Clinical Diagnosis and Early Medical Management for Endometriosis: Consensus from Asian Expert Group
Abstract
1. Introduction
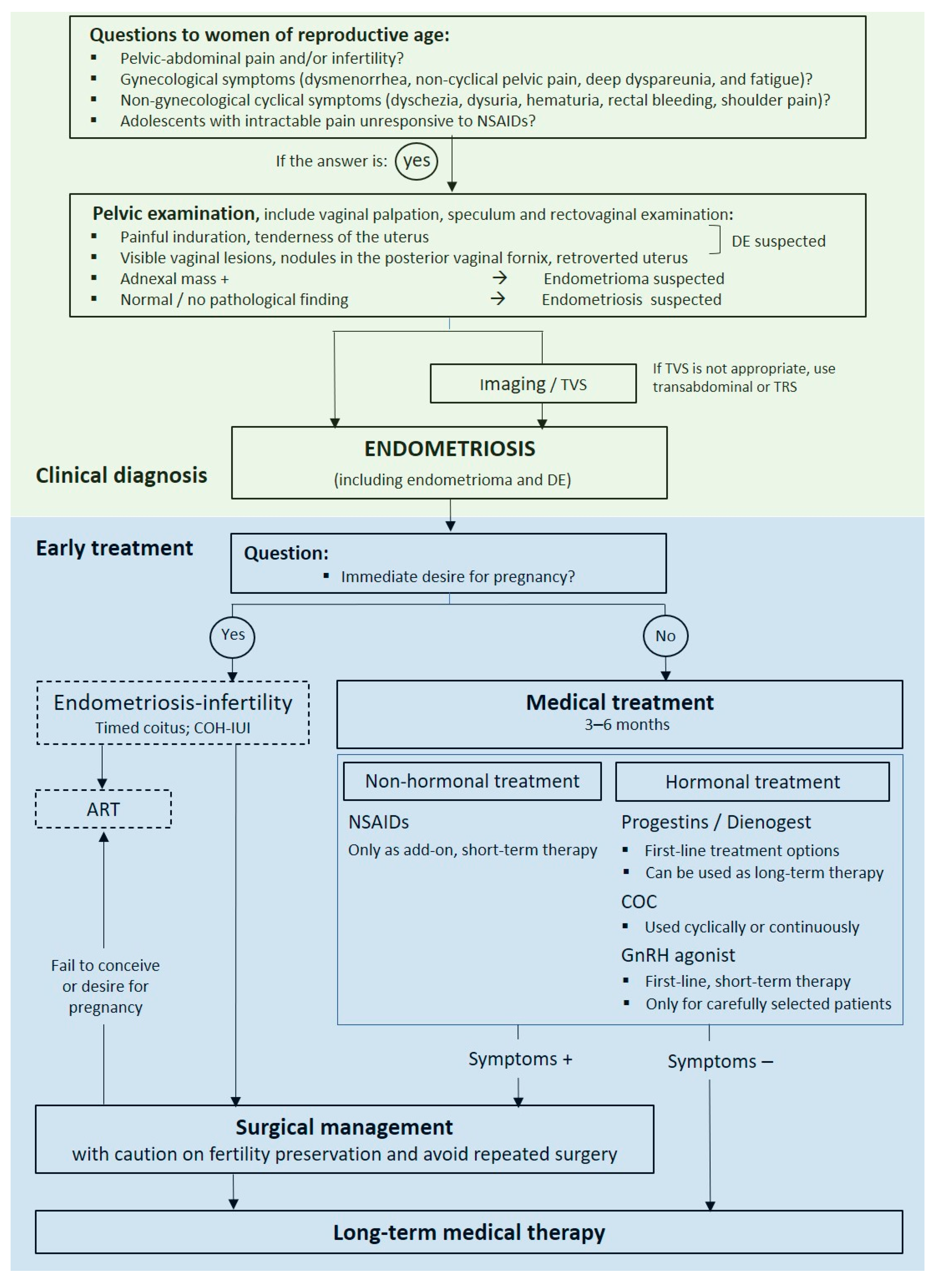
2. Clinical Diagnosis
2.1. Consensus: Focus Should Be Directed towards the Recognition of Symptoms That May Lead to the Diagnosis of Endometriosis, Such as Abdominal-Pelvic Pain and Infertility. These Symptoms Can Be Presumed to Be Endometriosis without the Need for Laparoscopy
2.2. Consensus: Transvaginal Sonography Is an Appropriate Imaging Technique in the Diagnosis of Pelvic Endometriosis
3. Early Empiric Medical Management
3.1. Consensus: Management of Women with a Presumptive Clinical Presentation Suggestive of Endometriosis Depends on the Individual Patient and Should Consider Her Presentation at That Time and the Need for Therapy
3.2. Consensus: Medical Treatment Is Recommended to Reduce Endometriosis-Associated Pelvic Pain for Patients Who Have No Immediate Desire for Pregnancy
3.3. Consensus: Hormonal Treatment Is a More Effective Option in the Treatment of Pelvic Pain from Clinically Diagnosed Endometriosis. Progestins Are among the First-Line Management Options for Early Medical Treatment
3.4. Consensus: Oral Progestin-Based Therapies Are Generally a Better Option Compared with COCs Because of Their Safety Profile
3.5. Consensus: Dienogest Can Be Used Long-Term If Needed
3.6. Consensus: A Large Evidence Base Exists Supporting the Use of Dienogest Compared with GnRH agonists as First-Line Medical Therapy for Endometriosis
3.7. Consensus: GnRH Agonists May Be Considered for First-Line Therapy Only in Some Specific Situations or as Short-Term Therapy before Dienogest
3.8. Consensus: NSAIDs May Be Considered as Add-on Therapy for Endometriosis-Associated Pelvic Pain
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giudice, L.C. Clinical practice. Endometriosis. N. Engl. J. Med. 2010, 362, 2389. [Google Scholar] [CrossRef] [PubMed]
- Parente Barbosa, C.; Bentes De Souza, A.M.; Bianco, B.; Christofolini, D.M. The effect of hormones on endometriosis development. Minerva Ginecol. 2011, 63, 375–386. [Google Scholar] [PubMed]
- Donnez, J.; Binda, M.M.; Donnez, O.; Dolmans, M.M. Oxidative stress in the pelvic cavity and its role in the pathogenesis of endometriosis. Fertil. Steril. 2016, 106, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Greene, A.D.; Lang, S.A.; Kendziorski, J.A.; Sroga-Rios, J.M.; Herzog, T.J.; Burns, K.A. Endometriosis: Where are we and where are we going? Reproduction 2016, 152, R63–R78. [Google Scholar] [CrossRef]
