Topics Mentioned by Stroke Patients during Supportive Phone Calls—Implications for Individualized Aftercare Programs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Extraction and Processing
2.3. Statistical Analyses
3. Results
3.1. Patients’ Characteristics and Frequency of Topics Mentioned after Hospital Stay
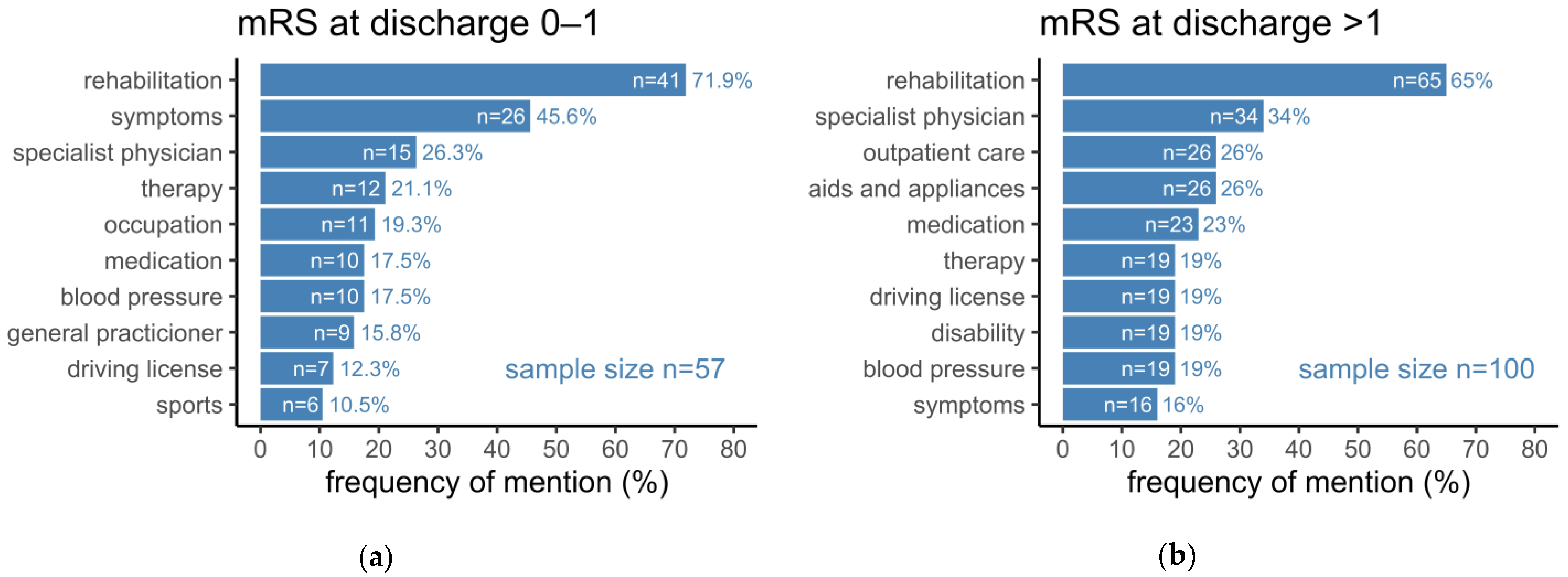
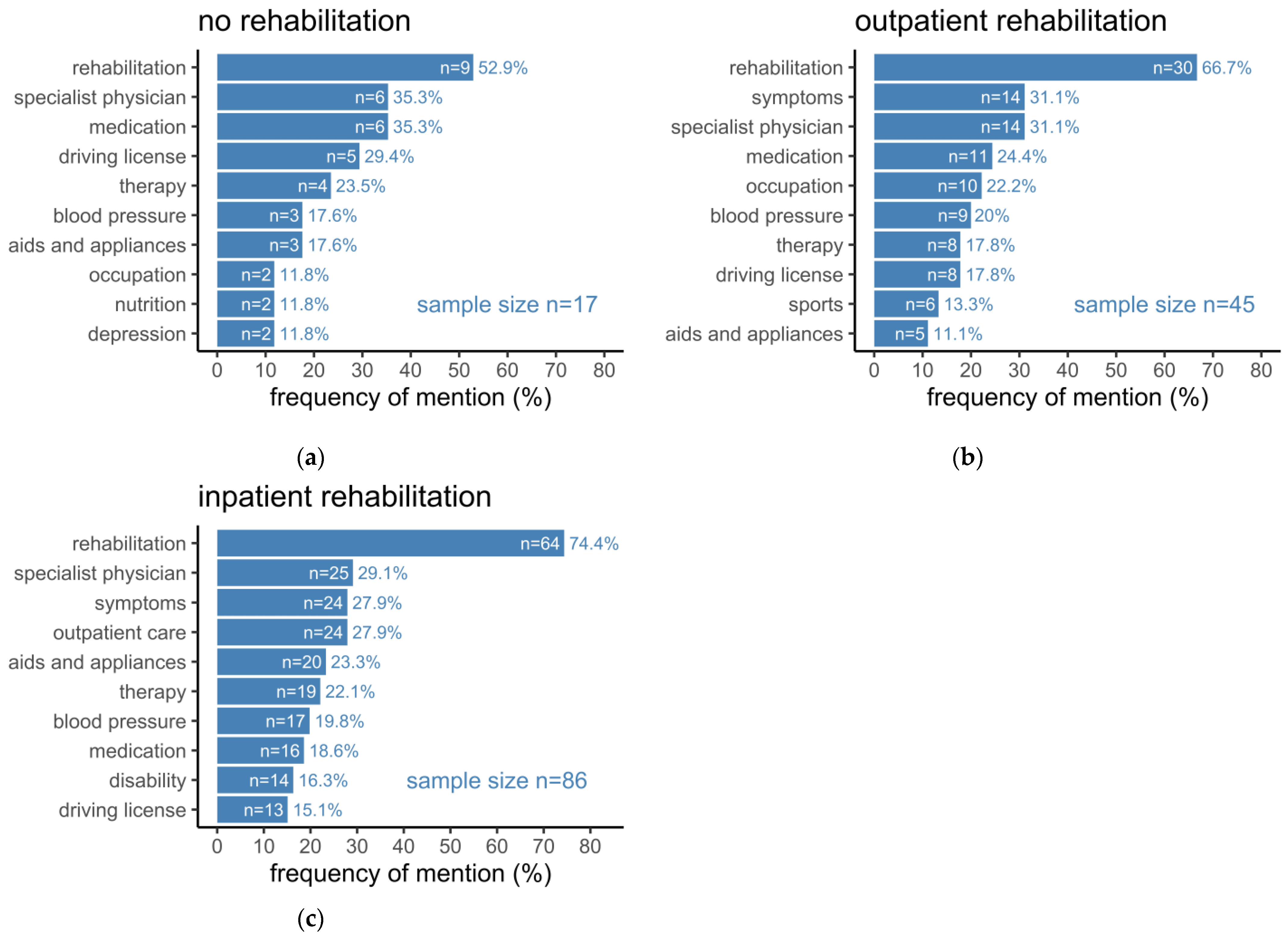
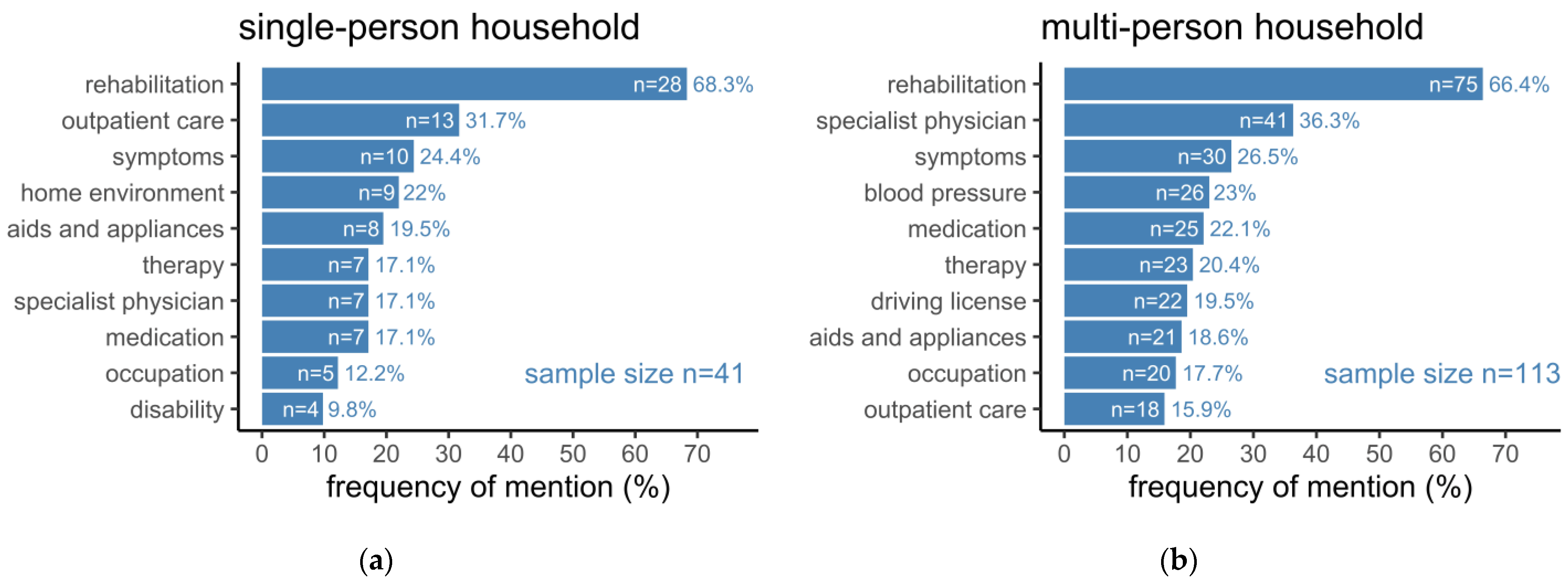
3.2. Frequency of Mentioned Topics Depending on Disability and Social Environment
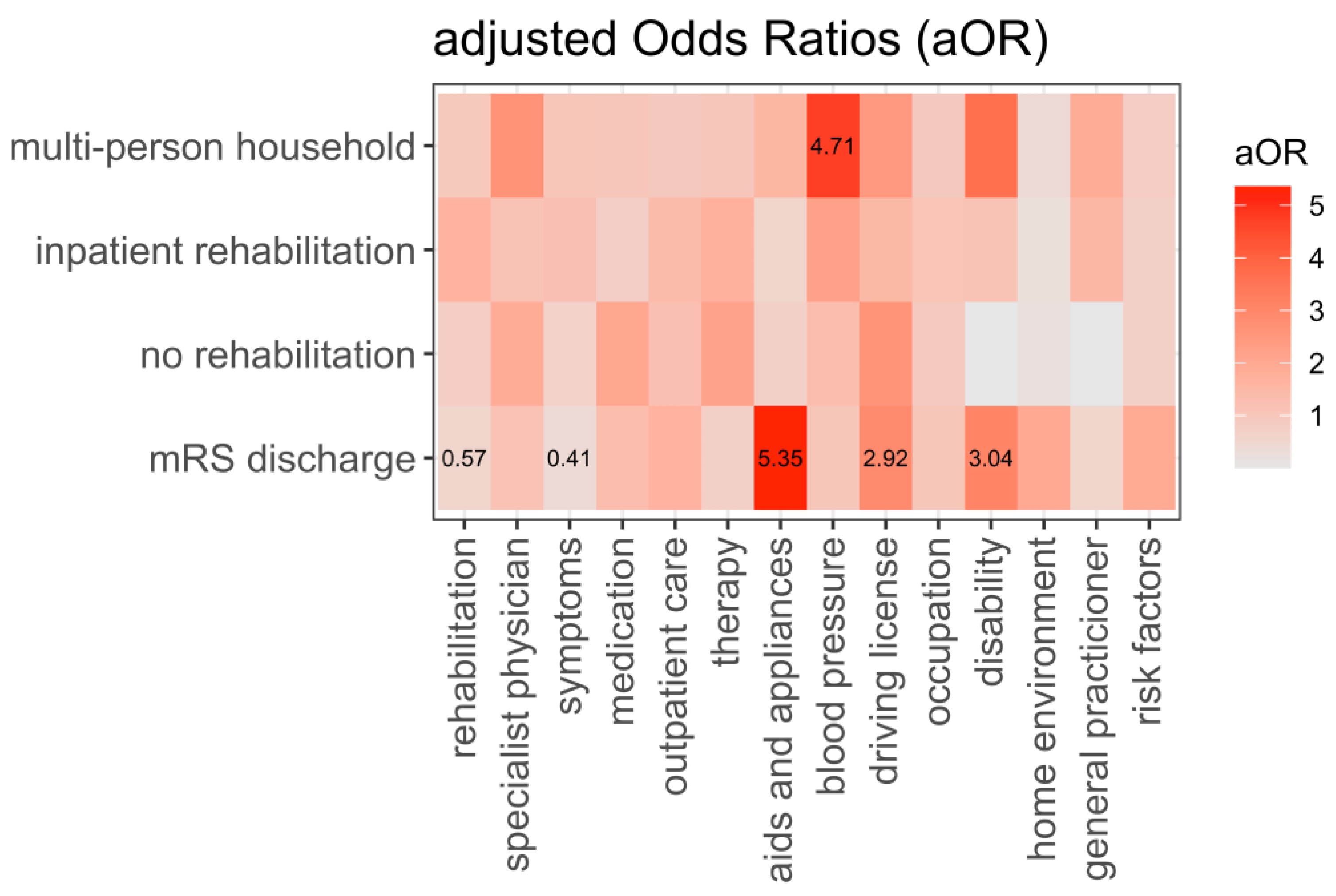
3.3. Probability for Mentioning Topics in Stroke Aftercare Depending on Patients’ Characteristics and Social Environment
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hankey, G.J. Stroke. Lancet 2017, 389, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef]
- Heuschmann, P.; Busse, O.; Wagner, M.; Endres, M.; Villringer, A.; Röther, J.; Kolominsky-Rabas, P.; Berger, K. Schlaganfallhäufigkeit und Versorgung von Schlaganfallpatienten in Deutschland. Aktuelle Neurol. 2010, 37, 333–340. [Google Scholar] [CrossRef]
- Owolabi, M.O.; Thrift, A.G.; Mahal, A.; Ishida, M.; Martins, S.; Johnson, W.D.; Pandian, J.; Abd-Allah, F.; Yaria, J.; Phan, H.T.; et al. Stroke Experts Collaboration Group. Primary stroke prevention worldwide: Translating evidence into action. Lancet Public Health 2022, 7, e74–e85. [Google Scholar] [CrossRef]
