Monocyte–Lymphocyte Ratio and Dysglycemia: A Retrospective, Cross-Sectional Study of the Saudi Population
Abstract
1. Introduction
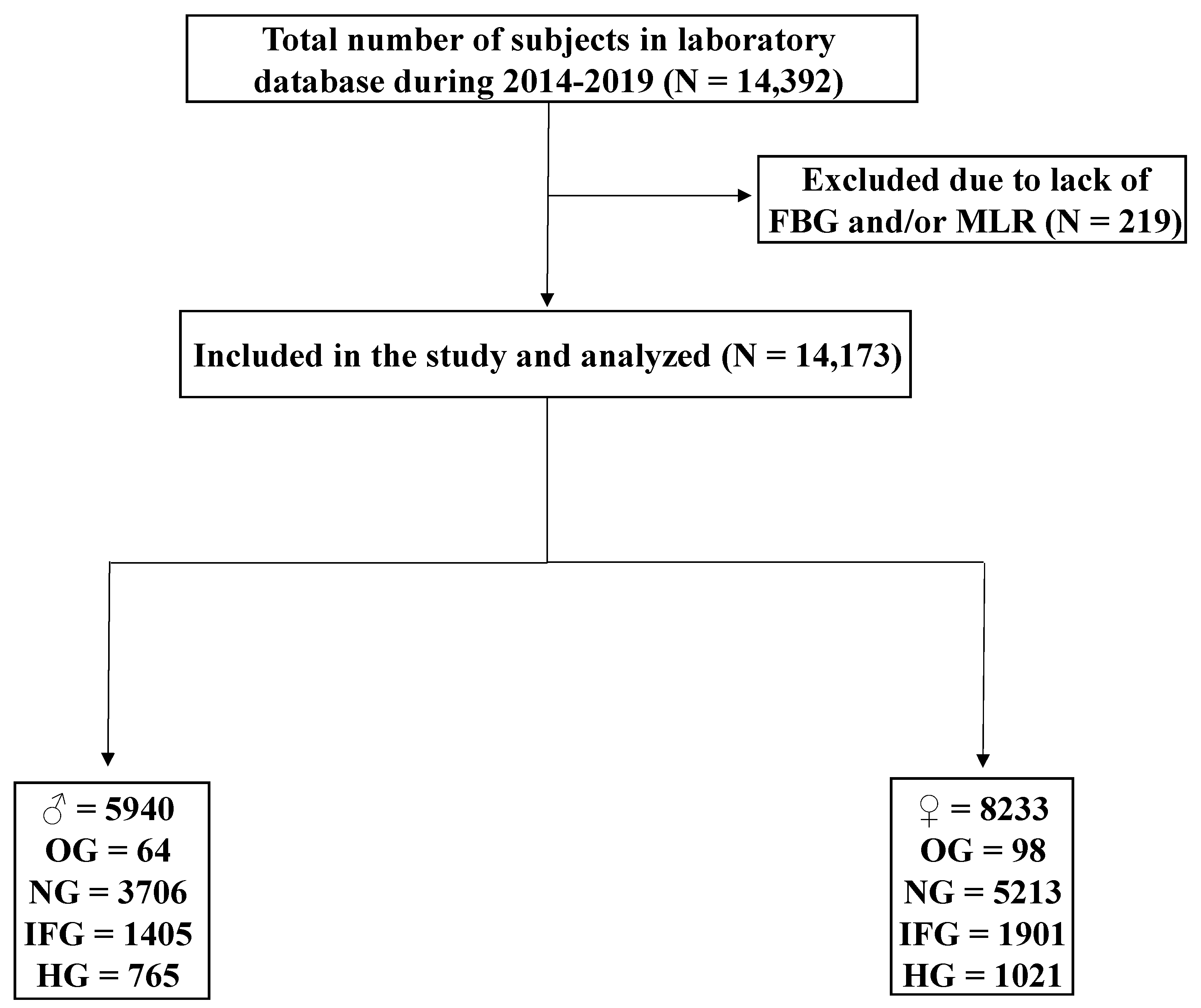
2. Materials and Methods
2.1. Data Collection and Study Design
2.2. Statistical Analysis
3. Results
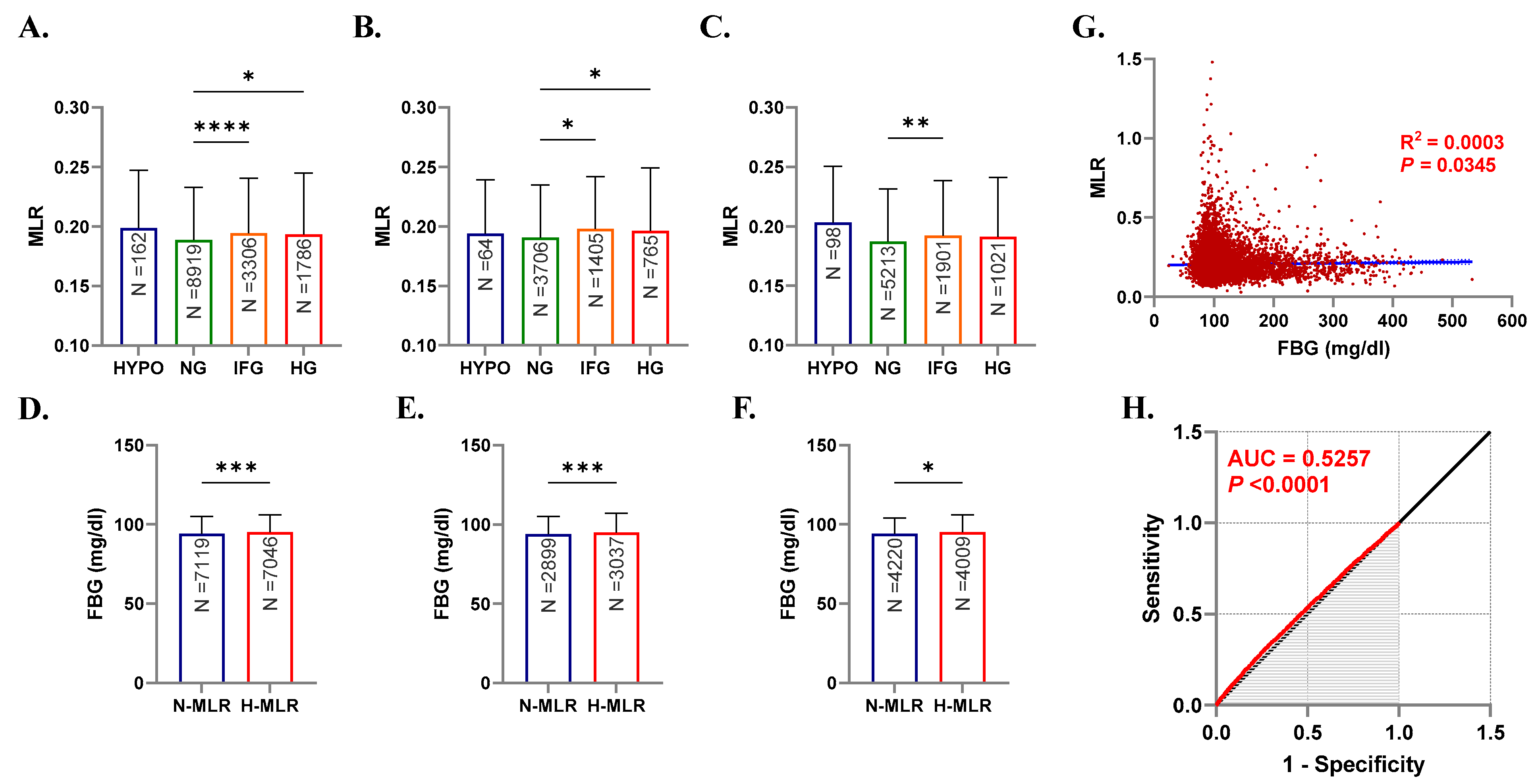
3.1. MLR Is Significantly Elevated in IFG and HG
3.2. FBG Is Significantly Increased in Individuals with Elevated MLR
3.3. Correlation between MLR and FBG
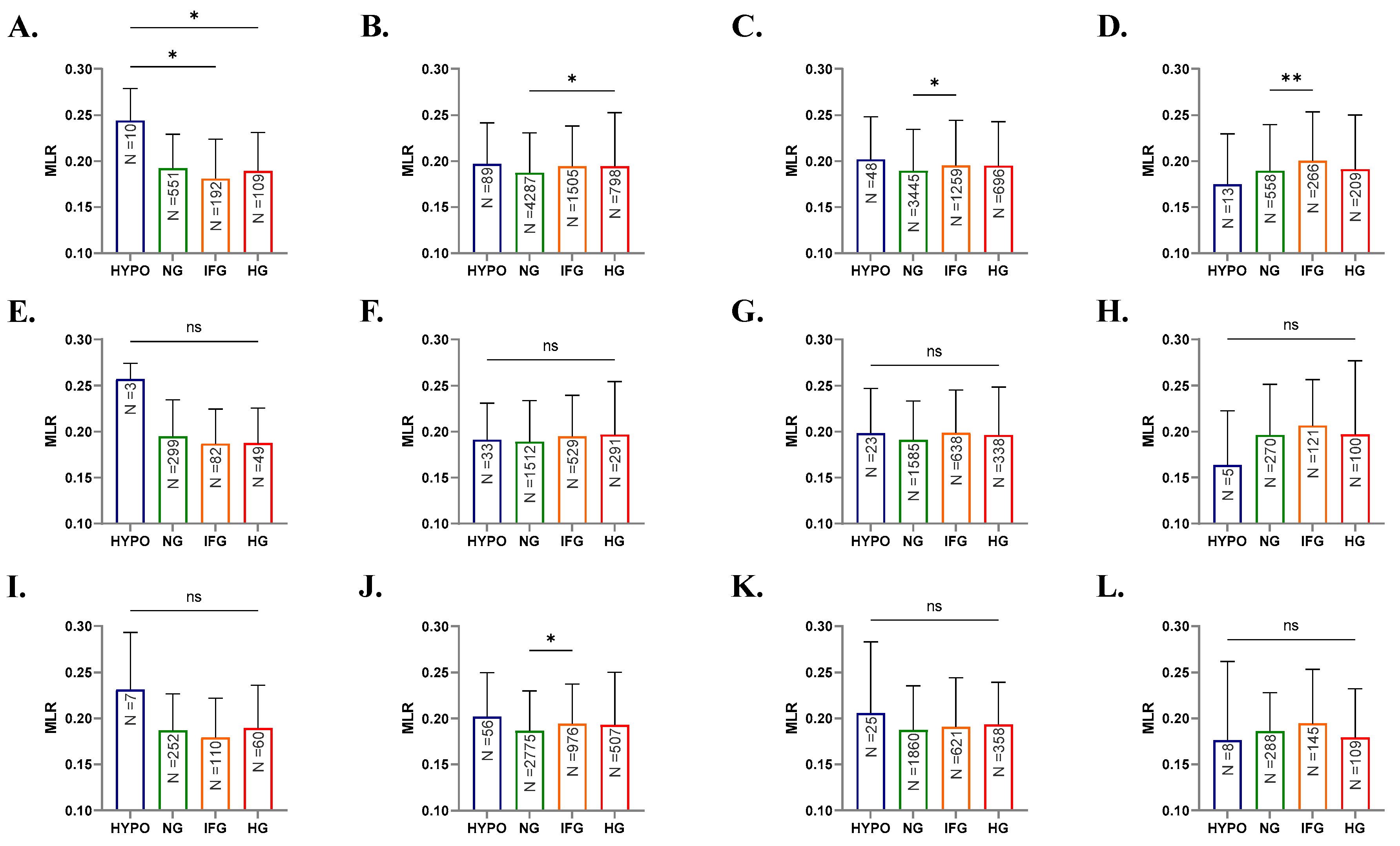
3.4. Differential Influence of Age and Gender on MLR
3.5. Elevated MLR Is Associated with Increased Risk of IFG and HG
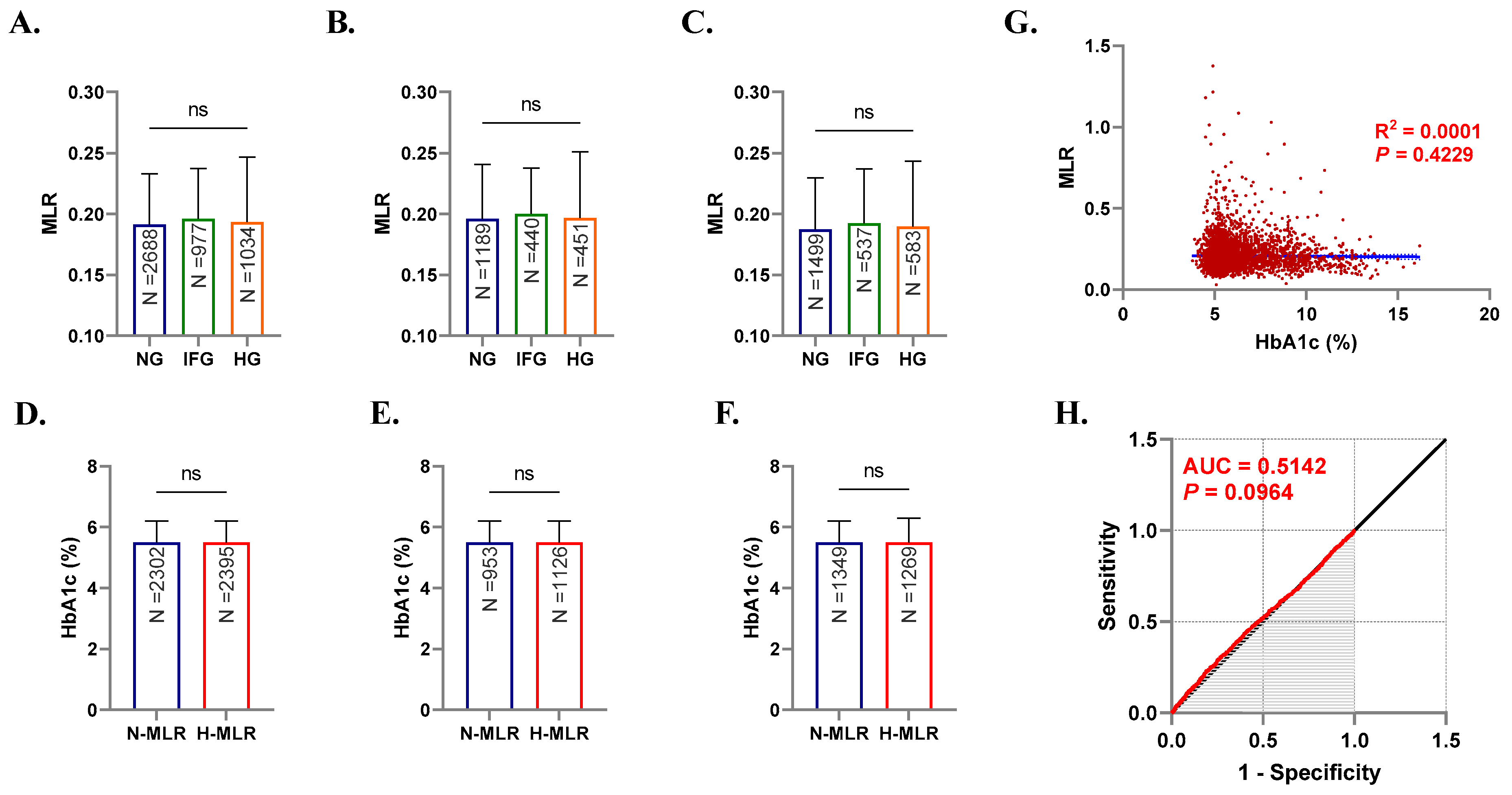
3.6. MLR Is Not Influenced by HbA1c Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Koch, C.A.; Petersenn, S. Black swans—Neuroendocrine tumors of rare locations. Rev. Endocr. Metab. Disord. 2018, 19, 111–121. [Google Scholar] [CrossRef]
- Bano, G. Glucose homeostasis, obesity and diabetes. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 715–726. [Google Scholar] [CrossRef]
- Pond, C.M. Adipose tissue and the immune system. Prostaglandins Leukot. Essent. Fat. Acids 2005, 73, 17–30. [Google Scholar] [CrossRef]
- Kanter, J.E.; Hsu, C.C.; Bornfeldt, K.E. Monocytes and Macrophages as Protagonists in Vascular Complications of Diabetes. Front. Cardiovasc. Med. 2020, 7, 10. [Google Scholar] [CrossRef]
- Burke, A.P.; Kolodgie, F.D.; Zieske, A.; Fowler, D.R.; Weber, D.K.; Varghese, P.J.; Farb, A.; Virmani, R. Morphologic findings of coronary atherosclerotic plaques in diabetics: A postmortem study. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1266–1271. [Google Scholar] [CrossRef]
- Yan, J.; Tie, G.; Wang, S.; Tutto, A.; DeMarco, N.; Khair, L.; Fazzio, T.G.; Messina, L.M. Diabetes impairs wound healing by Dnmt1-dependent dysregulation of hematopoietic stem cells differentiation towards macrophages. Nat. Commun. 2018, 9, 33. [Google Scholar] [CrossRef]
- Rahman, K.; Vengrenyuk, Y.; Ramsey, S.A.; Vila, N.R.; Girgis, N.M.; Liu, J.; Gusarova, V.; Gromada, J.; Weinstock, A.; Moore, K.J.; et al. Inflammatory Ly6Chi monocytes and their conversion to M2 macrophages drive atherosclerosis regression. J. Clin. Investig. 2017, 127, 2904–2915. [Google Scholar] [CrossRef]
- Bailin, S.S.; McGinnis, K.A.; McDonnell, W.J.; So-Armah, K.; Wellons, M.; Tracy, R.P.; Doyle, M.F.; Mallal, S.; Justice, A.C.; Freiberg, M.S.; et al. T Lymphocyte Subsets Associated With Prevalent Diabetes in Veterans With and Without Human Immunodeficiency Virus. J. Infect. Dis. 2020, 222, 252–262. [Google Scholar] [CrossRef]