- Marinho, M.C.P.; Magalhaes, T.F.; Fernandes, L.F.C.; Augusto, K.L.; Brilhante, A.V.M.; Bezerra, L. Quality of Life in Women with Endometriosis: An Integrative Review. J. Womens Health (Larchmt) 2018, 27, 399–408. [Google Scholar] [CrossRef]
- Mehedintu, C.; Plotogea, M.N.; Ionescu, S.; Antonovici, M. Endometriosis still a challenge. J. Med. Life 2014, 7, 349–357. [Google Scholar]
- Subramaniam, R.; Sinthamoney, E.; Damodaran, P.; Kumarasamy, S.; Wai, T.S. Obstetrical and Gynecological Society of Malaysia Clinical Guidelines for the Management of Endometriosis. 2016. Available online: http://www.ogsm.org.my (accessed on 4 August 2019).
- Johnson, N.P.; Hummelshoj, L.; World Endometriosis Society Montpellier Consortium; Abrao, M.S.; Adamson, G.D.; Allaire, C.; Amelung, V.; Andersson, E.; Becker, C.; Birna Árdal, K.B.; et al. Consensus on current management of endometriosis. Hum. Reprod. 2013, 28, 1552–1568. [Google Scholar] [CrossRef]
- Rogers, P.A.; D’Hooghe, T.M.; Fazleabas, A.; Giudice, L.C.; Montgomery, G.W.; Petraglia, F.; Taylor, R.N. Defining future directions for endometriosis research: Workshop report from the 2011 World Congress of Endometriosis in Montpellier, France. Reprod Sci. 2013, 20, 483–499. [Google Scholar] [CrossRef]
- Dunselman, G.A.J.; Vermeulen, N.; Becker, C.; Calhaz-Jorge, C.; D’Hooghe, T.; De Bie, B.; Heikinheimo, O.; Horne, A.W.; Kiesel, L.; Nap, A.; et al. ESHRE guideline: Management of women with endometriosis. Hum. Reprod. 2014, 29, 400–412. [Google Scholar] [CrossRef]
- Fuldeore, M.J.; Soliman, A.M. Prevalence and Symptomatic Burden of Diagnosed Endometriosis in the United States: National Estimates from a Cross-Sectional Survey of 59,411 Women. Gynecol. Obstet. Investig. 2017, 82, 453–461. [Google Scholar] [CrossRef]
- Yen, C.F.; Kim, M.R.; Lee, C.L. Epidemiologic Factors Associated with Endometriosis in East Asia. Gynecol. Minim. Invasive Ther. 2019, 8, 4–11. [Google Scholar] [PubMed]
- Yasui, T.; Hayashi, K.; Nagai, K.; Mizunuma, H.; Kubota, T.; Lee, J.-S.; Suzuki, S. Risk profiles for endometriosis in Japanese women: Results from a repeated survey of self-reports. J. Epidemiol. 2015, 25, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.K.; Chapron, C.; Giudice, L.C.; Laufer, M.R.; Leyland, N.; Missmer, S.A.; Singh, S.S.; Taylor, H.S. Clinical diagnosis of endometriosis: A call to action. Am. J. Obstet. Gynecol. 2019, 220, 354.e1–354.e12. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.; Parker, M.; Sneddon, A.; Lopez, V.; Ellwood, D. Impact of endometriosis on women’s lives: A qualitative study. BMC Womens Health 2014, 14, 123. [Google Scholar] [CrossRef] [PubMed]
