Evaluating a Novel Extended Scope of Occupational Therapy Service Aimed at Hospital Avoidance in Tasmania, Australia, from the Perspective of Stakeholders
Abstract
:1. Introduction
2. Materials and Methods
2.1. Characteristics and Recruitment of Participants
2.2. Data Collection
- Priority 1 = urgent, to be responded to within 24 h
- Priority 2 = semi-urgent, to be responded to within 3 days
- Priority 3 = less urgent, to be responded to within 5 days
2.3. Data Analysis
3. Results
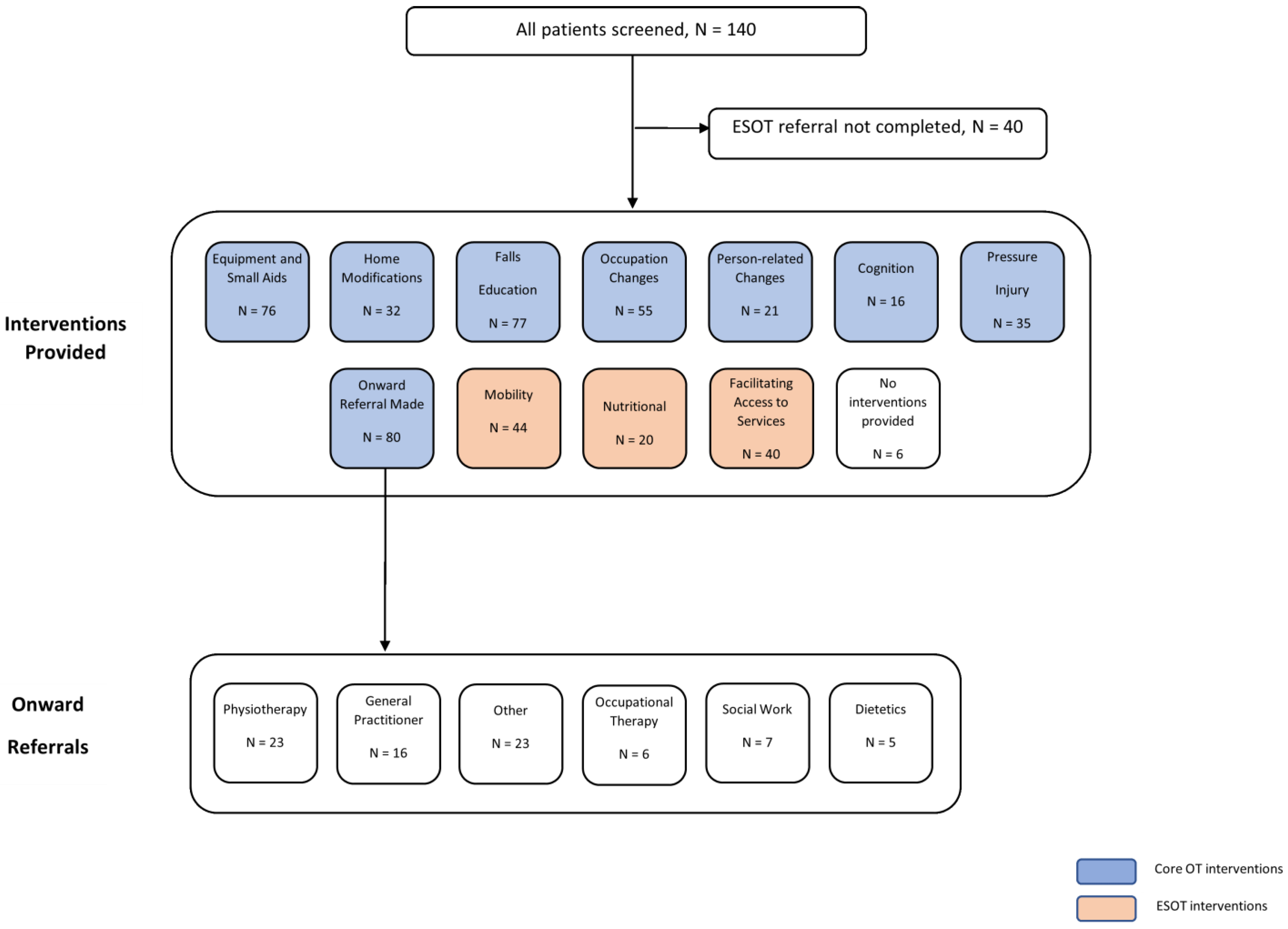
3.1. Quantitative Findings
3.2. Qualitative Findings
3.2.1. Global Theme 1: Staying at Home Is Preferred
“He doesn’t want to leave home, it is his world.”
