The Health Belief Model Modifying Factors Associated with Missed Clinic Appointments among Individuals with Sickle Cell Disease in the Jazan Province, Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area and Design
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection
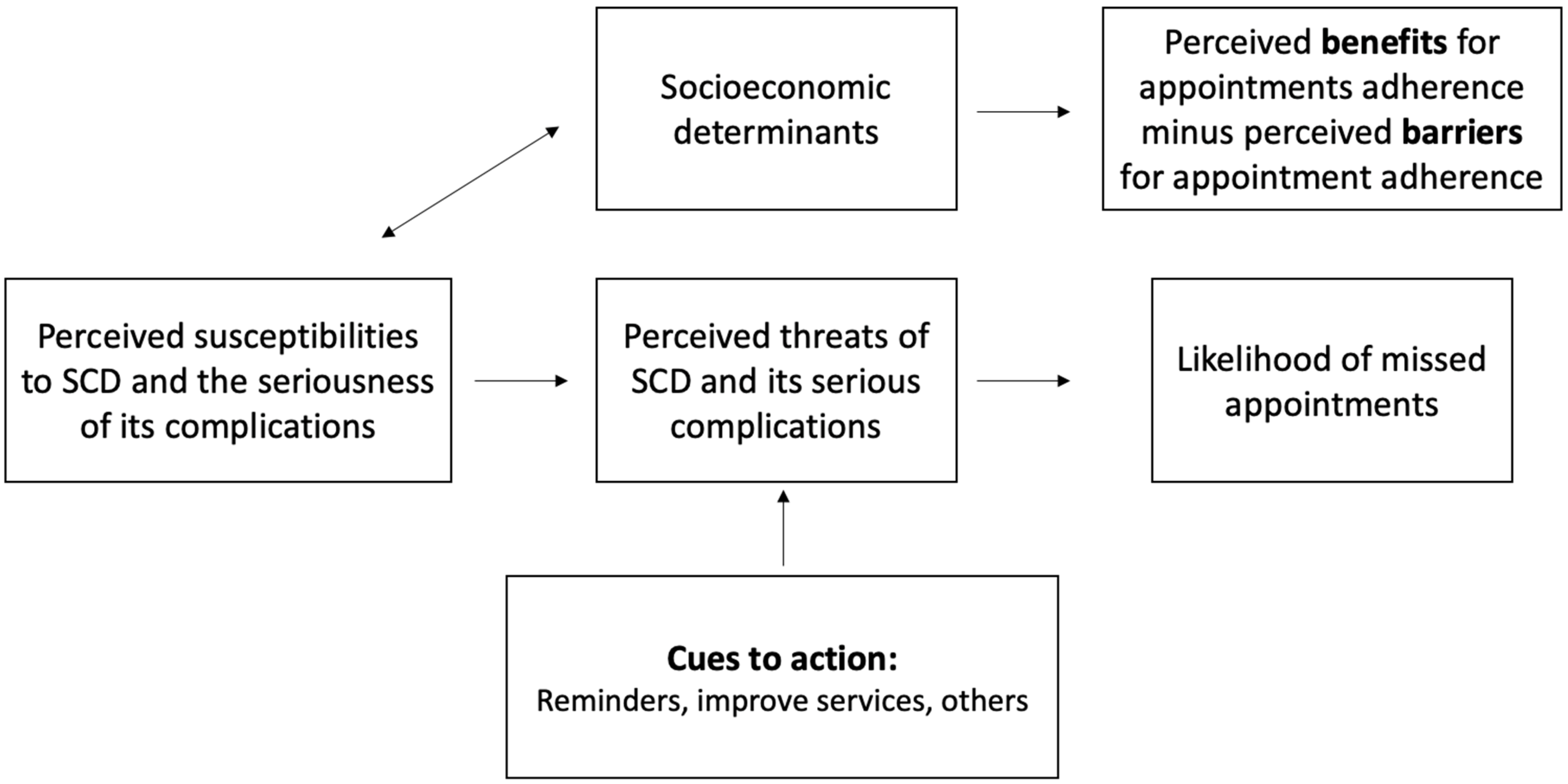
2.4. Study Measures
2.5. Pilot Study
2.6. Sampling Size and Statistical Analysis
2.7. Ethical Consideration
3. Results
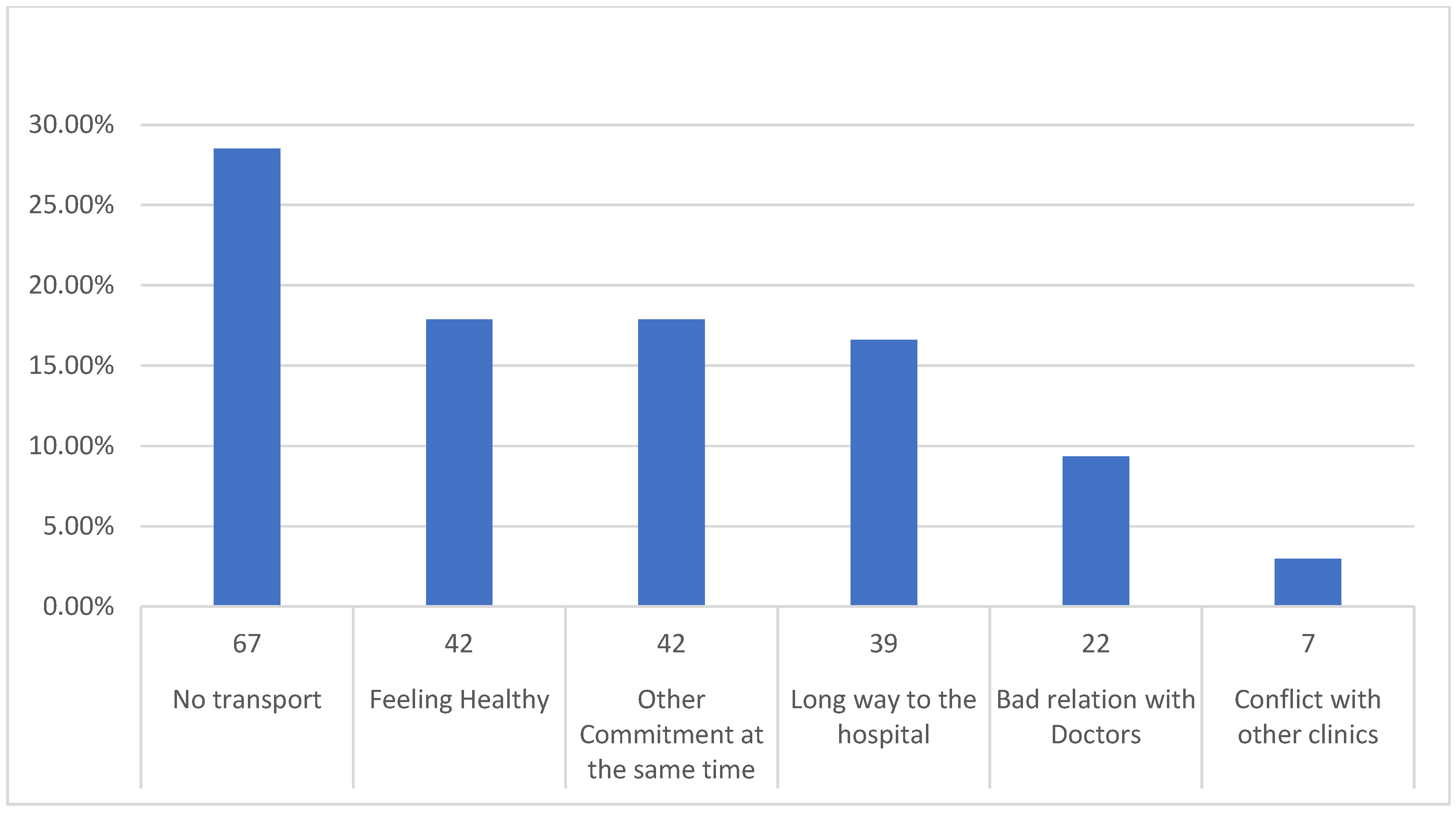
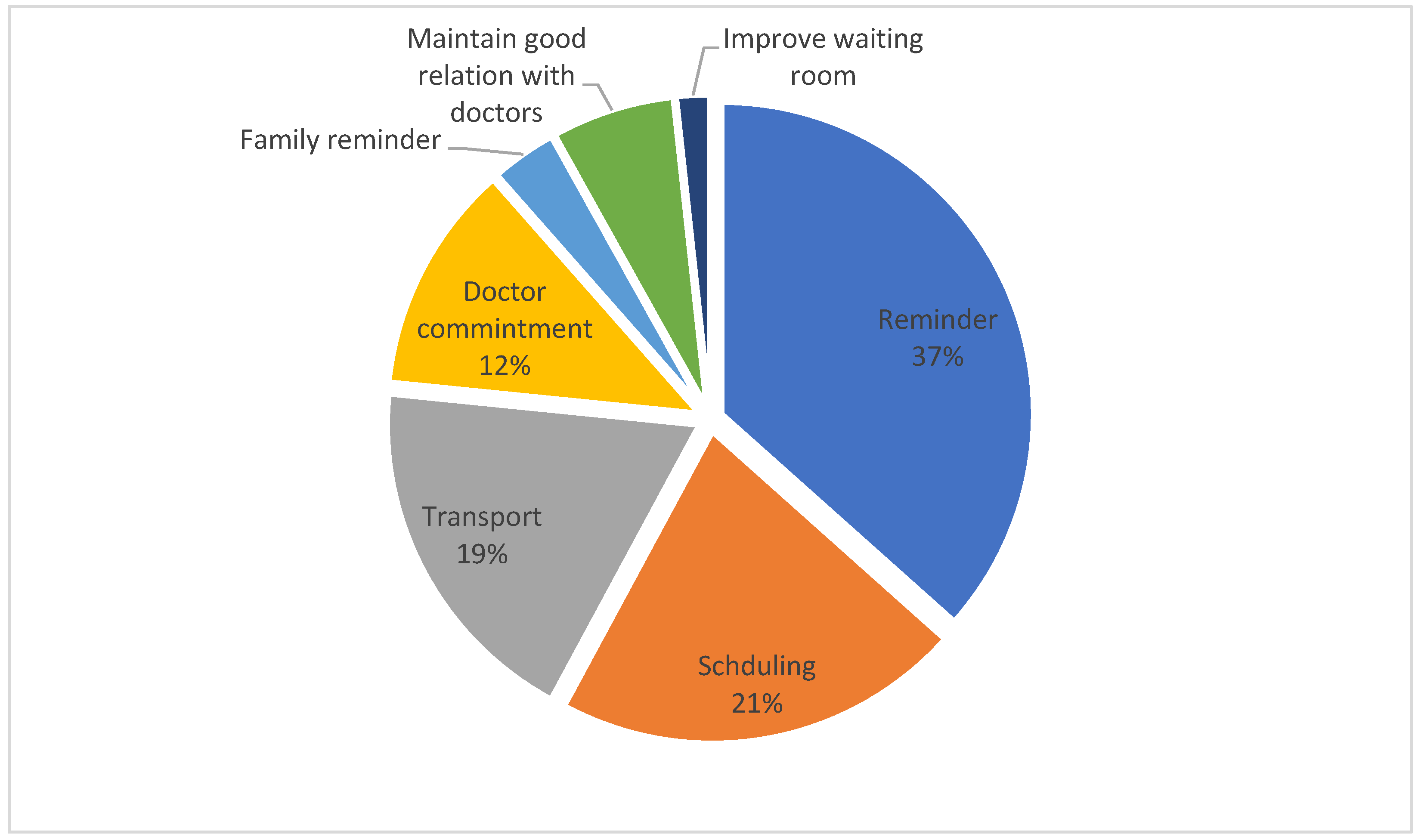
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hazzazi, A.; Ageeli, M.; Alfaqih, A.; Jaafari, A.; Malhan, H.; Bakkar, M. Epidemiology and Characteristics of Sickle Cell Patients Admitted to Hospitals in Jazan Region, Saudi Arabia. J. Appl. Hematol. 2020, 11, 10. [Google Scholar] [CrossRef]
