Development of the Japanese Version of the Infertility Stigma Scale: Examination of Its Reliability and Validity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Scale Development
2.1.1. The Infertility Stigma Scale
2.1.2. Translation Process
2.1.3. Content Validity through Expert Panel
2.1.4. Content Validity through Cognitive Interviews
2.2. Scale Validation
2.2.1. Participants and Recruitment Procedure
2.2.2. Data Collection
2.2.3. Data Analysis
Item Exclusion Criteria
Examination of the Structural Validity
Examination of Reliability
Examination of the Known-Groups, Convergent, and Discriminant Validity
2.2.4. Ethical Considerations
3. Results
3.1. Item Score Distribution
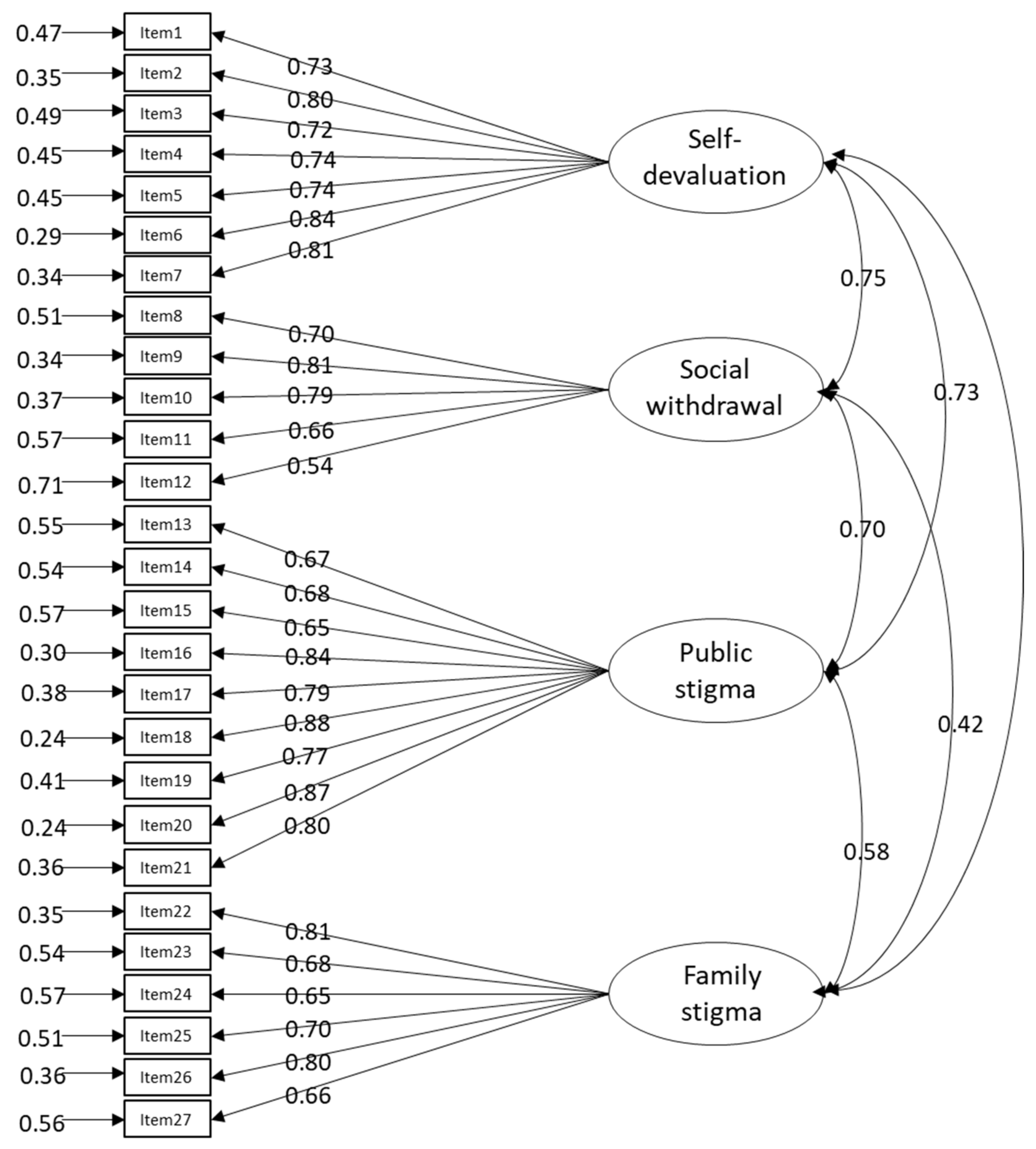
3.2. Structural Validity: Exploratory Factor Analysis and Confirmatory Factor Analysis
3.3. Internal Consistency and Intra-Rater Reliability
3.4. Known-Groups Validity
3.5. Convergent Validity
3.6. Convergent and Discriminant Validity: Multitrait Scaling Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Item | Ne a | CVR b | Interpretation c |
|---|---|---|---|
| Item 1 | 8 | 1.00 | Remained |
| Item 2 | 8 | 1.00 | Remained |
| Item 3 | 8 | 1.00 | Remained |
| Item 4 | 8 | 1.00 | Remained |
| Item 5 | 8 | 1.00 | Remained |
| Item 6 | 8 | 1.00 | Remained |
| Item 7 | 8 | 1.00 | Remained |
| Item 8 | 8 | 1.00 | Remained |
| Item 9 | 8 | 1.00 | Remained |
| Item 10 | 7 | 0.75 | Remained |
| Item 11 | 8 | 1.00 | Remained |
| Item 12 | 8 | 1.00 | Remained |
| Item 13 | 7 | 0.75 | Remained |
| Item 14 | 8 | 1.00 | Remained |
| Item 15 | 8 | 1.00 | Remained |
| Item 16 | 8 | 1.00 | Remained |
| Item 17 | 8 | 1.00 | Remained |
| Item 18 | 7 | 0.75 | Remained |
| Item 19 | 8 | 1.00 | Remained |
| Item 20 | 8 | 1.00 | Remained |
| Item 21 | 8 | 1.00 | Remained |
| Item 22 | 7 | 0.75 | Remained |
| Item 23 | 8 | 1.00 | Remained |
| Item 24 | 8 | 1.00 | Remained |
| Item 25 | 8 | 1.00 | Remained |
| Item 26 | 7 | 0.75 | Remained |
| Item 27 | 7 | 0.75 | Remained |
Appendix B
| Item | Relevance | Clarity | Interpretation d | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Agreement | I-CVI a | Pc b | K c | Agreement | I-CVI a | Pc b | K c | ||
| Item 1 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 2 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 3 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 4 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 5 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 6 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 7 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 8 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 9 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 10 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 11 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 12 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 13 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 14 | 7/8 | 0.88 | 0.03 | 0.87 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 15 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 16 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 17 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 18 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 19 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 20 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 21 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 22 | 7/8 | 0.88 | 0.03 | 0.87 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 23 | 8/8 | 1.00 | <0.01 | 1.00 | 7/8 | 0.88 | 0.03 | 0.87 | Excellent |
