Analysis of the Psychosocial Impact of the COVID-19 Pandemic on the Nursing Staff of the Intensive Care Units (ICU) in Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Aims and Study Design
2.2. Population and Scope of the Study
2.3. Instrument, Data Collection, and Procedure
- Perception of working conditions during the pandemic: five questions (four yes/no questions and one with five options) aimed to determine the nurses’ opinions regarding the management of the pandemic in their unit, in terms of material and personnel support.
- Work relationships: three questions (two yes/no and one with different answer options) about the impact on the relationship between co-workers, difficulty in concentrating, and impact on work performance and, therefore, the health care provided.
- Perception of the state of mental health: we inquired regarding the feelings and mental states experienced by the health workers, such as worry, mental fatigue, sleep problems, fear, anxiety, psychological stress, and depression. In addition, nurses were also asked about psychological or psychiatric help (if they had to seek it, as well as if they were aware of the free services offered by the hospital) and the use of psychotropic medication. This section consisted of 11 questions, of which, eight had different options, and three were yes/no questions.
- Life events: whether they have suffered any traumatic event related to the pandemic, such as personal or family infection, admission, or death, due to COVID-19. It consisted of two yes/no response items.
- Social relations: focused on determining the social impact that the situation has had on professionals and their immediate environment. It was about the fear of infecting someone close to them, as well as whether drastic measures have been used to avoid it, they had people in their environment who were at risk of the disease, they were at risk, or they felt their relationships have been affected. This section consists of five yes/no response items.
2.4. Study Variables
2.5. Statistical Procedures
2.6. Ethical Considerations
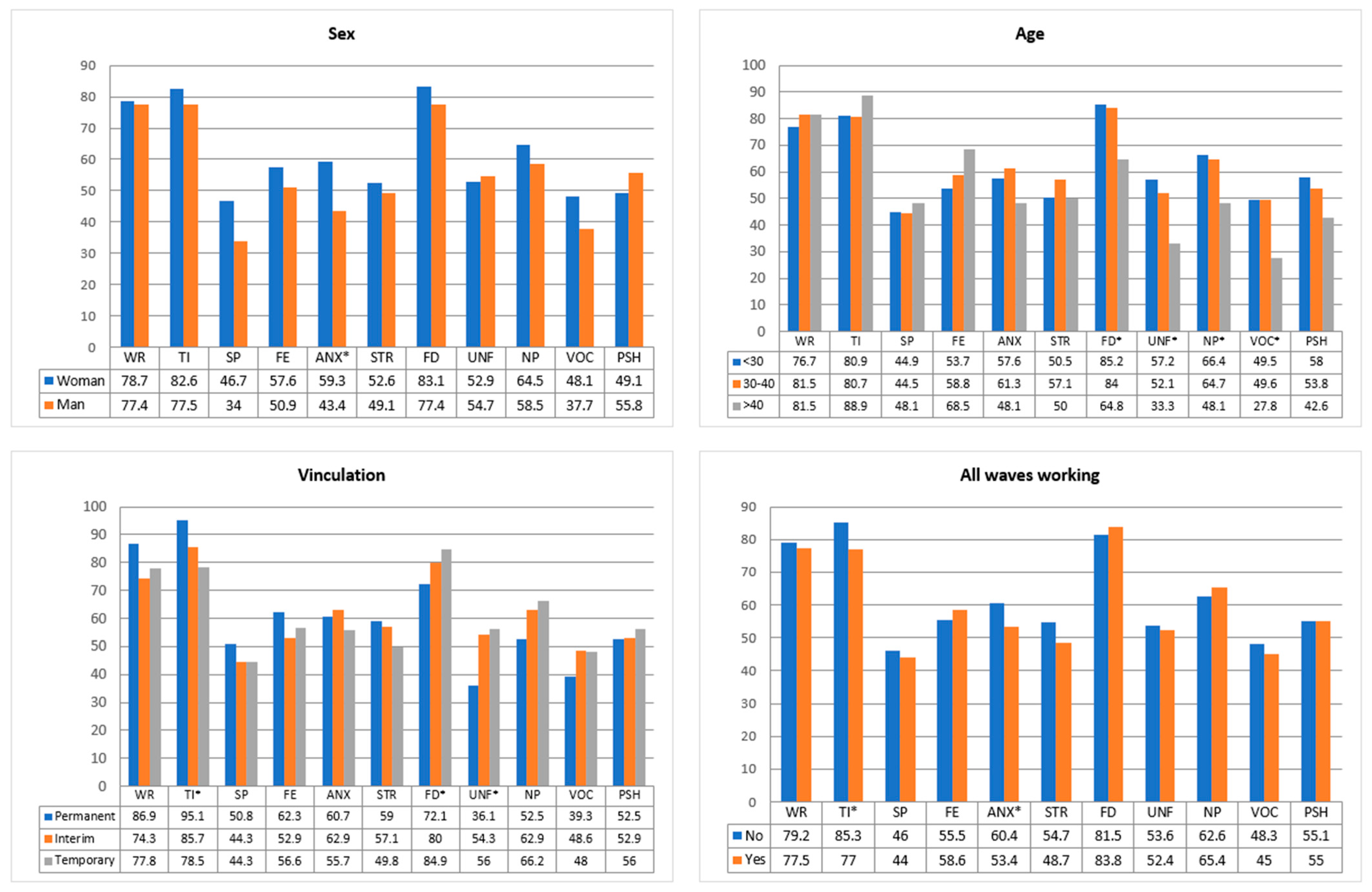
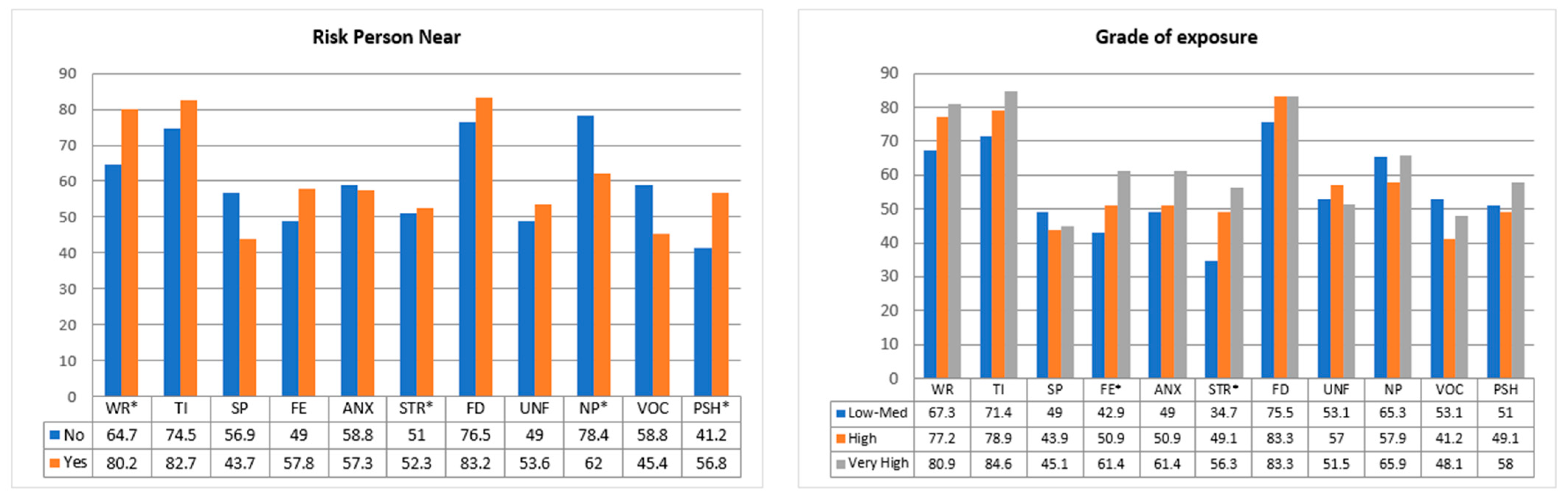
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- España. Ministerio de la Presidencia. Real Decreto 463/2020. Boletín Of. Estado. 2020, 67, 25390–25400. [Google Scholar]
- ISCIII. RENAVE. Situación de COVID-19 en España. Casos diagnosticados a partir 10 de mayo. Red Nac. Vigil. Epidemiol. 2021, 72, 17. [Google Scholar]
- ISCIII. RENAVE. Análisis de los casos de COVID-19 notificados a la RENAVE Informe COVID-19 no 33. 29 de mayo de 2020. Red Nac. Vigil. Epidemiol. 2020, 11, 2–4. [Google Scholar]
