The Effect of Public Healthcare Expenditure on the Reduction in Mortality Rates Caused by Unhealthy Habits among the Population
Abstract
1. Introduction
- Act 28/2005 and Act 42/2010 on the production, sale, and consumption of tobacco.
- The National Strategy for Nutrition, Physical Activity, and Prevention of Obesity (NAOS).
- The National Integral Plan for Physical Activity and Sports.
- The Comprehensive Tobacco Action Plan for Andalusia (PITA).
- The Strategy for Promoting Healthy Eating and Physical Activity (PASEAR), 2013–2018, in Aragon.
- The Physical Activity, Sports, and Health Plan (PAFES) in Catalonia.
2. Methodology
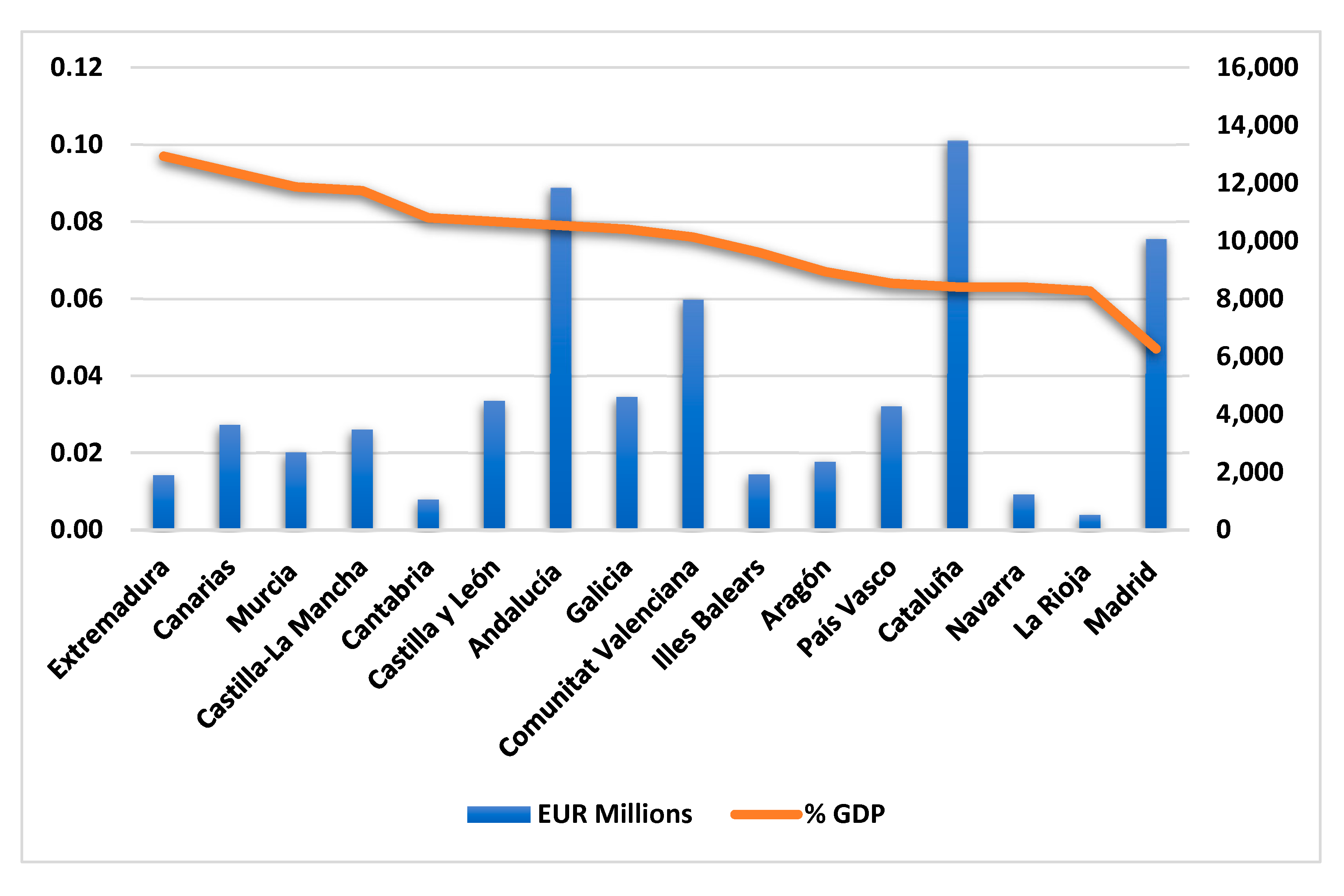
2.1. Sample and Data Collection
2.2. Variables
2.3. Statistical Method
3. Results
3.1. Evaluation of the Measurement Models
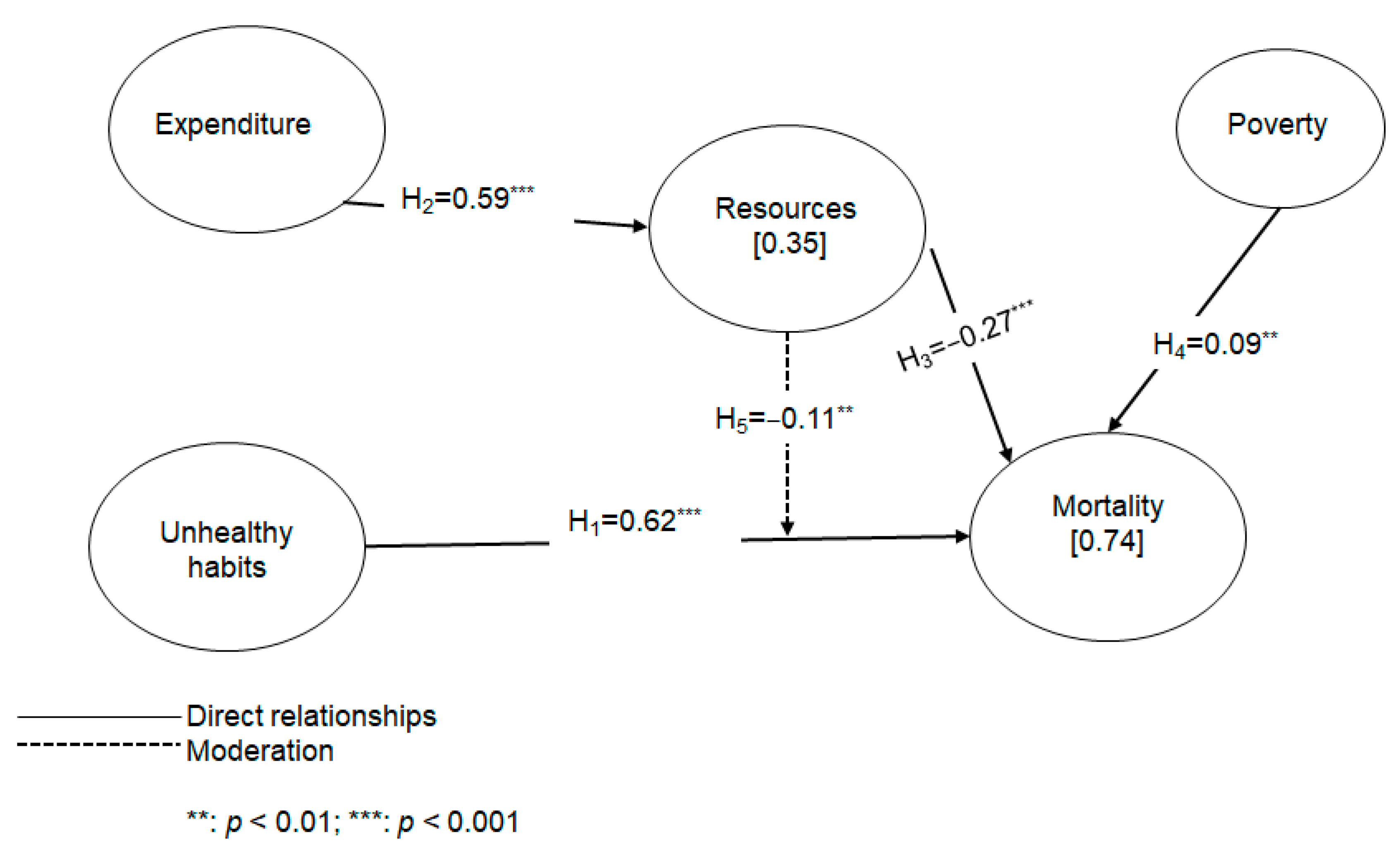
3.2. Evaluation of the Structural Models
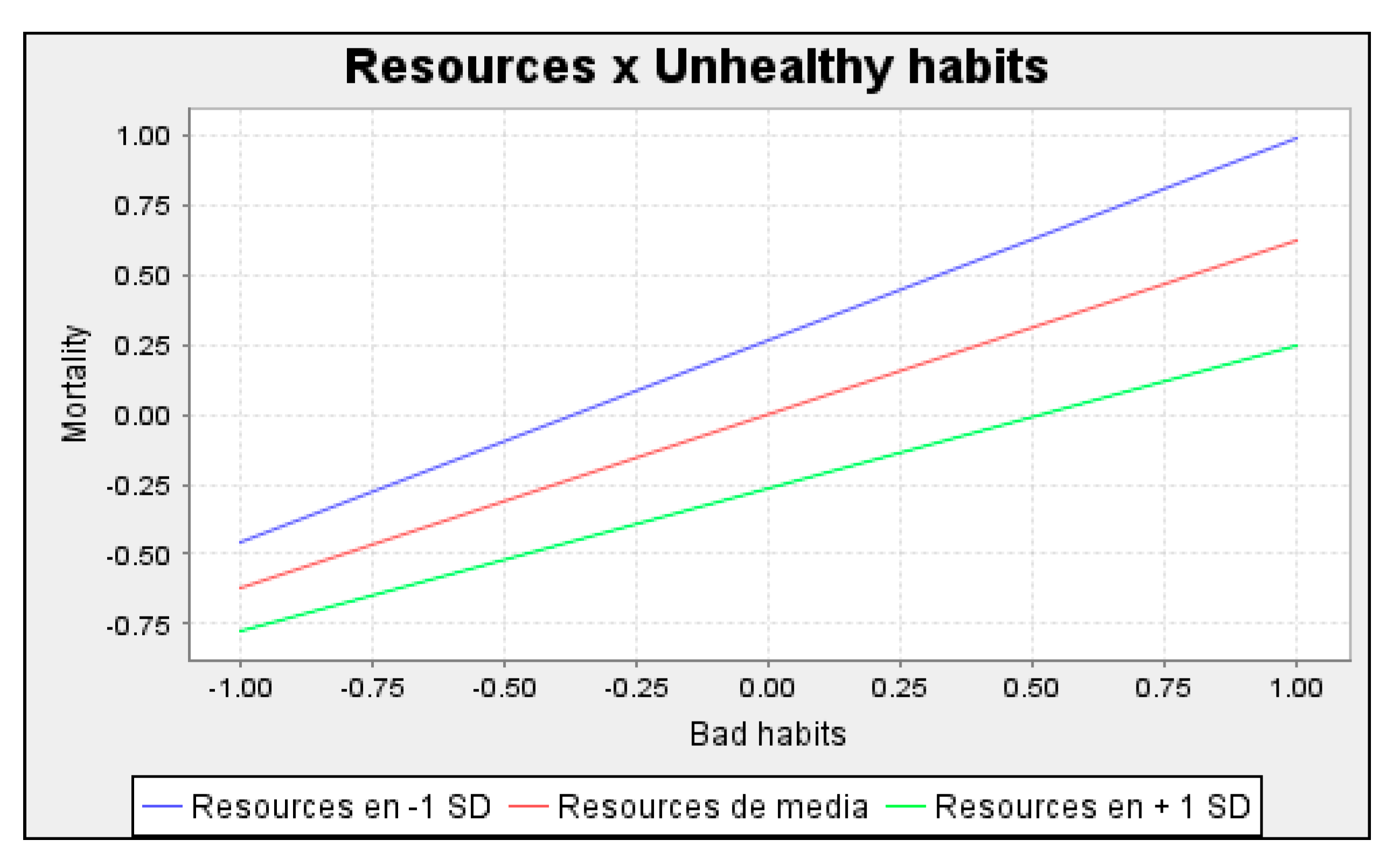
3.3. Moderating Effect