- Nnoaham, K.E.; Hummelshoj, L.; Webster, P.; d’Hooghe, T.; de Cicco Nardone, F.; de Cicco Nardone, C.; Jenkinson, C.; Kennedy, S.H.; Zondervan, K.T. World Endometriosis Research Foundation Global Study of Women’s Health consortium Impact of endometriosis on quality of life and work productivity: A multicenter study across ten countries. Fertil. Steril. 2011, 96, 366–373.e8. [Google Scholar] [CrossRef] [PubMed]
- Hudelist, G.; Fritzer, N.; Thomas, A.; Niehues, C.; Oppelt, P.; Haas, D.; Tammaa, A.; Salzer, H. Diagnostic delay for endometriosis in Austria and Germany: Causes and possible consequences. Hum. Reprod. 2012, 27, 3412–3416. [Google Scholar] [CrossRef] [PubMed]
- Fourquet, J.; Sinaii, N.; Stratton, P.; Khayel, F.; Alvarez-Garriga, C.; Bayona, M.; Ballweg, M.L.; Flores, I. Characteristics of women with endometriosis from the USA and Puerto Rico. J. Endometr. Pelvic. Pain Disord. 2015, 7, 129–135. [Google Scholar] [CrossRef]
- Staal, A.H.; van der Zanden, M.; Nap, A.W. Diagnostic Delay of Endometriosis in the Netherlands. Gynecol. Obstet. Invest. 2016, 81, 321–324. [Google Scholar] [CrossRef]
- Soliman, A.M.; Fuldeore, M.; Snabes, M.C. Factors Associated with Time to Endometriosis Diagnosis in the United States. J. Women’s Health 2017, 26, 788–797. [Google Scholar] [CrossRef]
- Chapron, C.; Marcellin, L.; Borghese, B.; Santulli, P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat. Rev. Endocrinol. 2019, 15, 666–682. [Google Scholar] [CrossRef]
- Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: A committee opinion. Fertil. Steril. 2014, 101, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Rafique, S.; Decherney, A.H. Medical Management of Endometriosis. Clin. Obstet. Gynecol. 2017, 60, 485–496. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Endometriosis: Diagnosis and management (ng73); National Institute for Health and Care Excellence: London, UK, 2017. [Google Scholar]
- Ulrich, U.; Buchweitz, O.; Greb, R.; Keckstein, J.; von Leffern, I.; Oppelt, P.; Renner, S.P.; Sillem, M.; Stummvoll, W.; De Wilde, R.L. National German Guideline (S2k): Guideline for the Diagnosis and Treatment of Endometriosis: Long Version—AWMF Registry No. 015-045. Geburtshilfe Frauenheilkd 2014, 74, 1104–1118. [Google Scholar] [PubMed]
- Hwang, H.; Chung, Y.J.; Lee, S.R.; Park, H.T.; Song, J.Y.; Kim, H.; Lee, D.Y.; Lee, E.J.; Kim, M.R.; Oh, S.T. Clinical evaluation and management of endometriosis: Guideline for Korean patients from Korean Society of Endometriosis. Obstet. Gynecol. Sci. 2018, 61, 553–564. [Google Scholar] [CrossRef]
- FOGSI Good Clinical Practice Recommendations on Endometriosis. 2017. Available online: https://www.fogsi.org/wp-content/uploads/2017/01/GCRP-2017-final.pdf (accessed on 10 December 2022).
