reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist [14].
2.1. Inclusion and Exclusion Criteria
Beforehand, the authors defined the inclusion and exclusion criteria jointly and recurrently reviewed these during the process. Empirical qualitative and quantitative articles that included wishes and needs of people living permanently in a NH were included in the review. Both articles with self-reported and proxy-reported wishes and needs were considered. On average, residents were required to be 60 years of age or older. In addition, we considered only articles published between the years 1990 and 2020 written in English or German. Of interest were studies that included the constructs “wishes” and/or “needs”. To assure this, a definition was established in advance. Generally speaking, defining wishes and needs includes the initiation of a desire, fulfillment, and a positive resulting effect. In detail, wishes and needs are:
Any desire or craving that the person subjectively feels within him- or herself, whether this is material or immaterial, for change or preservation, already fulfilled or still unfulfilled, realistic or unrealistic, current or future, more or less urgent. The fulfillment of this desire causes a positive effect within the person. This positive effect can be related to the quality of life, satisfaction, self-image, autonomy, and any other aspect of the person’s life.
We excluded articles addressing people who were, on average, under 60 years old or people who did not live in a NH. We only included original empirical studies that had already been published in a journal in order to ensure, as far as possible, that only relevant and high-quality studies were considered. Accordingly, gray literature, conference proceedings, books, book chapters, reviews, and dissertations were rejected.
2.2. Searching for the Evidence
We explored relevant journal articles in 12 databases (PubMed, PsycINFO, CINAHL, LIVIVO, Embase, Cochrane Library, GeroLit, SCOPUS, AgeLine, SowiPort, WiSo, and Psyndex) during August and September 2020. A search strategy was developed for each database. Table 1. Search Terms contains the specific search terms in English and German.

Table 1.
Search Terms in English and German.
2.3. Selecting the Evidence
The article selection went through several phases. Three authors completed the database search separately, so each searched four databases. The studies identified by the database search were first screened by title and abstract by one author regarding relevance and fulfillment of the inclusion criteria. The remaining articles were sequentially screened for duplications and removed if necessary. In a final step, each article was screened for relevance and compliance with the inclusion criteria independently by two authors based on the full text. In case of discrepancies between the reviewers, the third author was consulted. Figure 1. Search flowchart following PRISMA guidelines illustrates the details of the article search.
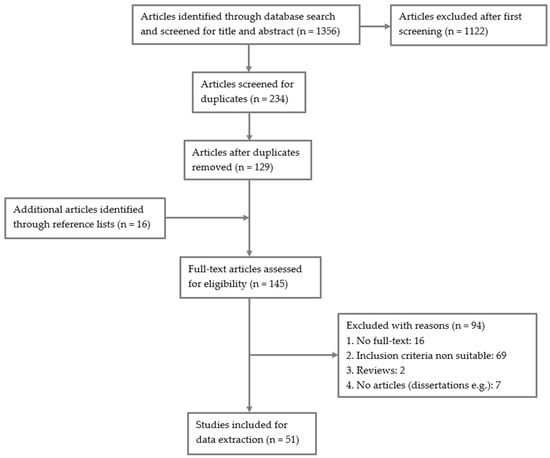
Figure 1.
Search flowchart following PRISMA guidelines.
Of the 1356 articles initially discovered through the database search, 51 articles met the inclusion criteria.
2.4. Extracting the Evidence
The included articles underwent a structured data extraction by three authors capturing essential study information. These include author(s), year, title, journal (number and page), country, sampling strategy, sample characteristics, design and method, data analysis, and relevant results. The reviewer’s name, who performed the extraction, and the data extraction date were also recorded. For quantitative studies, the five most frequently identified wishes and needs were extracted in each case to ensure that the most relevant outcomes were included.
2.5. Analysis of the Evidence
After extraction, the relevant results (which relate to the research question and thus to the wishes and needs of the NH residents) were analyzed using thematic analysis following Braun and Clarke [15]. We developed a category system inductively on the 51 included studies following this approach. Three authors performed the thematic analysis and synthesis. Agreement between the authors led to final system revisions, checks for consistency, and the decision to group individual needs in their context and assignment to the top themes.
3. Results
3.1. Characteristics of the Included Articles
The final analysis includes 51 articles consisting of 28 studies with a quantitative study design, 20 with a qualitative design, and three mixed-methods studies. Of the 28 quantitative studies, 26 were cross-sectional surveys and two were longitudinal. Questionnaires were used to collect data on 26 studies, one of which was a cluster randomized controlled trial (cRCT). The Camberwell Assessment of Need for the Elderly questionnaire (CANE) [16] was used for 10 studies, while four studies used the Preferences for Everyday Living Inventory-Nursing Home questionnaire (PELI-NH) [17]. Of the 20 studies with qualitative designs, 19 were cross-sectional surveys. Sixteen studies used interviews to generate data, one study used the focus group method, and three collected data in interviews and focus groups. All three mixed-methods studies had a cross-sectional design and used both questionnaires and open-ended questions. Thirty-five of the 51 studies assessed self-reported wishes and needs, while 12 interviewed both residents and others, including relatives and family members, caregivers, and nursing assistants. In contrast, four studies surveyed only proxies. Caregivers, volunteers, public guardians, relatives, family members, and non-nursing staff were interviewed. Table 2. Study Summary illustrates the summary of each study.

Table 2.
Study Summary.
3.2. Wishes and Needs
As a first step, we present the results of 41 studies on wishes and needs of NH residents, excluding those that used the CANE questionnaire. Subsequently, we present the results of the remaining ten studies that collected data on wishes and needs with the CANE instrument. This separation seemed reasonable, as the CANE questionnaire is the only instrument that explicitly distinguishes between met and unmet needs. Therefore, the separate presentation and summary of the CANE studies provide a comprehensive overview of the results collected with this questionnaire. The wishes and needs found in the 41 studies presented first could be mapped to 12 themes. These are shown in detail in Table 3.

Table 3.
Explicit description of the themes.
3.2.1. Activities, Leisure, and Daily Routine
The need to make the day active and momentous has been addressed in several studies [27,28,38,46,49,58,60]. Accordingly, wishes for meaningful, person-specific, enjoyable, social, and recreational activities were mentioned [27,28,38,46,60]. Residents like to practice their hobbies and consider activities on special occasions and events as important [27,38]. Various pursuits and leisure activities that residents like to do could be classified under this theme: Reading, listening to music, having contact with animals, keeping up with the news, spending time outside, doing activities outside the NH, playing games, partying, tea-time, gardening, helping others, doing crafts, and spending time with others [27,38,46,49,58]. In addition to the need for specific activities, a general wish for a varied life with diverse offerings and activities was also mentioned [60,62], in which residents can experience self-sufficiency [49].
