The Communication Challenges and Strength of Nurses’ Intensive Corona Care during the Two First Pandemic Waves: A Qualitative Descriptive Phenomenology Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants and Procedure
2.3. Research Tools
2.4. Data Collection and Analysis
2.5. Trustworthiness
2.6. Ethical Considerations
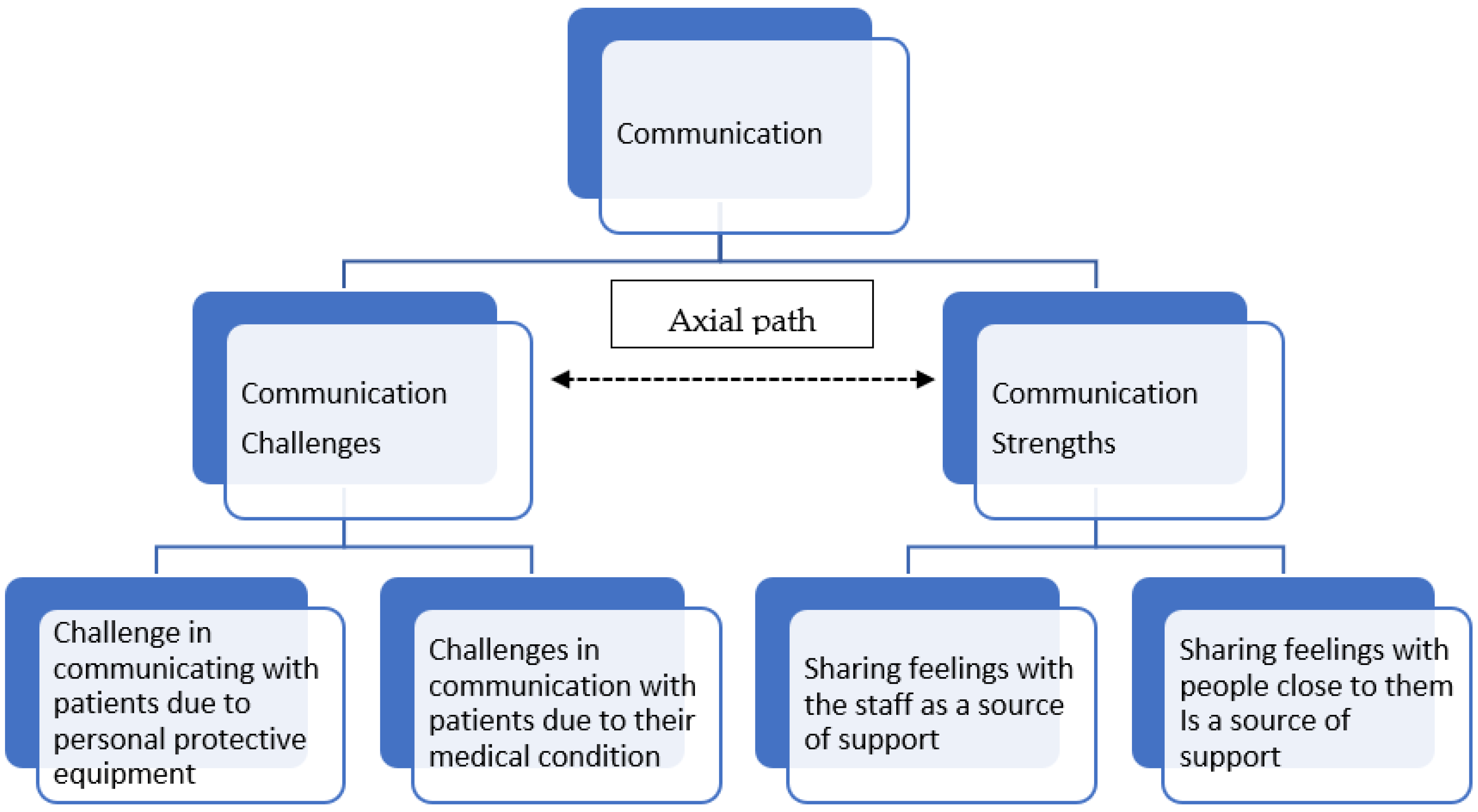
3. Findings
“At the beginning of the pandemic, I felt a great struggle with the communication with patients, however as time went on I also started to see the positive side regarding my ability to communicate with the staff....suddenly they started to understand me almost without any words, it improves my work with them. We became a winning team.”(ICCU nurse, 29 years old, 8 months experience.)
