Ataxia Rating Scales: Content Analysis by Linking to the International Classification of Functioning, Disability and Health
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Ataxia Rating Scales
2.2. Description of Ataxia Rating Scales
- (1)
- SARA has eight items to assess motor performance, speech disturbance, coordination, and limb kinetic functions. The application time is 14.2 ± 7.5 min [5].
- (2)
- ICARS consists of 19 items, divided into posture and gait disturbance, limb kinetic function, speech disorders, and oculomotor disorders. The application time is 21.3 ± 7 min [9].
- (3)
- FARS has 36 items distributed in 4 domains: (I) functional staging of ataxia; (II) activity of daily life; (III) neurological assessment of bulbar, upper and lower limbs, peripheral nerve, and upright stability/gait functions; and (IV) quantitative timed activities—PATA rate, nine-hole pegboard, and timed 25-foot walk test. It needs more than 30 min to be administrated [7].
- (4)
- UMSARS has 30 items comprising four parts, including a historical review of disease-related impairments, motor examination, autonomic examination, and the global disability scale. The application time is 30–45 min [10].
2.3. ICF
2.4. Procedure of ICF Linking
2.5. Interrater Rating Agreement
2.6. ICF Linking Indicators
2.6.1. Measure to ICF Linkage
2.6.2. Measure of Linking to Unique ICF Codes
3. Results
3.1. Meaningful Concepts
3.2. ICF Linking Results
3.2.1. Representation of Body Structure
3.2.2. Representation of Body Function
3.2.3. Representation of Activity and Participation
3.2.4. Representation of Environmental Factors
3.3. Content Comparison
3.4. Unspecified-ICF Categories
- (1)
- “b 7159 Stability of joint functions, unspecified” that was linked to “Falling” concept in UMSARS and FARS.
- (2)
- “d 4509 Walking, unspecified” that was linked for “changing walking direction” or “tandem walking” concepts in all included scales.
- (3)
- “d 599 Self-care, unspecified” that was linked to “hygiene care” concept in FARS.
3.5. Agreement between Authors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Klockgether, T. Sporadic Adult-Onset Ataxia. Handb. Clin. Neurol. 2018, 155, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Xiong, E.; Lynch, A.E.; Corben, L.A.; Delatycki, M.B.; Subramony, S.H.; Bushara, K.; Gomez, C.M.; Hoyle, J.C.; Yoon, G.; Ravina, B.; et al. Health Related Quality of Life in Friedreich Ataxia in a Large Heterogeneous Cohort. J. Neurol. Sci. 2020, 410, 116642. [Google Scholar] [CrossRef] [PubMed]
- Milne, S.C.; Corben, L.A.; Georgiou-Karistianis, N.; Delatycki, M.B.; Yiu, E.M. Rehabilitation for Individuals with Genetic Degenerative Ataxia: A Systematic Review. Neurorehabil. Neural Repair 2017, 31, 609–622. [Google Scholar] [CrossRef] [PubMed]