3.2.2. Autonomy, Independence, Choice, and Control
Moving into an NH can result in a loss of autonomy and independence. Over half of the 41 studies [20,22,25,26,28,30,31,32,33,35,36,38,39,49,50,52,57,58,60,62,63] demonstrate that it is essential for residents to do things for themselves, to have a say in decisions, and to maintain their autonomy to the greatest extent possible. In various studies, NH residents described an experienced dependence and a wish to gain more autonomy and independence: “The stroke nurse who was to do the swallowing test never came. She was to sign me off for swallowing so that I could eat bread… You see I am very determined to be as independent as I can be? I would love to be able to walk to the toilet on my own” [52]. Residents reported a wish to make decisions for themselves or to be involved in the decision-making process and that this is central to their well-being and quality of life [60,62]. The need to have a say relates to both day-to-day issues and far-reaching decisions. For example, residents wish to have control over daily concerns such as deciding when to get up and go to bed [28,38,39], what clothes to wear [38,58], what and when they eat [28,39,49,63], how they spend their day [49], who they share a room with [39], and whether they participate in social activities [49]. Residents also want to make their own decisions on issues related to hygiene and care routines, including bathing and showering type, how often to bathe or shower, and oral hygiene [35,36,38,39,63]. Control over medical matters is highly important to many residents. For instance, residents would like to have a choice regarding how often and which physician they consult [35,39]. Residents are concerned about their future and would like to make advance directives and living wills. According to one study [67], over one-third of residents have a written advance directive, i.e., either an advance directive, or a living will, or a combination of different documents. Residents who already have an advance directive most often want their son or daughter, or a close relative, to act as surrogate decision makers should their own decision-making capacity cease [26,50]. In decisions concerning care, residents wish to determine who has a say for themselves. Some residents wish to make all decisions on their own, but many would also like family members and relatives to have a say, while still others would like staff or the attending physician to make final decisions and hand over responsibility to them [22,25,31,32,35,62].
To maintain a sense of freedom and independence, residents feel the need to regularly leave the NH on their own and independently [39,57,63]: “I tell a member of staff when I leave the NH. This is not a problem. Sometimes I am not back before midnight. I have a key. So, I can come and go whenever I want. That’s great. Because the staff do not have to give a key to the residents” [57]. Some residents want to move out of the NH or want to have control over their own discharge. This is partly based on the need to live in familiar surroundings again, but also on the wish for more self-determination and freedom [33,39,62].
3.2.3. Death, Dying, and End-of-Life
People often move into a NH at a late stage in life, when the issues of dying and death become increasingly important. Residents have different ideas about the end of their lives and dying in the home. NH residents wish not to become bedridden and in need of care in the last phase of life. Furthermore, they wish that their health condition does not deteriorate further allowing for a degree of mobility and activity. Despite impending death, residents want to continue to make plans and be content [40,41]. Contact with family members, friends, relatives, and other confidants, such as nursing staff, or the attending physician, plays an essential role in this phase of life [40,66]. The results show that residents are concerned about discussing the topics of dying and death with familiar people. Residents want to prepare for death and plan for the process of dying and the time after [57]. In addition to a general need to talk about the approaching death, residents are particularly concerned about symptom management, emotional, psychological, and spiritual support, possible counseling services, and funeral issues [27]. One study [32] found that there is often a lack of opportunities to discuss one’s values and needs regarding end-of-life treatment and care with the nursing staff. Resident reactions to such staff discussions vary greatly from unnecessary to a very strong need. Wishes for pain management and more personal and time-intensive care include maintaining personal hygiene and the requirement of additional medical care in the last phase of life [40,56]. There are also clear wishes and needs on the part of NH residents regarding the dying process. In this context, several studies shed light on the context in which people want to die, such as the place of dying, the condition in which they want to die, and the people they would like to have by their side when dying [26,41,50,66,67]. In most cases, residents would like to die in the NH and not be transferred to another facility, such as a hospital. [26,41,50,66,67]. However, needs for passing away at home, in hospice, or in a hospital are also cited [66,67]. Most residents in one study [66] reported wanting to pass away in their sleep (31%). Fewer residents would like to be unconscious or comatose during dying (7%) and a small percentage would like to experience the dying process while conscious (3%). The other residents were not clear at the time of the survey about the condition in which they would like to die or did not make any statement for other reasons.
The question of end-of-life care also seems to be essential for residents. For example, most residents wish to die in the presence of familiar people, such as relatives, friends, nursing staff, or hospice companions. “That I can cling somewhere,… to any hands…” [41]. Others would rather be alone when the time comes [22,41]. When dealing with dying people, physical closeness, human warmth, support, and respectful, open, and honest communication are of great importance [41,66]. Medical and nursing factors are also central. Residents do not want to suffer pain and thirst during the dying process and want to be able to breathe comfortably [22,40,41,56,66]. Many residents do not want to receive life-sustaining measures, including artificial nutrition, resuscitation, surgery, heart–lung machine, ventilator, or dialysis, during the dying phase [22,40,41,56,66]. However, others want to receive life-sustaining treatment in the event of a life-threatening condition [50]. Residents consider a natural and quick death, which they see as a release, important [22,49].
Spiritual factors also play an essential role when residents face death in a NH. Residents want to die quietly and peacefully, which means that they do not want to be a burden on anyone and want to die without much fuss. They wish for forgiveness and reconciliation, for their mistakes not to be of great relevance in retrospect, and for their loved ones to think back on them positively after their passing [41]. During the dying process, residents feel the need to maintain their dignity and self-respect and to leave the world laughing [66].
The wish to die or to actively end life has also been cited in studies [33,57,66]. Three of 18 residents interviewed in the Goodman et al. study [33] want their life to end. Van der Steen et al. [66] found that residents wish to have ways to end life if they feel it is necessary.
3.2.4. Economics
Four of the 41 studies [24,27,60,62] captured residents’ financial wishes and needs. All four studies found a desire for more money or financial support and financial security. Chuang et al. [27] also found that residents feel a need to be able to pay the monthly NH fee. If this cannot be accomplished, residents would be discharged or transferred to another NH with lower standards, which they try to avoid.