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Stroke Unit Trialists’ Collaboration. Organised Inpatient (Stroke Unit) Care for Stroke. Cochrane Database Syst. Rev. 2013, CD000197. [Google Scholar] [CrossRef]
- Hacke, W.; Kaste, M.; Bluhmki, E.; Brozman, M.; Dávalos, A.; Guidetti, D.; Larrue, V.; Lees, K.R.; Medeghri, Z.; Machnig, T.; et al. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. N. Engl. J. Med. 2008, 359, 1317–1329. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Menon, B.K.; van Zwam, W.H.; Dippel, D.W.J.; Mitchell, P.J.; Demchuk, A.M.; Dávalos, A.; Majoie, C.B.L.M.; van der Lugt, A.; de Miquel, M.A.; et al. Endovascular Thrombectomy after Large-Vessel Ischaemic Stroke: A Meta-Analysis of Individual Patient Data from Five Randomised Trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef]
- Leys, D.; Ringelstein, E.B.; Kaste, M.; Hacke, W. The Main Components of Stroke Unit Care: Results of a European Expert Survey. Cerebrovasc. Dis. 2007, 23, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Seminog, O.O.; Scarborough, P.; Wright, F.L.; Rayner, M.; Goldacre, M.J. Determinants of the Decline in Mortality from Acute Stroke in England: Linked National Database Study of 795 869 Adults. BMJ 2019, 365, l1778. [Google Scholar] [CrossRef]
- The GBD 2016 Lifetime Risk of Stroke Collaborators. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [CrossRef]