| Item 24 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 25 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 26 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| Item 27 | 8/8 | 1.00 | <0.01 | 1.00 | 8/8 | 1.00 | <0.01 | 1.00 | Excellent |
| S-CVI/Ave e | 0.99 | 1.00 | |||||||
| S-CVI/UA f | 0.93 | 0.96 | |||||||
Appendix C
| Topics | Probing Question |
|---|---|
| General impression of the scale | What were your feelings when you were answering the questionnaire? Did you experience any psychological distress while completing the questionnaire? |
| Comprehensibility | How comprehensible was the instructional text to you? How comprehensible was item X to you? How comprehensible were the response options to you? Are there any questions that would be better phrased in a more specific way? |
| Relevance | Does item X relate to the situation of infertile women? Are there any questions that are duplicated, repeated, or very similar? |
| Comprehensiveness | Is there anything missing from this questionnaire regarding the feeling that infertile women are socially different compared with others? To what extent did you feel that the content of this questionnaire covered the sense of infertile women that you just described? Is the grouping of questions appropriate? |
| Response options | Are the response options appropriate? |
| Suggestions for improvement | Do you have any suggestions on how to improve the questionnaire? |
Appendix D
| Item | Comprehensibility | Relevance |
|---|---|---|
| Instruction | 87.5 | |
| Item 1 | 100.0 | 100.0 |
| Item 2 | 100.0 | 100.0 |
| Item 3 | 87.5 | 87.5 |
| Item 4 | 100.0 | 100.0 |
| Item 5 | 87.5 | 100.0 |
| Item 6 | 100.0 | 100.0 |
| Item 7 | 75.0 | 100.0 |
| Item 8 | 100.0 | 100.0 |
| Item 9 | 87.5 | 100.0 |
| Item 10 | 100.0 | 100.0 |
| Item 11 | 100.0 | 100.0 |
| Item 12 | 100.0 | 100.0 |
| Item 13 | 100.0 | 100.0 |
| Item 14 | 87.5 | 100.0 |
| Item 15 | 100.0 | 100.0 |
| Item 16 | 100.0 | 100.0 |
| Item 17 | 100.0 | 100.0 |
| Item 18 | 87.5 | 100.0 |
| Item 19 | 87.5 | 100.0 |
| Item 20 | 100.0 | 100.0 |
| Item 21 | 100.0 | 100.0 |
| Item 22 | 75.0 | 100.0 |
| Item 23 | 100.0 | 100.0 |
| Item 24 | 100.0 | 100.0 |
| Item 25 | 100.0 | 75.0 |
| Item 26 | 100.0 | 100.0 |
| Item 27 | 62.5 | 100.0 |
| Response options | 87.5 |
References
- Anderson, K.; Norman, R.J.; Middleton, P. Preconception lifestyle advice for people with subfertility. Cochrane Database Syst. Rev. 2010, 4, Cd008189. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population and Social Security Research. Basic Survey on Social Security and Population Problems 2015 Marriage and Childbirth in Japan Today: The Fifteenth Japanese National Fertility Survey, 2015 (Results of Singles and Married Couples Survey). 2017. Available online: http://www.ipss.go.jp/ps-doukou/j/doukou15/NFS15_reportALL.pdf (accessed on 7 December 2021).