“You can see the communication competence in two ways. One view is that it is very difficult to communicate with patients with respiratory aids. However, another view is that it makes us, as a team, more bonded and more qualified.”(ICCU nurse, 35 years old, 5 months experience.)
3.1. Communication Challenges
3.2. Challenge in Communicating with Patients Due to Personal Protective Equipment (PPE)
“I found it difficult to breathe and hear. Work was very difficult because I could not see well because of the mask, there was steam. When I spoke to the patients and tried to communicate with them, they couldn’t really see my facial expression, I felt I had to shout for them to hear and understand me.”(ICCU nurse, 26 years old, 9 months experience.)
“I begin my shift and care for people, but they cannot see my face, my smile, they cannot see my mouth speaking, this is frustrating. I’m talking about basic communication, the most basic impressions, even that was faulty.” (ICCU nurse, 29 years old, 8 months experience.) The communication-related effort was so great that it made the caregivers uncomfortable.
“Communication was very difficult, very challenging. I had a shield and an N-95 mask, so it was almost impossible to speak. My mouth was dry, and I longed for air… The patients found it very difficult to hear us. Most of the time I wasn’t sure whether or not they had understood what I said.”(ICCU nurse, 37 years old, 5 months experience.)
“The mask made it very difficult for me to speak. I am used to verbal communication together with facial expressions, presenting myself in a manner best for the patient, and suddenly they couldn’t see my face and it was difficult for them to hear me. I used a lot of hand gestures, and sometimes wrote what I wanted to say on a whiteboard. There is no doubt that there was much difficulty in interpersonal communication.”(ICCU nurse, 35 years old, 10 months experience.)
3.3. Challenges in Communication with Patients Due to Their Medical Condition
“When I was in the COVID-19 ward, patients were anesthetized and ventilated, so there was no communication between us, and I couldn’t understand what they were feeling. There were very few patients whose medical condition allowed them to communicate.”(ICCU nurse, 35 years old, 8 months experience.)
“Most patients were anesthetized and ventilated, so it was extremely difficult and challenging to communicate. With the few patients who were not ventilated, I identified myself by the name, I presented myself. I explained that they could not see me. But with the ventilated patients, I don’t know… but I said that I was there, and I could hear, and they could speak to me.”(ICCU nurse, 37 years old, 5 months experience.)
“You take care of them and speak to them but you don’t know what they can hear or understand if anything… Most of them are ventilated and connected to ventilation aids such as a ventilation machine… People don’t see faces, don’t see a smile, you don’t know whether or not they are in pain, whether or not the treatment is helping, they can’t say… this is extremely frustrating.”(ICCU nurse, 26 years old, 9 months experience.)
“Of course, there was no real communication, most patients had already been anesthetized and ventilated.”(ICCU nurse, 37 years old, 5 months experience.)
“It is known that compassion and empathy contribute to a patient’s recovery; however, I found it difficult to communicate compassionately and empathetically and not knowing whether the patient received it.”(ICCU nurse, 27 years old, 5 months experience.)
3.4. Communication Strengths
3.5. Sharing Feelings with the Staff as a Source of Support
“Look, the people I work with understand me, the staff. Sometimes I also talk to family and friends, and they understand less. And even if they do understand, it’s not like the way the staff understands me. It’s different.”(ICCU nurse, 27 years old, 5 months experience.)
“I mostly share with the staff. I have an amazing staff; we are each other’s psychologists. We deal with this thing together, as a group. We had some sort of powerful consolidation among the staff, and that’s really what made the work we did together easier, that’s what helped.”(ICCU nurse, 26 years old, 12 months experience.)