3.2.5. Environment, Structural Conditions, Meals, and Food
Studies reported facility-related needs and needs at the structural level, for example, concerning the room occupied [19,20,36,38,46,47,60,62]. Residents wish for a comfortable bed [19], larger [62] and temperature-controlled rooms [36], and the ability to personally furnish the rooms with their own furniture, objects, photos, a television, and a radio [46,60]. Further, needs were expressed for housing facilities that are designed for the elderly and disabled such as the presence of elevators [62]. Clean housing and sanitary facilities are also important to residents. Regarding these, the wish for improvement was mentioned [20,62]. It is also essential that residents can take care of their own belongings and have a way to lock and store smaller items safely [19,36,38]. Other needs related to facility structure include a wish to separate residents with dementia from those without dementia and a wish for more flexible routines. For example, residents would like more flexibility in the timing of taking pills [62]. Culinary care in the NH also plays an essential role for residents. According to Sonntag et al. [62], residents feel the need for better food that is age-appropriate and not so monotonous. In addition, residents want to decide what food they get, how much of it, and whether they eat according to a recommended diet. Some wish for more traditional food to be offered and to take meals at their leisure, without time stress, at set times of the day, and with patient and respectful assistance if necessary [47]. Housen et al. [38] reported that it is important for residents to have snacks available at their convenience in the NH.
3.2.6. Health Condition
An inability of older people living alone with deteriorating health and physical condition often requires a transition to NH. Thus, the issue of health is of high importance for these NH residents. Most common among this theme was the need to maintain and improve health or to prevent a decline in health [33,49,57,60,61,62]. In this context, maintaining both cognitive and physical health status is of high importance. The abilities are seen as a prerequisite for enjoying the last years in the NH: “The few years I have left to live, I want to enjoy them. I can still walk, more or less, well around what you can call walking. You don’t need to put me in a chair yet, a wheelchair or one of them frames. Yeah, I do and wash myself and everything” [60]. As the worst imaginable scenario, residents describe their condition as a nursing case: “I have no expectations anymore. The principal thing is not to become a nursing case. I do not want to become an invalid like some of the other residents. I do not want to lose my mind. In this case, I would rather die” [57]. According to Schmidt et al. [61], residents wish to maintain their physical and sensory awareness.
Additionally, full and honest information about one’s health status is also noted to be essential. While three studies [20,26,60] reported that residents want to be fully informed about health status and, if applicable, fatal diagnoses, Gjerberg et al. [32] found that a small number of residents were unsure whether they might want to receive information of a severe nature or indicated that they did not want to receive information. This is due to fear of harmful consequences, “…that will just leave me thinking. And I would rather not”.
Wishes for mobility or physical activity [57,60,61], for physical comfort [63], and for restful sleep and sleep comfort [58,60,61] were also mentioned under the topic of health condition.
3.2.7. Medication, Care, Treatment, and Hygiene
Thirteen of the 41 studies [18,19,20,27,30,33,35,37,42,46,49,58,62] addressed needs related to the behaviors or characteristics of nursing staff or care received. For example, residents want to receive care that is good [37,58], humane [62], continuous [37,42], competent, skilled [27,62], affectionate [62], encouraging [42], and professional [19]. According to Bangerter et al. [19], professional care in this regard can be defined as friendly, kind, courteous, emphatic, respectful, and characterized by symmetrical communication. Further, residents want to be perceived as individuals, treated personally and with dignity, and taken seriously [30,37,62]. This includes addressing residents personally by name [19]. They wish staff would reliably take care of them and be concerned about them [18,27,33,35]. Residents feel the need to trust the nursing staff [20] and have a good relationship with them [33]. Sensitivity and motivation on the part of caregivers are necessary to form a trusting relationship possible according to residents [42]. This does not always seem to be guaranteed: “Not too many of them help too much when we’re not well-they don’t have feelings… They are tired-they have to lift me and I’m heavy. If they have a bad day or bad night, they lose the ability to be sensitive to our condition. Sometimes I feel that they take their frustrations out on us. They lack a little sensitivity” [42]. Residents wish they were not treated as if they were a nuisance, a problem case, or a child [46,49].
In addition to needs primarily related to nursing staff, residents also reported wishes and needs related to medical care and hygiene. According to different studies [42,58,61] personal hygiene is important to residents. This includes bathing and washing facilities [58], oral hygiene, and regular changing of linens [42]. In one qualitative study with 10 women and 10 men, some women reported a gender-specific need for personal care to be performed by a caregiver who is a woman herself [37]. High-quality medical care includes the use of proper equipment during treatments [20], good skin and wound treatment, expert pain management to prevent discomfort due to physical illness [61], and monitoring for adverse drug reactions [46]. Referring to the study by Michelson et al. [45], residents refuse aggressive medical treatment unless the intervention alleviates pain or results in greater patient comfort or safety. Nakrem et al. [49] and Sonntag et al. [62] found that residents hope to receive more active care in the NH, more therapeutic interventions, more physical therapy, and regular fall prevention by NH staff. To provide more quality of life in the NH, residents wish for more help and support with daily living activities [27,62]. Frustration is reported because this support is not provided by staff without being asked [42]. Residents reported care needs for eating and drinking, excreting, constipation, sleep disturbances, loss of appetite, chronic illnesses (including asthma, arthritis, hypertension), and visual impairment [23,61]: “The constipation has given me piles in that my whole body is affected” [23].
In the study by Levy-Storms et al. [42], excessive cross-boundary support from nursing staff is sometimes reported: “Let me eat (feed myself) with a spoon, like normal people”. This is countered by the reports of residents who experience a lack of individualized and skilled care and attention from NH staff. This is seen as a problem of limited staff capacity, which is why the wish for more staff was mentioned to make the above-mentioned needs and wishes feasible [62].
3.2.8. Peer Relationship, Company, and Social Contact
Contact with other people is a central need for many NH residents. While a good and trusting relationship with the nursing staff has already been presented as the basis for humane and personal care, residents name social contacts and friendships as significant for a satisfying life in the NH. Residents described needs for sociability and conversation in their lives [30,62], for human connection [52], for belonging [30], for a good and personal atmosphere in the home [60], for harmony [23], and for meaningful relationships [55].
Relationships with other NH residents are highly relevant, as these play a significant role in determining the daily environment. Residents actively choose their contacts in the NH, talking about their experiences in the home, their past lives, and their families. They spend time together and do things together: “I am in touch with Anna. She lives down the corridor. She is lucid, and we can talk. She comes to visit me, and then we talk… and if she gets some sweets, she comes to me [to share] and if I get something she appreciates from my family, then I share it with her” [21]. Residents reported a wish for all residents to live better together [62] and a desire for personal and social relationships with other residents [21,27,28,49,60].
In addition to the need for in-home relationships with peer residents, the wish for good relationships with family members, relatives, and friends outside the home was also frequently mentioned. For example, residents would like to maintain family and friendship ties [21,27,28,52,60,63] and spend more time with and are regularly visited by their loved ones [18,20,21,30,35,62].
Residents also wish to maintain contact with their former social environment and the community they lived in before moving. Residents do not want to lose connection to their former lives and the world outside the NH [28,49,52,63]: “I like getting out to the town, you know. I just like to see if there is any building going on or what’s happening in the town” [52]. Residents indicate they want to maintain their past relationships and ties because they are identity-building [52]. Ways to maintain a connection to the outside world include: watching television, listening to the radio, reading the newspaper, or sitting at the front door to watch people come and go [63].