- Serjeant, G.R. The Natural History of Sickle Cell Disease. Cold Spring Harb. Perspect. Med. 2013, 3, a011783. [Google Scholar] [CrossRef] [PubMed]
- Crosby, L.E.; Modi, A.C.; Lemanek, K.L.; Guilfoyle, S.M.; Kalinyak, K.A.; Mitchell, M.J. Perceived Barriers to Clinic Appointments for Adolescents with Sickle Cell Disease. J. Pediatr. Hematol. Oncol. 2009, 31, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Ohnso, P.L.; Lombardo, F.A.; Moore, C.D. Options in the Management of Sickle Cell Disease. US Pharm. 2015, 40, 4–7. [Google Scholar]
- Wong, W.Y. Prevention and Management of Infection in Children with Sickle Cell Anaemia. Paediatr. Drugs 2001, 3, 793–801. [Google Scholar] [CrossRef]
- Dunbar-Jacob, J.; Mortimer-Stephens, M.K. Treatment Adherence in Chronic Disease. J. Clin. Epidemiol. 2001, 54 (Suppl. 1), S57–S60. [Google Scholar] [CrossRef]
- Nelson, E.A.; Maruish, M.E.; Axler, J.L. Effects of Discharge Planning and Compliance with Outpatient Appointments on Readmission Rates. Psychiatr. Serv. 2000, 51, 885–889. [Google Scholar] [CrossRef]
- Schectman, J.M.; Schorling, J.B.; Voss, J.D. Appointment Adherence and Disparities in Outcomes among Patients with Diabetes. J. Gen. Intern. Med. 2008, 23, 1685–1687. [Google Scholar] [CrossRef]
- Cronin, R.M.; Hankins, J.S.; Byrd, J.; Pernell, B.M.; Kassim, A.; Adams-Graves, P.; Thompson, A.A.; Kalinyak, K.; DeBaun, M.R.; Treadwell, M. Modifying Factors of the Health Belief Model Associated with Missed Clinic Appointments among Individuals with Sickle Cell Disease. Hematology 2018, 23, 683–691. [Google Scholar] [CrossRef]
- Haywood, C., Jr.; Lanzkron, S.; Bediako, S.; Strouse, J.J.; Haythornthwaite, J.; Carroll, C.P.; Diener-West, M.; Onojobi, G.; Beach, M.C. IMPORT Investigators Perceived Discrimination, Patient Trust, and Adherence to Medical Recommendations among Persons with Sickle Cell Disease. J. Gen. Intern. Med. 2014, 29, 1657–1662. [Google Scholar] [CrossRef]
- Population in Jazan Region by Gender, Age Group, and Nationality (Saudi/Non-Saudi). Available online: https://www.stats.gov.sa/en/6140 (accessed on 23 October 2022).