3.2.2. Global Theme 2: Preventing Falls through Tools and Education
“I don’t have to watch him all the time now.”
3.2.3. Global Theme 3: Feeling Important
“She had time for him and explained it to him in such a way that he understood.”
“If you have someone sick (in your family) you don’t know where to get help.”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Australia’s Health 2018; AIHW: Canberra, Australia, 2018.
- Morley, C.; Stankovich, J.; Peterson, G.; Kinsman, L. Planning for the future: Emergency department presentation patterns in Tasmania, Australia. Int. Emerg. Nurs. 2018, 38, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Regional Population by Age and Sex. Available online: https://www.abs.gov.au/statistics/people/population/regional-population-age-and-sex/latest-release#key-statistics (accessed on 18 January 2022).
- Australian Institute of Health and Welfare. Emergency Department Care 2017–18: Australian Hospital Statistics. Available online: https://www.aihw.gov.au/reports/hospitals/emergency-department-care-2017-18 (accessed on 18 January 2022).
- Salter, A.E.; Khan, K.M.; Donaldson, M.G.; Davis, J.C.; Buchanan, J.; Abu-Laban, R.B.; Cook, W.L.; Lord, S.R.; McKay, H.A. Community-dwelling seniors who present to the emergency department with a fall do not receive Guideline care and their fall risk profile worsens significantly: A 6-month prospective study. Osteoporos. Int. 2006, 17, 672–683. [Google Scholar] [CrossRef]
- Bloch, F.; Jegou, D.; Dhainaut, J.-F.; Rigaud, A.-S.; Coste, J.; Lundy, J.-E.; Claessens, Y.-E. Do ED staffs have a role to play in the prevention of repeat falls in elderly patients? Am. J. Emerg. Med. 2009, 27, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Russell, M.A.; Hill, K.D.; Day, L.M.; Blackberry, I.; Schwartz, J.; Giummarra, M.J.; Dorevitch, M.; Ibrahim, J.E.; Dalton, A.C.; Dharmage, S.C. A randomized controlled trial of a multifactorial falls prevention intervention for older fallers presenting to emergency departments. J. Am. Geriatr. Soc. 2010, 58, 2265–2274. [Google Scholar] [CrossRef] [PubMed]
- Close, J.; Ellis, M.; Hooper, R.; Glucksman, E.; Jackson, S.; Swift, C. Prevention of falls in the elderly trial (PROFET): A randomised controlled trial. Lancet 1999, 353, 93–97. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Disease Expenditure in Australia. Available online: https://www.aihw.gov.au/reports/health-welfare-expenditure/disease-expenditure-australia (accessed on 18 January 2022).