- Ishihara, O.; Jwa, S.C.; Kuwahara, A.; Katagiri, Y.; Kuwabara, Y.; Hamatani, T.; Harada, M.; Ichikawa, T. Assisted reproductive technology in Japan: A summary report for 2017 by the Ethics Committee of the Japan Society of Obstetrics and Gynecology. Reprod. Med. Biol. 2020, 19, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health Labour and Welfare. Summary of Demographic Statistics for 2017. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei17/dl/03_h1.pdf (accessed on 7 December 2021).
- Kato, T.; Sampei, M.; Saito, K.; Morisaki, N.; Urayama, K.Y. Depressive symptoms, anxiety, and quality of life of Japanese women at initiation of ART treatment. Sci. Rep. 2021, 11, 7538. [Google Scholar] [CrossRef]
- Donkor, E.S.; Sandall, J. The impact of perceived stigma and mediating social factors on infertility-related stress among women seeking infertility treatment in Southern Ghana. Soc. Sci. Med. 2007, 65, 1683–1694. [Google Scholar] [CrossRef]
- Fang, M.; Li, G.; Kang, X.; Hou, F.; Lv, G.; Xu, X.; Kong, L.; Li, P. The role of gender and self-esteem as moderators of the relationship between stigma and psychological distress among infertile couples. Psychol. Health Med. 2021, 26, 1181–1194. [Google Scholar] [CrossRef]
- Jing, X.; Gu, W.; Xu, X.; Yan, C.; Jiao, P.; Zhang, L.; Li, X.; Wang, X.; Wang, W. Stigma predicting fertility quality of life among Chinese infertile women undergoing in vitro fertilization-embryo transfer. J. Psychosom. Obs. Gynaecol. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.M.; Keitel, M.; Jackson, M.; Harris, A.; Licciardi, F. Predictors of distress in women being treated for infertility. J. Reprod. Infant. Psychol. 2009, 27, 238–257. [Google Scholar] [CrossRef]
- Slade, P.; O’Neill, C.; Simpson, A.J.; Lashen, H. The relationship between perceived stigma, disclosure patterns, support and distress in new attendees at an infertility clinic. Hum. Reprod. 2007, 22, 2309–2317. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, E.; Kavak, F. The effect of stigma on depression levels of Turkish women with infertility. Perspect. Psychiatr. Care 2019, 55, 378–382. [Google Scholar] [CrossRef]
- Öztürk, R.; Bloom, T.L.; Li, Y.; Bullock, L.F.C. Stress, stigma, violence experiences and social support of US infertile women. J. Reprod. Infant Psychol. 2021, 39, 205–217. [Google Scholar] [CrossRef]
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; Prentice Hall: Englewood Criffs, NJ, USA, 1963. [Google Scholar]
- Ainlay, S.C.; Becker, G.; Coleman, L.M. The Dilemma of Difference; Plenum: New York, NY, USA, 1986. [Google Scholar]
- Araki, A. The problem of the reproductive medicine due to infertility psychology–A problem to hide behind in the relationship do not treat by medical care that interface submits. Ritsumeikan J. Hum. Sci. 2008, 16, 81–94. [Google Scholar]
- Takeya, K. Choice and loss in infertility experience: Reanalysis of a narrative text through dialogic reflexivity. Kyoto Univ. Res. Stud. Educ. 2009, 55, 351–363. [Google Scholar]
- Yasuda, Y. Life Choices of Infertility Patients: A Narrative Approach to Capturing Life Stories; Shinyosya: Tokyo, Japan, 2012. [Google Scholar]
- National Institute of Population and Social Security Research, Summary of the Results of the 6th National Survey on Household Trends. 2018. Available online: http://www.ipss.go.jp/ps-katei/j/NSFJ6/Kohyo/NSFJ6_gaiyo.pdf (accessed on 19 December 2021).
