A Case of Oral Health Management for a Patient with Extensive Ulceration of the Oral Mucosa Due to Herpes Zoster
Abstract
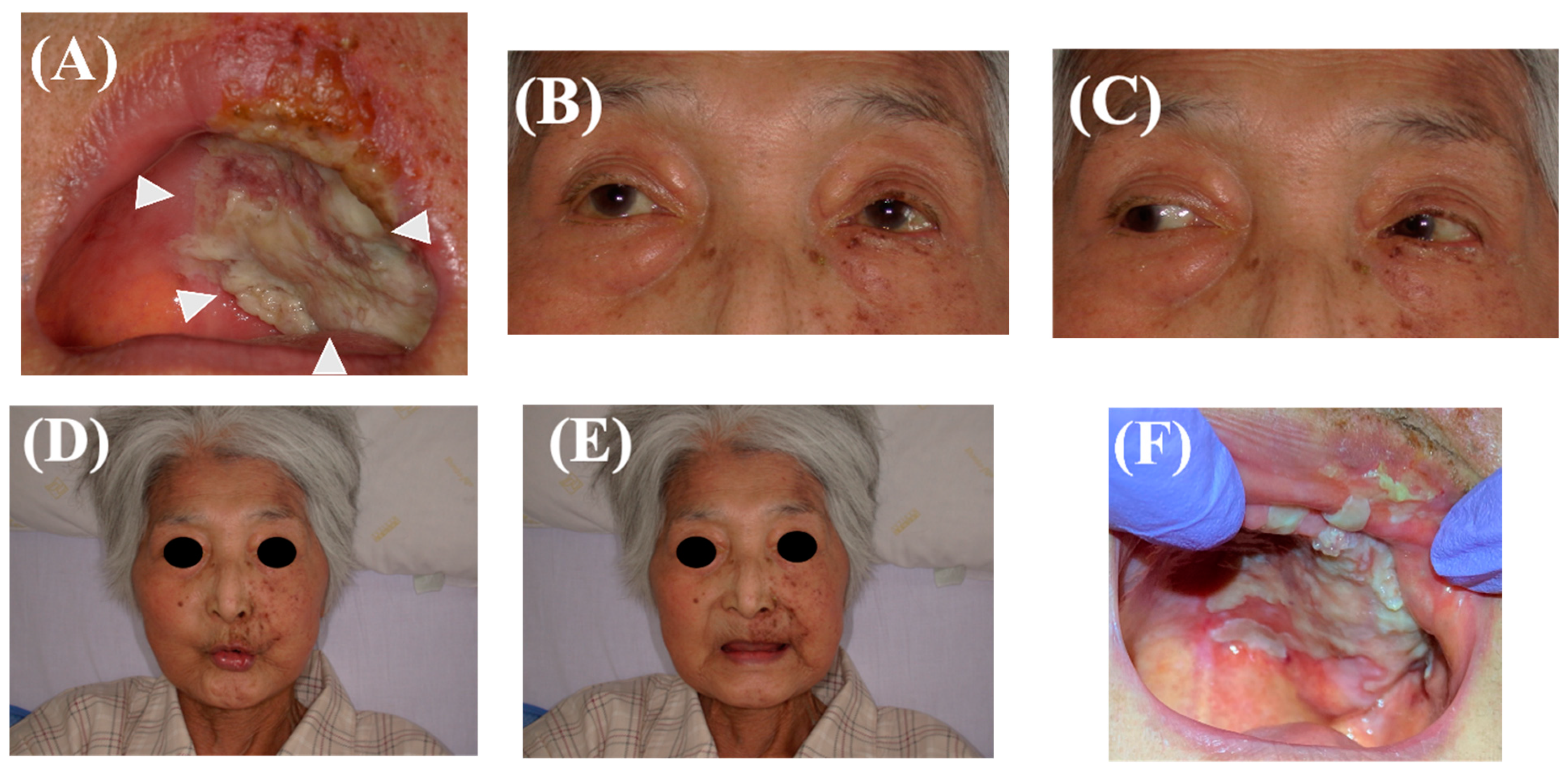
1. Introduction
2. Case Presentation
2.1. Case History
2.2. Initial Oral Evaluation
2.3. Oral Hygiene Management
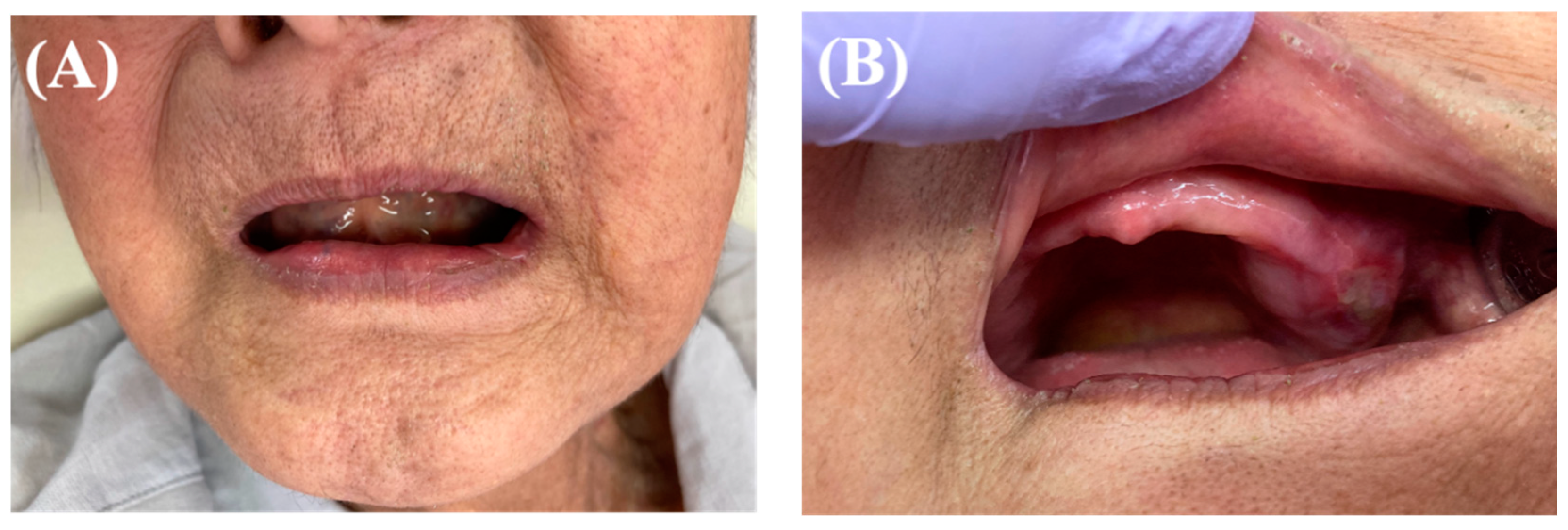
2.4. Follow-Up after Discharge
2.5. Treatment Result
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sadaksharam, J.; Kathiresan, I. Palatal fibroma in a geriatric patient: A rarity. Indian J. Med. Res. 2020, 152, S27–S28. [Google Scholar] [CrossRef] [PubMed]
- Bharti, V.; Singh, J. Capillary hemangioma of palatal mucosa. J. Indian Soc. Periodontol. 2012, 16, 475–478. [Google Scholar] [CrossRef] [PubMed]
- Aboh, I.V.; Chisci, G.; Salini, C.; Gennaro, P.; Cascino, F.; Gabriele, G.; Iannetti, G. Submandibular ossifying lipoma. J. Craniofac. Surg. 2015, 26, 973–974. [Google Scholar] [CrossRef] [PubMed]
- Orenuga, O.O.; Oluwo, A.; Oluwakuyide, R.T.; Olawuyi, A.B. Recurrent oral squamous papilloma in a pediatric patient: Case report and review of the literature. Niger J. Clin. Pract. 2018, 21, 1674–1677. [Google Scholar] [CrossRef]
- Aboh, I.V.; Chisci, G.; Cascino, F.; Parigi, S.; Gennaro, P.; Gabriele, G.; Iannetti, G. Giant palatal schwannoma. J. Craniofac. Surg. 2014, 25, e418–e420. [Google Scholar] [CrossRef]
- Pappas, D.A.; Hooper, M.M.; Kremer, J.M.; Reed, G.; Shan, Y.; Wenkert, D.; Greenberg, J.D.; Curtis, J.R. Herpes Zoster Reactivation in Patients With Rheumatoid Arthritis: Analysis of Disease Characteristics and Disease-Modifying Antirheumatic Drugs. Arthritis Care Res. 2015, 67, 1671–1678. [Google Scholar] [CrossRef]
- Nair, P.; Gharote, H.; Singh, P.; Jain-Choudhary, P. Herpes zoster on the face in the elderly. BMJ Case Rep. 2014, 2014, bcr2013200101. [Google Scholar] [CrossRef]
- Schmader, K. Herpes Zoster. Ann. Intern. Med. 2018, 169, ITC19–ITC31. [Google Scholar] [CrossRef]