- Otton, R.; Mendonca, J.R.; Curi, R. Diabetes causes marked changes in lymphocyte metabolism. J. Endocrinol. 2002, 174, 55–61. [Google Scholar] [CrossRef]
- Muniyappa, R.; Gubbi, S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am. J. Physiol. Endocrinol. Metab. 2020, 318, E736–E741. [Google Scholar] [CrossRef]
- Xia, C.; Rao, X.; Zhong, J. Role of T Lymphocytes in Type 2 Diabetes and Diabetes-Associated Inflammation. J. Diabetes Res. 2017, 2017, 6494795. [Google Scholar] [CrossRef]
- Mangaonkar, A.A.; Tande, A.J.; Bekele, D.I. Differential Diagnosis and Workup of Monocytosis: A Systematic Approach to a Common Hematologic Finding. Curr. Hematol. Malig. Rep. 2021, 16, 267–275. [Google Scholar] [CrossRef]
- Aluri, J.; Gupta, M.R.; Dalvi, A.; Mhatre, S.; Kulkarni, M.; Desai, M.; Shah, N.K.; Madkaikar, M.R. Lymphopenia and Severe Combined Immunodeficiency (SCID)—Think Before You Ink. Indian J. Pediatr. 2019, 86, 584–589. [Google Scholar] [CrossRef]
- Martin, M.; Guffroy, A.; Argemi, X.; Martin, T. Systemic lupus erythematosus and lymphopenia: Clinical and pathophysiological features. Rev. Med. Interne 2017, 38, 603–613. [Google Scholar] [CrossRef]
- Cheng, Y.; Yue, L.; Wang, Z.; Zhang, J.; Xiang, G. Hyperglycemia associated with lymphopenia and disease severity of COVID-19 in type 2 diabetes mellitus. J. Diabetes Complicat. 2021, 35, 107809. [Google Scholar] [CrossRef]
- Lepe-Zuniga, J.L.; Morales-Molina, P.; Garcia-Nandayapa, G.A. End stage renal disease lymphopenia; characterization and clinical correlation. Rev. Médica Del Inst. Mex. Del Seguro Soc. 2016, 54, 446–453. [Google Scholar]
- Tang, C.; Liao, Z.; Gomez, D.; Levy, L.; Zhuang, Y.; Gebremichael, R.A.; Hong, D.S.; Komaki, R.; Welsh, J.W. Lymphopenia association with gross tumor volume and lung V5 and its effects on non-small cell lung cancer patient outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 1084–1091. [Google Scholar] [CrossRef]
- Guo, Z.; Zhang, Z.; Prajapati, M.; Li, Y. Lymphopenia Caused by Virus Infections and the Mechanisms Beyond. Viruses 2021, 13, 1876. [Google Scholar] [CrossRef]
- Turett, G.S.; Telzak, E.E. Normalization of CD4+ T-lymphocyte depletion in patients without HIV infection treated for tuberculosis. Chest 1994, 105, 1335–1337. [Google Scholar] [CrossRef]
- Kumarasamy, C.; Tiwary, V.; Sunil, K.; Suresh, D.; Shetty, S.; Muthukaliannan, G.K.; Baxi, S.; Jayaraj, R. Prognostic Utility of Platelet-Lymphocyte Ratio, Neutrophil-Lymphocyte Ratio and Monocyte-Lymphocyte Ratio in Head and Neck Cancers: A Detailed PRISMA Compliant Systematic Review and Meta-Analysis. Cancers 2021, 13, 4166. [Google Scholar] [CrossRef]