- Chapron, C.; Dubuisson, J.-B.; Pansini, V.; Vieira, M.; Fauconnier, A.; Barakat, H.; Dousset, B. Routine clinical examination is not sufficient for diagnosing and locating deeply infiltrating endometriosis. J. Am. Assoc. Gynecol. Laparosc 2002, 9, 115–119. [Google Scholar] [CrossRef]
- Hurd, W.W. Criteria that indicate endometriosis is the cause of chronic pelvic pain. Obstet. Gynecol. 1998, 92, 1029–1032. [Google Scholar]
- Chapron, C.; Lang, J.-H.; Leng, J.-H.; Zhou, Y.; Zhang, X.; Xue, M.; Popov, A.; Romanov, V.; Maisonobe, P.; Cabri, P. Factors and Regional Differences Associated with Endometriosis: A Multi-Country, Case-Control Study. Adv. Ther. 2016, 33, 1385–1407. [Google Scholar] [CrossRef]
- Saha, R.; Marions, L.; Tornvall, P. Validity of self-reported endometriosis and endometriosis-related questions in a Swedish female twin cohort. Fertil. Steril. 2017, 107, 174–178.e2. [Google Scholar] [CrossRef]
- Flores, I.; Abreu, S.; Abac, S.; Fourquet, J.; Laboy, J.; Rios-Bedoya, C. Self-reported prevalence of endometriosis and its symptoms among Puerto Rican women. Int. J. Gynaecol. Obstet. 2008, 100, 257–261. [Google Scholar] [CrossRef]
- Ballard, K.D.; Seaman, H.E.; de Vries, C.S.; Wright, J.T. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study—Part 1. BJOG 2008, 115, 1382–1391. [Google Scholar] [CrossRef]
- Lafay Pillet, M.C.; Huchon, C.; Santulli, P.; Borghese, B.; Chapron, C.; Fauconnier, A. A clinical score can predict associated deep infiltrating endometriosis before surgery for an endometrioma. Hum. Reprod. 2014, 29, 1666–1676. [Google Scholar] [CrossRef] [PubMed]
- Matalliotakis, I.M.; Cakmak, H.; Fragouli, Y.G.; Goumenou, A.G.; Mahutte, N.G.; Arici, A. Epidemiological characteristics in women with and without endometriosis in the Yale series. Arch. Gynecol. Obstet. 2008, 277, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Ashrafi, M.; Sadatmahalleh, S.J.; Akhoond, M.R.; Talebi, M. Evaluation of Risk Factors Associated with Endometriosis in Infertile Women. Int. J. Fertil. Steril. 2016, 10, 11–21. [Google Scholar] [PubMed]
- Arruda, M.S.; Petta, C.A.; Abrao, M.S.; Benetti-Pinto, C.L. Time elapsed from onset of symptoms to diagnosis of endometriosis in a cohort study of Brazilian women. Hum. Reprod. 2003, 18, 756–759. [Google Scholar] [CrossRef]
- ACOG Committee Opinion No.760: Dysmenorrhea and Endometriosis in the Adolescent. Obstet. Gynecol. 2018, 132, e249–e258.
- Hudelist, G.; Oberwinkler, K.; Singer, C.; Tuttlies, F.; Rauter, G.; Ritter, O.; Keckstein, J. Combination of transvaginal sonography and clinical examination for preoperative diagnosis of pelvic endometriosis. Hum. Reprod. 2009, 24, 1018–1024. [Google Scholar] [CrossRef]
- Bazot, M.; Lafont, C.; Rouzier, R.; Roseau, G.; Thomassin-Naggara, I.; Darai, E. Diagnostic accuracy of physical examination, transvaginal sonography, rectal endoscopic sonography, and magnetic resonance imaging to diagnose deep infiltrating endometriosis. Fertil. Steril. 2009, 92, 1825–1833. [Google Scholar] [CrossRef]
- Hudelist, G.; Ballard, K.; English, J.; Wright, J.; Banerjee, S.; Mastoroudes, H.; Thomas, A.; Singer, C.F.; Keckstein, J. Transvaginal sonography vs. clinical examination in the preoperative diagnosis of deep infiltrating endometriosis. Ultrasound Obs. Gynecol. 2011, 37, 480–487. [Google Scholar] [CrossRef]
- Riazi, H.; Tehranian, N.; Ziaei, S.; Mohammadi, E.; Hajizadeh, E.; Montazeri, A. Clinical diagnosis of pelvic endometriosis: A scoping review. BMC Womens Health 2015, 15, 39. [Google Scholar] [CrossRef]
- Long, W.N. Pelvic Examination. In Clinical Methods: The History, Physical, and Laboratory Examinations; A division of Reed Publishing, Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworth Publishers: Boston, MA, USA, 1990. [Google Scholar]