- Alotaibi, M.M. Sickle Cell Disease in Saudi Arabia: A Challenge or Not. J. Epidemiol. Glob. Health 2017, 7, 99. [Google Scholar] [CrossRef]
- Alhazmi, A.; Hakami, K.; Abusageah, F.; Jaawna, E.; Khawaji, M.; Alhazmi, E.; Zogel, B.; Qahl, S.; Qumayri, G. The Impact of Sickle Cell Disease on Academic Performance among Affected Students. Children 2021, 9, 15. [Google Scholar] [CrossRef]
- Ismail, A.F.; Tarawah, R.A.; Azzouni, Z.Y.; Alharbi, L.T.; Altayyar, R.M. The Relation between Regular Outpatient Follow-up and Frequency of Emergency Department Visits in Sickle Cell Pediatric Patients. Saudi Med. J. 2020, 41, 1324–1329. [Google Scholar] [CrossRef]
- Khan, S.A.; AlSiny, F.; Makki, A.; Ali, A.; AlAnsari, I.; Khan, S. Socioeconomic Status Dependent Medical Complexities in Children with Sickle Cell Disease in Saudi Arabia. Saudi J. Biol. Sci. 2020, 27, 1781–1787. [Google Scholar] [CrossRef]
- Farber, M.D.; Koshy, M.; Kinney, T.R. Cooperative Study of Sickle Cell Disease: Demographic and Socioeconomic Characteristics of Patients and Families with Sickle Cell Disease. J. Chronic Dis. 1985, 38, 495–505. [Google Scholar] [CrossRef]
- Osunkwo, I.; Andemariam, B.; Minniti, C.P.; Inusa, B.P.D.; El Rassi, F.; Francis-Gibson, B.; Nero, A.; Trimnell, C.; Abboud, M.R.; Arlet, J.-B.; et al. Impact of Sickle Cell Disease on Patients’ Daily Lives, Symptoms Reported, and Disease Management Strategies: Results from the International Sickle Cell World Assessment Survey (SWAY). Am. J. Hematol. 2021, 96, 404–417. [Google Scholar] [CrossRef]
- Crosby, L.E.; Quinn, C.T.; Kalinyak, K.A. A Biopsychosocial Model for the Management of Patients with Sickle-Cell Disease Transitioning to Adult Medical Care. Adv. Ther. 2015, 32, 293–305. [Google Scholar] [CrossRef]
- Weiss, S.; Yang, S.; Zhang, S.; David, M.; Lanzkron, S.M.; Eakin, M. The Telemedicine Experience for Individuals with Sickle Cell Disease. Blood 2021, 138, 1893. [Google Scholar] [CrossRef]
- Kheirkhah, P.; Feng, Q.; Travis, L.M.; Tavakoli-Tabasi, S.; Sharafkhaneh, A. Prevalence, Predictors and Economic Consequences of No-Shows. BMC Health Serv. Res. 2016, 16, 13. [Google Scholar] [CrossRef]