- Mazza, M.G.; Lucchi, S.; Rossetti, A.; Clerici, M. Neutrophil-lymphocyte ratio, monocyte-lymphocyte ratio and platelet-lymphocyte ratio in non-affective psychosis: A meta-analysis and systematic review. World J. Biol. Psychiatry 2020, 21, 326–338. [Google Scholar] [CrossRef]
- Ji, H.; Li, Y.; Fan, Z.; Zuo, B.; Jian, X.; Li, L.; Liu, T. Monocyte/lymphocyte ratio predicts the severity of coronary artery disease: A syntax score assessment. BMC Cardiovasc. Disord. 2017, 17, 90. [Google Scholar] [CrossRef]
- Wang, J.; Zhu, Q.W.; Cheng, X.Y.; Liu, J.Y.; Zhang, L.L.; Tao, Y.M.; Cui, Y.B.; Wei, Y. Assessment efficacy of neutrophil-lymphocyte ratio and monocyte-lymphocyte ratio in preeclampsia. J. Reprod. Immunol. 2019, 132, 29–34. [Google Scholar] [CrossRef]
- Cheng, H.R.; Song, J.Y.; Zhang, Y.N.; Chen, Y.B.; Lin, G.Q.; Huang, G.Q.; He, J.C.; Wang, Z. High Monocyte-To-Lymphocyte Ratio Is Associated With Stroke-Associated Pneumonia. Front. Neurol. 2020, 11, 575809. [Google Scholar] [CrossRef]
- Wang, W.; Wang, L.F.; Liu, Y.Y.; Yang, F.; Zhu, L.; Zhang, X.H. Value of the Ratio of Monocytes to Lymphocytes for Monitoring Tuberculosis Therapy. Can. J. Infect. Dis. Med. Microbiol. 2019, 2019, 3270393. [Google Scholar] [CrossRef]
- Nishijima, T.F.; Muss, H.B.; Shachar, S.S.; Tamura, K.; Takamatsu, Y. Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: A systematic review and meta-analysis. Cancer Treat. Rev. 2015, 41, 971–978. [Google Scholar] [CrossRef]
- Alfhili, M.A.; Alsughayyir, J.; Basudan, A.; Ghneim, H.K.; Aboul-Soud, M.A.; Marie, M.; Dera, A.; Alfaifi, M.; Alkhathami, A.G.; Awan, Z.A.; et al. Isolated and Combined Effect of Age and Gender on Neutrophil-Lymphocyte Ratio in the Hyperglycemic Saudi Population. Medicina 2022, 58, 1040. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care 2014, 37 (Suppl. S1), S14–S80. [Google Scholar] [CrossRef]
- Alfhili, M.A.; Alsughayyir, J.; Basudan, A.M.; Ghneim, H.K.; Alfaifi, M.; Alamri, H.S.; Awan, Z.A.; Algethami, M.R. Patterns of Dyslipidemia in the Anemic and Nonanemic Hypertensive Saudi Population: A Cross-Sectional Study. Int. J. Gen. Med. 2022, 15, 7895–7906. [Google Scholar] [CrossRef]
- Allan, C.A. Sex steroids and glucose metabolism. Asian J. Androl. 2014, 16, 232–238. [Google Scholar] [CrossRef]
- Reinehr, T.; Roth, C.L. Inflammation Markers in Type 2 Diabetes and the Metabolic Syndrome in the Pediatric Population. Curr. Diabetes Rep. 2018, 18, 131. [Google Scholar] [CrossRef]