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raeesi, P.; Harati-Khalilabad, T.; Rezapour, A.; Azari, S.; Javan-Noughabi, J. Effects of private and public health expenditure on health outcomes among countries with different health care systems: 2000 and 2014. Med. J. Islam. Repub. Iran 2018, 32, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Bayati, M.; Akbarian, R.; Kavosi, Z. Determinants of Life Expectancy in Eastern Mediterranean Region: A Health Production Function. Int. J. Heal. Policy Manag. 2013, 1, 57–61. [Google Scholar] [CrossRef] [PubMed]
- von Schirnding, Y. The World Summit on Sustainable Development: Reaffirming the centrality of health. Global. Health 2005, 1, 8. [Google Scholar] [CrossRef]
- Valls Martínez, M.d.C.; Ramírez-Orellana, A. Patient Satisfaction in the Spanish National Health Service: Partial Least Squares Structural Equation Modeling. Int. J. Environ. Res. Public Health 2019, 16, 4886. [Google Scholar] [CrossRef] [PubMed]
- Arrazola-Vacas, M.; de Hevia-Payá, J.; Rodríguez-Esteban, L. Qué factores ayudan a explicar la satisfacción con la Atención Primaria en España? Rev. Calid. Asist. 2015, 30, 226–236. [Google Scholar] [CrossRef]
- Kruk, M.E.; Gage, A.D.; Joseph, N.T.; Danaei, G.; García-Saisó, S.; Salomon, J.A. Mortality due to low-quality health systems in the universal health coverage era: A systematic analysis of amenable deaths in 137 countries. Lancet 2018, 392, 2203–2212. [Google Scholar] [CrossRef]
- Expansión Mortalidad España. Available online: https://datosmacro.expansion.com/demografia/mortalidad/espana (accessed on 2 September 2022).
- Esai Selvan, M. Risk factors for death from COVID-19. Nat. Rev. Immunol. 2020, 20, 407. [Google Scholar] [CrossRef] [PubMed]
- Rueda-Salazar, S.; Spijker, J.; Devolder, D.; Albala, C. The contribution of social participation to differences in life expectancy and healthy years among the older population: A comparison between Chile, Costa Rica and Spain. PLoS ONE 2021, 16, e0248179. [Google Scholar] [CrossRef] [PubMed]
- INE INEbase/Sociedad/Salud/Encuesta Europea de Salud en España/Resultados. Available online: https://www.ine.es/dyngs/INEbase/operacion.htm?c=Estadistica_C&cid=1254736176784&menu=resultados&idp=1254735573175 (accessed on 7 September 2022).