- Flach, C.; Muruet, W.; Wolfe, C.D.A.; Bhalla, A.; Douiri, A. Risk and Secondary Prevention of Stroke Recurrence: A Population-Base Cohort Study. Stroke 2020, 51, 2435–2444. [Google Scholar] [CrossRef]
- van den Bussche, H.; Berger, K.; Kemper, C.; Barzel, A.; Glaeske, G.; Koller, D. Inzidenz, Rezidiv, Pflegebedürftigkeit und Mortalität von Schlaganfall. Aktuelle Neurol. 2010, 37, 131–135. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Paul, N.L.M.; Gray, A.M.; Pendlebury, S.T.; Bull, L.M.; Welch, S.J.V.; Cuthbertson, F.C.; Rothwell, P.M. Population-Based Study of Disability and Institutionalization After Transient Ischemic Attack and Stroke: 10-Year Results of the Oxford Vascular Study. Stroke 2013, 44, 2854–2861. [Google Scholar] [CrossRef] [PubMed]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef]
- Diener, H.-C.; Hankey, G.J. Primary and Secondary Prevention of Ischemic Stroke and Cerebral Hemorrhage. J. Am. Coll. Cardiol. 2020, 75, 1804–1818. [Google Scholar] [CrossRef] [PubMed]
- Kalra, L.; Eade, J. Role of Stroke Rehabilitation Units in Managing Severe Disability After Stroke. Stroke 1995, 26, 2031–2034. [Google Scholar] [CrossRef]