- Weyand, C.M.; Goronzy, J.J. Aging of the Immune System. Mechanisms and Therapeutic Targets. Ann. Am. Thorac. Soc. 2016, 13 (Suppl. S5), S422–S428. [Google Scholar] [CrossRef]
- Morbach, H.; Eichhorn, E.M.; Liese, J.G.; Girschick, H.J. Reference values for B cell subpopulations from infancy to adulthood. Clin. Exp. Immunol. 2010, 162, 271–279. [Google Scholar] [CrossRef]
- Liu, S.; Hempe, J.M.; McCarter, R.J.; Li, S.; Fonseca, V.A. Association between Inflammation and Biological Variation in Hemoglobin A1c in U.S. Nondiabetic Adults. J. Clin. Endocrinol. Metab. 2015, 100, 2364–2371. [Google Scholar] [CrossRef]
- Jaiswal, A.; Tabassum, R.; Podder, A.; Ghosh, S.; Tandon, N.; Bharadwaj, D. Elevated level of C-reactive protein is associated with risk of prediabetes in Indians. Atherosclerosis 2012, 222, 495–501. [Google Scholar] [CrossRef]
- Simental-Mendía, L.E.; Lazalde, B.; Zambrano-Galván, G.; Simental-Saucedo, L.; Rábago-Sánchez, E.; Rodríguez-Morán, M.; Guerrero-Romero, F. Relation between C-reactive protein and impaired fasting glucose in obese subjects. Inflammation 2012, 35, 1742–1746. [Google Scholar] [CrossRef]
- Al-Rubeaan, K.; Al-Manaa, H.; Khoja, T.; Ahmad, N.; Al-Sharqawi, A.; Siddiqui, K.; AlNaqeb, D.; Aburisheh, K.; Youssef, A.; Al-Batil, A.; et al. The Saudi Abnormal Glucose Metabolism and Diabetes Impact Study (SAUDI-DM). Ann. Saudi Med. 2014, 34, 465–475. [Google Scholar] [CrossRef]
- Mendes, B.B.; Oliveira, A.C.R.; Alcantara, K.C. Comparison of the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in normoglycemic and hyperglycemic subjects. Einstein (Sao Paulo) 2019, 17, eAO4403. [Google Scholar] [CrossRef]
- Demirtas, L.; Degirmenci, H.; Akbas, E.M.; Ozcicek, A.; Timuroglu, A.; Gurel, A.; Ozcicek, F. Association of hematological indicies with diabetes, impaired glucose regulation and microvascular complications of diabetes. Int. J. Clin. Exp. Med. 2015, 8, 11420–11427. [Google Scholar]
- Kocak, M.Z.; Aktas, G.; Duman, T.T.; Atak, B.M.; Kurtkulagi, O.; Tekce, H.; Bilgin, S.; Alaca, B. Monocyte lymphocyte ratio As a predictor of Diabetic Kidney Injury in type 2 Diabetes mellitus; The MADKID Study. J. Diabetes Metab. Disord. 2020, 19, 997–1002. [Google Scholar] [CrossRef]