- Reynolds, S.L. Successful aging in spite of bad habits: Introduction to the special section on ‘Life style and health expectancy’. Eur. J. Ageing 2008, 5, 275–278. [Google Scholar] [CrossRef][Green Version]
- Loef, M.; Walach, H. The combined effects of healthy lifestyle behaviors on all cause mortality: A systematic review and meta-analysis. Prev. Med. 2012, 55, 163–170. [Google Scholar] [CrossRef]
- Yun, J.E.; Won, S.; Kimm, H.; Jee, S.H. Effects of a combined lifestyle score on 10-year mortality in Korean men and women: A prospective cohort study. BMC Public Health 2012, 12, 673. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, M.; Lopez, A.D.; Rodgers, A.; Vander Hoorn, S.; Murray, C.J. Selected major risk factors and global and regional burden of disease. Lancet 2022, 360, 1347–1360. [Google Scholar] [CrossRef]
- Yang, J.J.; Yu, D.; Wen, W.; Shu, X.-O.; Saito, E.; Rahman, S.; Gupta, P.C.; He, J.; Tsugane, S.; Xiang, Y.-B.; et al. Tobacco Smoking and Mortality in Asia. JAMA Netw. Open 2019, 2, e191474. [Google Scholar] [CrossRef] [PubMed]
- Thurber, K.A.; Banks, E.; Joshy, G.; Soga, K.; Marmor, A.; Benton, G.; White, S.L.; Eades, S.; Maddox, R.; Calma, T.; et al. Tobacco smoking and mortality among Aboriginal and Torres Strait Islander adults in Australia. Int. J. Epidemiol. 2021, 50, 942–954. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Alghamdi, S.M.; Almehmadi, M.; Alqahtani, A.S.; Quaderi, S.; Mandal, S.; Hurst, J.R. Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0233147. [Google Scholar] [CrossRef]
- Rostron, B.L.; Chang, C.M.; Davis Lynn, B.C.; Ren, C.; Salazar, E.; Ambrose, B.K. The contribution of smoking-attributable mortality to differences in mortality and life expectancy among US African-American and white adults, 2000–2019. Demogr. Res. 2022, 46, 905–918. [Google Scholar] [CrossRef]
- Piñeiro, B.; Trias-Llimós, S.; Spijker, J.J.A.; Blanes Llorens, A.; Permanyer, I. Estimation of smoking-related mortality and its contribution to educational inequalities in life expectancy in Spain: An observational study, 2016–2019. BMJ Open 2022, 12, e059370. [Google Scholar] [CrossRef]
- Rao, K.P.; Nigussie, G.A.; Rao Koya, P. Modeling and Simulation Study of Population Subjected to the Smoking Habit. IOSR J. Math. 2016, 12, 56–63. [Google Scholar] [CrossRef]
- Brennan, P.; Crispo, A.; Zaridze, D.; Szeszenia-Dabrowska, N.; Rudnai, P.; Lissowska, J.; Fabianova, E.; Mates, D.; Bencko, V.; Foretova, L.; et al. High Cumulative Risk of Lung Cancer Death among Smokers and Nonsmokers in Central and Eastern Europe. Am. J. Epidemiol. 2006, 164, 1233–1241. [Google Scholar] [CrossRef]
- Singh, A.; Kamal, R.; Ahamed, I.; Wagh, M.; Bihari, V.; Sathian, B.; Kesavachandran, C.N. PAH exposure-associated lung cancer: An updated meta-analysis. Occup. Med. 2018, 68, 255–261. [Google Scholar] [CrossRef]
- Berrington de Gonzalez, A.; Hartge, P.; Cerhan, J.R.; Flint, A.J.; Hannan, L.; MacInnis, R.J.; Moore, S.C.; Tobias, G.S.; Anton-Culver, H.; Freeman, L.B.; et al. Body-Mass Index and Mortality among 1.46 Million White Adults. N. Engl. J. Med. 2010, 363, 2211–2219. [Google Scholar] [CrossRef] [PubMed]
- Jee, S.H.; Sull, J.W.; Park, J.; Lee, S.-Y.; Ohrr, H.; Guallar, E.; Samet, J.M. Body-Mass Index and Mortality in Korean Men and Women. N. Engl. J. Med. 2006, 355, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef]
- Ku, P.-W.; Steptoe, A.; Liao, Y.; Hsueh, M.-C.; Chen, L.-J. A cut-off of daily sedentary time and all-cause mortality in adults: A meta-regression analysis involving more than 1 million participants. BMC Med. 2018, 16, 74. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.R.; Galvão, L.L.; Meneguci, J.; Santos, D.d.A.T.; Virtuoso Júnior, J.S.; Tribess, S. Dynapenia in all-cause mortality and its relationship with sedentary behavior in community-dwelling older adults. Sport. Med. Heal. Sci. 2022. [Google Scholar] [CrossRef]
- Tiberi, M.; Piepoli, M.F. Regular physical activity only associated with low sedentary time increases survival in post myocardial infarction patient. Eur. J. Prev. Cardiol. 2019, 26, 94–96. [Google Scholar] [CrossRef]
- Schuler, G.; Adams, V.; Goto, Y. Role of exercise in the prevention of cardiovascular disease: Results, mechanisms, and new perspectives. Eur. Heart J. 2013, 34, 1790–1799. [Google Scholar] [CrossRef]
- Park, L.G.; Dracup, K.; Whooley, M.A.; McCulloch, C.; Lai, S.; Howie-Esquivel, J. Sedentary lifestyle associated with mortality in rural patients with heart failure. Eur. J. Cardiovasc. Nurs. 2019, 18, 318–324. [Google Scholar] [CrossRef]
- Vesely, D.L.; Overton, R.M.; Blankenship, M.; McCormick, M.T.; Schocken, D.D. Atrial Natriuretic Peptide Increases Urodilatin in the Circulation. Am. J. Nephrol. 1998, 18, 204–213. [Google Scholar] [CrossRef]