3.2.9. Privacy
As important as human contact is, a certain degree of privacy is likewise important. This was shown by seven studies [19,20,27,28,33,38,60]. Residents desire privacy when using the restroom and performing personal hygiene [19,60]. The wish for privacy further includes the need for a private space [60], which residents understand to mean, for example, occupying a single room [28], but also being able to receive visits or make telephone calls in a private setting [38].
Quietness in the NH is also crucial to residents’ privacy. They wish to rest undisturbed [33] and that they are not disturbed by loud noises [60].
Residents who inevitably interact with others due to the institutional setting want to spend time alone [60] and consider it important for social and psychological privacy that nursing staff knocks upon entering the room [28]. Cooney et al. [28] found that residents of large facilities particularly complained about a lack of privacy. In some cases, beds are separated only by curtains, which ensures a very low level of quiet and privacy: “You only have a curtain separating you” [28].
3.2.10. Psychological and Emotional Aspects, Security, and Safety
Many of the wishes and needs of residents are also in the psychological, emotional, and safety domains. Inner-personal and psycho-emotional needs, for example, were named in the study by O’Neill et al. [52]. Residents wish to have a positive attitude and maintain their own identity, self-efficacy, resilience, and coping strategies. They would like to take each day as it comes and not worry too much about tomorrow. According to Franklin et al. [30] and Schmidt et al. [61], residents want to experience a daily routine, to be able to enjoy the little things in everyday life, and to find a sense of meaning in the NH’s daily routine to experience themselves as part of the environment. It seems essential for residents to have a sense of belonging, to feel understood, and to have a sense of community [60]. Other studies report similar findings [28,61,63]: residents want to be themselves, not lose a sense of self, and be recognized as independent individuals. To ensure this, residents are concerned about their appearance among others. One qualitative study showed that some women want to take care of their appearance. They state that this has a positive effect on their self-expression and self-esteem [28].
Further, having options to do what they want when they are miserable is essential [18,36]. Fundamental to residents is that they feel needed, valued, and welcomed [27]. Schmidt et al. [61] also found that expressing emotions, expressing one’s will, being talked to and touched, as well as touching others are important for residents’ emotional and psychological well-being. NH residents wish for social and emotional support in the home [46] and psychological support for depression, confidence loss, memory loss, anxiety, anger, and irritability [23].
A sense of security is also important to residents. They wish to be safe and secure in the NH [49,60,61]. This includes knowing that the home has safety and security measures installed and that residents always have quick access to emergency services [20,49]. Being protected from self-harm and from disturbance by other residents is also part of living safely in an NH [46].
3.2.11. Religion and Spirituality
Religiosity and spirituality play an important role for many residents. For example, they wish to participate in religious ceremonies [27,38,43,58,61]. They want to express themselves religiously in their lives, follow cultural customs, and feel spiritually connected to others [27,38,61,63]: “I can’t go to the Sunday ceremony, but I read the Bible by myself… You will feel consoled after you read it” [27]. Specific activities that residents undertake to meet their religious and spiritual needs are cited by Man-Ging et al. [43]: praying for themselves, reflecting on past lives, turning to a higher presence, and plunging into the beauty of nature.
3.2.12. Sexuality
One study [48] addressed the sexual needs of NH residents. More than half (51%) of the residents surveyed reported a sexual tension, including more men (65%) than women (41%). In addition, residents reported the following as their most important sexual needs: need for conversation, need for respect, need for tenderness, need for support in any situation, and need for giving and receiving emotional support, by which residents primarily mean empathy and understanding.
3.2.13. CANE Studies
The ten studies that used the CANE questionnaire for data collection are presented separately. The CANE questionnaire covers 25 areas of daily life in the NH to assess older people’s physical, psychological, social, and environmental needs. A distinction is made between met and unmet needs. Table 4 shows the outcomes of CANE studies and gives an overview of the five most frequently mentioned needs in each of these ten studies. Eight studies reported both unmet and met needs [29,34,44,51,54,59,64,68]. One study reported only unmet needs [53], and the study by van der Ploeg et al. [65] reported the sum of met and unmet needs differentiated between residents with dementia, residents without dementia, and relatives. Looking at the results without including the study by van der Ploeg et al. [65], the five most frequently mentioned met needs are in the areas of food, household skills, physical health, accommodation, and self-care. In comparison, the five most frequently unmet needs are in the areas of daytime activities, psychological distress, company, eyesight/hearing, and memory. Some of the five most frequently identified needs that residents have according to CANE studies were also highlighted by the analysis of the 41 other studies. These include the following needs in the area of unmet needs: daytime activities, psychological distress, and company. The met needs, which have also been addressed by the other studies, are as follows: food, physical health, and accommodation. Additional needs identified through the CANE studies that have not been mentioned in the previous analysis are household skills and self-care in the area of met needs and memory and eyesight/hearing related to unmet needs.

Table 4.
Outcomes CANE studies.
4. Discussion
The objective of this scoping review was to identify the wishes and needs of NH residents. The results show numerous needs that were mapped to 12 themes. In 35 studies, residents were interviewed; in 12 studies, residents and proxies were interviewed; and only proxies were interviewed in four studies. This shows that residents can be aware of perceived needs and wishes and can communicate them. This is valid not only for residents without cognitive impairment [69], but also for residents with dementia [11]. Studies show that third-party assessments of needs sometimes differ from what NH residents report [20,35,44,46,54,65]. This finding is especially important for residents with dementia, as needs elicitation for these individuals is often only collected through a proxy survey [11]. It is essential to directly survey NH residents, including residents with dementia, about their wishes and needs. Interviewing proxies can provide additional and helpful information, but is not a substitute for speaking directly with the affected resident.
The scoping review results further indicate that wishes and needs on specific topics differ between individual residents. For example, some would like to receive life-sustaining measures, while others reject them. This high degree of individuality and complexity must be considered in assessing needs. The wishes and needs should be recorded with the individual residents in private conversations, reflected on repeatedly, and the way they are dealt with should be adjusted if necessary. This requires time, expertise, and willingness. Often, there is a lack of human resources to ensure this task is completed. Complaints about a shortage of skilled workers and high workloads in NHs are frequent. [70,71]. These circumstances can lead to less quality in care and can make it difficult to have an individualized approach to residents [72]. Assessment tools, such as the PELI-NH or CANE questionnaire, can be helpful in conducting a comprehensive needs assessment. Such tools can provide clues to existing needs and wishes and present an overview. The CANE questionnaire, for example, does not address all the areas in which NH residents experience needs. Topics that are relevant for residents according to the present study, such as death/dying, autonomy, interaction of nursing staff with residents, and religion/spirituality, are not surveyed by this instrument. When caregivers or other persons refer to the CANE questionnaire in order to assess needs, they should be aware of this. Accordingly, in-depth and recurring interviews with residents are indispensable to consider the high complexity and individuality of wishes and needs. Only in this way can the results be validated and unmet needs can be discovered.