- Foti, P.V.; Farina, R.; Palmucci, S.; Vizzini, I.A.A.; Libertini, N.; Coronella, M.; Spadola, S.; Caltabiano, R.; Iraci, M.; Basile, A.; et al. Endometriosis: Clinical features, MR imaging findings and pathologic correlation. Insights Imaging 2018, 9, 149–172. [Google Scholar] [CrossRef]
- Bianek-Bodzak, A.; Szurowska, E.; Sawicki, S.; Liro, M. The importance and perspective of magnetic resonance imaging in the evaluation of endometriosis. Biomed. Res. Int. 2013, 2013, 436589. [Google Scholar] [CrossRef] [PubMed]
- Marasinghe, J.P.; Senanayake, H.; Saravanabhava, N.; Arambepola, C.; Condous, G.; Greenwood, P. History, pelvic examination findings and mobility of ovaries as a sonographic marker to detect pelvic adhesions with fixed ovaries. J. Obstet. Gynaecol. Res. 2014, 40, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, S.; Condous, G.; van den Bosch, T.; Valentin, L.; Leone, F.P.G.; Van Schoubroeck, D.; Exacoustos, C.; Installé, A.J.F.; Martins, W.P.; Abrao, M.S.; et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: A consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet. Gynecol. 2016, 48, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, V.H.; Alcazar, J.L.; Arbib, N.; Schiff, E.; Achiron, R.; Goldenberg, M.; et, al. Applying a statistical method in transvaginal ultrasound training: Lessons from the learning curve cumulative summation test (LC-CUSUM) for endometriosis mapping. Gynecol. Surg. 2017, 14, 19. [Google Scholar] [CrossRef] [PubMed]
- Alborzi, S.; Rasekhi, A.; Shomali, Z.; Madadi, G.; Alborzi, M.; Kazemi, M.; Nohandani, A.H. Diagnostic accuracy of magnetic resonance imaging, transvaginal, and transrectal ultrasonography in deep infiltrating endometriosis. Medicine 2018, 97, e9536. [Google Scholar] [CrossRef]
- Janssen, E.B.; Rijkers, A.C.; Hoppenbrouwers, K.; Meuleman, C.; D’Hooghe, T.M. Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: A systematic review. Hum. Reprod. Update 2013, 19, 570–582. [Google Scholar] [CrossRef]
- Becker, C.M.; Bokor, A.; Heikinheimo, O.; Horne, A.; Jansen, F.; Kiesel, L.; King, K.; Kvaskoff, M.; Nap, A.; Petersen, K. ESHRE guideline: Endometriosis. Hum. Reprod. Open 2022, 2022, hoac009. [Google Scholar] [CrossRef]
- Brown, J.; Kives, S.; Akhtar, M. Progestagens and anti-progestagens for pain associated with endometriosis. Cochrane Database Syst. Rev. 2012, 2012, CD002122. [Google Scholar] [CrossRef]
- Li, Y.; Adur, M.K.; Kannan, A.; Davila, J.; Zhao, Y.; Nowak, R.A.; Bagchi, M.K.; Bagchi, I.C.; Li, Q. Progesterone Alleviates Endometriosis via Inhibition of Uterine Cell Proliferation, Inflammation and Angiogenesis in an Immunocompetent Mouse Model. PLoS ONE 2016, 11, e0165347. [Google Scholar] [CrossRef]
- Patel, B.G.; Rudnicki, M.; Yu, J.; Shu, Y.; Taylor, R.N. Progesterone resistance in endometriosis: Origins, consequences and interventions. Acta Obstet. Gynecol. Scand. 2017, 96, 623–632. [Google Scholar] [CrossRef]
- Casper, R.F. Progestin-only pills may be a better first-line treatment for endometriosis than combined estrogen-progestin contraceptive pills. Fertil. Steril. 2017, 107, 533–536. [Google Scholar] [CrossRef] [PubMed]
- Vercellini, P.; Trespidi, L.; Colombo, A.; Vendola, N.; Marchini, M.; Crosignani, P.G. A gonadotropin-releasing hormone agonist versus a low-dose oral contraceptive for pelvic pain associated with endometriosis. Fertil. Steril. 1993, 60, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Hillard, P.A. Menstrual suppression: Current perspectives. Int. J. Womens Health 2014, 6, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Grimes, D.A.; Lopez, L.M.; O’Brien, P.A.; Raymond, E.G. Progestin-only pills for contraception. Cochrane Database Syst. Rev. 2013, 2013, CD007541. [Google Scholar] [CrossRef] [PubMed]