- Wen, C.P.; Wai, J.P.M.; Tsai, M.K.; Yang, Y.C.; Cheng, T.Y.D.; Lee, M.-C.; Chan, H.T.; Tsao, C.K.; Tsai, S.P.; Wu, X. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet 2011, 378, 1244–1253. [Google Scholar] [CrossRef]
- Belvederi Murri, M.; Folesani, F.; Zerbinati, L.; Nanni, M.G.; Ounalli, H.; Caruso, R.; Grassi, L. Physical Activity Promotes Health and Reduces Cardiovascular Mortality in Depressed Populations: A Literature Overview. Int. J. Environ. Res. Public Health 2020, 17, 5545. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Sheriff, H.; Kheirbek, R. Physical Inactivity and Mortality Risk. Cardiol. Res. Pract. 2011. [Google Scholar] [CrossRef] [PubMed]
- Rehm, J.; Gmel, G.; Sempos, C.T.; Trevisan, M. Alcohol-related morbidity and mortality. Alcohol Res. Heal. 2003, 27, 39. [Google Scholar]
- Saul, C.; Lange, S.; Probst, C. Employment Status and Alcohol-Attributable Mortality Risk—A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 7354. [Google Scholar] [CrossRef] [PubMed]
- Pechholdová, M.; Jasilionis, D. Contrasts in alcohol-related mortality in Czechia and Lithuania: Analysis of time trends and educational differences. Drug Alcohol Rev. 2020, 39, 846–856. [Google Scholar] [CrossRef]
- White, A.M.; Castle, I.P.; Hingson, R.W.; Powell, P.A. Using Death Certificates to Explore Changes in Alcohol-Related Mortality in the United States, 1999 to 2017. Alcohol. Clin. Exp. Res. 2020, 44, 178–187. [Google Scholar] [CrossRef]
- Probst, C.; Kilian, C.; Sanchez, S.; Lange, S.; Rehm, J. The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: A systematic review. Lancet Public Heal. 2020, 5, e324–e332. [Google Scholar] [CrossRef]
- De Marinis, M.G.; Piredda, M.; Petitti, T. Governance of Prevention in Spain. Biomed. Prev. 2018, 3, 226–229. [Google Scholar]
- Sanidad, M.d. Sistema de Cuentas de Salud; 2020. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/sisInfSanSNS/SCS.htm (accessed on 2 September 2022).
- European Commission. State of Health in the EU The Country Health Profile Series; European Commission: Brussels, Belgium, 2022. [Google Scholar]
- Moliné, E.B.; Ocaña Pérez De Tudela, C.; Carbó, S.; Ma, V.; Fernández, J.; Juan, S.; Ganuza, J.; Jesús, A.; Mora, R.; Torres, R. Cuadernos de Información Económica. Funcas 2022, 288, 1–112. [Google Scholar]
- CHRODIS, J.A. Joint Action on Chronic Diseases and Promoting Healthy Ageing Across the Life Cycle. Good Practice in the Field of Health Promotion and Primary Prevention. Spain Country Review; CHRODIS: Santander, Spain, 2014. [Google Scholar]
- Isaacs, S.L.; Schroeder, S.A. Class—The Ignored Determinant of the Nation’s Health. N. Engl. J. Med. 2004, 351, 1137–1142. [Google Scholar] [CrossRef]
- Kimmel, P.L.; Fwu, C.-W.; Eggers, P.W. Segregation, Income Disparities, and Survival in Hemodialysis Patients. J. Am. Soc. Nephrol. 2013, 24, 293–301. [Google Scholar] [CrossRef][Green Version]
- Nuru-Jeter, A.M.; LaVeist, T.A. Racial Segregation, Income Inequality, and Mortality in US Metropolitan Areas. J. Urban Heal. 2011, 88, 270–282. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, R.A.; Sen, S.; Mehta, K.; Moody-Ayers, S.; Bacchetti, P.; O’Hare, A.M. Geography Matters: Relationships among Urban Residential Segregation, Dialysis Facilities, and Patient Outcomes. Ann. Intern. Med. 2007, 146, 493. [Google Scholar] [CrossRef] [PubMed]
- Kimmel, P.L.; Fwu, C.-W.; Abbott, K.C.; Ratner, J.; Eggers, P.W. Racial disparities in poverty account for mortality differences in US medicare beneficiaries. SSM-Popul. Heal. 2016, 2, 123–129. [Google Scholar] [CrossRef]
- Baril, C.; Gascon, V.; Vadeboncoeur, D. Discrete-event simulation and design of experiments to study ambulatory patient waiting time in an emergency department. J. Oper. Res. Soc. 2019, 70, 2019–2038. [Google Scholar] [CrossRef]
- Golinelli, D.; Toscano, F.; Bucci, A.; Lenzi, J.; Fantini, M.P.; Nante, N.; Messina, G. Health Expenditure and All-Cause Mortality in the ‘Galaxy’ of Italian Regional Healthcare Systems: A 15-Year Panel Data Analysis. Appl. Health Econ. Health Policy 2017, 15, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Novignon, J.; Olakojo, S.A.; Nonvignon, J. The effects of public and private health care expenditure on health status in sub-Saharan Africa: New evidence from panel data analysis. Health Econ. Rev. 2012, 2, 22. [Google Scholar] [CrossRef] [PubMed]
- Rezapour, A.; Mousavi, A.; Lotfi, F.; Soleimani Movahed, M.; Alipour, S. The Effects of Health Expenditure on Health Outcomes Based on the Classification of Public Health Expenditure: A Panel Data Approach. Shiraz E-Med. J. 2019, 20. [Google Scholar] [CrossRef]
- Ministry of Health Sanidad en Datos; 2021. Available online: https://datos.gob.es/es/catalogo?publisher_display_name=Ministerio+de+Sanidad (accessed on 2 September 2022).