- Peña-Ramos, J.A.; Recuero-López, F.; Sánchez-Bayón, A.; Sastre, F.J. Evaluation of Spanish Health System during the COVID-19 Pandemic: Accountability and Wellbeing Results. Int. J. Environ. Res. Public Health 2021, 18, 12907. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Díaz, V. Estigmatización y nuevas formas de agresión a personal sanitario y celadores en tiempos del COVID-19. Rev. Médica 2020, 6, 33. [Google Scholar]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Lázaro-Pérez, C.; Martínez-López, J.Á.; Gómez-Galán, J.; López-Meneses, E. Anxiety about the risk of death of their patients in health professionals in spain: Analysis at the peak of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5938. [Google Scholar]
- Luceño-Moreno, L.; Talavera-Velasco, B.; García-Albuerne, Y.; Martín-García, J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5514. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Vilagut, G.; Mortier, P.; Ferrer, M.; Alayo, I.; Aragón-Peña, A.; Aragonés, E.; Campos, M.; Cura-González, I.D.; Emparanza, J.I.; et al. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Rev. Psiquiatr. Y Salud Ment. 2021, 14, 90–105. [Google Scholar] [CrossRef]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef] [PubMed]
- Villca Villegas, J.L.; Moreno Choque, R.A.; Gomez Verduguez, C.A.; Vargas Aguilar, A.A. Influencia de la pandemia del COVID-19 en la Salud Mental de los Trabajadores en salud: Pandemia de COVID-19 y Salud Mental en trabajadores en salud. Gac. Med. Bol. 2021, 44, 75–80. [Google Scholar] [CrossRef]
- Shacham, M.; Hamama-Raz, Y.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; Mijiritsky, E. COVID-19 Factors and Psychological Factors Associated with Elevated Psychological Distress among Dentists and Dental Hygienists in Israel. Int. J. Environ. Res. Public Health 2020, 17, 2900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo-Campos, R.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- Del Pozo-Herce, P.; Garrido-García, R.; Santolalla-Arnedo, I.; Gea-Caballero, V.; García-Molina, P.; Ruiz de Viñas, P.; Hernández, R.; Rodríguez-Velasco, F.J.; Juárez-Vela, R. Psychological Impact on the Nursing Professionals of the Rioja Health Service (Spain) Due to the SARS-CoV-2 Virus. Int. J. Environ. Res. Public Health 2021, 18, 580. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Falcó-Pegueroles, A.; Rosa, D.; Tolotti, A.; Graffigna, G.; Bonetti, L. The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID-19 emergency: A rapid review. Int. J. Public Health 2020, 65, 1205–1216. [Google Scholar] [CrossRef] [PubMed]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef] [PubMed]
- Albott, C.S.; Wozniak, J.R.; McGlinch, B.P.; Wall, M.H.; Gold, B.S.; Vinogradov, S. Battle Buddies: Rapid Deployment of a Psychological Resilience Intervention for Health Care Workers during the COVID-19 Pandemic. Anesth. Analg. 2020, 131, 43–54. [Google Scholar] [CrossRef]
- Azoulay, E.; Cariou, A.; Bruneel, F.; Demoule, A.; Kouatchet, A.; Reuter, D.; Souppart, V.; Combes, A.; Klouche, K.; Argaud, L.; et al. Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study. Am. J. Respir. Crit. Care Med. 2020, 202, 1388–1398. [Google Scholar] [CrossRef] [PubMed]