- Edelman, A.; Micks, E.; Gallo, M.F.; Jensen, J.T.; Grimes, D.A. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst. Rev. 2014, 2014, CD004695. [Google Scholar] [CrossRef]
- Kitawaki, J.; Kado, N.; Ishihara, H.; Koshiba, H.; Kitaoka, Y.; Honjo, H. Endometriosis: The pathophysiology as an estrogen-dependent disease. J. Steroid. Biochem. Mol. Biol. 2002, 83, 149–155. [Google Scholar] [CrossRef]
- Noël, J.-C.; Chapron, C.; Bucella, D.; Buxant, F.; Peny, M.-O.; Fayt, I.; Borghese, B.; Anaf, V. Estrogen and progesterone receptors in smooth muscle component of deep infiltrating endometriosis. Fertil. Steril. 2010, 93, 1774–1777. [Google Scholar] [CrossRef]
- Zeun, S.; Lu, M.; Uddin, A.; Zeiler, B.; Morrison, D.; Blode, H. Pharmacokinetics of an oral contraceptive containing oestradiol valerate and dienogest. Eur. J. Contracept Reprod Health Care 2009, 14, 221–232. [Google Scholar] [CrossRef]
- Vercellini, P.; Eskenazi, B.; Consonni, D.; Somigliana, E.; Parazzini, F.; Abbiati, A.; Fedele, L. Oral contraceptives and risk of endometriosis: A systematic review and meta-analysis. Hum. Reprod. Update 2011, 17, 159–170. [Google Scholar] [CrossRef]
- Chapron, C.; Souza, C.; Borghese, B.; Lafay-Pillet, M.-C.; Santulli, P.; Bijaoui, G.; Goffinet, F.; de Ziegler, D. Oral contraceptives and endometriosis: The past use of oral contraceptives for treating severe primary dysmenorrhea is associated with endometriosis, especially deep infiltrating endometriosis. Hum. Reprod. 2011, 26, 2028–2035. [Google Scholar] [CrossRef]
- Meresman, G.F.; Auge, L.; Baranao, R.I.; Lombardi, E.; Tesone, M.; Sueldo, C. Oral contraceptives suppress cell proliferation and enhance apoptosis of eutopic endometrial tissue from patients with endometriosis. Fertil. Steril. 2002, 77, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- OHara, R.; Rowe, H.; Roufeil, L.; Fisher, J. Should endometriosis be managed within a chronic disease framework? An analysis of national policy documents. Aust. Health Rev. 2018, 42, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Canis, M.; Bourdel, N.; Houlle, C.; Gremeau, A.S.; Botchorishvili, R.; Matsuzaki, S. Endometriosis may not be a chronic disease: An alternative theory offering more optimistic prospects for our patients. Fertil. Steril. 2016, 105, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Andres Mde, P.; Lopes, L.A.; Baracat, E.C.; Podgaec, S. Dienogest in the treatment of endometriosis: Systematic review. Arch. Gynecol. Obstet. 2015, 292, 523–529. [Google Scholar] [CrossRef]
- Grandi, G.; Mueller, M.; Bersinger, N.A.; Cagnacci, A.; Volpe, A.; McKinnon, B. Does dienogest influence the inflammatory response of endometriotic cells? A systematic review. Inflamm. Res. 2016, 65, 183–192. [Google Scholar] [CrossRef]
- Hayashi, A.; Tanabe, A.; Kawabe, S.; Hayashi, M.; Yuguchi, H.; Yamashita, Y.; Okuda, K.; Ohmichi, M. Dienogest increases the progesterone receptor isoform B/A ratio in patients with ovarian endometriosis. J. Ovarian. Res. 2012, 5, 31. [Google Scholar] [CrossRef]
- Flores, V.A.; Vanhie, A.; Dang, T.; Taylor, H.S. Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis. J. Clin. Endocrinol. Metab. 2018, 103, 4561–4568. [Google Scholar] [CrossRef] [PubMed]
- Petraglia, F.; Hornung, D.; Seitz, C.; Faustmann, T.; Gerlinger, C.; Luisi, S.; Lazzeri, L.; Strowitzki, T. Reduced pelvic pain in women with endometriosis: Efficacy of long-term dienogest treatment. Arch. Gynecol. Obstet. 2012, 285, 167–173. [Google Scholar] [CrossRef]