- Davies, M.L.; Goffman, R.M.; May, J.H.; Monte, R.J.; Rodriguez, K.L.; Tjader, Y.C.; Vargas, D.L. Large-Scale No-Show Patterns and Distributions for Clinic Operational Research. Healthcare 2016, 4, 15. [Google Scholar] [CrossRef]
- Robotham, D.; Satkunanathan, S.; Reynolds, J.; Stahl, D.; Wykes, T. Using Digital Notifications to Improve Attendance in Clinic: Systematic Review and Meta-Analysis. BMJ Open 2016, 6, e012116. [Google Scholar] [CrossRef] [PubMed]
- Sanger, M.; Jordan, L.; Pruthi, S.; Day, M.; Covert, B.; Merriweather, B.; Rodeghier, M.; DeBaun, M.; Kassim, A. Cognitive Deficits Are Associated with Unemployment in Adults with Sickle Cell Anemia. J. Clin. Exp. Neuropsychol. 2016, 38, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Edwards, C.L.; Green, M.; Wellington, C.C.; Muhammad, M.; Wood, M.; Feliu, M.; Edwards, L.; Hill, L.; Sollers, J.J., 3rd; Barksdale, C.; et al. Depression, Suicidal Ideation, and Attempts in Black Patients with Sickle Cell Disease. J. Natl. Med. Assoc. 2009, 101, 1090–1095. [Google Scholar] [CrossRef] [PubMed]
- Alhazmi, A.; Moafa, W.; Madkhali, J.; Saifain, O.; Alyahyawi, F.; Adhabi, O.; Alharbi, A. Coronavirus Disease 2019 in Patients with Sickle Cell Disease: A Cross-Sectional Study from Jazan Province, Saudi Arabia. J. Nat. Sci. Med. 2022, 5, 199. [Google Scholar] [CrossRef]
- Jain, A.; Patel, A.; Oyoyo, U.; Wiafe, S. Impact of COVID 19 Pandemic on Health Care Utilization for Patients with Sickle Cell Disease-a Specialty Treatment Center Experience. Blood 2021, 138, 4955. [Google Scholar] [CrossRef]
- McCloskey, K.A.; Meenan, J.; Hall, R.; Tsitsikas, D.A. COVID-19 Infection and Sickle Cell Disease: A UK Centre Experience. Br. J. Haematol. 2020, 190, e57–e58. [Google Scholar] [CrossRef]
| Variables | N | % | |
|---|---|---|---|
| Age | Less than one year | 4 | 1.0% |
| 1 to 10 | 62 | 16.3% | |
| 11 to 20 | 82 | 21.5% | |
| 21 to 30 | 155 | 40.7% | |
| 31 to 40 | 55 | 14.4% | |
| More than 40 | 23 | 6.0% | |
| Sex | Female | 226 | 59.3% |
| Male | 155 | 40.7% | |
| Marital Status | Single | 258 | 67.7% |
| Married | 108 | 28.3% | |
| Divorce or Widow | 15 | 3.9% | |
| Education | None | 28 | 7.3% |
| Primary | 66 | 17.3% | |
| Middle | 40 | 10.5% | |