- Perez-Lloret, S.; van de Warrenburg, B.; Rossi, M.; Rodríguez-Blázquez, C.; Zesiewicz, T.; Saute, J.A.M.; Durr, A.; Nishizawa, M.; Martinez-Martin, P.; Stebbins, G.T.; et al. Assessment of Ataxia Rating Scales and Cerebellar Functional Tests: Critique and Recommendations. Mov. Disord. 2021, 36, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Schmitz-Hübsch, T.; Du Montcel, S.T.; Baliko, L.; Berciano, J.; Boesch, S.; Depondt, C.; Giunti, P.; Globas, C.; Infante, J.; Kang, J.S.; et al. Scale for the Assessment and Rating of Ataxia: Development of a New Clinical Scale. Neurology 2006, 66, 1717–1720. [Google Scholar] [CrossRef]
- Trouillas, P.; Takayanagi, T.; Hallett, M.; Currier, R.D.; Subramony, S.H.; Wessel, K.; Bryer, A.; Diener, H.C.; Massaquoi, S.; Gomez, C.M.; et al. International Cooperative Ataxia Rating Scale for Pharmacological Assessment of the Cerebellar Syndrome. J. Neurol. Sci. 1997, 145, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Subramony, S.H.; May, W.; Lynch, D.; Gomez, C.; Fischbeck, K.; Hallett, M.; Taylor, P.; Wilson, R.; Ashizawa, T. Measuring Friedreich Ataxia: Interrater Reliability of a Neurologic Rating Scale. Neurology 2005, 64, 1261–1262. [Google Scholar] [CrossRef]
- Meissner, W.G.; Fernagut, P.O.; Dehay, B.; Péran, P.; Traon, A.P.-L.; Foubert-Samier, A.; Lopez Cuina, M.; Bezard, E.; Tison, F.; Rascol, O. Multiple System Atrophy: Recent Developments and Future Perspectives. Mov. Disord. 2019, 34, 1629–1642. [Google Scholar] [CrossRef]
- Schmitz-Hübsch, T.; du Montcel, S.T.; Baliko, L.; Boesch, S.; Bonato, S.; Fancellu, R.; Giunti, P.; Globas, C.; Kang, J.S.; Kremer, B.; et al. Reliability and Validity of the International Cooperative Ataxia Rating Scale: A Study in 156 Spinocerebellar Ataxia Patients. Mov. Disord. 2006, 21, 699–704. [Google Scholar] [CrossRef]
- Wenning, G.K.; Tison, F.; Seppi, K.; Sampiao, C.; Diem, A.; Yekhlef, F.; Ghorayeb, I.; Ory, F.; Galitzky, M.; Scaravilli, T.; et al. Development and Validation of the Unified Multiple System Atrophy Rating Scale (UMSARS). Mov. Disord. 2004, 19, 1391–1402. [Google Scholar] [CrossRef]
- Organization World Health. International Classification of Functioning, Disability and Health; Organization World Health: Geneva, Switzerland, 2001. [Google Scholar]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Üstün, B.; Stucki, G. ICF Linking Rules: An Update Based on Lessons Learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Fayed, N.; Bickenbach, J.; Prodinger, B. Refinements of the ICF Linking Rules to Strengthen Their Potential for Establishing Comparability of Health Information. Disabil. Rehabil. 2016, 41, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Whitney, S.L.; Alghadir, A.; Alghwiri, A.; Alshebber, K.M.; Alshehri, M.; Furman, J.M.; Mueller, M.; Grill, E. The Development of the ICF Vestibular Environmental Scale. J. Vestib. Res. 2016, 26, 297–302. [Google Scholar] [CrossRef]