- Momoeda, M.; Harada, T.; Terakawa, N.; Aso, T.; Fukunaga, M.; Hagino, H.; Taketani, Y. Long-term use of dienogest for the treatment of endometriosis. J. Obstet. Gynaecol. Res. 2009, 35, 1069–1076. [Google Scholar] [CrossRef]
- Kohler, G.; Faustmann, T.A.; Gerlinger, C.; Seitz, C.; Mueck, A.O. A dose-ranging study to determine the efficacy and safety of 1, 2, and 4 mg of dienogest daily for endometriosis. Int. J. Gynaecol. Obstet. 2010, 108, 21–25. [Google Scholar] [CrossRef]
- Strowitzki, T.; Marr, J.; Gerlinger, C.; Faustmann, T.; Seitz, C. Dienogest is as effective as leuprolide acetate in treating the painful symptoms of endometriosis: A 24-week, randomized, multicentre, open-label trial. Hum. Reprod. 2010, 25, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Harada, T.; Momoeda, M.; Taketani, Y.; Aso, T.; Fukunaga, M.; Hagino, H.; Terakawa, N. Dienogest is as effective as intranasal buserelin acetate for the relief of pain symptoms associated with endometriosis--a randomized, double-blind, multicenter, controlled trial. Fertil. Steril. 2009, 91, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Cosson, M.; Querleu, D.; Donnez, J.; Madelenat, P.; Konincks, P.; Audebert, A.; Manhes, H. Dienogest is as effective as triptorelin in the treatment of endometriosis after laparoscopic surgery: Results of a prospective, multicenter, randomized study. Fertil. Steril. 2002, 77, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Romer, T. Long-term treatment of endometriosis with dienogest: Retrospective analysis of efficacy and safety in clinical practice. Arch. Gynecol. Obstet. 2018, 298, 747–753. [Google Scholar] [CrossRef]
- Ota, Y.; Andou, M.; Yanai, S.; Nakajima, S.; Fukuda, M.; Takano, M.; Kurotsuchi, S.; Ebisawa, K.; Hada, T.; Ota, I. Long-Term Administration of Dienogest Reduces Recurrence after Excision of Endometrioma. J. Endometr. Pelvic Pain Disord. 2015, 7, 63–67. [Google Scholar] [CrossRef]
- Ebert, A.D.; Dong, L.; Merz, M.; Kirsch, B.; Francuski, M.; Böttcher, B.; Roman, H.; Suvitie, P.; Hlavackova, O.; Gude, K.; et al. Dienogest 2 mg Daily in the Treatment of Adolescents with Clinically Suspected Endometriosis: The VISanne Study to Assess Safety in ADOlescents. J. Pediatr. Adolesc. Gynecol. 2017, 30, 560–567. [Google Scholar] [CrossRef]
- Ferrero, S.; Remorgida, V.; Venturini, P.L.; Bizzarri, N. Endometriosis: The effects of dienogest. BMJ Clin. Evid 2015, 2015, 0802. [Google Scholar]
- Strowitzki, T.; Marr, J.; Gerlinger, C.; Faustmann, T.; Seitz, C. Detailed analysis of a randomized, multicenter, comparative trial of dienogest versus leuprolide acetate in endometriosis. Int. J. Gynaecol. Obstet. 2012, 117, 228–233. [Google Scholar] [CrossRef]
- Brown, J.; Pan, A.; Hart, R.J. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst. Rev. 2010, 2010, CD008475. [Google Scholar]
- Kitawaki, J.; Kusuki, I.; Yamanaka, K.; Suganuma, I. Maintenance therapy with dienogest following gonadotropin-releasing hormone agonist treatment for endometriosis-associated pelvic pain. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 157, 212–216. [Google Scholar] [CrossRef]
- Brown, J.; Crawford, T.J.; Allen, C.; Hopewell, S.; Prentice, A. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst. Rev. 2017, 1, CD004753. [Google Scholar] [CrossRef] [PubMed]
- Marjoribanks, J.; Ayeleke, R.O.; Farquhar, C.; Proctor, M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst. Rev. 2015, 2015, CD001751. [Google Scholar] [CrossRef] [PubMed]
- Salman, S.; Sherif, B.; Al-Zohyri, A. OP0131 Effects of Some Non Steroidal Anti-Inflammatory Drugs on Ovulation in Women with Mild Musculoskeletal Pain. Ann. Rheum. Dis. 2015, 74, 117–118. [Google Scholar] [CrossRef]
| Group | Title | Reference |
|---|---|---|
| Global | ||