- Takeya, K. The narratives of women who received infertility treatment: The choice of a life as a woman without children. Qual. Res. Psychol. Jpn. J. Qual. Psychol. 2008, 7, 118–137. [Google Scholar]
- Justo, J.M.R.M.; Paris Vieira, C.F.S.; Veiga Costa, E. Stigma consciousness and self-efficacy in infertile couples; Correlation and gender differences. Int. J. Dev. Educ. Psychol. 2010, 2, 17–24. [Google Scholar]
- McCarthy, M.P.; Chiu, S.H. Differences in women’s psychological well-being based on infertility treatment choice and outcome. J. Midwifery Womens Health 2011, 56, 475–480. [Google Scholar] [CrossRef]
- Taebi, M.; Kariman, N.; Montazeri, A.; Majd, H.A. Development and psychometric evaluation of the female infertility stigma instrument (ISI-F): Protocol for a mixed method study. Reprod. Health 2020, 17, 70. [Google Scholar] [CrossRef]
- Fu, B.; Qin, N.; Cheng, L.; Tang, G.; Cao, Y.; Yan, C.; Huang, X.; Yan, P.; Zhu, S.; Lei, J. Development and validation of an Infertility Stigma Scale for Chinese women. J. Psychosom. Res. 2015, 79, 69–75. [Google Scholar] [CrossRef]
- Çapık, A.; Aksoy, M.; Yılmaz, E.; Yılmaz, F. Infertility stigma scale: A psychometric study in a Turkish sample. Perspect. Psychiatr. Care 2019, 55, 328–335. [Google Scholar] [CrossRef]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [Green Version]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. Principles of good practice for the translation and cultural adaptation process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [Green Version]
- Jowell, R.; Roberts, C.; Fitzgerald, R.; Eva, G. Measuring Attitudes Cross-Nationally: Lesson from the European Social Survey; Sage: Los Angeles, CA, USA, 2007. [Google Scholar] [CrossRef]
- Behr, D. Assessing the use of back translation: The shortcomings of back translation as a quality testing method. Int. J. Soc. Res. Methodol. 2017, 20, 573–584. [Google Scholar] [CrossRef]
- Almanasreh, E.; Moles, R.; Chen, T.F. Evaluation of methods used for estimating content validity. Res. Soc. Adm. Pharm. 2019, 15, 214–221. [Google Scholar] [CrossRef]
- Caruso, R.; Arrigoni, C.; Groppelli, K.; Magon, A.; Dellafiore, F.; Pittella, F.; Grugnetti, A.M.; Chessa, M.; Yorke, J. Italian version of Dyspnoea-12: Cultural-linguistic validation, quantitative and qualitative content validity study. Acta Biomed. 2018, 88, 426–434. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Prinsen, C.A.C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. COSMIN Study Design Checklist for Patient-Reported Outcome Measurement Instruments. 2019. Available online: https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf (accessed on 20 December 2021).
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, I.B.; Adachi, J.D.; Beattie, K.A.; MacDermid, J.C. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculoskelet. Disord. 2017, 18, 540. [Google Scholar] [CrossRef] [Green Version]
- Zamanzadeh, V.; Ghahramanian, A.; Rassouli, M.; Abbaszadeh, A.; Alavi-Majd, H.; Nikanfar, A.R. Design and implementation content validity study: Development of an instrument for measuring patient-centered communication. J. Caring Sci. 2015, 4, 165–178. [Google Scholar] [CrossRef]
- Lawshe, C.H. A quantitative approach to content validity. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- Schwarz, N.; Sudman, S. Answering Questions: Methodology for Determining Cognitive and Communicative Processes in Survey Research; Jossey-Bass Pub: San Francisco, CA, USA, 1996. [Google Scholar]
- Willis, G.B. Cognitive Interviewing: A Tool for Improving Questionnaire Design; Sage: Thousand Oaks, CA, USA, 2005. [Google Scholar]
- Apfelbacher, C.J.; Jones, C.J.; Frew, A.; Smith, H. Validity of three asthma-specific quality of life questionnaires: The patients’ perspective. BMJ Open 2016, 6, e011793. [Google Scholar] [CrossRef]
- Collins, D. Pretesting survey instruments: An overview of cognitive methods. Qual. Life Res. 2003, 12, 229–238. [Google Scholar] [CrossRef]
- Gabes, M.; Tischer, C.; Herrmann, A.; Howells, L.; Apfelbacher, C. The German RECAP questionnaire: Linguistic validation and cognitive debriefing in German adults with self-reported atopic eczema and parents of affected children. J. Patient-Rep. Outcomes 2021, 5, 13. [Google Scholar] [CrossRef]
- Irwin, D.E.; Varni, J.W.; Yeatts, K.; DeWalt, D.A. Cognitive interviewing methodology in the development of a pediatric item bank: A patient reported outcomes measurement information system (PROMIS) study. Health Qual. Life Outcomes 2009, 7, 3. [Google Scholar] [CrossRef] [Green Version]