| High | 95 | 24.9% | |
| University | 147 | 38.6% | |
| Postgrad | 5 | 1.3% | |
| Employment status | Unemployed | 291 | 76.4% |
| Employed | 84 | 22.0% | |
| Retired | 6 | 1.6% | |
| Monthly income in SAR | Less than 2 k | 102 | 26.8% |
| 2 k to 5 k | 111 | 29.1% | |
| 5 k to 10 k | 109 | 28.6% | |
| More than 10 k | 59 | 15.5% | |
| Living with | Parents | 251 | 65.9% |
| Relatives | 27 | 7.1% | |
| Spouse | 84 | 22.0% | |
| Alone | 19 | 5.0% | |
| Residence | Gizan | 64 | 16.8% |
| Sabya | 44 | 11.5% | |
| Samtah | 36 | 9.4% | |
| AbuArish | 104 | 27.3% | |
| Damad | 26 | 6.8% | |
| Alardah | 23 | 6.0% | |
| AhadAlmasarah | 22 | 5.8% | |
| Alhuerrath | 8 | 2.1% | |
| Addarb | 8 | 2.1% | |
| Alaidabi | 7 | 1.8% | |
| Baish | 17 | 4.5% | |
| Other | 22 | 5.8% | |
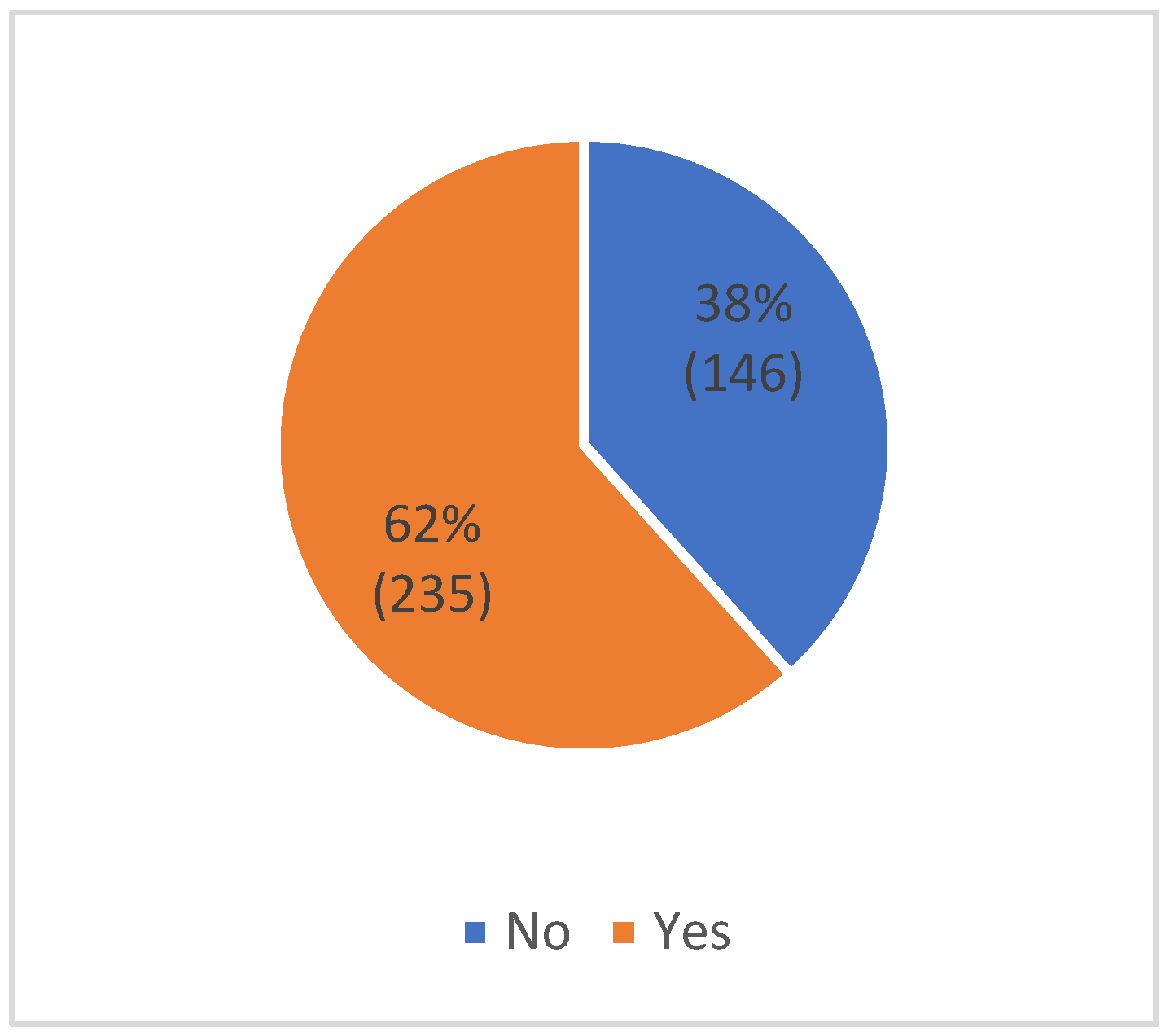
| Missed Clinics | No (n = 146, 38%) | Yes (n = 235, 62%) | p-Value | |||
|---|---|---|---|---|---|---|
| Variables | N | % | n | % | ||
| Age | Less than one year | 3 | 2.1% | 1 | 0.4% | 0.003 * |
| 1 to 10 | 34 | 23.3% | 28 | 11.9% | ||
| 11 to 20 | 38 | 26.0% | 44 | 18.7% | ||
| 21 to 30 | 47 | 32.2% | 108 | 46.0% | ||
| 31 to 40 | 17 | 11.6% | 38 | 16.2% | ||
| More than 40 | 7 | 4.8% | 16 | 6.8% | ||
| Sex | Female | 81 | 55.5% | 145 | 61.7% | 0.240 |
| Male | 65 | 44.5% | 90 | 38.3% | ||
| Marital Status | Single | 98 | 67.1% | 160 | 68.1% | 0.676 |
| Married | 40 | 27.4% | 68 | 28.9% | ||
| Divorce or Widow | 8 | 5.5% | 7 | 3.0% | ||
| Education | None | 14 | 9.6% | 14 | 6.0% | 0.017 * |
| Primary | 36 | 24.7% | 30 | 12.8% | ||
| Middle | 17 | 11.6% | 23 | 9.8% | ||
| High | 30 | 20.5% | 65 | 27.7% | ||
| University | 48 | 32.9% | 99 | 42.1% | ||
| Postgrad | 1 | 0.7% | 4 | 1.7% | ||
| Employment status | Unemployed | 117 | 80.1% | 174 | 74.0% | 0.285 |
| Employed | 28 | 19.2% | 56 | 23.8% | ||
| Retired | 1 | 0.7% | 5 | 2.1% | ||
| Monthly income in SAR | Less than 2 k | 46 | 31.5% | 56 | 23.8% | 0.022 * |
| 2 k to 5 k | 40 | 27.4% | 71 | 30.2% | ||
| 5 k to 10 k | 31 | 21.2% | 78 | 33.2% | ||
| More than 10 k | 29 | 19.9% | 30 | 12.8% | ||
| Living with | Parents | 96 | 65.8% | 155 | 66.0% | 0.077 |
| Relatives | 10 | 6.8% | 5 | 2.1% | ||
| Spouse | 30 | 20.5% | 54 | 23.0% | ||