“I think that the fact that we are experiencing this together, as a team, makes it much easier. It has helped us consolidate as a team, I think we discovered amazing abilities in each one of us, and our teamwork is also amazing. I always share with the staff because when we are on shift, we have the same experiences, so we have the same feelings, more or less.”(ICCU nurse, 30 years old, 7 months experience.)
“I think that the fact that we are experiencing this challenge in communication together allowed us, as a team, to look for other alternative ways for communication among us. Thus it helped us to be united as a team.”(ICCU nurse, 26 years old, 9 months experience.)
3.6. Sharing Feelings with People Close to Them Is a Source of Support
“Of course, I shared with my husband throughout. That’s obvious. He is my solid rock.”(ICCU nurse, 31 years old, 7 months experience.)
“I talked a lot about it with my husband. He was the person who always supported me.”(ICCU nurse, 37 years old, 5 months experience.)
“I shared with my husband and my friends, mostly my husband. He was always there. By the way, I shared with the children as well. They were always asking.”(ICCU nurse, 31 years old, 10 months experience.)
“I mostly share with my household. My husband relates to my experiences. I talk about it a lot at home, that’s part of the things that helped me deal with these things, I always had someone to share with.”(ICCU nurse, 31 years old, 8 months experience.)
“I also talked to the extended family, I told them how difficult it was. In these situations, why people don’t keep safe. I thought about them when I went home, yes.”(ICCU nurse, 27 years old, 10 months experience.)
“I talk to my wife, she is also a nurse, and she is in charge of ventilated patients. No, the feelings, I am extremely charged, I’m finding the situation very difficult, what I went through in the ICCU during the pandemic.”(ICCU male-nurse, 30 years old, 7 months experience.)
4. Discussion
4.1. Strengths and Limitations and Future Studies
4.2. Implications to Practice and Policy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- World Health Organization, Coronavirus disease 2019 (COVID-19) Situation Report—65. Available online: https://www.who.int/publications/m/item/situation-report---65 (accessed on 24 August 2021).
- World Health Organization Novel Coronavirus (2019-NCoV) Situation Report—10. 2020. Available online: https://apps.who.int/iris/handle/10665/330775 (accessed on 24 August 2021).
- Birenbaum-Carmeli, D.; Chassida, J. Health and Socio-Demographic Implications of the Covid-19 Second Pandemic Wave in Israel, Compared with the First Wave. Int. J. Equity Health 2021, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Álvarez, N.Y.; Vuelvas-Olmos, C.R. COVID-19: Psychological Effects and Associated Factors in Mexican Nurses. Disaster Med. Public Health Prep. 2020, 1–7. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.M.; Lin, C.C.; Lin, C.Y.; Chen, J.Y.; Chue, C.M.; Chou, P. Survey of Stress Reactions among Health Care Workers Involved with the SARS Outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.G.; Lancee, W.J.; Balderson, K.E.; Bennett, J.P.; Borgundvaag, B.; Evans, S.; Fernandes, C.M.B.; Goldbloom, D.S.; Gupta, M.; Hunter, J.J.; et al. Long-Term Psychological and Occupational Effects of Providing Hospital Healthcare during SARS Outbreak. Emerg. Infect. Dis. 2006, 12, 1924–1932. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.M.; Wong, J.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, C.-M.; Wong, P.-C.; Tsang, K.W.; Chua, S.E. Stress and Psychological Distress Among SARS Survivors 1 Year After the Outbreak. Can. J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [Green Version]
- Maunder, R.G.; Leszcz, M.; Savage, D.; Adam, M.A.; Peladeau, N.; Romano, D.; Rose, M.; Schulman, R.B. Applying the Lessons of SARS to Pandemic Influenza. Can. J. Public Health 2008, 99, 486–488. [Google Scholar] [CrossRef]
- Nissan, D.; Weiss, G.; Siman-Tov, M.; Spitz, A.; Bodas, M.; Shenhar, G.; Adini, B. Differences in Levels of Psychological Distress, Perceived Safety, Trust, and Efficacy amongst Hospital Personnel during the COVID-19 Pandemic. Res. Nurs. Health 2021, 44, 776–786. [Google Scholar] [CrossRef]