- Huang, Q.; Wu, H.; Wo, M.; Ma, J.; Fei, X.; Song, Y. Monocyte-lymphocyte ratio is a valuable predictor for diabetic nephropathy in patients with type 2 diabetes. Medicine (Baltimore) 2020, 99, e20190. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Guo, Z.; Xu, Y. Association of monocyte-lymphocyte ratio and proliferative diabetic retinopathy in the U.S. population with type 2 diabetes. J. Transl. Med. 2022, 20, 219. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Wu, H.; Wo, M.; Ma, J.; Song, Y.; Fei, X. Clinical and predictive significance of Plasma Fibrinogen Concentrations combined Monocyte-lymphocyte ratio in patients with Diabetic Retinopathy. Int. J. Med. Sci. 2021, 18, 1390–1398. [Google Scholar] [CrossRef] [PubMed]
- Ilhan, C.; Citirik, M.; Uzel, M.M.; Kiziltoprak, H.; Tekin, K. The usefulness of systemic inflammatory markers as diagnostic indicators of the pathogenesis of diabetic macular edema. Arq. Bras. De Oftalmol. 2020, 83, 299–304. [Google Scholar] [CrossRef]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Tramunt, B.; Smati, S.; Grandgeorge, N.; Lenfant, F.; Arnal, J.F.; Montagner, A.; Gourdy, P. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia 2020, 63, 453–461. [Google Scholar] [CrossRef]
- Anagnostis, P.; Christou, K.; Artzouchaltzi, A.M.; Gkekas, N.K.; Kosmidou, N.; Siolos, P.; Paschou, S.A.; Potoupnis, M.; Kenanidis, E.; Tsiridis, E.; et al. Early menopause and premature ovarian insufficiency are associated with increased risk of type 2 diabetes: A systematic review and meta-analysis. Eur. J. Endocrinol. 2019, 180, 41–50. [Google Scholar] [CrossRef]
- Beumer, W.; Gibney, S.M.; Drexhage, R.C.; Pont-Lezica, L.; Doorduin, J.; Klein, H.C.; Steiner, J.; Connor, T.J.; Harkin, A.; Versnel, M.A.; et al. The immune theory of psychiatric diseases: A key role for activated microglia and circulating monocytes. J. Leukoc. Biol. 2012, 92, 959–975. [Google Scholar] [CrossRef]
- Cai, H.Q.; Catts, V.S.; Webster, M.J.; Galletly, C.; Liu, D.; O’Donnell, M.; Weickert, T.W.; Weickert, C.S. Increased macrophages and changed brain endothelial cell gene expression in the frontal cortex of people with schizophrenia displaying inflammation. Mol. Psychiatry 2020, 25, 761–775. [Google Scholar] [CrossRef]
- Palm, M.; Axelsson, O.; Wernroth, L.; Larsson, A.; Basu, S. Involvement of inflammation in normal pregnancy. Acta Obstet. Gynecol. Scand. 2013, 92, 601–605. [Google Scholar] [CrossRef]
- Liu, L.; Zhao, G.; Fan, H.; Zhao, X.; Li, P.; Wang, Z.; Hu, Y.; Hou, Y. Mesenchymal stem cells ameliorate Th1-induced pre-eclampsia-like symptoms in mice via the suppression of TNF-alpha expression. PLoS ONE 2014, 9, e88036. [Google Scholar]