- Alghwiri, A.A.; Almhdawi, K.A.; Marchetti, G. Are Fatigue Scales the Same? A Content Comparison Using the International Classification of Functioning, Disability and Health. Mult. Scler. Relat. Disord. 2020, 46, 102596. [Google Scholar] [CrossRef]
- Alghwiri, A.A.; Marchetti, G.F.; Whitney, S.L. Content Comparison of Self-Report Measures Used in Vestibular Rehabilitation Based on the International Classification of Functioning, Disability and Health. Phys. Ther. 2011, 91, 346–357. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gliner, J.A.; Morgan, G.A.; Harmon, R.J. Measurement Reliability. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 486–488. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C. ICF Linking and Cognitive Interviewing Are Complementary Methods for Optimizing Content Validity of Outcome Measures: An Integrated Methods Review. Front. Rehabil. Sci. 2021, 2, 702596. [Google Scholar] [CrossRef]
- Bladh, S.; Nilsson, M.H.; Carlsson, G.; Lexell, J. Content Analysis of 4 Fear of Falling Rating Scales by Linking to the International Classification of Functioning, Disability and Health. PM&R 2013, 5, 573–582. [Google Scholar] [CrossRef]
- Tiwari, D.; Clock, C.; Gore, S.; Alsalaheen, B. Content Comparison of Neck Pain Outcome Measures Using the International Classification of Functioning, Disability and Health. Int. J. Rehabil. Res. 2022, 45, 24–32. [Google Scholar] [CrossRef]
- Cieza, A.; Stucki, G. Content Comparison of Health-Related Quality of Life (HRQOL) Instruments Based on the International Classification of Functioning, Disability and Health (ICF). Qual. Life Res. 2005, 14, 1225–1237. [Google Scholar] [CrossRef]
- Pearson, T.S. More than Ataxia: Hyperkinetic Movement Disorders in Childhood Autosomal Recessive Ataxia Syndromes. Tremor Other Hyperkinetic Mov. 2016, 6, 368. [Google Scholar] [CrossRef]
- Moon, Y.; Sung, J.H.; An, R.; Hernandez, M.E.; Sosnoff, J.J. Gait Variability in People with Neurological Disorders: A Systematic Review and Meta-Analysis. Hum. Mov. Sci. 2016, 47, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Saute, J.A.M.; Donis, K.C.; Serrano-Munuera, C.; Genis, D.; Ramirez, L.T.; Mazzetti, P.; Pérez, L.V.; Latorre, P.; Sequeiros, J.; Matilla-Duenas, A.; et al. Ataxia Rating Scales-Psychometric Profiles, Natural History and Their Application in Clinical Trials. Cerebellum 2012, 11, 488–504. [Google Scholar] [CrossRef] [PubMed]
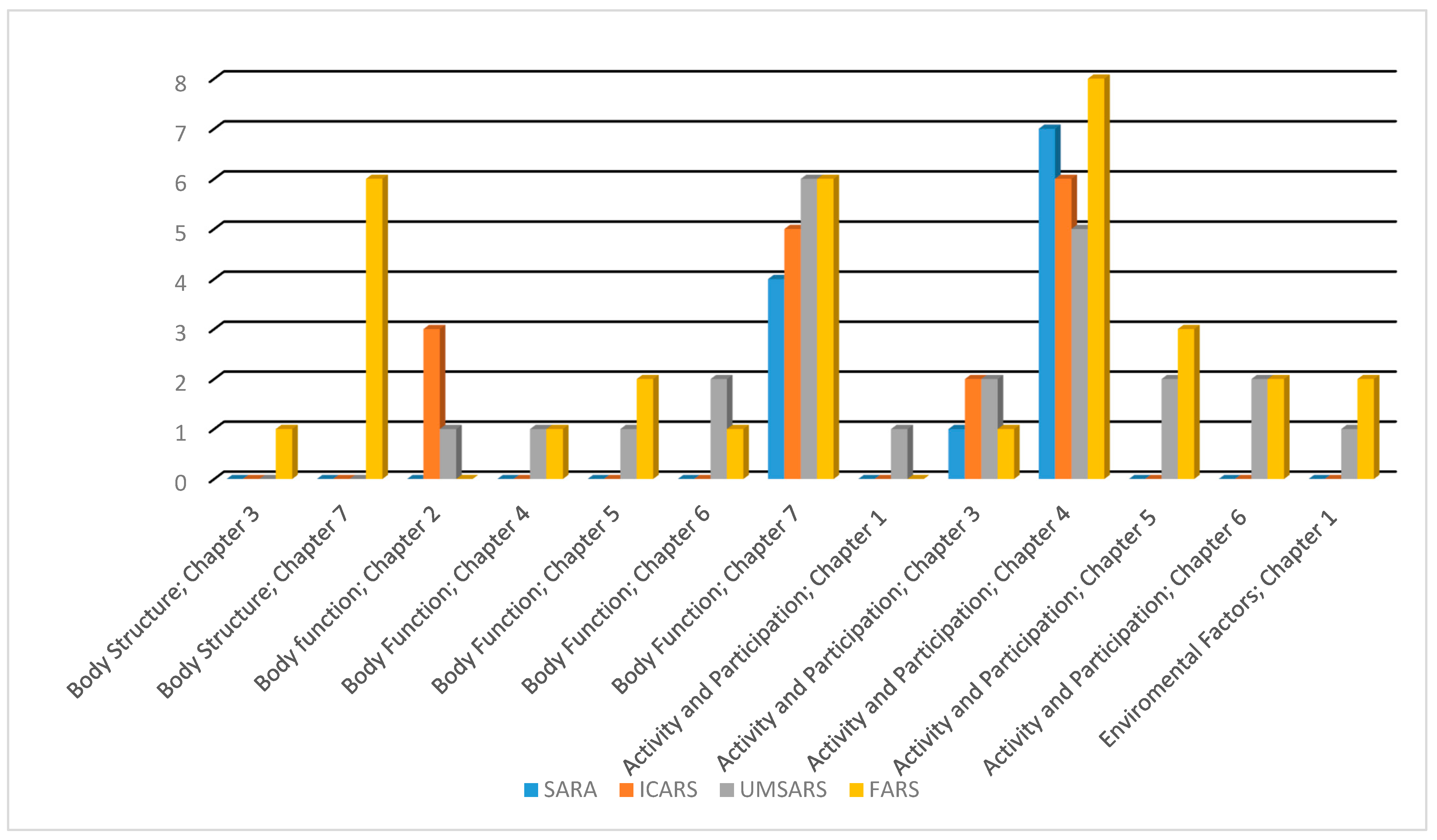
| Scale | SARA | ICARS | UMSARS | FARS |
|---|---|---|---|---|
| Numbers of items | 8 | 19 | 30 | 36 |
| Number of concepts (Different) | 14 (10) | 26 (15) | 39 (28) | 45 (34) |
| Concept not linked to ICF | 0 | 0 | 1 | 1 |
| Total ICF categories (Unique) | 15 (13) | 33 (16) | 40 (30) | 56 (39) |
| Body structure | 0 | 0 | 1 | 7 |
| Body function | 8 | 21 | 22 | 23 |
| Activity and participation | 7 | 12 | 16 | 22 |