- Toyama, N.; Shiraki, K.; Society of the Miyazaki Prefecture, D. Epidemiology of herpes zoster and its relationship to varicella in Japan: A 10-year survey of 48,388 herpes zoster cases in Miyazaki prefecture. J. Med. Virol. 2009, 81, 2053–2058. [Google Scholar] [CrossRef]
- Decroix, J.; Partsch, H.; Gonzalez, R.; Mobacken, H.; Goh, C.L.; Walsh, L.; Shukla, S.; Naisbett, B. Factors influencing pain outcome in herpes zoster: An observational study with valaciclovir. Valaciclovir International Zoster Assessment Group (VIZA). J. Eur. Acad. Dermatol. Venereol. 2000, 14, 23–33. [Google Scholar] [CrossRef]
- Koshy, E.; Mengting, L.; Kumar, H.; Jianbo, W. Epidemiology, treatment and prevention of herpes zoster: A comprehensive review. Indian J. Dermatol. Venereol. Leprol. 2018, 84, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Freites-Martinez, A.; Santana, N.; Arias-Santiago, S.; Viera, A. Using the Common Terminology Criteria for Adverse Events (CTCAE—Version 5.0) to Evaluate the Severity of Adverse Events of Anticancer Therapies. Actas Dermosifiliogr. 2021, 112, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Kakuta, R.; Okata, U.; Funakoshi, T.; Fujio, Y.; Inoue, N.; Takahashi, S.; Amagai, M.; Ohyama, M. Unusually extensive disseminated herpes zoster with multiple ulcer formation in a methotrexate-treated rheumatoid arthritis patient. J. Dermatol. 2014, 41, 181–182. [Google Scholar] [CrossRef]
- Kolokotronis, A.; Louloudiadis, K.; Fotiou, G.; Matiais, A. Oral manifestations of infections of infections due to varicella zoster virus in otherwise healthy children. J. Clin. Pediatr. Dent. 2001, 25, 107–112. [Google Scholar] [CrossRef]
- Elad, S.; Cheng, K.K.F.; Lalla, R.V.; Yarom, N.; Hong, C.; Logan, R.M.; Bowen, J.; Gibson, R.; Saunders, D.P.; Zadik, Y.; et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 2020, 126, 4423–4431. [Google Scholar] [CrossRef] [PubMed]
- Kiyomi, A.; Yoshida, K.; Arai, C.; Usuki, R.; Yamazaki, K.; Hoshino, N.; Kurokawa, A.; Imai, S.; Suzuki, N.; Toyama, A.; et al. Salivary inflammatory mediators as biomarkers for oral mucositis and oral mucosal dryness in cancer patients: A pilot study. PLoS ONE 2022, 17, e0267092. [Google Scholar] [CrossRef] [PubMed]