- Valls Martínez, M.d.C.; Ramírez-Orellana, A.; Grasso, M.S. Health Investment Management and Healthcare Quality in the Public System: A Gender Perspective. Int. J. Environ. Res. Public Health 2021, 18, 2304. [Google Scholar] [CrossRef]
- Santos-Jaén, J.M.; Valls Martínez, M.d.C.V.; Palacios-Manzano, M.; Grasso, M.S. Analysis of Patient Satisfaction through the Effect of Healthcare Spending on Waiting Times for Consultations and Operations. Healthcare 2022, 10, 1229. [Google Scholar] [CrossRef]
- Mazzanti, M.; Mazzarano, M.; Pronti, A.; Quatrosi, M. Fiscal policies, public investments and wellbeing: Mapping the evolution of the EU. Insights Into Reg. Dev. 2020, 2, 725–749. [Google Scholar] [CrossRef]
- Lopez I Casasnovas, G. Health care and cost containment in Spain. In Health Care and Cost Containment in the European Union; Mossialos, E., Le Grand, J., Eds.; Routledge: Aldershot, UK, 2019; pp. 547–572. ISBN 9780429426971. [Google Scholar]
- Ruangratanatrai, W.; Lertmaharit, S.; Hanvoravongchai, P. Equity in health personnel financing after Universal Coverage: Evidence from Thai Ministry of Public Health’s hospitals from 2008–2012. Hum. Resour. Health 2015, 13, 59. [Google Scholar] [CrossRef] [PubMed]
- Muthui, J.N.; Kosimbei, G.; Maingi, J.; Thuku, G.K. The impact of public expenditure components on economic growth in Kenya 1964–2011. Int. J. Bus. Soc. Sci. 2013, 4, 233–253. [Google Scholar]
- Feyisa, D.; Yitbarek, K.; Daba, T. Cost of provision of essential health Services in Public Health Centers of Jimma zone, Southwest Ethiopia; a provider perspective, the pointer for major area of public expenditure. Health Econ. Rev. 2021, 11, 34. [Google Scholar] [CrossRef] [PubMed]
- Vogt, T.C.; Kluge, F.A. Can public spending reduce mortality disparities? Findings from East Germany after reunification. J. Econ. Ageing 2015, 5, 7–13. [Google Scholar] [CrossRef]
- Edney, L.C.; Haji Ali Afzali, H.; Cheng, T.C.; Karnon, J. Mortality reductions from marginal increases in public spending on health. Health Policy 2018, 122, 892–899. [Google Scholar] [CrossRef] [PubMed]
- National Statistical Institute. Defunciones; National Statistical Institute: Sofia, Bulgaria, 2022. [Google Scholar]
- Indicadores Clave del Sistema Nacional de Salud. Available online: http://inclasns.msssi.es/main.html (accessed on 7 May 2022).
- Sarstedt, M.; Hair, J.F.; Ringle, C.M.; Thiele, K.O.; Gudergan, S.P. Estimation issues with PLS and CBSEM: Where the bias lies! J. Bus. Res. 2016, 69, 3998–4010. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage Publications: New York, NY, USA, 2016; ISBN 1483377431. [Google Scholar]
- Ramírez-Orellana, A.; del Carmen Valls Martínez, M.; Grasso, M.S. Using Higher-Order Constructs to Estimate Health-Disease Status: The Effect of Health System Performance and Sustainability. Mathematics 2021, 9, 1228. [Google Scholar] [CrossRef]
- INE INEbase/Sociedad/Salud/Estadística de Defunciones Según la Causa de Muerte/Últimos Datos. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176780&menu=ultiDatos&idp=1254735573175 (accessed on 5 September 2022).
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a silver bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Chin, W.W.; Dibbern, J. Handbook of Partial Least Squares; Sprionger: Berlin/Heidelberg, Germany, 2010; pp. 171–193. [Google Scholar] [CrossRef]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Ringle, C.M.; Sarstedt, M.; Mitchell, R.; Gudergan, S.P. Partial least squares structural equation modeling in HRM research. Int. J. Hum. Resour. Manag. 2020, 31, 1617–1643. [Google Scholar] [CrossRef]
- Yusif, S.; Hafeez-Baig, A.; Soar, J.; Teik, D.O.L. PLS-SEM path analysis to determine the predictive relevance of e-Health readiness assessment model. Health Technol. 2020, 10, 1497–1513. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, V.G. Partial least squares structural equation modeling (PLS-SEM): An emerging tool in business research. Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- León-Gómez, A.; Santos-Jaén, J.M.; Ruiz-Palomo, D.; Palacios-Manzano, M. Disentangling the impact of ICT adoption on SMEs performance: The mediating roles of corpo-rate social responsibility and innovation. Oeconomia Copernic. 2022, 13, 831–866. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R.; Classroom Companion: Business; Springer International Publishing: Cham, Switzerland, 2021; ISBN 978-3-030-80518-0. [Google Scholar]
- Martínez Ávila, M.; Fierro Moreno, E. Aplicación de la Técnica PLS-SEM en la Gestión del Conocimiento: Un Enfoque Técnico Práctico/Application of the PLS-SEM Technique in Knowledge Management: A Practical Technical Approach; 2018; Volume 8; ISBN 0000000243971. Available online: https://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S2007-74672018000100130 (accessed on 2 September 2022).