Themes of high relevance seem to be the following, as they were mentioned frequently and in multiple studies: “autonomy, independence, choice, and control”, “death, dying, and end-of-life”, and “medication, care, treatment, and hygiene”. Notably, needs cannot be categorized in a blanket way in which some needs are of higher importance than others. For example, needs in the nursing area may weigh the heaviest for some residents, while others consider the needs for autonomy and self-determination to be most important.
Older adults are aware of their wishes and needs, but in many cases they do not communicate them [73]. Sometimes, when asked about their wishes and needs, residents report that they do not wish for anything because nothing would change anyway. The reason for this seems to be an experienced lack of respect for their wishes. For residents who have the feeling that their personal and subjective wishes and needs are not heard and that addressing them does not lead to any change, communicating their needs does not make sense [62,69]. As another reason for non-communication, older adults in home care state that they do not want to be a burden to anyone, and they do not want to complain about the age-related ailments that are common for them [73]. In these situations, caregivers should treat residents with appreciation and respect. It is important to schedule sufficient time to talk about wishes and needs. It is also important to take residents seriously and show them that expressing their wishes and needs will lead to positive changes in their lives by addressing them. The patronizing communication that often occurs on the part of NH staff may also contribute to NH residents not always openly communicating their wishes and needs, as satisfaction with such interactions can be low [74]. Further, the use of elderspeak due to stereotypical expectations of NH residents’ communication skills can lead to residents not feeling understood or respected and, as a result, they tend to be quiet and accept things without argument [75,76]. As a result, non-communicated needs go unrecognized and, accordingly, unmet. Communication training or person-centered interventions for caregivers could contribute to improved caregiver–patient communication, which could lead to more openness on the part of the residents and, consequently, fewer unmet residents’ needs [77,78].
Shared decision making was a frequently mentioned need. However, sometimes less is more. The study by Reed et al. [79] shows that older people prefer to have fewer options from which to choose than younger people. This suggests that some NH residents may be overwhelmed by too many options. NH staff should individually ask residents whether they prefer to choose from reduced options in some areas of their lives.
The present study has some limitations. First, it must be said that the concepts of “wishes” and “needs” are very complex, and there is no common definition [80]. This can lead to the fact that all researchers involved understand something different by the concept under investigation. A definition was created and applied throughout to prevent this from happening and to ensure consistent study inclusion, data extraction, and analysis. Further, the 51 included studies are diverse in research design, study population, and objectives. For example, there are studies that surveyed residents as well as studies that surveyed proxies. Some studies focused on residents with dementia, while others focused on residents without cognitive impairment, or on unbefriended residents. The research focus was not primarily on wishes and needs in all studies. Constructs such as quality of life, dignity, or thriving were sometimes of substantial research interest. However, relevant wishes and needs were mentioned in the survey on these constructs, which were analyzed here. In the analysis of the quantitative studies, only the five most frequently mentioned wishes and needs were recorded in each case. The disadvantage here is that some wishes and needs were not recorded as a result. As qualitative studies do not include frequencies and therefore no ranking, all needs and wishes were extracted in these, which can lead to an overweighting of the qualitatively surveyed wishes and needs. Further, only studies in English and German were included. This can be explained by the language skills of the researchers but presents the possibility that relevant studies were not included. Consequently, the results only represent an overview of possible wishes and needs as stated by residents or their proxies. In no way do the results claim to be exhaustive of all wishes and needs of NH residents.
Among this study’s strengths is a very extensive literature search of 12 databases that was conducted. Additionally, the evidence examined is extensive, with 51 studies, as demonstrated by the high richness of results.
5. Conclusions
Twelve topics were identified to which the wishes and needs of NH residents can be assigned. This reflects the high complexity and diversity of the needs and wishes of the heterogeneous group of NH residents.
For many NH residents, the NH represents the last phase of life before death. Residents should live a contented and fulfilling life in the home. Essential to achieving satisfaction is the fulfillment of individual wishes and needs. A comprehensive needs assessment on resident wishes and needs should take place in NHs. Speaking directly with the residents is essential to success.
The results of this study provide an evidence-based framework that can serve as a basis for holistic and person-centered care in NHs.
Author Contributions
R.S. contributed to the design, evidence search, data extraction, data analysis, and drafted the manuscript. J.L.O. contributed to the design, evidence search, data extraction, data analysis, and revised the manuscript. M.K. contributed to the design, evidence search, data extraction, data analysis, and revised the manuscript. S.N. initiated the study, contributed to the design, and revised the manuscript. A.T. initiated the study, contributed to the design, and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Department of Economic and Social Affairs, Population Division. World Population Ageing 2015; United Nations: New York, NY, USA, 2015.
- Statistisches Bundesamt, Destatis [Federal Statistical Office of Germany]. Pflegestatistik—Pflege im Rahmen der Pflegeversicherung Deutschlandergebnisse [Care Statistics—Care under Long-Term Care Insurance Germany Results]. 2020. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Pflege/Publikationen/Downloads-Pflege/pflege-deutschlandergebnisse-5224001199004.pdf?__blob=publicationFile (accessed on 6 April 2022).
- Gesellschaft für Wirtschaftliche Strukturforschung [Society for Economic Structural Research]. Struktur des Pflegemarktes in Deutschland und Potentiale Seiner Entwicklung [Structure of the Care Market in Germany and Potentials for Its Development]. 2016. Available online: https://www.bmwk.de/Redaktion/DE/Publikationen/Studien/forschungsvorhaben-struktur-des-pflegemarktes-in-deutschland-und-potentiale-seiner-entwicklung.pdf?__blob=publicationFile&v=4 (accessed on 6 April 2022).