- Wang, J.; Zhu, Q.W.; Cheng, X.Y.; Sha, C.X.; Cui, Y.B. Clinical significance of neutrophil-lymphocyte ratio and monocyte-lymphocyte ratio in women with hyperglycemia. Postgrad. Med. 2020, 132, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, M.; Liu, L.; Dang, X.; Zhu, D.; Tian, G. Monocyte/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients with non-ST-elevation myocardial infarction. Medicine (Baltimore) 2019, 98, e16267. [Google Scholar] [CrossRef] [PubMed]
- Mirna, M.; Schmutzler, L.; Topf, A.; Hoppe, U.C.; Lichtenauer, M. Neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio predict length of hospital stay in myocarditis. Sci. Rep. 2021, 11, 18101. [Google Scholar] [CrossRef]
- Aydin, C.; Engin, M. The Value of Inflammation Indexes in Predicting Patency of Saphenous Vein Grafts in Patients With Coronary Artery Bypass Graft Surgery. Cureus 2021, 13, e16646. [Google Scholar] [CrossRef]
- Kadiyoran, C.; Zengin, O.; Cizmecioglu, H.A.; Tufan, A.; Kucuksahin, O.; Cure, M.C.; Cure, E.; Kucuk, A.; Ozturk, M.A. Monocyte to Lymphocyte Ratio, Neutrophil to Lymphocyte Ratio, and Red Cell Distribution Width are the Associates with Gouty Arthritis. Acta Med. 2019, 62, 99–104. [Google Scholar] [CrossRef][Green Version]
- Buttle, T.S.; Hummerstone, C.Y.; Billahalli, T.; Ward, R.J.; Barnes, K.E.; Marshall, N.J.; Spong, V.C.; Bothamley, G.H. The monocyte-to-lymphocyte ratio: Sex-specific differences in the tuberculosis disease spectrum, diagnostic indices and defining normal ranges. PLoS ONE 2021, 16, e0247745. [Google Scholar]
- Long, V.S.; Ngiam, J.N.; Chew, N.; Tham, S.M.; Lim, Z.Y.; Li, T.; Cen, S.; Annadurai, J.K.; Thant, S.M.; Tambyah, P.A.; et al. Haematological profile of COVID-19 patients from a centre in Singapore. Hematology 2021, 26, 1007–1012. [Google Scholar] [CrossRef]
- Muto, R.; Kato, S.; Lindholm, B.; Qureshi, A.R.; Ishimoto, T.; Kosugi, T.; Maruyama, S. Increased Monocyte/Lymphocyte Ratio as Risk Marker for Cardiovascular Events and Infectious Disease Hospitalization in Dialysis Patients. Blood Purif. 2022, 51, 747–755. [Google Scholar] [CrossRef]
- Li, Y.; Liu, Y.; Zhou, C.; Zhang, Z.; Zuo, X.; Li, J.; Cao, Q. Monocyte/lymphocyte ratio as a predictor of 30-day mortality and adverse events in critically ill patients: Analysis of the MIMIC-III database. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2021, 33, 582–586. [Google Scholar]
- Kamiya, N.; Ishikawa, Y.; Kotani, K.; Hatakeyama, S.; Matsumura, M. Monocyte-to-Lymphocyte Ratio in the Diagnosis of Lymphoma in Adult Patients. Int. J. Gen. Med. 2022, 15, 4221–4226. [Google Scholar] [CrossRef] [PubMed]