- Labrague, L.J.; de los Santos, J.A.A. Fear of COVID-19, Psychological Distress, Work Satisfaction and Turnover Intention among Frontline Nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef]
- Gunawan, J.; Aungsuroch, Y.; Marzilli, C.; Fisher, M.L.; Nazliansyah; Sukarna, A. A Phenomenological Study of the Lived Experience of Nurses in the Battle of COVID-19. Nurs. Outlook 2021, 69, 652–659. [Google Scholar] [CrossRef]
- Kameg, B.N. Psychiatric-Mental Health Nursing Leadership during Coronavirus Disease 2019 (COVID-19). J. Psychiatr. Ment. Health Nurs. 2021, 28, 507–508. [Google Scholar] [CrossRef]
- Shahrour, G.; Dardas, L.A. Acute Stress Disorder, Coping Self-Efficacy and Subsequent Psychological Distress among Nurses amid COVID-19. J. Nurs. Manag. 2020, 28, 1686–1695. [Google Scholar] [CrossRef] [PubMed]
- Wharton, C.; Kotera, Y.; Brennan, S. A Well-Being Champion and the Role of Self-Reflective Practice for ICU Nurses during COVID-19 and Beyond. Nurs. Crit. Care 2021, 26, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Moradi, Y.; Baghaei, R.; Hosseingholipour, K.; Mollazadeh, F. Challenges Experienced by ICU Nurses throughout the Provision of Care for COVID-19 Patients: A Qualitative Study. J. Nurs. Manag. 2021, 29, 1159–1168. [Google Scholar] [CrossRef]
- Lake, E.T.; Narva, A.M.; Holland, S.; Smith, J.G.; Cramer, E.; Rosenbaum, K.E.F.; French, R.; Clark, R.R.S.; Rogowski, J.A. Hospital Nurses’ Moral Distress and Mental Health during COVID-19. J. Adv. Nurs. 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De los Santos, J.A.A. COVID-19 Anxiety among Front-Line Nurses: Predictive Role of Organisational Support, Personal Resilience and Social Support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef]
- Halcomb, E.; Williams, A.; Ashley, C.; McInnes, S.; Stephen, C.; Calma, K.; James, S. The Support Needs of Australian Primary Health Care Nurses during the COVID-19 Pandemic. J. Nurs. Manag. 2020, 28, 1553–1560. [Google Scholar] [CrossRef]
- Houchens, N.; Tipirneni, R. Compassionate Communication amid the COVID-19 Pandemic. J. Hosp. Med. 2020, 15, 437–439. [Google Scholar] [CrossRef]
- Rose, L.; Yu, L.; Casey, J.; Cook, A.; Metaxa, V.; Pattison, N.; Rafferty, A.M.; Ramsay, P.; Saha, S.; Xyrichis, A.; et al. Communication and Virtual Visiting for Families of Patients in Intensive Care during the COVID-19 Pandemic: A UK National Survey. Ann. Am. Thorac. Soc. 2021, 18, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Liu, Y.; Wang, X.; Dong, H. Transition Shock, Preceptor Support and Nursing Competency among Newly Graduated Registered Nurses: A Cross-Sectional Study. Nurse Educ. Today 2021, 102, 104891. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.H.; Liu, J.E.; Bai, X.Y.; Yue, P.; Luo, S.X. Providing Targeted Psychological Support to Frontline Nurses Involved in the Management of COVID-19: An Action Research. J. Nurs. Manag. 2021, 29, 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, C.; Pan, W.; Zheng, J.; Gao, J.; Huang, X.; Cai, S.; Zhai, Y.; Latour, J.M.; Zhu, C. Stress, Burnout, and Coping Strategies of Frontline Nurses During the COVID-19 Epidemic in Wuhan and Shanghai, China. Front. Psychiatry 2020, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kılınç, T.; Sis Çelik, A. Relationship between the Social Support and Psychological Resilience Levels Perceived by Nurses during the COVID-19 Pandemic: A Study from Turkey. Perspect. Psychiatr. Care 2021, 57, 1000–1008. [Google Scholar] [CrossRef]
- van Manen, M. Phenomenology of Practice. Phenomenol. Prahctice 2007, 1, 11–30. [Google Scholar] [CrossRef] [Green Version]
- Husserl, E. Cartesian Meditations: An Introduction to Phenomenology; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Kaplan, A.F. Cultivating Supports While Venturing into Interviewing during COVID-19. Oral Hist. Rev. 2021, 47, 214–226. [Google Scholar] [CrossRef]
- Zoom Zoom Video Communications. Available online: https://zoom.us/ (accessed on 21 December 2020).