- Zimmerman, S.; Shier, V.; Saliba, D. Transforming Nursing Home Culture: Evidence for Practice and Policy. Gerontologist 2014, 54 (Suppl. 1), S1–S5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellchambers, H.; Penning, C. Editorial: Person-Centered Approach to Care (PCA): A Philosophy of Care and Management for Carers. Contemp. Nurse 2007, 26, 196–197. [Google Scholar] [CrossRef] [PubMed]
- Poey, J.L.; Hermer, L.; Cornelison, L.; Kaup, M.L.; Drake, P.; Stone, R.I.; Doll, G. Does Person-Centered Care Improve Residents’ Satisfaction With Nursing Home Quality. J. Am. Med. Dir. Assoc. 2017, 18, 974–979. [Google Scholar] [CrossRef]
- Yasuda, M.; Sakakibara, H. Care Staff Training Based on Person-Centered Care and Dementia Care Mapping, and Its Effects on the Quality of Life of Nursing Home Residents with Dementia. Aging Ment. Health 2017, 21, 991–996. [Google Scholar] [CrossRef] [PubMed]
- Custers, A.F.J.; Westerhof, G.J.; Kuin, Y.; Riksen-Walraven, M. Need Fulfillment in Caring Relationships: Its Relation with Well-Being of Residents in Somatic Nursing Homes. Aging Ment. Health 2010, 14, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Dostálová, V.; Bártová, A.; Bláhová, H.; Holmerová, I. The Needs of Older People Receiving Home Care: A Scoping Review. Aging Clin. Exp. Res. 2021, 33, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Cadieux, M.A.; Garcia, L.J.; Patrick, J. Needs of People with Dementia in Long-Term Care: A Systematic Review. Am. J. Alzheimers Dis. Other Demen. 2013, 28, 723–733. [Google Scholar] [CrossRef]
- Shiells, K.; Pivodic, L.; Holmerová, I.; Van den Block, L. Self-Reported Needs and Experiences of People with Dementia Living in Nursing Homes: A Scoping Review. Aging Ment. Health 2020, 24, 1553–1568. [Google Scholar] [CrossRef] [Green Version]
- Peters, M.; Godfrey, C.; McInerney, P.; Munn, Z.; Trico, A.; Khalil, H. Chapter 11: Scoping Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; ISBN 978-0-648-84880-6. [Google Scholar]
- Schweighart, R.; O’Sullivan, J.L.; Klemmt, M. Needs and Wishes of Elderly People Living in Nursing Homes: A Scoping Review Protocol. 2020. Available online: https://doi.org/10.17605/OSF.IO/SAKT4 (accessed on 6 April 2022).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, T.; Thornicroft, G.; Abas, M.; Woods, B.; Hoe, J.; Leese, M.; Orrell, M. Camberwell Assessment of Need for the Elderly (CANE): Development, Validity and Reliability. Br. J. Psychiatry 2000, 176, 444–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curyto, K.; van Haitsma, K.S.; Towsley, G.L. Cognitive Interviewing: Revising the Preferences for Everyday Living Inventory for Use in the Nursing Home. Res. Gerontol. Nurs. 2016, 9, 24–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbott, K.M.; Heid, A.R.; Kleban, M.; Rovine, M.J.; van Haitsma, K. The Change in Nursing Home Residents’ Preferences Over Time. J. Am. Med. Dir. Assoc. 2018, 19, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Bangerter, L.R.; Van Haitsma, K.; Heid, A.R.; Abbott, K. “Make Me Feel at Ease and at Home”: Differential Care Preferences of Nursing Home Residents. Gerontologist 2016, 56, 702–713. [Google Scholar] [CrossRef] [Green Version]
- Ben Natan, M. Perceptions of Nurses, Families, and Residents in Nursing Homes Concerning Residents’ Needs. Int. J. Nurs. Pract. 2008, 14, 195–199. [Google Scholar] [CrossRef]
- Bergland, Å.; Kirkevold, M. The Significance of Peer Relationships to Thriving in Nursing Homes. J. Clin. Nurs. 2008, 17, 1295–1302. [Google Scholar] [CrossRef]
- Bollig, G.; Gjengedal, E.; Rosland, J.H. They Know!—Do They? A Qualitative Study of Residents and Relatives Views on Advance Care Planning, End-of-Life Care, and Decision-Making in Nursing Homes. Palliat. Med. 2016, 30, 456–470. [Google Scholar] [CrossRef] [Green Version]
- Chabeli, M. Health Care Needs of Older People Living Permanently in a Residential Home Setting in Gauteng. Curationis 2003, 26, 14–21. [Google Scholar] [CrossRef] [Green Version]
- Chamberlain, S.A.; Duggleby, W.; Teaster, P.; Estabrooks, C. Characteristics and Unmet Care Needs of Unbefriended Residents in Long-Term Care: A Qualitative Interview Study. Aging Ment. Health 2020, 24, 659–667. [Google Scholar] [CrossRef]
- Chan, H.Y.; Pang, S.M. Quality of Life Concerns and End-of-Life Care Preferences of Aged Persons in Long-Term Care Facilities. J. Clin. Nurs. 2007, 16, 2158–2166. [Google Scholar] [CrossRef]
- Chu, L.W.; Luk, J.K.H.; Hui, E.; Chiu, P.K.C.; Chan, C.S.Y.; Kwan, F.; Kwok, T.; Lee, D.; Woo, J. Advance Directive and End-of-Life Care Preferences Among Chinese Nursing Home Residents in Hong Kong. J. Am. Med. Dir. Assoc. 2011, 12, 143–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chuang, Y.-H.; Abbey, J.-A.; Yeh, Y.-C.; Tseng, J.; Liu, M.-F. As They See It: A Qualitative Study of How Older Residents in Nursing Homes Perceive Their Care Needs. Collegian 2015, 22, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Cooney, A.; Murphy, K.; O’Shea, E. Resident Perspectives of the Determinants of Quality of Life in Residential Care in Ireland. J. Adv. Nurs. 2009, 65, 1029–1038. [Google Scholar] [CrossRef]
- Ferreira, A.R.; Dias, C.C.; Fernandes, L. Needs in Nursing Homes and Their Relation with Cognitive and Functional Decline, Behavioral and Psychological Symptoms. Front. Aging Neurosci. 2016, 8, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franklin, L.L.; Ternestedt, B.-M.; Nordenfelt, L. Views on Dignity of Elderly Nursing Home Residents. Nurs. Ethics 2006, 13, 130–146. [Google Scholar] [CrossRef]
- Funk, L.M. Who Wants to Be Involved? Decision-Making Preferences among Residents of Long-Term Care Facilities. Can. J. Aging 2004, 23, 47–58. [Google Scholar] [CrossRef]