- Tse, E.T.Y.; Lam, C.L.K.; Wong, C.K.H.; Chin, W.Y.; Etz, R.S.; Zyzanski, S.J.; Stange, K.C. Cultural adaptation and content validity of a Chinese translation of the Person-Centered Primary Care Measure: Findings from cognitive debriefing. Fam. Med. Commun. Health 2020, 8, e000621. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Frley, G.K. The multidimensional scale of perceived social support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef] [Green Version]
- Zimet, G.D.; Powell, S.S.; Farley, G.K.; Werkman, S.; Berkoff, K.A. Psychometric characteristics of the multidimensional scale of perceived social support. J. Personal. Assess. 1990, 55, 610–617. [Google Scholar] [CrossRef]
- Iwasa, H.; Gondo, Y.; Masui, Y.; Inagaki, H.; Kawai, C.; Ootsuka, R.; Ogawa, M.; Takayama, M.; Imuta, H.; Suzuki, T. Reliability and validity of the Japanese version of the Social Support Scale: A study of middle-aged and older adults. J. Health Welf. Stat. 2007, 54, 26–33. [Google Scholar]
- Rosenberg, M. Society and Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Mimura, C.; Griffiths, P. A Japanese version of the Rosenberg Self-Esteem Scale: Translation and equivalence assessment. J. Psychosom. Res. 2007, 62, 589–594. [Google Scholar] [CrossRef]
- Uchida, T.; Ueno, T. Reliability and validity of the Rosenberg Self Esteem Scale: Using the Japanese version of the RSES by Mimura & Griffiths (2007). Annu. Rep. Grad. Sch. Educ. Tohoku Univ. 2010, 58, 257–266. [Google Scholar]
- Smilkstein, G. The family APGAR: A proposal for a family function test and its use by physicians. J. Fam. Pract. 1978, 6, 1231–1239. [Google Scholar]
- Smilkstein, G.; Ashworth, C.; Montano, D. Validity and reliability of the family APGAR as a test of family function. J. Fam. Pract. 1982, 15, 303–311. [Google Scholar]
- Kokubu, M.; Kamibeppu, K. Development of a Family Functioning Scale: The Japanese Version of Family APGAR. Establishment of Family Nursing Skills and Liaison Systems between Hospitals and Other Social Resources to Realize Abuse Prevention from the Perinatal Period (Principal Researcher: Kamibeppu, K). Working Report of Grant-in-Aid for Scientific Research in 2009–2011. 2013. Available online: https://kaken.nii.ac.jp/file/KAKENHI-PROJECT-21390589/21390589seika.pdf (accessed on 7 December 2021).
- Toyoda, H. Covariance Structure Analysis—Structural Equation Modeling Using R; TokyoTosho Co., Ltd.: Tokyo, Japan, 2014. [Google Scholar]
- Toyoda, H. Covariance Structure Analysis [Q&A]—Structural Equation Modeling; Asakura Publishing Co., Ltd.: Tokyo, Japan, 2003. [Google Scholar]
- Kwon, M.Y.; Kim, N.Y. Validity and reliability of a Korean version of the ConCom Safety Management Scale. Int. J. Environ. Res. Public Health 2021, 18, 12514. [Google Scholar] [CrossRef] [PubMed]
- Asano, H.; Suzuki, T.; Kojima, T. Introduction to Covariance Structure Aanalysis in Practice; Kodansha Ltd.: Tokyo, Japan, 2005. [Google Scholar]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papreen, N.; Sharma, A.; Sabin, K.; Begum, L.; Ahsan, S.K.; Baqui, A.H. Living with infertility: Experiences among Urban slum populations in Bangladesh. Reprod. Health Matters 2000, 8, 33–44. [Google Scholar] [CrossRef] [Green Version]
- Remennick, L. Childless in the land of imperative motherhood: Stigma and coping among infertile Israeli women. Sex Roles 2000, 43, 821–841. [Google Scholar] [CrossRef]
- Araya, L.T.; Gebretekle, G.B.; Gebremariam, G.T.; Fenta, T.G. Reliability and validity of the Amharic version of European Organization for Research and Treatment of cervical Cancer module for the assessment of health related quality of life in women with cervical cancer in Addis Ababa, Ethiopia. Health Qual. Life Outcomes 2019, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Goo, A.J.; Shin, D.W.; Yang, H.K.; Park, J.H.; Kim, S.Y.; Shin, J.Y.; Kim, Y.A.; Kim, C.; Hong, N.S.; Min, Y.J.; et al. Cross-cultural application of the Korean version of the EORTC QLQ-ELD14 questionnaire for elderly patients with cancer. J. Geriatr. Oncol. 2017, 8, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Okui, T. Marriage and fertility rates of Japanese women according to employment status: An age-period-cohort analysis. Nihon Koshu Eisei Zasshi 2020, 67, 892–903. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population and Social Security Research. The 6th National Survey on Household Trends in Japan2018. Available online: https://www.ipss.go.jp/ps-katei/j/NSFJ6/Mhoukoku/Mhoukoku.pdf (accessed on 28 December 2021).