| World Endometriosis Society Montpellier Consortium | Consensus on current management of endometriosis | Johnson et al., 2013 [8] |
| European | ||
| The European Society of Human Reproduction and Embryology (ESHRE) | ESHRE guideline: management of women with endometriosis | Dunselman et al., 2014 [10] |
| National Institute for Health and Care Excellence (NICE) | Endometriosis: diagnosis and management | NICE 2017 [24] |
| National German Guideline | National German guideline (S2k): Guideline for the diagnosis and treatment of endometriosis | Ulrich et al., 2014 [25] |
| North American | ||
| American Society for Reproductive Medicine (ASRM) | Treatment of pelvic pain associated with endometriosis: a committee opinion | The Practice Committee of the American Society for Reproductive Medicine 2014 [22] |
| Asian | ||
| Korean Society of Endometriosis (KSE) | Clinical evaluation and management of endometriosis: guideline for Korean patients from Korean Society of Endometriosis | Hwang et al., 2018 [26] |
| Obstetrical and Gynaecological Society of Malaysia | Clinical guidelines for the management of endometriosis 2016 | Subramaniam et al., 2016 [7] |
| The Federation of Obstetric and Gynaecological Societies of India (FOGSI) | Good Clinical Practice Recommendations on Endometriosis | FOGSI 2017 [27] |
| Study | Population (Age) | Intervention a (Setting) | Treatment Length | Outcomes |
|---|---|---|---|---|
| Cosson et al. [77] | n = 130 (mean: 28.5–30.3 y) | DNG vs. GnRH b (post-surgical consolidation therapy) | 16 wks |
|
| Harada et al. [76] | n = 271 (mean: 33.5–33.8 y) | DNG vs. GnRH c | 24 wks |
|
| Strowitzki et al. [75] | n = 229 (mean: 30.6–31.0 y) | DNG vs. GnRH d | 24 wks |
|
| Köhler et al. [74] | n = 68 (mean: 27.6–33.5 y) | DNG e (dose-finding study) | 24 wks |
|
| Momoeda et al. [73] | n = 135 (mean: 34.1 y) | DNG | 52 wks |
|
| Petraglia et al. [72] | n = 152 (18–45 y f) | DNG | 36–52 wks |
|
| Ebert et al. [80] | n = 111 (adolescents; median [range] 16.0 [12,13,14,15,16,17] y) | DNG | 52 wks |
|
| Römer [78] | n = 37 (39 y) | DNG | 60 mo |
|
| Ota et al. [79] | n = 151 (32.6 y) | DNG vs. no therapy (post-surgical therapy) | 60 mo |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.-R.; Chapron, C.; Römer, T.; Aguilar, A.; Chalermchockcharoenkit, A.; Chatterjee, S.; Dao, L.T.A.; Fong, Y.F.; Hendarto, H.; Hidayat, S.T.; et al. Clinical Diagnosis and Early Medical Management for Endometriosis: Consensus from Asian Expert Group. Healthcare 2022, 10, 2515. https://doi.org/10.3390/healthcare10122515
Kim M-R, Chapron C, Römer T, Aguilar A, Chalermchockcharoenkit A, Chatterjee S, Dao LTA, Fong YF, Hendarto H, Hidayat ST, et al. Clinical Diagnosis and Early Medical Management for Endometriosis: Consensus from Asian Expert Group. Healthcare. 2022; 10(12):2515. https://doi.org/10.3390/healthcare10122515
Chicago/Turabian StyleKim, Mee-Ran, Charles Chapron, Thomas Römer, Angela Aguilar, Amphan Chalermchockcharoenkit, Siddharta Chatterjee, Le Thi Anh Dao, Yoke Fai Fong, Hendy Hendarto, Syarief Taufik Hidayat, and et al. 2022. "Clinical Diagnosis and Early Medical Management for Endometriosis: Consensus from Asian Expert Group" Healthcare 10, no. 12: 2515. https://doi.org/10.3390/healthcare10122515
APA StyleKim, M.-R., Chapron, C., Römer, T., Aguilar, A., Chalermchockcharoenkit, A., Chatterjee, S., Dao, L. T. A., Fong, Y. F., Hendarto, H., Hidayat, S. T., Khong, S. Y., Ma, L., Kumar, P., Primariawan, R. Y., Siow, A., Sophonsritsuk, A., Devi Thirunavukarasu, R., Thuong, B. C., & Yen, C.-F. (2022). Clinical Diagnosis and Early Medical Management for Endometriosis: Consensus from Asian Expert Group. Healthcare, 10(12), 2515. https://doi.org/10.3390/healthcare10122515