- McPherson, K.; Kersten, P.; George, S.; Lattimer, V.; Breton, A.; Ellis, B.; Kaur, D.; Frampton, G. A systematic review of evidence about extended roles for allied health professionals. J. Health Serv. Res. Policy 2006, 11, 240–247. [Google Scholar] [CrossRef]
- Saxon, R.L.; Gray, M.A.; Oprescu, F.I. Extended roles for allied health professionals: An updated systematic review of the evidence. J. Multidiscip. Healthc. 2014, 7, 479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopewell, S.; Adedire, O.; Copsey, B.J.; Boniface, G.J.; Sherrington, C.; Clemson, L.; Close, J.C.; Lamb, S.E. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2018, 7, Cd012221. [Google Scholar] [CrossRef] [PubMed]
- Middlebrook, S.; Mackenzie, L. The Enhanced Primary Care program and falls prevention: Perceptions of private occupational therapists and physiotherapists. Australas J. Ageing 2012, 31, 72–77. [Google Scholar] [CrossRef]
- Cumming, R.G.; Thomas, M.; Szonyi, G.; Salkeld, G.; O’Neill, E.; Westbury, C.; Frampton, G. Home visits by an occupational therapist for assessment and modification of environmental hazards: A randomized trial of falls prevention. J. Am. Geriatr. Soc. 1999, 47, 1397–1402. [Google Scholar] [CrossRef]
- Mackenzie, L.; Clemson, L.; Roberts, C. Occupational therapists partnering with general practitioners to prevent falls: Seizing opportunities in primary health care. Aust. Occup. Ther. J. 2013, 60, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, L.; Clemson, L.; Irving, D. Fall prevention in primary care using chronic disease management plans: A process evaluation of provider and consumer perspectives. Aust. Occup. Ther. J. 2020, 67, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Lau, G.W.C.; Yu, M.-L.; Brown, T.; Locke, C. Clients’ Perspectives of the Effectiveness of Home Modification Recommendations by Occupational Therapists. Occup. Ther. Health Care 2018, 32, 230–250. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Human Services. Royal Hobart Hospital 2022. Available online: https://www.dhhs.tas.gov.au/hospital/royal-hobart-hospital/information_for_patients_and_visitors2/rhh_patient_information_guide/welcome (accessed on 15 April 2022).
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th ed.; SAGE: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Kroll, T.; Neri, M. Designs for mixed methods research. Mix. Methods Res. Nurs. Health Sci. 2009, 31, 31–49. [Google Scholar]
- Russell, M.A.; Hill, K.D.; Blackberry, I.; Day, L.M.; Dharmage, S.C. The reliability and predictive accuracy of the falls risk for older people in the community assessment (FROP-Com) tool. Age Ageing 2008, 37, 634–639. [Google Scholar] [CrossRef] [Green Version]
- Russell, M.A.; Hill, K.D.; Day, L.M.; Blackberry, I.; Gurrin, L.C.; Dharmage, S.C. Development of the Falls Risk for Older People in the Community (FROP-Com) screening tool. Age Ageing 2009, 38, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Bergstrom, N. The Braden Scale for predicting pressure sore risk. Nurs. Res. 1987, 36, 205–210. [Google Scholar] [CrossRef]
- Ferguson, M.; Capra, S.; Bauer, J.; Banks, M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999, 15, 458–464. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 2033.0.55.001—Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia. 2016. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~IRSD%20Interactive%20Map~15 (accessed on 8 April 2022).
- Attride-Stirling, J. Thematic networks: An analytic tool for qualitative research. Qual. Res. 2001, 1, 385–405. [Google Scholar] [CrossRef]
- Gulliford, M.; Naithani, S.; Morgan, M. What is ’continuity of care’? J. Health Serv. Res. Policy 2006, 11, 248–250. [Google Scholar] [CrossRef]