- Davidov, E.; Meuleman, B.; Cieciuch, J.; Schmidt, P.; Billiet, J. Measurement equivalence in cross-national research. Annu. Rev. Sociol. 2014, 40, 55–75. [Google Scholar] [CrossRef]
- Ministry of Health Labour and Welfare. Figure 1.1.7 Trends in the Number of Births and Total Fertility Rate. Available online: https://www.mhlw.go.jp/stf/wp/hakusyo/kousei/19/backdata/index.html (accessed on 28 December 2021).
- Tanabe, Y.; Hayashi, K.; Ideno, Y. The Internalized Stigma of Mental Illness (ISMI) scale: Validation of the Japanese version. BMC Psychiatry 2016, 16, 116. [Google Scholar] [CrossRef] [Green Version]
- Lv, Y.; Wolf, A.; Wang, X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen. Hosp. Psychiatry 2013, 35, 83–88. [Google Scholar] [CrossRef]
- Gender Equality Bureau Cabinet Office. World Economic Forum releases Gender Gap Index. 2021. Available online: https://www.gender.go.jp/public/kyodosankaku/2021/202105/202105_05.html (accessed on 28 December 2021).
- Link, B.G.; Phelan, J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Greil, A.L.; Slauson-Blevins, K.; McQuillan, J. The experience of infertility: A review of recent literature. Sociol. Health Illn. 2010, 32, 140–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Mean | SD a | |
|---|---|---|
| Age (years) | 35.93 | 5.55 |
| Duration of marriage (years) | 4.67 | 3.78 |
| Duration of infertility (years) | 3.32 | 2.88 |
| Duration of infertility treatment (years) | 2.27 | 2.44 |
| N | % | |
| Education | ||
| Less than high school | 1 | 0.4 |
| High school graduate | 43 | 16.9 |
| Vocational school graduate | 33 | 13.0 |
| Junior colleges or technical colleges | 44 | 17.3 |
| University graduate | 125 | 49.2 |
| Graduate school graduate | 8 | 3.1 |
| Annual household income | ||
| Less than JPY 2,000,000 | 12 | 4.7 |
| JPY 2,000,000 to JPY 4,000,000 | 38 | 15.0 |
| JPY 4,000,000 to JPY 6,000,000 | 72 | 28.3 |
| JPY 6,000,000 to JPY 8,000,000 | 59 | 23.2 |
| JPY 8,000,000 to JPY 10,000,000 | 33 | 13.0 |
| More than JPY 10,000,000 | 40 | 15.7 |
| Occupation | ||
| Office worker (regular employee) | 87 | 34.3 |
| Office worker (contract employee) | 11 | 4.3 |
| Public officer | 10 | 3.9 |
| Self-employed | 13 | 5.1 |
| Part-time worker | 53 | 20.9 |
| Housemaker | 79 | 31.1 |
| Unemployed | 1 | 0.4 |
| Living with parents | ||
| Yes | 15 | 5.9 |
| No | 239 | 94.1 |
| Causes of infertility | ||
| Male factor | 15 | 5.9 |
| Female factor | 84 | 33.1 |
| Both male and female factors | 38 | 15.0 |
| Unexplained factor | 117 | 46.1 |
| Treatment for infertility | ||
| Timing therapy | 74 | 29.1 |
| Artificial insemination (AIH) | 56 | 22.0 |
| In vitro fertilization (IVF) | 64 | 25.2 |
| Microinsemination (ICSI) | 56 | 22.0 |
| Other | 4 | 1.6 |
| Item | Factor I Self-Devaluation | Factor II Social Withdrawal | Factor III Public Stigma | Factor IV Family Stigma |
|---|---|---|---|---|
| Item 1: Because of infertility, I feel that I have an unfortunate fate. | 0.65 | 0.28 | 0.15 | 0.22 |
| Item 2: Because of infertility, I feel that I am a failure to be a woman. | 0.69 | 0.14 | 0.25 | 0.29 |
| Item 3: Because of infertility, I feel like a burden to my family. | 0.59 | −0.01 | 0.34 | 0.25 |
| Item 4: I feel inferior to others because of infertility. | 0.73 | 0.27 | 0.20 | 0.08 |
| Item 5: I am ashamed of being infertile. | 0.53 | 0.29 | 0.36 | 0.08 |
| Item 6: I look down on myself because of infertility. | 0.77 | 0.14 | 0.31 | 0.19 |
| Item 7: I feel useless at times because of infertility. | 0.76 | 0.02 | 0.31 | 0.24 |