| Environmental factors | 0 | 0 | 2 | 4 |
| ICF indicators: | ||||
| Measure to ICF linkage | 100% | 100% | 96.7% | 97.2% |
| Measure of linking to unique ICF codes | 6/8 (75%) | 9/19 (47.4%) | 23/30 (76.7%) | 24/36 (66.7%) |
| ICF Component | ICF Category | SARA | ICARS | UMSARS | FARS |
|---|---|---|---|---|---|
| Body structure | Chapter 3: Structures involved in voice and speech | ||||
| s 3203 Tongue | 0 | 0 | 0 | 1 | |
| Chapter 7: Structures related to movement | |||||
| s 7104 Muscles of head and neck region | 0 | 0 | 0 | 1 | |
| s 73002 Muscles of upper arm | 0 | 0 | 0 | 1 | |
| s 73012 Muscles of forearm | 0 | 0 | 0 | 1 | |
| s 73022 Muscles of hand | 0 | 0 | 0 | 1 | |
| s 75002 Muscles of thigh | 0 | 0 | 0 | 1 | |
| s 75012 Muscles of lower leg | 0 | 0 | 0 | 1 | |
| s 760 Structure of trunk | 0 | 0 | 1 | 0 | |
| Body Function | Chapter 2: Sensory functions and pain | ||||
| b 2152 Functions of external muscles of the eye | 0 | 3 | 1 | 0 | |
| Chapter 4: Functions of the cardiovascular, hematological, immunological and respiratory systems | |||||
| b 4201 Decreased blood pressure | 0 | 0 | 2 | 0 | |
| b 450 Additional respiratory functions | 0 | 0 | 0 | 1 | |
| Chapter 5: Functions of the digestive, metabolic and endocrine systems | |||||
| b 51050 Oral swallowing | 0 | 0 | 1 | 1 | |
| b 5253 Faecal continence | 0 | 0 | 0 | 1 | |
| Chapter 6: Genitourinary and reproductive functions | |||||
| b 6202 Urinary continence | 0 | 0 | 1 | 1 | |
| b 640 Sexual functions | 0 | 0 | 1 | 0 | |
| Chapter 7: Neuromusculoskeletal and movement-related functions | |||||
| b 7152 Stability of joints generalized | 0 | 0 | 1 | 0 | |
| b 7159 Stability of joint functions, unspecified | 0 | 0 | 1 | 1 | |
| b 7300 Power of isolated muscles and muscle groups | 0 | 0 | 0 | 3 | |
| b 7350 Tone of isolated muscles and muscle groups | 0 | 0 | 1 | 0 | |
| b 7500 Stretch motor reflex | 0 | 0 | 0 | 1 | |
| b 755 Involuntary movement reaction functions | 2 | 0 | 0 | 0 | |
| b 7600 Control of simple voluntary movements | 1 | 0 | 4 | 2 | |
| b 7602 Coordination of voluntary movements | 3 | 5 | 0 | 5 | |
| b 7650 Involuntary movement functions | 0 | 1 | 0 | 0 | |
| b 7651 Tremor | 1 | 5 | 2 | 0 | |
| b 770 Gait pattern functions | 0 | 1 | 1 | 1 | |
| Activity and participation | Chapter 1: Learning and applying knowledge | ||||
| d 170 Writing | 0 | 0 | 1 | 0 | |
| Chapter 3: Communication | |||||
| d 330 Speaking | 1 | 1 | 2 | 3 | |
| d 3350 Producing body language | 0 | 0 | 1 | 0 | |
| d 3352 Producing drawings and photographs | 0 | 1 | 0 | 0 | |
| Chapter 4: Mobility | |||||
| d 4103 Sitting | 1 | 0 | 1 | 0 | |
| d 4104 Standing | 1 | 1 | 1 | 0 | |
| d 4153 Maintaining a sitting position | 1 | 2 | 0 | 2 | |
| d 4154 Maintaining a standing position | 1 | 1 | 1 | 4 | |
| d 4301 Carrying in the hands | 0 | 0 | 0 | 1 | |
| d 4400 Picking up | 0 | 0 | 0 | 1 | |