- Ayerbe, L.; Ayis, S.; Wolfe, C.D.A.; Rudd, A.G. Natural History, Predictors and Outcomes of Depression after Stroke: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2013, 202, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Xiao, L.D.; Chamberlain, D.; Newman, P. Enablers and Barriers in Hospital-to-home Transitional Care for Stroke Survivors and Caregivers: A Systematic Review. J. Clin. Nurs. 2021, 30, 2786–2807. [Google Scholar] [CrossRef]
- Hempler, I.; Maun, A.; Kampling, H.; Thielhorn, U.; Farin, E. Poststroke care in Germany: Results of an online survey of inpatient and outpatient experts in southern Germany. Nervenarzt 2019, 90, 824–831. [Google Scholar] [CrossRef]
- Kjörk, E.K.; Gunnel, C.; Lundgren-Nilsson, Å.; Sunnerhagen, K.S. Experiences, Needs, and Preferences for Follow-up after Stroke Perceived by People with Stroke and Healthcare Professionals: A Focus Group Study. PLoS ONE 2019, 14, e0223338. [Google Scholar] [CrossRef] [PubMed]
- Teipen, V.; Bode, S. Handbuch Schlaganfall-Lotsen: Leitfaden für Die Einführung von Schlaganfall-Lotsen auf Basis des STROKE OWL-Projekts; Case Management in der Praxis; Brinkmeier, M., Galle, G., Eds.; Medhochzwei: Heidelberg, Germany, 2021; ISBN 978-3-86216-881-1. [Google Scholar]
- Ahmadi, M.; Laumeier, I.; Ihl, T.; Steinicke, M.; Ferse, C.; Endres, M.; Grau, A.; Hastrup, S.; Poppert, H.; Palm, F.; et al. A Support Programme for Secondary Prevention in Patients with Transient Ischaemic Attack and Minor Stroke (INSPiRE-TMS): An Open-Label, Randomised Controlled Trial. Lancet Neurol. 