- García-Iglesias, J.J.; Gómez-Salgado, J.; Martín-Pereira, J.; Fagundo-Rivera, J.; Ayuso-Murillo, D.; Martínez-Riera, J.R.; Ruiz Frutos, C. Impacto del SARS-CoV-2 (COVID-19) en la salud mental de los profesionales sanitarios: Una revisión sistemática. Rev. Española Salud Publica 2020, 94, 1–20. [Google Scholar]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ Clin. Res. 2020, 369, m1642. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Tavakol, M.; Reg, D. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Khaledi-Paveh, B.; Kazeminia, M.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Eskandari, S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Hum. Resour. Health 2020, 18, 100. [Google Scholar] [CrossRef] [PubMed]
- Sanghera, J.; Pattani, N.; Hashmi, Y.; Varley, K.F.; Cheruvu, M.S.; Bradley, A.; Burke, J.R. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—A Systematic Review. J. Occup. Health 2020, 62, 12175. [Google Scholar] [CrossRef] [PubMed]
- Spoorthy, M.S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatry 2020, 51, 2018–2021. [Google Scholar] [CrossRef]
- Hammond, N.E.; Crowe, L.; Abbenbroek, B.; Elliott, R.; Tian, D.H.; Donaldson, L.H.; Fitzgerald, E.; Flower, O.; Grattan, S.; Harris, R.; et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers’ depression, anxiety, and stress levels. Aust. Crit. Care 2021, 34, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Shin, J.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Carmassi, C.; Foghi, C.; Dell’Oste, V.; Cordone, A.; Bertelloni, C.A.; Bui, E.; Dell’Osso, L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res. 2020, 292, 113312. [Google Scholar] [CrossRef] [PubMed]
- Vizheh, M.; Qorbani, M.; Arzaghi, S.M.; Muhidin, S.; Javanmard, Z.; Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020, 26, 1–12. [Google Scholar] [CrossRef]
- Raudenská, J.; Steinerová, V.; Javůrková, A.; Urits, I.; Kaye, A.D.; Viswanath, O.; Varrassi, G. Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pract. Res. Clin. Anaesthesiol. 2020, 34, 553–560. [Google Scholar] [CrossRef] [PubMed]
- da Silva, F.C.T.; Neto, M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110057. [Google Scholar] [CrossRef] [PubMed]
- Santolalla-Arnedo, I.; Del Pozo-Herce, P.; De Viñaspre-Hernandez, R.R.; Gea-Caballero, V.; Juarez-Vela, R.; Gil-Fernandez, G.; Rodriguez-Velasco, F.J. Psychological impact on care professionals due to the SARS-Cov-2 virus in Spain. Int. Nurs. Rev. 2022, 1, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Neitzke, A.B. An illness of power: Gender and the social causes of depression. Cult. Med. Psychiatry 2016, 40, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Almaguer, A.C.; Alvarez, A.K.G.; Santos, E.Z. Management of health personnel’ psychological safety, in emergency situations by COVID-19 in the hospitable or isolation context. Rev. Cuba. Enf. 2020, 36, 2. [Google Scholar]