| d 4403 Releasing | 0 | 0 | 0 | 1 | |
| d 4500 Walking short distances | 1 | 2 | 2 | 2 | |
| d 4509 Walking, unspecified | 1 | 2 | 0 | 2 | |
| d 465 Moving around using equipment | 1 | 1 | 2 | 1 | |
| Chapter 5: Self-care | |||||
| d 510 Washing oneself | 0 | 0 | 1 | 0 | |
| d 5400 Putting on clothes | 0 | 0 | 1 | 1 | |
| d 5402 Putting on footwear | 0 | 0 | 0 | 1 | |
| d 599 Self-care, unspecified | 0 | 0 | 0 | 1 | |
| Chapter 6: Domestic life | |||||
| d 6300 Preparing simple meals | 0 | 0 | 1 | 1 | |
| d 6600 Assisting others with self-care | 0 | 0 | 1 | 1 | |
| Environmental Factors | Chapter 1 Products and technology | ||||
| e 1151 Assistive products and technology for personal use in daily living | 0 | 0 | 1 | 1 | |
| e 1201 Assistive products and technology for personal indoor and outdoor mobility and transportation | 0 | 0 | 0 | 2 | |
| Chapter 3 Support and relationships | |||||
| e 340 Personal care providers and personal assistants | 0 | 0 | 1 | 1 | |
| Scale | SARA | ICARS | UMSARS | FARS | Overall |
|---|---|---|---|---|---|
| Meaningful concepts | 0.75 (0.486 to 1.000) | 0.668 (0.372 to 0.965) | 0.732 (0.511 to 0.952) | 0.835 (0.655 to 1.000) | 0.762 (0.622 to 0.903) |
| ICF Component | 1 | 0.878 (0.713 to 1) | 0.781 (0.578 to 0.985) | 0.842 (0.669 to 1) | 0.843 (0.749 to 0.937) |
| First/chapter level | 0.732(0.387 to 1) | 0.824 (0.632 to 1) | 0.733 (0.514 to 0.953) | 0.796 (0.605 to 0.988) | 0.747 (0.625 to 0.868) |
| Second Level | 0.714 (0.348 to 1) | 0.721 (0.493 to 0.949) | 0.689 (0.459 to 0.918) | 0.714 (0.499 to 0.929) | 0.705 (0.577 to 0.832) |
| Third Level | 0.717 (0.462 to 0.972) | 0.666 (0.421 to 0.911) | 0.645 (0.405 to 0.885) | 0.675 (0.453 to 0.898) | 0.644 (0.504 to 0.783) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Etoom, M.; Jahan, A.M.; Alghwiri, A.; Lena, F.; Modugno, N. Ataxia Rating Scales: Content Analysis by Linking to the International Classification of Functioning, Disability and Health. Healthcare 2022, 10, 2459. https://doi.org/10.3390/healthcare10122459
Etoom M, Jahan AM, Alghwiri A, Lena F, Modugno N. Ataxia Rating Scales: Content Analysis by Linking to the International Classification of Functioning, Disability and Health. Healthcare. 2022; 10(12):2459. https://doi.org/10.3390/healthcare10122459
Chicago/Turabian StyleEtoom, Mohammad, Alhadi M. Jahan, Alia Alghwiri, Francesco Lena, and Nicola Modugno. 2022. "Ataxia Rating Scales: Content Analysis by Linking to the International Classification of Functioning, Disability and Health" Healthcare 10, no. 12: 2459. https://doi.org/10.3390/healthcare10122459
APA StyleEtoom, M., Jahan, A. M., Alghwiri, A., Lena, F., & Modugno, N. (2022). Ataxia Rating Scales: Content Analysis by Linking to the International Classification of Functioning, Disability and Health. Healthcare, 10(12), 2459. https://doi.org/10.3390/healthcare10122459