2020, 19, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Willeit, P.; Toell, T.; Boehme, C.; Krebs, S.; Mayer, L.; Lang, C.; Seekircher, L.; Tschiderer, L.; Willeit, K.; Rumpold, G.; et al. STROKE-CARD study group. STROKE-CARD care to prevent cardiovascular events and improve quality of life after acute ischaemic stroke or TIA: A randomised clinical trial. eClinicalMedicine 2020, 25, 100476. [Google Scholar] [CrossRef] [PubMed]
- Norrving, B.; Barrick, J.; Davalos, A.; Dichgans, M.; Cordonnier, C.; Guekht, A.; Kutluk, K.; Mikulik, R.; Wardlaw, J.; Richard, E.; et al. Action Plan for Stroke in Europe 2018–2030. Eur. Stroke J. 2018, 3, 309–336. [Google Scholar] [CrossRef]
- Ihl, T.; Ahmadi, M.; Laumeier, I.; Steinicke, M.; Ferse, C.; Klyscz, P.; Endres, M.; Hastrup, S.; Poppert, H.; Palm, F.; et al. Patient-Centered Outcomes in a Randomized Trial Investigating a Multimodal Prevention Program After Transient Ischemic Attack or Minor Stroke: The INSPiRE-TMS Trial. Stroke 2022, 53, 2730–2738. [Google Scholar] [CrossRef]
- Rimmele, D.L.; Schrage, T.; Lebherz, L.; Kriston, L.; Gerloff, C.; Härter, M.; Thomalla, G. Profiles of Patients’ Self-Reported Health after Acute Stroke. Neurol. Res. Pract. 2021, 3, 43. [Google Scholar] [CrossRef]
- NINDS Know Stroke Campaign—NIH Stroke Scale. Available online: https://www.stroke.nih.gov/resources/scale.htm (accessed on 14 October 2022).