- Sampaio, F.; Sequeira, C.; Teixeira, L. Impact of COVID-19 outbreak on nurses’ mental health: A prospective cohort study. Environ. Res. 2021, 194, 110620. [Google Scholar] [CrossRef] [PubMed]
- Crowe, S.; Howard, A.F.; Vanderspank-Wright, B.; Gillis, P.; McLeod, F.; Penner, C.; Haljan, G. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: A mixed method study. Intensive Crit. Care Nurs. 2021, 63, 102999. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. J. Psychiatr. Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Y.; Yang, Y.Z.; Zhang, X.M.; Xu, X.; Dou, Q.L.; Zhang, W.W.; Cheng, A.S. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%) |
|---|---|
| Sex | |
| Woman | 403 (88.4) |
| Man | 53 (11.6) |
| Age | |
| <30 years | 283 (62.1) |
| 30–40 years | 119 (26.1) |
| >40 years | 54 (11.8) |
| Employment relationship | |
| Temporary | 325 (71.3) |
| Interim | 70 (15.4) |
| Fixed | 61 (13.4) |
| Indicate in which wave of the pandemic you have worked in the Intensive Care Unit | |
| In all waves | 191 (41.9) |
| Only in some | 265 (58.1) |
| COVID-19 infection | |
| Yes | 101 (22.1) |
| No | 355 (77.9) |
| Person at risk in close proximity | |
| Yes | 405 (88.8) |
| No | 51 (11.2) |
| What do you consider your level of exposure has been within the unit? | |
| Very high | 290 (63.6) |
| High | 114 (25) |
| Medium | 38 (8.3) |
| Low | 11 (2.4) |
| Very Low | 3 (0.7) |
| How has the relationship with your colleagues been? | |
| Better | 352 (77.2) |
| The same as always | 62 (13.6) |
| Worst | 42 (9.2) |
| Do you think you have been provided with adequate working conditions to cope with the situation since the beginning of the pandemic? | |
| Yes | 97 (21.3) |
| No | 359 (78.7) |
| Have you been provided with all the assistance you have needed, both material and personnel? | |
| Yes | 147 (32.2) |
| No | 309 (67.8) |
| Do you think our healthcare system was prepared for this situation? | |
| Yes | 7 (1.5) |
| No | 449 (98.5) |
| Have you experienced any traumatic events related to the pandemic? | |
| Yes | 169 (37.1) |
| No | 287 (62.9) |
| Variable | n (%) |
|---|---|
| Have you felt more worried (either about your health or your family’s health, work or anything related to the pandemic)? | |
| Much more | 358 (78.5) |
| More | 89 (19.5) |
| Equal | 8 (1.8) |
| No | 1 (0.2) |
| Have you experienced difficulties in focusing on your work? | |
| Yes | 242 (53.1) |
| No | 214 (46.9) |
| Have you felt more tired? | |
| Much more | 373 (81.8) |
| More | 80 (17.5) |
| Equal | 2 (0.4) |
| No | 1 (0.2) |
| Have you had sleep problems? | |
| Much more | 206 (45.2) |
| More | 184 (40.4) |
| Equal | 20 (4.4) |
| No | 46 (10.1) |
| Have you ever felt fear? To what degree? | |
| Much more | 259 (56.8) |
| More | 178 (39) |