- Gjerberg, E.; Lillemoen, L.; Førde, R.; Pedersen, R. End-of-Life Care Communications and Shared Decision-Making in Norwegian Nursing Homes—Experiences and Perspectives of Patients and Relatives. BMC Geriatr. 2015, 15, 103. [Google Scholar] [CrossRef] [Green Version]
- Goodman, C.; Amador, S.; Elmore, N.; Machen, I.; Mathie, E. Preferences and Priorities for Ongoing and End-of-Life Care: A Qualitative Study of Older People with Dementia Resident in Care Homes. Int. J. Stud. Nurs. 2013, 50, 1639–1647. [Google Scholar] [CrossRef] [Green Version]
- Hancock, G.A.; Woods, B.; Challis, D.; Orrell, M. The Needs of Older People with Dementia in Residential Care. Int. J. Geriat. Psychiatry 2006, 21, 43–49. [Google Scholar] [CrossRef]
- Heid, A.R.; Bangerter, L.R.; Abbott, K.M.; van Haitsma, K. Do Family Proxies Get It Right? Concordance in Reports of Nursing Home Residents’ Everyday Preferences. J. Appl. Gerontol. 2017, 36, 667–691. [Google Scholar] [CrossRef] [Green Version]
- Heid, A.R.; Abbott, K.M.; Kleban, M.; Rovine, M.J.; van Haitsma, K. The Impact of Nursing Home Residents’ Characteristics on Ratings of Importance of Autonomy Preferences in Daily Care over Time. Aging Ment. Health 2020, 24, 1334–1341. [Google Scholar] [CrossRef] [PubMed]
- Heusinger, J.; Dummert, S. Gender-specific needs of nursing home residents: Focus on personal hygiene. Z. Gerontol. Geriat. 2016, 49, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Housen, P.; Shannon, G.R.; Simon, B.; Edelen, M.O.; Cadogan, M.P.; Jones, M.; Buchanan, J.; Saliba, D. Why Not Just Ask the Resident? Refinement of a Preference Assessment Tool for Nursing Homes. J. Gerontol. Nurs. 2009, 35, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Kane, R.A.; Caplan, A.L.; Urv-Wong, E.K.; Freeman, I.C.; Aroskar, M.A.; Finch, M. Everyday Matters in the Lives of Nursing Home Residents: Wish for and Perception of Choice and Control. J. Am. Geriatr. Soc. 1997, 45, 1086–1093. [Google Scholar] [CrossRef]
- Klemmt, M.; Henking, T.; Heizmann, E.; Best, L.; Oorschot, B.; Neuderth, S. Wishes and Needs of Nursing Home Residents and Their Relatives Regarding End-of-life Decision-making and Care Planning—A Qualitative Study. J. Clin. Nurs. 2020, 29, 2663–2674. [Google Scholar] [CrossRef]
- Kurkowski, S.; Heckel, M.; Volland-Schüssel, K. Wishes of nursing home residents for their dying. Z. Gerontol. Geriat. 2018, 51, 912–920. [Google Scholar] [CrossRef]
- Levy-Storms, L.; Schnelle, J.F.; Simmons, S.F. A Comparison of Methods to Assess Nursing Home Residents’ Unmet Needs. Gerontologist 2002, 42, 454–461. [Google Scholar] [CrossRef] [Green Version]
- Man-Ging, C.I.; Öven Uslucan, J.; Fegg, M.; Frick, E.; Büssing, A. Reporting Spiritual Needs of Older Adults Living in Bavarian Residential and Nursing Homes. Ment. Health Relig. Cult. 2015, 18, 809–821. [Google Scholar] [CrossRef]
- Mazurek, J.; Szcześniak, D.; Talarska, D.; Wieczorowska-Tobis, K.; Kropińska, S.; Kachaniuk, H.; Rymaszewska, J. Needs Assessment of Elderly People Living in Polish Nursing Homes. Geriatr. Ment. Health Care 2015, 2, 9–15. [Google Scholar] [CrossRef]
- Michelson, C.; Mulvihill, M.; Hsu, M.A.; Olson, E. Eliciting Medical Care Preferences from Nursing Home Residents. Gerontologist 1991, 31, 358–363. [Google Scholar] [CrossRef]
- Milke, D.L.; Beck, C.H.M.; Danes, S. Meeting the Needs in Continuing Care of Facility-Based Residents Diagnosed With Dementia: Comparison of Ratings by Families, Direct Care Staff, and Other Staff. J. Appl. Gerontol. 2006, 25, 103–119. [Google Scholar] [CrossRef]
- Milte, R.; Ratcliffe, J.; Chen, G.; Miller, M.; Crotty, M. Taste, Choice and Timing: Investigating Resident and Carer Preferences for Meals in Aged Care Homes: Meal Preferences in Aged Care Homes. Nurs. Health Sci. 2018, 20, 116–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mroczek, B.; Kurpas, D.; Gronowska, M.; Kotwas, A.; Karakiewicz, B. Psychosexual Needs and Sexual Behaviors of Nursing Care Home Residents. Arch. Gerontol. Geriatr. 2013, 57, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Nakrem, S.; Vinsnes, A.G.; Seim, A. Residents’ Experiences of Interpersonal Factors in Nursing Home Care: A Qualitative Study. Int. J. Nurs. Stud. 2011, 48, 1357–1366. [Google Scholar] [CrossRef]
- Ni, P.; Zhou, J.; Wang, Z.X.; Nie, R.; Phillips, J.; Mao, J. Advance Directive and End-of-Life Care Preferences among Nursing Home Residents in Wuhan, China: A Cross-Sectional Study. J. Am. Med. Dir. Assoc. 2014, 15, 751–756. [Google Scholar] [CrossRef]
- Nikmat, A.W.; Almashoor, S.H. Older adults with cognitive impairment living in Malaysian nursing homes—Have we met their needs? ASEAN J. Psychiatry 2015, 16, 14–24. [Google Scholar]
- O’Neill, M.; Ryan, A.; Tracey, A.; Laird, L. ‘Waiting and Wanting’: Older Peoples’ Initial Experiences of Adapting to Life in a Care Home: A Grounded Theory Study. Ageing Soc. 2020, 42, 351–375. [Google Scholar] [CrossRef]
- Orrell, M.; Hancock, G.; Hoe, J.; Woods, B.; Livingston, G.; Challis, D.A. Cluster Randomised Controlled Trial to Reduce the Unmet Needs of People with Dementia Living in Residential Care. Int. J. Geriat. Psychiatry 2007, 22, 1127–1134. [Google Scholar] [CrossRef]
- Orrell, M.; Hancock, G.A.; Liyanage, K.C.G.; Woods, B.; Challis, D.; Hoe, J. The Needs of People with Dementia in Care Homes: The Perspectives of Users, Staff and Family Caregivers. Int. Psychogeriatr. 2008, 20, 941–951. [Google Scholar] [CrossRef]
- Paque, K.; Bastiaens, H.; van Bogaert, P.; Dilles, T. Living in a Nursing Home: A Phenomenological Study Exploring Residents’ Loneliness and Other Feelings. Scand. J. Caring Sci. 2018, 32, 1477–1484. [Google Scholar] [CrossRef]