- Van Swieten, J.C.; Koudstaal, P.J.; Visser, M.C.; Schouten, H.J.; van Gijn, J. Interobserver Agreement for the Assessment of Handicap in Stroke Patients. Stroke 1988, 19, 604–607. [Google Scholar] [CrossRef] [PubMed]
- R Core Team R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022.
- R Studio Team RStudio: Integrated Development Environment for R; RStudio, PBC: Boston, MA, USA, 2022.
- Deen, T.; Terna, T.; Kim, E.; Leahy, B.; Fedder, W. The Impact of Stroke Nurse Navigation on Patient Compliance Postdischarge. Rehabil. Nurs. 2018, 2, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Verberne, D.P.J.; Kroese, M.E.A.L.; Staals, J.; Ponds, R.W.H.M.; van Heugten, C.M. Nurse-Led Stroke Aftercare Addressing Long-Term Psychosocial Outcome: A Comparison to Care-as-Usual. Disabil. Rehabil. 2022, 44, 2849–2857. [Google Scholar] [CrossRef] [PubMed]
- Lynch, E.A.; Cadilhac, D.A.; Luker, J.A.; Hillier, S.L. Inequities in access to inpatient rehabilitation after stroke: An international scoping review. Top Stroke Rehabil. 2017, 24, 619–626. [Google Scholar] [CrossRef]
- Cameron, J.; Lannin, N.A.; Harris, D.; Andrew, N.E.; Kilkenny, M.F.; Purvis, T.; Thrift, A.G.; Thayabaranathan, T.; Ellery, F.; Sookram, G.; et al. Recovery-focused Community support to Avoid readmissions and improve Participation after Stroke (ReCAPS) Investigators. A mixed-methods feasibility study of a new digital health support package for people after stroke: The Recovery-focused Community support to Avoid readmissions and improve Participation after Stroke (ReCAPS) intervention. Pilot Feasibility Stud. 2022, 8, 241. [Google Scholar] [CrossRef] [PubMed]
- Freed, C.R.; Hansberry, S.T.; Arrieta, M.I. Structural and hidden barriers to a local primary health care infrastructure: Autonomy, decisions about primary health care and the centrality and significance of power. Res. Sociol. Health Care 2013, 31, 57–81. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Nguyen, T.; Hahn-Goldberg, S.; Lewis-Fung, S.; Smith-Bayley, S.; Nelson, M.L.A. A qualitative study exploring the experiences of individuals living with stroke and their caregivers with community-based poststroke services: A critical need for action. PLoS ONE 2022, 17, e0275673. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Gong, Y.; Zhao, Y.; Jiang, N.; Wang, J.; Yin, X. Post-stroke medication adherence and persistence rates: A meta-analysis of observational studies. J. Neurol. 2021, 268, 2090–2098. [Google Scholar] [CrossRef]
- Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Forbes, S.; Anderson, C.S. Long-Term Disability after First-Ever Stroke and Related Prognostic Factors in the Perth Community Stroke Study, 1989–1990. Stroke 2002, 33, 1034–1040. [Google Scholar] [CrossRef]
- Seidel, G.; Röttinger, A.; Lorenzen, J.; Kücken, D.; Majewski, A.; Klose, K.; Terborg, C.; Klass, I.; Wohlmuth, P.; Zukunft, E.; et al. Quality of life and disability after severe stroke and early neurological rehabilitation. Nervenarzt 2019, 90, 1031–1036. [Google Scholar] [CrossRef]
- Broomfield, N.M.; Quinn, T.J.; Abdul-Rahim, A.H.; Walters, M.R.; Evans, J.J. Depression and anxiety symptoms post-stroke/TIA: Prevalence and associations in cross-sectional data from a regional stroke registry. BMC Neurol. 2014, 14, 198. [Google Scholar] [CrossRef]