| Equal | 12 (2.6) |
| No | 7 (1.5) |
| Have you experienced fear of infecting your close family/social environment? | |
| Yes | 445 (97.6) |
| No | 11 (2.4) |
| Do you feel that your relationships have been affected to some extent by the situation you have faced? | |
| Yes | 423 (92.8) |
| No | 33 (7.2) |
| Have you changed your behaviour towards those close to you, or even felt compelled to take isolation measures by them? | |
| Yes | 429 (94.1) |
| No | 27 (5.9) |
| Indicate the degree to which you have felt anxiety. | |
| Much more | 262 (57.5) |
| More | 156 (34.2) |
| Equal | 17 (3.7) |
| No | 21 (4.6) |
| Do you consider that you have suffered psychological stress and to what degree? | |
| Much more | 238 (52.2) |
| More | 186 (40.8) |
| Equal | 11 (4.6) |
| No | 21 (2.4) |
| Have you ever felt down, depressed or hopeless? | |
| Yes | 376 (82.5) |
| No | 80 (17.5) |
| Have you had times when you felt you had lost your vocation or even considered giving up your job? | |
| Yes | 214 (46.9) |
| No | 242 (53.1) |
| Do you think this has had a negative impact on your job performance, and therefore on the quality of patient care? | |
| Yes | 291 (63.8) |
| No | 165 (36.2) |
| Are you aware of the counselling services offered in your hospital to professionals? | |
| Yes | 239 (52.4) |
| No | 217 (47.6) |
| Have you had to seek psychological or psychiatric help? | |
| Yes | 82 (18) |
| No | 205 (45) |
| No, but I think I need it | 169 (37) |
| Has the use of psychotropic medicines increased? | |
| Yes | 83 (18.2) |
| I consume the same | 33 (7.2) |
| Non-consumption | 340 (4.6) |
| Question | D1 | D2 | D3 |
|---|---|---|---|
| Have you felt more worried (either about your health or your family’s health, work or anything related to the pandemic)? | 0.808 | ||
| Have you felt more fear? | 0.805 | ||
| Have you felt more tired or exhausted? | 0.507 | ||
| Have you had sleep problems? | 0.636 | ||
| Indicate the degree to which you have felt anxiety. | 0.727 | ||
| Do you consider that you have suffered psychological stress, and to what degree? | 0.783 | ||
| Have you ever felt down, depressed, or hopeless? | 0.495 | ||
| Have you had to seek psychological or psychiatric help? | 0.685 | ||
| Have you experienced difficulties in focusing on your work? | 0.696 | ||
| Do you think this has had a negative impact on your job performance, and therefore on the quality of patient care? | 0.817 | ||
| Have you had times when you felt you had lost your vocation or even considered giving up your job? | 0.507 |
| Sex | Age | Employment Relationship | All Waves Working | Risk Person Near | Degree of Exposure | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Question | Chi2 | p-Value | Chi2 | p-Value | Chi2 | p-Value | Chi2 | p-Value | Chi2 | p-Value | Chi2 | p-Value |
| Worried | 0.047 | 0.828 | 1.481 | 0.477 | 3.361 | 0.186 | 0.203 | 0.652 | 6.484 | 0.011 * | 4.718 | 0.095 |