- Xiang, J.; Zhou, L.; Li, X.; Bao, W.; Chen, T.; Xi, X.; He, Y.; Wan, X. Preoperative Monocyte-to-Lymphocyte Ratio in Peripheral Blood Predicts Stages, Metastasis, and Histological Grades in Patients with Ovarian Cancer. Transl. Oncol. 2017, 10, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Soibi-Harry, A.P.; Amaeshi, L.C.; Garba, S.R.; Anorlu, R.I. The relationship between pre-operative lymphocyte to monocyte ratio and serum cancer antigen-125 among women with epithelial ovarian cancer in Lagos, Nigeria. Ecancermedicalscience 2021, 15, 1288. [Google Scholar] [CrossRef] [PubMed]
- Adamkiewicz, M.; Bryniarski, P.; Kowalik, M.; Burzynski, B.; Rajwa, P.; Paradysz, A. Lymphocyte-to-Monocyte Ratio Is the Independent Prognostic Marker of Progression in Patients Undergoing BCG-Immunotherapy for Bladder Cancer. Front. Oncol. 2021, 11, 655000. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, D.; Moschini, M.; Gust, K.M.; Abufaraj, M.; Özsoy, M.; Mathieu, R.; Soria, F.; Briganti, A.; Rouprêt, M.; Karakiewicz, P.I.; et al. Lymphocyte-to-monocyte ratio and neutrophil-to-lymphocyte ratio as biomarkers for predicting lymph node metastasis and survival in patients treated with radical cystectomy. J. Surg. Oncol. 2017, 115, 455–461. [Google Scholar]
- Zhang, G.M.; Zhu, Y.; Luo, L.; Wan, F.N.; Zhu, Y.P.; Sun, L.J.; Ye, D.W. Preoperative lymphocyte-monocyte and platelet-lymphocyte ratios as predictors of overall survival in patients with bladder cancer undergoing radical cystectomy. Tumour Biol. 2015, 36, 8537–8543. [Google Scholar] [CrossRef]
- Yoshida, T.; Kinoshita, H.; Yoshida, K.; Mishima, T.; Yanishi, M.; Inui, H.; Komai, Y.; Sugi, M.; Inoue, T.; Murota, T.; et al. Prognostic impact of perioperative lymphocyte-monocyte ratio in patients with bladder cancer undergoing radical cystectomy. Tumour Biol. 2016, 37, 10067–10074. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, F.; Sheng, X.G.; Zhang, S.Q. Decreased pretreatment lymphocyte/monocyte ratio is associated with poor prognosis in stage Ib1-IIa cervical cancer patients who undergo radical surgery. OncoTargets Ther. 2015, 8, 1355–1362. [Google Scholar]
- Hu, P.; Shen, H.; Wang, G.; Zhang, P.; Liu, Q.; Du, J. Prognostic significance of systemic inflammation-based lymphocyte- monocyte ratio in patients with lung cancer: Based on a large cohort study. PLoS ONE 2014, 9, e108062. [Google Scholar] [CrossRef]
- Kang, Y.; Zhu, X.; Lin, Z.; Zeng, M.; Shi, P.; Cao, Y.; Chen, F. Compare the Diagnostic and Prognostic Value of MLR, NLR and PLR in CRC Patients. Clin. Lab. 2021, 67. [Google Scholar] [CrossRef]