- Bushnell, C.D.; Chaturvedi, S.; Gage, K.R.; Herson, P.S.; Hurn, P.D.; Jiménez, M.C.; Kittner, S.J.; Madsen, T.E.; McCullough, L.D.; McDermott, M.; et al. Sex Differences in Stroke: Challenges and Opportunities. J. Cereb. Blood Flow Metab. 2018, 38, 2179–2191. [Google Scholar] [CrossRef]
- Lin, S.; Wang, C.; Wang, Q.; Xie, S.; Tu, Q.; Zhang, H.; Peng, M.; Zhou, J.; Redfern, J. The Experience of Stroke Survivors and Caregivers during Hospital-to-Home Transitional Care: A Qualitative Longitudinal Study. Int. J. Nurs. Stud. 2022, 130, 104213. [Google Scholar] [CrossRef]
- Nursiswati, N.; Halfens, R.J.G.; Lohrmann, C. Care Dependency of Hospitalized Stroke Patients Based on Family Caregivers’ and Nurses’ Assessments: A Comparative Study. Healthcare 2022, 10, 1007. [Google Scholar] [CrossRef]

| Characteristic | M ± SD or n (%) |
|---|---|
| Age (years) | 69.32 ± 13.21 |
| Sex (female) | 57 (36.31%) |
| BMI | 27.45 (4.97%) |
| Diagnosis | |
| TIA | 3 (1.91%) |
| Ischemic stroke | 154 (98.09%) |
| Cardiovascular risk factors per patient | 3.74 ± 1.73 |
| Recanalization strategy | |
| None | 115 (73.25%) |
| Intravenous thrombolysis | 34 (21.66%) |
| Endovascular procedure | 24 (15.29%) |
| Patients with first stroke | 129 (82.69%) |
| Secondary diagnoses per patient | 6.16 ± 3.23 |
| pre-mRS | |
| total | 0.29 ± 0.68 |
| 0 | 127 (80.89%) |
| 1 | 18 (11.46%) |
| ≥2 | 12 (7.64%) |
| NIHSS at hospital admission | |
| total | 4.09 ± 4.32 |
| 0 | 25 (15.92%) |
| 1–3 | 67 (42.68%) |
| 4–8 | 43 (27.39%) |
| ≥9 | 22 (14.01%) |
| Days in hospital | 8.82 ± 5.14 |
| mRS at hospital discharge | |
| total | 1.77 ± 1.10 |
| 0 | 23 (14.65%) |
| 1 | 34 (21.66%) |
| 2 | 66 (42.04%) |
| ≥3 | 34 (21.66%) |
| NIHSS at hospital discharge | |
| total | 1.69 ± 2.27 |
| 0 | 55 (35.03%) |
| 1 | 43 (27.39%) |
| 2–3 | 42 (26.75%) |
| ≥4 | 17 (10.83%) |
| Medications 1 at hospital discharge | 6.64 ± 2.89 |
| Type of rehabilitation 2 | |
| none | 17 (11.49%) |
| outpatient | 45 (30.41%) |
| inpatient | 86 (58.11%) |
| Patients in single-person households 2 | 41 (26.62%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmidt, R.; Geisler, D.; Urban, D.; Wagner, M.; Ivanova, G.; Neumuth, T.; Classen, J.; Michalski, D. Topics Mentioned by Stroke Patients during Supportive Phone Calls—Implications for Individualized Aftercare Programs. Healthcare 2022, 10, 2394. https://doi.org/10.3390/healthcare10122394
Schmidt R, Geisler D, Urban D, Wagner M, Ivanova G, Neumuth T, Classen J, Michalski D. Topics Mentioned by Stroke Patients during Supportive Phone Calls—Implications for Individualized Aftercare Programs. Healthcare. 2022; 10(12):2394. https://doi.org/10.3390/healthcare10122394
Chicago/Turabian StyleSchmidt, Richard, Daniela Geisler, Daniela Urban, Markus Wagner, Galina Ivanova, Thomas Neumuth, Joseph Classen, and Dominik Michalski. 2022. "Topics Mentioned by Stroke Patients during Supportive Phone Calls—Implications for Individualized Aftercare Programs" Healthcare 10, no. 12: 2394. https://doi.org/10.3390/healthcare10122394
APA StyleSchmidt, R., Geisler, D., Urban, D., Wagner, M., Ivanova, G., Neumuth, T., Classen, J., & Michalski, D. (2022). Topics Mentioned by Stroke Patients during Supportive Phone Calls—Implications for Individualized Aftercare Programs. Healthcare, 10(12), 2394. https://doi.org/10.3390/healthcare10122394