| Alone | 10 | 6.8% | 21 | 8.9% | ||
| Residence | Gizan | 38 | 26.0% | 26 | 11.1% | 0.006 * |
| Sabya | 17 | 11.6% | 27 | 11.5% | ||
| Samtah | 11 | 7.5% | 25 | 10.6% | ||
| AbuArish | 36 | 24.7% | 68 | 28.9% | ||
| Damad | 8 | 5.5% | 18 | 7.7% | ||
| Alardah | 5 | 3.4% | 18 | 7.7% | ||
| AhadAlmasarah | 6 | 4.1% | 16 | 6.8% | ||
| Alhuerrath | 0 | 0.0% | 8 | 3.4% | ||
| Addarb | 3 | 2.1% | 5 | 2.1% | ||
| Alaidabi | 3 | 2.1% | 4 | 1.7% | ||
| Baish | 10 | 6.8% | 7 | 3.0% | ||
| Other | 9 | 6.2% | 13 | 5.5% | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhazmi, S.A.; Maashi, A.Q.; Shabaan, S.K.; Majrashi, A.A.; Thakir, M.A.; Almetahr, S.M.; Qadri, A.M.; Hakami, A.A.; Abdelwahab, S.I.; Alhazmi, A.H. The Health Belief Model Modifying Factors Associated with Missed Clinic Appointments among Individuals with Sickle Cell Disease in the Jazan Province, Saudi Arabia. Healthcare 2022, 10, 2376. https://doi.org/10.3390/healthcare10122376
Alhazmi SA, Maashi AQ, Shabaan SK, Majrashi AA, Thakir MA, Almetahr SM, Qadri AM, Hakami AA, Abdelwahab SI, Alhazmi AH. The Health Belief Model Modifying Factors Associated with Missed Clinic Appointments among Individuals with Sickle Cell Disease in the Jazan Province, Saudi Arabia. Healthcare. 2022; 10(12):2376. https://doi.org/10.3390/healthcare10122376
Chicago/Turabian StyleAlhazmi, Sami A., Afnan Q. Maashi, Shahad K. Shabaan, Aisha A. Majrashi, Mawaeed A. Thakir, Safa M. Almetahr, Alanoud M. Qadri, Abdulaziz A. Hakami, Siddig I. Abdelwahab, and Abdulaziz H. Alhazmi. 2022. "The Health Belief Model Modifying Factors Associated with Missed Clinic Appointments among Individuals with Sickle Cell Disease in the Jazan Province, Saudi Arabia" Healthcare 10, no. 12: 2376. https://doi.org/10.3390/healthcare10122376
APA StyleAlhazmi, S. A., Maashi, A. Q., Shabaan, S. K., Majrashi, A. A., Thakir, M. A., Almetahr, S. M., Qadri, A. M., Hakami, A. A., Abdelwahab, S. I., & Alhazmi, A. H. (2022). The Health Belief Model Modifying Factors Associated with Missed Clinic Appointments among Individuals with Sickle Cell Disease in the Jazan Province, Saudi Arabia. Healthcare, 10(12), 2376. https://doi.org/10.3390/healthcare10122376