| Tired | 1.612 | 0.204 | 2.072 | 0.355 | 10.381 | 0.006 * | 5.160 | 0.023 * | 2.049 | 0.152 | 5.752 | 0.056 |
| Sleep problems | 3.044 | 0.081 | 0.222 | 0.895 | 0.906 | 0.636 | 0.190 | 0.663 | 3.167 | 0.075 | 0.368 | 0.832 |
| Fear | 0.838 | 0.360 | 4.322 | 0.115 | 1.199 | 0.549 | 0.454 | 0.501 | 1.416 | 0.234 | 8.075 | 0.018 * |
| Anxiety | 4.850 | 0.028 * | 2.652 | 0.265 | 1.504 | 0.471 | 2.209 | 0.137 | 0.044 | 0.834 | 5.355 | 0.069 |
| Stress | 0.236 | 0.627 | 1.586 | 0.452 | 2.543 | 0.280 | 1.615 | 0.204 | 0.034 | 0.854 | 8.438 | 0.015 * |
| Felt down | 1.077 | 0.299 | 13.251 | 0.001 * | 6.155 | 0.046 * | 0.392 | 0.531 | 1.422 | 0.233 | 1.831 | 0.400 |
| Unfocused | 0.065 | 0.798 | 10.470 | 0.005 * | 8.244 | 0.016 * | 0.067 | 0.795 | 0.378 | 0.539 | 0.990 | 0.610 |
| Negative performance | 0.736 | 0.391 | 6.620 | 0.037 * | 4.204 | 0.122 | 0.378 | 0.539 | 5.312 | 0.021 * | 2.314 | 0.314 |
| Vocation | 2.035 | 0.154 | 9.022 | 0.011 * | 1.634 | 0.442 | 0.478 | 0.489 | 3.261 | 0.071 | 2.395 | 0.302 |
| Psychological help | 0.869 | 0.351 | 4.426 | 0.109 | 0.420 | 0.811 | 0.001 | 0.989 | 4.462 | 0.035 * | 2.985 | 0.225 |
| Sex | Age | Employment Relationship | All Waves Working | Risk Person Near | Degree of Exposure | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dimension | t | p-Value | F | p-Value | F | p-Value | t | p-Value | t | p-Value | F | p-Value |
| D1 | 0.448 | 0.654 | 2.715 | 0.067 | 1.679 | 0.188 | 0.306 | 0.759 | 1.867 | 0.062 | 2.582 | 0.077 |
| D2 | 1.821 | 0.069 | 0.868 | 0.420 | 0.694 | 0.500 | −1.450 | 0.148 | 0.568 | 0.570 | 2.396 | 0.092 |
| D3 | 0.244 | 0.808 | 8.926 | 0.000 * | 6.813 | 0.001 * | 0.641 | 0.522 | −1.116 | 0.265 | 0.285 | 0.752 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muñoz-Muñoz, M.; Carretero-Bravo, J.; Pérez-Muñoz, C.; Díaz-Rodríguez, M. Analysis of the Psychosocial Impact of the COVID-19 Pandemic on the Nursing Staff of the Intensive Care Units (ICU) in Spain. Healthcare 2022, 10, 796. https://doi.org/10.3390/healthcare10050796
Muñoz-Muñoz M, Carretero-Bravo J, Pérez-Muñoz C, Díaz-Rodríguez M. Analysis of the Psychosocial Impact of the COVID-19 Pandemic on the Nursing Staff of the Intensive Care Units (ICU) in Spain. Healthcare. 2022; 10(5):796. https://doi.org/10.3390/healthcare10050796
Chicago/Turabian StyleMuñoz-Muñoz, María, Jesús Carretero-Bravo, Celia Pérez-Muñoz, and Mercedes Díaz-Rodríguez. 2022. "Analysis of the Psychosocial Impact of the COVID-19 Pandemic on the Nursing Staff of the Intensive Care Units (ICU) in Spain" Healthcare 10, no. 5: 796. https://doi.org/10.3390/healthcare10050796
APA StyleMuñoz-Muñoz, M., Carretero-Bravo, J., Pérez-Muñoz, C., & Díaz-Rodríguez, M. (2022). Analysis of the Psychosocial Impact of the COVID-19 Pandemic on the Nursing Staff of the Intensive Care Units (ICU) in Spain. Healthcare, 10(5), 796. https://doi.org/10.3390/healthcare10050796