- Xu, Z.; Zhang, J.; Zhong, Y.; Mai, Y.; Huang, D.; Wei, W.; Huang, J.; Zhao, P.; Lin, F.; Jin, J. Predictive value of the monocyte-to-lymphocyte ratio in the diagnosis of prostate cancer. Medicine (Baltimore) 2021, 100, e27244. [Google Scholar] [CrossRef] [PubMed]
- Wan, H.; Cai, Y.; Wang, Y.; Fang, S.; Chen, C.; Chen, Y.; Xia, F.; Wang, N.; Guo, M.; Lu, Y. The unique association between the level of peripheral blood monocytes and the prevalence of diabetic retinopathy: A cross-sectional study. J. Transl. Med. 2020, 18, 248. [Google Scholar] [CrossRef] [PubMed]
| OG | NG | IFG | HG | |
|---|---|---|---|---|
| Overall | 1.14 | 62.92 | 22.98 | 12.94 |
| N-MLR | 0.50 | 32.47 | 10.97 | 6.30 |
| H-MLR | 0.64 | 30.45 | 12.00 | 6.64 |
| Within-group | ||||
| N-MLR | 43.82 | 51.60 | 47.77 | 48.66 |
| H-MLR | 56.17 | 48.39 | 52.22 | 51.33 |
| Score | 95% CI | z Statistic | P | |
|---|---|---|---|---|
| RR | ||||
| OG | 1.36 | 0.99 to 1.85 | 1.96 | 0.0505 |
| IFG | 1.12 | 1.06 to 1.19 | 3.74 | 0.0002 |
| HG | 1.10 | 1.01 to 1.20 | 2.30 | 0.0216 |
| OR | ||||
| OG | 1.37 | 0.99 to 1.87 | 1.96 | 0.0504 |
| IFG | 1.17 | 1.08 to 1.26 | 3.74 | 0.0002 |
| HG | 1.13 | 1.02 to 1.24 | 2.30 | 0.0216 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfhili, M.A.; Alsughayyir, J.; Basudan, A.M.; Alsubki, R.; Alqahtani, S.; Awan, Z.A.; Algethami, M.R.; Al-Sheikh, Y.A. Monocyte–Lymphocyte Ratio and Dysglycemia: A Retrospective, Cross-Sectional Study of the Saudi Population. Healthcare 2022, 10, 2289. https://doi.org/10.3390/healthcare10112289
Alfhili MA, Alsughayyir J, Basudan AM, Alsubki R, Alqahtani S, Awan ZA, Algethami MR, Al-Sheikh YA. Monocyte–Lymphocyte Ratio and Dysglycemia: A Retrospective, Cross-Sectional Study of the Saudi Population. Healthcare. 2022; 10(11):2289. https://doi.org/10.3390/healthcare10112289
Chicago/Turabian StyleAlfhili, Mohammad A., Jawaher Alsughayyir, Ahmed M. Basudan, Roua Alsubki, Saleh Alqahtani, Zuhier A. Awan, Mohammed R. Algethami, and Yazeed A. Al-Sheikh. 2022. "Monocyte–Lymphocyte Ratio and Dysglycemia: A Retrospective, Cross-Sectional Study of the Saudi Population" Healthcare 10, no. 11: 2289. https://doi.org/10.3390/healthcare10112289
APA StyleAlfhili, M. A., Alsughayyir, J., Basudan, A. M., Alsubki, R., Alqahtani, S., Awan, Z. A., Algethami, M. R., & Al-Sheikh, Y. A. (2022). Monocyte–Lymphocyte Ratio and Dysglycemia: A Retrospective, Cross-Sectional Study of the Saudi Population. Healthcare, 10(11), 2289. https://doi.org/10.3390/healthcare10112289