- DiCicco-Bloom, B.; Crabtree, B.F. The Qualitative Research Interview. Med. Educ. 2006, 40, 314–321. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the Framework Method for the Analysis of Qualitative Data in Multidisciplinary Health Research. BMC Med. Res. Methodol. 2013, 13, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Hochwald, I.H.; Yakov, G.; Radomyslsky, Z.; Danon, Y.; Nissanholtz-Gannot, R. Ethical Challenges in End-Stage Dementia: Perspectives of Professionals and Family Care-Givers. Nurs. Ethics 2021, 28, 1228–1243. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in Qualitative Research: Exploring Its Conceptualization and Operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.G.; Walls, R.M. Supporting the Health Care Workforce during the COVID-19 Global Epidemic. JAMA—J. Am. Med. Assoc. 2020, 323, 1439–1440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amin, S.; Chin, J.; Terrell, M.A.; Lomiguen, C.M. Addressing Challenges in Humanistic Communication During COVID-19 Through Medical Education. Front. Commun. 2021, 6, 1–6. [Google Scholar] [CrossRef]
- Bowers, B.; Pollock, K.; Oldman, C.; Barclay, S. End-of-Life Care during Covid-19: Opportunities and Challenges for Community Nursing. Br. J. Community Nurs. 2021, 26, 44–46. [Google Scholar] [CrossRef]
- Wolf, L.A.; Perhats, C.; Delao, A.M.; Moon, M.D.; Clark, P.R.; Zavotsky, K.E. “It’s a Burden You Carry”: Describing Moral Distress in Emergency Nursing. J. Emerg. Nurs. 2016, 42, 37–46. [Google Scholar] [CrossRef]
- Boulton, A.J.; Jordan, H.; Adams, C.E.; Polgarova, P.; Morris, A.C.; Arora, N. Intensive Care Unit Visiting and Family Communication during the COVID-19 Pandemic: A UK Survey. J. Intensive Care Soc. 2021, 1–4. [Google Scholar] [CrossRef]
- Sonis, J.D.; Kennedy, M.; Aaronson, E.L.; Baugh, J.J.; Raja, A.S.; Yun, B.J.; White, B.A. Humanism in the Age of Covid-19: Renewing Focus on Communication and Compassion. West. J. Emerg. Med. 2020, 21, 499–502. [Google Scholar] [CrossRef]
- McCarthy, B.; O’Donovan, M.; Trace, A. A New Therapeutic Communication Model “TAGEET” to Help Nurses Engage Therapeutically with Patients Suspected of or Confirmed with COVID-19. J. Clin. Nurs. 2021, 30, 1184–1191. [Google Scholar] [CrossRef]
- Scott-Cawiezell, J.; Schenkman, M.; Moore, L.; Vojir, C.; Connolly, R.P.; Pratt, M.; Palmer, L. Exploring Nursing Home Staff’s Perceptions of Communication and Leadership to Facilitate Quality Improvement. J. Nurs. Care Qual. 2004, 19, 242–252. [Google Scholar] [CrossRef]
- Kovner, C.; Raveis, V.H.; Van Devanter, N.; Yu, G.; Glassman, K.; Ridge, L.J. The Psychosocial Impact on Frontline Nurses of Caring for Patients with COVID-19 during the First Wave of the Pandemic in New York City. Nurs. Outlook 2021, 69, 744–754. [Google Scholar] [CrossRef]
- Huynh, J.Y.; Winefield, A.H.; Xanthopoulou, D. Social Support Moderates the Impact of Demands on Burnout and Organizational Connectedness: A Two-Wave Study of Volunteer Firefighters. J. Occup. Health Psychol. 2013, 18, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Apker, J.; Ray, E.B. Stress and Social Support in Health Care Organizations. In Handbook of Health Communication; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2013. [Google Scholar]