- Lowry, P.B.; Gaskin, J. Partial least squares (PLS) structural equation modeling (SEM) for building and testing behavioral causal theory: When to choose it and how to use it. IEEE Trans. Prof. Commun. 2014, 57, 123–146. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 2nd ed.; Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Palacios-Manzano, M.; Leon-Gomez, A.; Santos-Jaen, J.M. Corporate Social Responsibility as a Vehicle for Ensuring the Survival of Construction SMEs. The Mediating Role of Job Satisfaction and Innovation. IEEE Trans. Eng. Manag. 2021, 1–14. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988; Available online: https://www.taylorfrancis.com/books/mono/10.4324/9780203771587/statistical-power-analysis-behavioral-sciences-jacob-cohen (accessed on 2 September 2022).
- Mayr, S.; Erdfelder, E.; Buchner, A.; Faul, F. A short tutorial of GPower. Tutor. Quant. Methods Psychol. 2007, 3, 51–59. [Google Scholar] [CrossRef]
- Ringle, C.M.; Wende, S.; Becker, J.-M. SmartPLS 3; SmartPLS GmbH: Boenningstedt, Germany, 2015. [Google Scholar]
- Cepeda-Carrion, G.; Cegarra-Navarro, J.G.; Cillo, V. Tips to use partial least squares structural equation modelling (PLS-SEM) in knowledge management. J. Knowl. Manag. 2019, 23, 67–89. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M. Rethinking some of the rethinking of partial least squares. Eur. J. Mark. 2019, 53, 566–584. [Google Scholar] [CrossRef]
- García-Machado, J.J.; Sroka, W.; Nowak, M. R&D and Innovation Collaboration between Universities and Business—A PLS-SEM Model for the Spanish Province of Huelva. Adm. Sci. 2021, 11, 83. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Gudergan, S.P. Advanced Issues in Partial Least Squares Structural Equation Modeling; Sage Publications Sage CA: Los Angeles, CA, USA, 2017; ISBN 1483377385. [Google Scholar]
- Tenenhaus, M.; Vinzi, V.E.; Chatelin, Y.M.; Lauro, C. PLS path modeling. Comput. Stat. Data Anal. 2005, 48, 159–205. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. Testing measurement invariance of composites using partial least squares. Int. Mark. Rev. 2016, 33, 405–431. [Google Scholar] [CrossRef]
- Hu, L.-T.; Bentler, P.M. Fit indices sensitivity to misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Henseler, J.; Dijkstra, T.K.; Sarstedt, M.; Ringle, C.M.; Diamantopoulos, A.; Straub, D.W.; Ketchen, D.J.; Hair, J.F.; Hult, G.T.M.; Calantone, R.J. Common Beliefs and Reality About PLS: Comments on Rönkkö and Evermann (2013). Organ. Res. Methods 2014, 17, 182–209. [Google Scholar] [CrossRef]
- Hair, J.F.; Astrachan, C.B.; Moisescu, O.I.; Radomir, L.; Sarstedt, M.; Vaithilingam, S.; Ringle, C.M. Executing and interpreting applications of PLS-SEM: Updates for family business researchers. J. Fam. Bus. Strateg. 2021, 12, 100392. [Google Scholar] [CrossRef]
- Chin, W.W. How to Write Up and Report PLS Analyses. In Handbook of Partial Least Squares; Springer: Berlin/Heidelberg, Germany, 2010; pp. 655–690. [Google Scholar]
- Ali, I.; Ali, M.; Leal-Rodríguez, A.L.; Albort-Morant, G. The role of knowledge spillovers and cultural intelligence in enhancing expatriate employees’ individual and team creativity. J. Bus. Res. 2019, 101, 561–573. [Google Scholar] [CrossRef]
- Conrad, D.A.; Perry, L. Quality-Based Financial Incentives in Health Care: Can We Improve Quality by Paying for It? Annu. Rev. Public Health 2009, 30, 357–371. [Google Scholar] [CrossRef]



| EXPENDITURE | |
| EXP_1 | Health expenditure (public) per capita |
| RESOURCES | |
| RES_1 | Specialist doctors per 1000 inhabitants |
| RES_2 | Operating rooms per 1000 inhabitants |
| RES_3 | Nuclear Magnetic Resonance Equipment per 1000 inhabitants |
| RES_4 | CT equipment per 1000 inhabitants |
| RES_5 | Hemodialysis equipment per 1000 inhabitants |
| RES_6 | Hemodynamic equipment per 1000 inhabitants |
| RES_7 | Day hospital places per 1000 inhabitants |
| UNHEALTHY HABITS | |
| BH_1 | Tobacco (percentage of smokers) |
| BH_2 | Alcohol (percentage of at-risk drinkers) |
| BH_3 | Inactivity in leisure time (prevalence of sedentary behavior among the adult population) |