- Ben-Tovim, D.I.; Bassham, J.E.; Bolch, D.; Martin, M.A.; Dougherty, M.; Szwarcbord, M. Lean thinking across a hospital: Redesigning care at the Flinders Medical Centre. Aust. Health Rev. 2007, 31, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 9, 1–366. [Google Scholar] [CrossRef]
- Cereda, E.; Pedrolli, C.; Klersy, C.; Bonardi, C.; Quarleri, L.; Cappello, S.; Turri, A.; Rondanelli, M.; Caccialanza, R. Nutritional status in older persons according to healthcare setting: A systematic review and meta-analysis of prevalence data using MNA®. Clin. Nutr. 2016, 35, 1282–1290. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.H.; Sandhu, N.; Coleman, K.; Phillips, K.E.; Sugarman, J.R. Improving care coordination in primary care. Med. Care 2014, 52, S33–S38. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, H.M.; Pearson, M.; Sheaff, R.; Asthana, S.; Wheat, H.; Sugavanam, T.P.; Britten, N.; Valderas, J.; Bainbridge, M.; Witts, L. Collaborative action for person-centred coordinated care (P3C): An approach to support the development of a comprehensive system-wide solution to fragmented care. Health Res. Policy Syst. 2017, 15, 98. [Google Scholar] [CrossRef] [Green Version]
- Mackenbach, J.P. Socioeconomic inequalities in health in high-income countries: The facts and the options. In Oxford Textbook of Global Public Health, 6th ed.; Detels, R., Gulliford, M., Karim, Q.A., Tan, C.C., Eds.; Oxford University Press: Oxford, UK, 2015; Volume 1. [Google Scholar]
- Thomson, H.; Thomas, S.; Sellstrom, E.; Petticrew, M. Housing improvements for health and associated socio-economic outcomes. Cochrane Database Syst. Rev. 2013, 2, CD008657. [Google Scholar] [CrossRef] [Green Version]
- Woo, B.F.Y.; Lee, J.X.Y.; San Tam, W.W. The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: A systematic review. Hum. Resour. Health 2017, 15, 63. [Google Scholar] [CrossRef]
- Stanik-Hutt, J.; Newhouse, R.P.; White, K.M.; Johantgen, M.; Bass, E.B.; Zangaro, G.; Wilson, R.; Fountain, L.; Steinwachs, D.M.; Heindel, L. The quality and effectiveness of care provided by nurse practitioners. J. Nurse Pract. 2013, 9, 492–500.e413. [Google Scholar] [CrossRef]
- Harnett, N.; Bak, K.; Lockhart, E.; Ang, M.; Zychla, L.; Gutierrez, E.; Warde, P. The Clinical Specialist Radiation Therapist (CSRT): A case study exploring the effectiveness of a new advanced practice role in Canada. J. Med. Radiat. Sci. 2018, 65, 86–96. [Google Scholar] [CrossRef]
- College of Occupational Therapists—Urgent Care: The Value of Occupational Therapy; College of Occupational Therapists: London, UK, 2015.
- Sach, T.H.; Logan, P.; Coupland, C.; Gladman, J.; Sahota, O.; Stoner-Hobbs, V.; Robertson, K.; Tomlinson, V.; Ward, M.; Avery, A. Community falls prevention for people who call an emergency ambulance after a fall: An economic evaluation alongside a randomised controlled trial. Age Ageing 2012, 41, 635–641. [Google Scholar] [CrossRef] [Green Version]
- Davis, R.; Rodd, R. Proving the effectiveness of community occupational therapy in the equipment and adaptation setting using the Canadian Occupational Performance Measure. Br. J. Occup. Ther. 2014, 77, 91–95. [Google Scholar] [CrossRef]
- Johansson, A.; Björklund, A. The impact of occupational therapy and lifestyle interventions on older persons’ health, well-being, and occupational adaptation. Scand. J. Occup. Ther. 2016, 23, 207–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turcotte, P.L.; Carrier, A.; Desrosiers, J. Are health promotion and prevention interventions integrated into occupational therapy practice with older adults having disabilities? Insights from six community health settings in Québec, Canada. Aust. Occup. Ther. J. 2016, 62, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. J. Aging Ment. Health 1986, 5, 165–173. [Google Scholar]