| Item 8: I am more sensitive to pregnancy and child because I can’t get pregnant. | 0.60 | 0.44 | 0.10 | 0.06 |
| Item 9: I feel embarrassed when being asked something about the kids. | 0.44 | 0.59 | 0.24 | 0.11 |
| Item 10: I avoid getting close to people who don’t have fertility problem because of infertility,. | 0.42 | 0.53 | 0.22 | 0.21 |
| Item 11: I am unwilling to mention infertility. | 0.16 | 0.70 | 0.27 | 0.08 |
| Item 12: I try to conceal my condition from others. | 0.12 | 0.62 | 0.24 | -0.01 |
| Item 13: It is common that people discriminate against infertile women. | 0.27 | 0.20 | 0.50 | 0.22 |
| Item 14: I dare not make new friends lest they find out that I have infertility. | 0.12 | 0.48 | 0.48 | 0.24 |
| Item 15: I worry that people may stay away from me when they find out I have infertility. | 0.13 | 0.24 | 0.57 | 0.25 |
| Item 16: I worry that people may look down on me when they find out I have infertility. | 0.31 | 0.29 | 0.71 | 0.15 |
| Item 17: I worry that people may laugh at me when they find out I have infertility. | 0.22 | 0.22 | 0.77 | 0.15 |
| Item 18: Because of infertility, I feel like a freak (an incomplete woman) in the eyes of others. | 0.43 | 0.14 | 0.69 | 0.24 |
| Item 19: I feel that people judge me behind my back because of infertility. | 0.19 | 0.18 | 0.74 | 0.23 |
| Item 20: I feel that people around me look down on me because of infertility. | 0.34 | 0.19 | 0.79 | 0.18 |
| Item 21: I feel that people view me differently because of infertility. | 0.30 | 0.22 | 0.67 | 0.20 |
| Item 22: Having infertility has spoiled my life. | 0.15 | 0.16 | 0.25 | 0.69 |
| Item 23: I worry that the relationship with my husband would be worse. | 0.24 | 0.02 | 0.02 | 0.80 |
| Item 24: I am afraid my husband would divorce with me. | 0.15 | 0.00 | 0.10 | 0.77 |
| Item 25: I feel that my family does not take care for me as much as before because of infertility. | 0.01 | 0.14 | 0.31 | 0.65 |
| Item 26: Because of infertility, my family was always trying to make trouble for me. | 0.14 | 0.16 | 0.31 | 0.63 |
| Item 27: I am afraid my remarriage would be affected, once people know my situation. | 0.25 | 0.01 | 0.17 | 0.55 |
| Proportion of variance explained | 0.18 | 0.10 | 0.19 | 0.13 |
| Cumulative proportion of variance explained | 0.60 | |||
| KMO value | 0.93 | |||
| Bartlett’s test | chi-squared 4712.64, p < 0.001 | |||
| Item Number | Mean | SD | Cronbach’s α | |
|---|---|---|---|---|
| Total (ISS) | 27 | 73.62 | 20.87 | 0.95 |
| Self-devaluation | 7 | 22.79 | 6.82 | 0.91 |
| Social withdrawal | 5 | 16.74 | 4.77 | 0.83 |
| Public stigma | 9 | 21.89 | 8.50 | 0.93 |
| Family stigma | 6 | 12.20 | 5.21 | 0.86 |
| Item Number | Mean | SD | Item-Total Correlation a | Item-Remainder Correlation a | α |
|---|---|---|---|---|---|
| if Item Deleted | |||||
| Self-devaluation | |||||
| Item 1 | 3.26 | 1.14 | 0.65 | 0.62 | 0.90 |
| Item 2 | 3.10 | 1.23 | 0.71 | 0.68 | 0.89 |
| Item 3 | 3.13 | 1.25 | 0.64 | 0.61 | 0.90 |
| Item 4 | 3.84 | 1.14 | 0.66 | 0.63 | 0.90 |
| Item 5 | 2.92 | 1.19 | 0.66 | 0.62 | 0.90 |
| Item 6 | 3.35 | 1.20 | 0.73 | 0.70 | 0.89 |
| Item 7 | 3.18 | 1.28 | 0.72 | 0.68 | 0.89 |
| Social withdrawal | |||||
| Item 8 | 3.94 | 1.10 | 0.58 | 0.54 | 0.81 |
| Item 9 | 3.74 | 1.18 | 0.68 | 0.64 | 0.77 |
| Item 10 | 2.87 | 1.34 | 0.68 | 0.64 | 0.80 |
| Item 11 | 3.05 | 1.26 | 0.56 | 0.51 | 0.78 |
| Item 12 | 3.14 | 1.28 | 0.45 | 0.40 | 0.82 |
| Public stigma | |||||
| Item 13 | 2.87 | 1.17 | 0.63 | 0.60 | 0.93 |
| Item 14 | 2.21 | 1.10 | 0.65 | 0.62 | 0.93 |