- Askari, R.; Rafiei, S.; Akbari, R.; Ebrahimi, E.H.; Dehghani, A.; Shafii, M. The Relationship between Work-Life Balance and Quality of Life among Hospital Employees. Int. J. Healthc. Manag. 2021, 14, 436–440. [Google Scholar] [CrossRef]
- Creese, J.; Byrne, J.P.; Conway, E.; Barrett, E.; Prihodova, L.; Humphries, N. “We All Really Need to Just Take a Breath”: Composite Narratives of Hospital Doctors’ Well-Being during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2051. [Google Scholar] [CrossRef] [PubMed]
| Variables | N = 22 | ||
|---|---|---|---|
| Frequencies | Percentages | ||
| Gender | Male | 5 | 27 |
| Female | 17 | 73 | |
| Marital Status | Single | 3 | 13 |
| Married | 17 | 78 | |
| Divorced | 2 | 9 | |
| Education | B.A. | 11 | 50 |
| M.A. | 11 | 50 | |
| Role in the ICCU | Regular Nurse | 20 | 91 |
| Clinical Instructor | 1 | 4.5 | |
| Nurse in Charge | 1 | 4.5 | |
| 1. | What is the communication experience of ICCU nurses in the COVID-19 battle? |
| 2. | Describe the communication process during your shift in the ward when working with a COVID-19 patient? |
| 3. | What are the main challenges or strengths you have experienced while working with a COVID-19 patient? |
| 4. | What are your feelings regarding patient-caregiver communication when working with COVID-19 patients? |
| 5. | Describe one case in which you had negative feelings and one case in which you had positive feelings regarding this communication process. |
| 6. | Do communication thoughts (good or bad) related to your patients and their families follow you after the end of a shift? |
| 7. | How does your environment react and communicate with you when they know that you work with COVID-19 patients? |
| 8. | Were there any complex communication situations you required to manage throughout the pandemic? |
| 9. | Did the pandemic create changes in your life? If so, how did you deal with them? |
| 10. | Do you share the feelings you experienced as ICCU nurses in the COVID-19 ward? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Green, G.; Sharon, C.; Gendler, Y. The Communication Challenges and Strength of Nurses’ Intensive Corona Care during the Two First Pandemic Waves: A Qualitative Descriptive Phenomenology Study. Healthcare 2022, 10, 837. https://doi.org/10.3390/healthcare10050837
Green G, Sharon C, Gendler Y. The Communication Challenges and Strength of Nurses’ Intensive Corona Care during the Two First Pandemic Waves: A Qualitative Descriptive Phenomenology Study. Healthcare. 2022; 10(5):837. https://doi.org/10.3390/healthcare10050837
Chicago/Turabian StyleGreen, Gizell, Cochava Sharon, and Yulia Gendler. 2022. "The Communication Challenges and Strength of Nurses’ Intensive Corona Care during the Two First Pandemic Waves: A Qualitative Descriptive Phenomenology Study" Healthcare 10, no. 5: 837. https://doi.org/10.3390/healthcare10050837
APA StyleGreen, G., Sharon, C., & Gendler, Y. (2022). The Communication Challenges and Strength of Nurses’ Intensive Corona Care during the Two First Pandemic Waves: A Qualitative Descriptive Phenomenology Study. Healthcare, 10(5), 837. https://doi.org/10.3390/healthcare10050837