| n | % | |
|---|---|---|
| Age, mean (SD) (years) | 76.8 | (12.4) |
| Male | 53 | (37.9) |
| Female | 87 | (62.1) |
| Lived Alone | 61 | (43.6) |
| Index of Relative Socio-economic Disadvantage | ||
| Quintile 1 (most disadvantaged) | 54 | 38.6 |
| Quintile 2 | 4 | 2.9 |
| Quintile 3 | 27 | 19.3 |
| Quintile 4 | 28 | 20.0 |
| Quintile 5 (most advantaged) | 27 | 19.3 |
| Falls in past 12 months | ||
| None | 78 | (55.7) |
| 1 | 23 | (16.4) |
| 2 | 16 | (11.4) |
| 3+ | 23 | (16.4) |
| No. Reasons for Referral † | ||
| 1 | 24 | (20.7) |
| 2 | 44 | (31.4) |
| 3 | 32 | (22.9) |
| 4 | 24 | (17.1) |
| 5 | 7 | (5) |
| 6 | 4 | (2.9) |
| Assessment | n | % |
|---|---|---|
| Braden Scale Score | ||
| Moderate (13–14) | 8 | (8) |
| Mild (15–18) | 24 | (24) |
| None (19–23) | 38 | (38) |
| Not scored | 30 | (30) |
| Malnutrition Screening Tool Score | ||
| High (3–5) | 9 | (9) |
| Moderate (2) | 9 | (9) |
| Low (0–1) | 52 | (52) |
| Not scored | 30 | (30) |
| Falls Risk for Older People in the Community Category | ||
| High (4–9) | 45 | (45) |
| Low (0–3) | 16 | (16) |
| Not scored | 39 | (39) |
| Referral Category | n | % |
|---|---|---|
| 1 (within 24 h) | 35/37 | 94.6% |
| 2 (within 3 days) | 37/49 | 75.5% |
| 3 (within 5 days) | 8/14 | 57.1% |
| Outcome | n | % |
|---|---|---|
| Addressed significant risk/prevented imminent admission | 81 | 81 |
| Advocated admission | 6 | 6 |
| Requiring care not provided by ESOT service | 7 | 7 |
| Not stated | 6 | 6 |
| Total | 100 | 100 |
| Intervention Type | Total Interventions Provided | Median No. of Interventions Per Subject |
|---|---|---|
| Core Occupational Therapist | 392 | 4 |
| Extended Scope Occupational Therapist | 104 | 1 |
| Core + ESOT overall | 496 | 4 |
| Question | Strongly Agree | Agree | Disagree | Strongly Disagree | Do Not Know | Total |
|---|---|---|---|---|---|---|
| The service made it easy for me to refer to Allied Health | 18 (60%) | 7 (23.33%) | 1 (3.33%) | 0 (0%) | 4 (13.33%) | 30 |
| I was able to get timely allied health services for the client I referred | 20 (66.67%) | 4 (13.33%) | 0 (0%) | 0 (0%) | 6 (20%) | 30 |
| The service supported comprehensive care of the client/s I referred | 20 (66.67%) | 4 (13.33%) | 0 (0%) | 0 (0%) | 6 (20%) | 30 |
| The service supported the people I referred to avoid emergency presentation or hospital admission | 18 (60%) | 5 (16.67%) | 0 (0%) | 0 (0%) | 7 (23.33%) | 30 |
| The service should continue | 24 (80%) | 2 (6.67%) | 0 (0%) | 0 (0%) | 4 (13.33%) | 30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Dam, P.J.; Reid, L.; Elliott, S.; Dwyer, M. Evaluating a Novel Extended Scope of Occupational Therapy Service Aimed at Hospital Avoidance in Tasmania, Australia, from the Perspective of Stakeholders. Healthcare 2022, 10, 842. https://doi.org/10.3390/healthcare10050842
Van Dam PJ, Reid L, Elliott S, Dwyer M. Evaluating a Novel Extended Scope of Occupational Therapy Service Aimed at Hospital Avoidance in Tasmania, Australia, from the Perspective of Stakeholders. Healthcare. 2022; 10(5):842. https://doi.org/10.3390/healthcare10050842
Chicago/Turabian StyleVan Dam, Pieter Jan, Leah Reid, Sarah Elliott, and Mitchell Dwyer. 2022. "Evaluating a Novel Extended Scope of Occupational Therapy Service Aimed at Hospital Avoidance in Tasmania, Australia, from the Perspective of Stakeholders" Healthcare 10, no. 5: 842. https://doi.org/10.3390/healthcare10050842
APA StyleVan Dam, P. J., Reid, L., Elliott, S., & Dwyer, M. (2022). Evaluating a Novel Extended Scope of Occupational Therapy Service Aimed at Hospital Avoidance in Tasmania, Australia, from the Perspective of Stakeholders. Healthcare, 10(5), 842. https://doi.org/10.3390/healthcare10050842