| MORTALITY | |
| MOR_1 | Ischemic heart disease mortality rate |
| MOR_2 | Cerebrovascular disease mortality rate |
| MOR_3 | Cancer mortality rate |
| MOR_4 | Chronic liver disease mortality rate |
| MOR_5 | Chronic obstructive pulmonary disease mortality rate |
| MOR_6 | Pneumonia and influenza mortality rate |
| POVERTY | |
| POV_1 | Poverty rate |
| TOTAL | Mean | SD | Loading | t-Student * | Q2 | α | ρA | ρC | AVE |
|---|---|---|---|---|---|---|---|---|---|
| EXPENDITURE | |||||||||
| EXP_01 | 1409.669 | 238.477 | 1.000 | 24.486 | |||||
| RESOURCES | 0.144 | 0.816 | 0.845 | 0.861 | 0.575 | ||||
| RES_1 | 1.806 | 0.296 | 0.702 | 14.582 | 0.298 | ||||
| RES_2 | 8.952 | 1.299 | 0.645 | 8.793 | 0.062 | ||||
| RES_3 | 0.996 | 0.416 | 0.854 | 40.140 | 0.192 | ||||
| RES_4 | 1.556 | 0.307 | 0.801 | 21.929 | 0.235 | ||||
| RES_5 | 9.713 | 3.752 | 0.567 | 7.787 | 0.050 | ||||
| RES_6 | 0.458 | 0.169 | 0.604 | 9.565 | 0.029 | ||||
| RES_7 | 0.305 | 0.183 | 0.601 | 9.119 | 0.143 | ||||
| UNHEALTHY HABITS | 0.702 | 0.734 | 0.742 | 0.510 | |||||
| BH_01 | 25.041 | 4.023 | 0.904 | 64.242 | |||||
| BH_02 | 2.394 | 1.455 | 0.416 | 5.584 | |||||
| BH_03 | 42.078 | 9.783 | 0.735 | 12.103 | |||||
| MORTALITY | 0.472 | 0.889 | 0.918 | 0.920 | 0.666 | ||||
| MOR_01 | 83.22 | 27.93 | 0.932 | 74.098 | 0.606 | ||||
| MOR_02 | 74.828 | 27.619 | 0.906 | 66.703 | 0.723 | ||||
| MOR_03 | 247.431 | 21.083 | 0.822 | 32.854 | 0.446 | ||||
| MOR_04 | 10.558 | 3.309 | 0.806 | 20.891 | 0.309 | ||||
| MOR_05 | 35.769 | 9.277 | 0.873 | 40.198 | 0.536 | ||||
| MOR_06 | 21.369 | 6.243 | 0.465 | 6.163 | 0.214 | ||||
| POVERTY | |||||||||
| POV_01 | 20.109 | 6.611 | 1.000 | 16.783 | |||||
| I | II | III | IV | V | ||
|---|---|---|---|---|---|---|
| I | EXPENDITURES | 1.000 | 0.605 | 0.715 | 0.622 | 0.088 |
| II | RESOURCES | 0.587 | 0.889 | 0.526 | 0.820 | 0.299 |
| III | UNHEALTHY HABITS | −0.542 | −0.790 | 0.814 | 0.634 | 0.288 |
| IV | MORTALITY | −0.588 | −0.719 | 0.734 | 0.816 | 0.264 |
| V | POVERTY | −0.088 | −0.213 | 0.139 | 0.209 | 1.000 |
| TOTAL | Path | SD | T-Value | f2 | 95CI | VIF | H | Supported |
|---|---|---|---|---|---|---|---|---|
| Direct effects | ||||||||
| Unhealthy habits -> Mortality | 0.618 | 0.074 | 8.370 *** | 0.554 | [0.487; −0.729] | 2.682 | H1 | Yes |
| Expenditure -> Resources | 0.587 | 0.053 | 11.153 *** | 0.527 | [0.488; −0.663] | 1.000 | H2 | Yes |
| Resources -> Mortality | −0.268 | 0.070 | 3.808 *** | 0.102 | [−0.386; −0.158] | 2.748 | H3 | Yes |
| Control variable paths | ||||||||
| Poverty -> Mortality | 0.083 | 0.037 | 2.275 ** | 0.025 | [0.025; 0.146] | 1.075 | H4 | Yes |
| Indirect effects | ||||||||
| Moderating effects | ||||||||
| Resources x Unhealthy habits -> Mortality | −0.107 | 0.042 | 2.563 ** | 0.042 | [−0.173; −0.036] | 1.030 | H5 | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos-Jaén, J.M.; León-Gómez, A.; Valls Martínez, M.d.C.; Gimeno-Arias, F. The Effect of Public Healthcare Expenditure on the Reduction in Mortality Rates Caused by Unhealthy Habits among the Population. Healthcare 2022, 10, 2253. https://doi.org/10.3390/healthcare10112253
Santos-Jaén JM, León-Gómez A, Valls Martínez MdC, Gimeno-Arias F. The Effect of Public Healthcare Expenditure on the Reduction in Mortality Rates Caused by Unhealthy Habits among the Population. Healthcare. 2022; 10(11):2253. https://doi.org/10.3390/healthcare10112253
Chicago/Turabian StyleSantos-Jaén, José Manuel, Ana León-Gómez, María del Carmen Valls Martínez, and Fernando Gimeno-Arias. 2022. "The Effect of Public Healthcare Expenditure on the Reduction in Mortality Rates Caused by Unhealthy Habits among the Population" Healthcare 10, no. 11: 2253. https://doi.org/10.3390/healthcare10112253
APA StyleSantos-Jaén, J. M., León-Gómez, A., Valls Martínez, M. d. C., & Gimeno-Arias, F. (2022). The Effect of Public Healthcare Expenditure on the Reduction in Mortality Rates Caused by Unhealthy Habits among the Population. Healthcare, 10(11), 2253. https://doi.org/10.3390/healthcare10112253