| Item 15 | 2.07 | 1.07 | 0.65 | 0.61 | 0.93 |
| Item 16 | 2.60 | 1.18 | 0.77 | 0.74 | 0.92 |
| Item 17 | 2.19 | 1.09 | 0.74 | 0.71 | 0.92 |
| Item 18 | 2.67 | 1.29 | 0.80 | 0.78 | 0.92 |
| Item 19 | 2.15 | 1.14 | 0.73 | 0.70 | 0.92 |
| Item 20 | 2.49 | 1.25 | 0.80 | 0.78 | 0.92 |
| Item 21 | 2.65 | 1.28 | 0.74 | 0.71 | 0.92 |
| Family stigma | |||||
| Item22 | 2.06 | 1.09 | 0.58 | 0.55 | 0.84 |
| Item 23 | 2.37 | 1.33 | 0.50 | 0.46 | 0.83 |
| Item 24 | 1.80 | 1.03 | 0.48 | 0.45 | 0.83 |
| Item 25 | 1.71 | 0.89 | 0.51 | 0.48 | 0.85 |
| Item 26 | 2.01 | 1.11 | 0.60 | 0.56 | 0.84 |
| Item 27 | 2.25 | 1.23 | 0.54 | 0.49 | 0.86 |
| Test–Retest Application | Spearman Correlation Coefficient |
|---|---|
| Total (ISS) | 0.87 * |
| Self-devaluation | 0.86 * |
| Social withdrawal | 0.88 * |
| Public stigma | 0.80 * |
| Family Stigma | 0.61 * |
| Duration of Infertility (years) | ≤3 (N = 148) | >3 (N = 106) | U | p-Value | ||
|---|---|---|---|---|---|---|
| Median | IQR a | Median | IQR a | |||
| Total (ISS) | 71.0 | 28.20 | 81.0 | 28.80 | 6180.0 | 0.004 **b |
| Self-devaluation | 22.0 | 9.25 | 25.0 | 9.00 | 6247.5 | 0.006 **b |
| Social withdrawal | 17.0 | 6.00 | 18.0 | 6.00 | 6683.5 | 0.044 *b |
| Public stigma | 20.0 | 12.00 | 25.0 | 13.00 | 6247.5 | 0.006 **b |
| Family Stigma | 11.0 | 8.00 | 12.5 | 9.00 | 6539.0 | 0.023 *b |
| Total (ISS) | Self- Devaluation | Social Withdrawal | Public Stigma | Family Stigma | ||
|---|---|---|---|---|---|---|
| Multidimensional Scale of Perceived Social Support | ||||||
| Family | −0.36 ** | −0.22 ** | −0.22 ** | −0.31 ** | −0.48 ** | |
| Significant other | −0.36 ** | −0.23 ** | −0.20 * | −0.30 ** | −0.47 ** | |
| Friends | −0.37 ** | −0.28 ** | −0.29 ** | −0.33 ** | −0.29 ** | |
| Total score | −0.43 ** | −0.29 ** | −0.29 ** | −0.38 ** | −0.46 ** | |
| Rosenberg Self-esteem Scale | −0.51 ** | −0.57 ** | −0.33 ** | −0.36 ** | −0.36 ** | |
| Family APGAR | −0.32 ** | −0.23 ** | −0.12 | −0.25 ** | −0.44 ** | |
| Item Number | Convergent Validity a | Discriminant Validity b | Scaling Errors | |
|---|---|---|---|---|
| Self-devaluation | 7 | 0.63–0.80 | 0.28–0.68 | 3 (14.3%) |
| Social withdrawal | 5 | 0.52–0.70 | 0.19–0.58 | 4 (26.7%) |
| Public stigma | 9 | 0.62–0.84 | 0.33–0.58 | 0 |
| Family stigma | 6 | 0.60–0.76 | 0.13–0.49 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yokota, R.; Okada, H.; Okuhara, T.; Goto, E.; Furukawa, E.; Shirabe, R.; Sakakibara, K.; Kiuchi, T. Development of the Japanese Version of the Infertility Stigma Scale: Examination of Its Reliability and Validity. Healthcare 2022, 10, 505. https://doi.org/10.3390/healthcare10030505
Yokota R, Okada H, Okuhara T, Goto E, Furukawa E, Shirabe R, Sakakibara K, Kiuchi T. Development of the Japanese Version of the Infertility Stigma Scale: Examination of Its Reliability and Validity. Healthcare. 2022; 10(3):505. https://doi.org/10.3390/healthcare10030505
Chicago/Turabian StyleYokota, Rie, Hiroko Okada, Tsuyoshi Okuhara, Eiko Goto, Emi Furukawa, Ritsuko Shirabe, Keiko Sakakibara, and Takahiro Kiuchi. 2022. "Development of the Japanese Version of the Infertility Stigma Scale: Examination of Its Reliability and Validity" Healthcare 10, no. 3: 505. https://doi.org/10.3390/healthcare10030505
APA StyleYokota, R., Okada, H., Okuhara, T., Goto, E., Furukawa, E., Shirabe, R., Sakakibara, K., & Kiuchi, T. (2022). Development of the Japanese Version of the Infertility Stigma Scale: Examination of Its Reliability and Validity. Healthcare, 10(3), 505. https://doi.org/10.3390/healthcare10030505