- Reynolds, K.; Henderson, M.; Schulman, A.; Hanson, L.C. Needs of the Dying in Nursing Homes. J. Palliat. Med. 2002, 5, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Riedl, M.; Mantovan, F.; Them, C. Being a Nursing Home Resident: A Challenge to One’s Identity. Nurs. Res. Pract. 2013, 2013, 932381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, T.J.; Gilmore-Bykovskyi, A.; Lor, M.; Liebzeit, D.; Crnich, C.J.; Saliba, D. Important Care and Activity Preferences in a Nationally Representative Sample of Nursing Home Residents. J. Am. Med. Dir. Assoc. 2018, 19, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Roszman, A.; Zuralska, R.; Sitek, E.; Slawek, J.; Skrzypek-Czerko, M.; Domagala, P.; Mziray, M. Needs assessment of long term care Institutions residents with dementia. Acta Neuropsychol. 2014, 12, 65–72. [Google Scholar]
- Schenk, L.; Meyer, R.; Behr, A.; Kuhlmey, A.; Holzhausen, M. Quality of Life in Nursing Homes: Results of a Qualitative Resident Survey. Qual. Life Res. 2013, 22, 2929–2938. [Google Scholar] [CrossRef]
- Schmidt, H.; Eisenmann, Y.; Golla, H.; Voltz, R.; Perrar, K.M. Needs of People with Advanced Dementia in Their Final Phase of Life: A Multi-Perspective Qualitative Study in Nursing Homes. Palliat. Med. 2018, 32, 657–667. [Google Scholar] [CrossRef]
- Sonntag, A.; Bischkopf, J.; Ritz, A.; Jakob, A.; Angermeyer, M.C. Wishes of nursing home residents concerning their life situation—Results of a qualitative study. Z. Gerontol. Geriat. 2003, 36, 280–286. [Google Scholar] [CrossRef]
- Strohbuecker, B.; Eisenmann, Y.; Galushko, M.; Montag, T.; Voltz, R. Palliative Care Needs of Chronically Ill Nursing Home Residents in Germany: Focusing on Living, Not Dying. Int. J. Palliat. Nurs. 2011, 17, 27–34. [Google Scholar] [CrossRef]
- Tobis, S.; Wieczorowska-Tobis, K.; Talarska, D.; Pawlaczyk, M.; Suwalska, A. Needs of Older Adults Living in Long-Term Care Institutions: An Observational Study Using Camberwell Assessment of Need for the Elderly. Clin. Interv. Aging 2018, 13, 2389–2395. [Google Scholar] [CrossRef] [Green Version]
- Van der Ploeg, E.S.; Bax, D.; Boorsma, M.; Nijpels, G.; van Hout, H.P. A Cross-Sectional Study to Compare Care Needs of Individuals with and without Dementia in Residential Homes in the Netherlands. BMC Geriatr. 2013, 13, 51. [Google Scholar] [CrossRef] [Green Version]
- Van der Steen, J.T.; Van Soest-Poortvliet, M.C.; Achterberg, W.P.; Ribbe, M.W.; De Vet, H.C.W. Family Perceptions of Wishes of Dementia Patients Regarding End-of-Life Care. Int. J. Geriat. Psychiatry 2011, 26, 217–220. [Google Scholar] [CrossRef]
- Van Oorschot, B.; Mücke, K.; Cirak, A.; Henking, T.; Neuderth, S. Desired place of death, living will and desired care at end of life: Initial results of a survey of nursing home residents. Z. Gerontol. Geriat. 2019, 52, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Wieczorowska-Tobis, K.; Talarska, D.; Kropińska, S.; Jaracz, K.; Tobis, S.; Suwalska, A.; Kachaniuk, H.; Mazurek, J.; Dymek-Skoczyńska, A.; Rymaszewska, J. The Camberwell Assessment of Need for the Elderly Questionnaire as a Tool for the Assessment of Needs in Elderly Individuals Living in Long-Term Care Institutions. Arch. Gerontol. Geriatr. 2016, 62, 163–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schweighart, R.; Klemmt, M.; Neuderth, S.; Teti, A. Experiences and perspectives of nursing home residents with depressive symptoms during the COVID-19 pandemic: A qualitative study. Z. Gerontol. Geriat. 2021, 54, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Diehl, E.; Rieger, S.; Letzel, S.; Schablon, A.; Nienhaus, A.; Escobar Pinzon, L.C.; Dietz, P. The Relationship between Workload and Burnout among Nurses: The Buffering Role of Personal, Social and Organisational Resources. PLoS ONE 2021, 16, e0245798. [Google Scholar] [CrossRef]
- Drennan, V.M.; Ross, F. Global Nurse Shortages—The Facts, the Impact and Action for Change. Br. Med. Bull. 2019, 130, 25–37. [Google Scholar] [CrossRef]
- Andela, M.; Truchot, D.; Huguenotte, V. Job Demands, Emotional Dissonance and Elderly Abuse: The Moderating Role of Organizational Resources. J. Elder Abus. Negl. 2018, 30, 368–384. [Google Scholar] [CrossRef]
- Bagchus, C.; Dedding, C.; Bunders, J.F.G. ‘I’m Happy That I Can Still Walk’—Participation of the Elderly in Home Care as a Specific Group with Specific Needs and Wishes. Health Expect. 2015, 18, 2183–2191. [Google Scholar] [CrossRef] [Green Version]
- Ryan, E.B.; Hamilton, J.M.; See, S.K. Patronizing the Old: How Do Younger and Older Adults Respond to Baby Talk in the Nursing Home? Int. J. Aging Hum. Dev. 1994, 39, 21–32. [Google Scholar] [CrossRef]
- Ryan, E.B.; Hummert, M.L.; Boich, L.H. Communication Predicaments of Aging: Patronizing Behavior toward Older Adults. J. Lang. Soc. Psychol. 1995, 14, 144–166. [Google Scholar] [CrossRef]
- Williams, K.; Shaw, C.; Lee, A.; Kim, S.; Dinneen, E.; Turk, M.; Jao, Y.-L.; Liu, W. Voicing Ageism in Nursing Home Dementia Care. J. Gerontol. Nurs. 2017, 43, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Ballard, C.; Corbett, A.; Orrell, M.; Williams, G.; Moniz-Cook, E.; Romeo, R.; Woods, B.; Garrod, L.; Testad, I.; Woodward-Carlton, B.; et al. Impact of Person-Centred Care Training and Person-Centred Activities on Quality of Life, Agitation, and Antipsychotic Use in People with Dementia Living in Nursing Homes: A Cluster-Randomised Controlled Trial. PLoS Med. 2018, 15, e1002500. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.N. Improving Outcomes of Nursing Home Interactions. Res. Nurs. Health 2006, 29, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Reed, A.E.; Mikels, J.A.; Simon, K.I. Older Adults Prefer Less Choice than Young Adults. Psychol. Aging 2008, 23, 671–675. [Google Scholar] [CrossRef]
- Asadi-Lari, M.; Packham, C.; Gray, D. Need for redefining needs. Health Qual. Life Outcomes 2003, 1, 34. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).