- Patil, A.; Goldust, M.; Wollina, U. Herpes zoster: A Review of Clinical Manifestations and Management. Viruses 2022, 14, 192. [Google Scholar] [CrossRef] [PubMed]
- Sio, T.T.; Le-Rademacher, J.G.; Leenstra, J.L.; Loprinzi, C.L.; Rine, G.; Curtis, A.; Singh, A.K.; Martenson, J.A., Jr.; Novotny, P.J.; Tan, A.D.; et al. Effect of Doxepin Mouthwash or Diphenhydramine-Lidocaine-Antacid Mouthwash vs Placebo on Radiotherapy-Related Oral Mucositis Pain: The Alliance A221304 Randomized Clinical Trial. JAMA 2019, 321, 1481–1490. [Google Scholar] [CrossRef]
- Ueno, T.; Yatsuoka, W.; Ishiki, H.; Miyano, K.; Uezono, Y. Effects of an oral mucosa protective formulation on chemotherapy- and/or radiotherapy-induced oral mucositis: A prospective study. BMC Cancer 2022, 22, 90. [Google Scholar] [CrossRef]
- Ogata, J.; Minami, K.; Horishita, T.; Shiraishi, M.; Okamoto, T.; Terada, T.; Sata, T. Gargling with sodium azulene sulfonate reduces the postoperative sore throat after intubation of the trachea. Anesth. Analg. 2005, 101, 290–293. [Google Scholar] [CrossRef]
- Keefe, D.M.; Schubert, M.M.; Elting, L.S.; Sonis, S.T.; Epstein, J.B.; Raber-Durlacher, J.E.; Migliorati, C.A.; McGuire, D.B.; Hutchins, R.D.; Peterson, D.E.; et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer 2007, 109, 820–831. [Google Scholar] [CrossRef] [PubMed]
- Sekiya, H.; Kurasawa, Y.; Kaneko, K.; Takahashi, K.I.; Maruoka, Y.; Michiwaki, Y.; Takeda, Y.; Ochiai, R. Preventive Effects of Sustainable and Developmental Perioperative Oral Management Using the "Oral Triage" System on Postoperative Pneumonia after Cancer Surgery. Int. J. Environ. Res. Public Health 2021, 18, 6296. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsuda, Y.; Mizuno, R.; Miyajima, S.; Arakawa, S.; Kabasawa, Y. A Case of Oral Health Management for a Patient with Extensive Ulceration of the Oral Mucosa Due to Herpes Zoster. Healthcare 2022, 10, 2249. https://doi.org/10.3390/healthcare10112249
Matsuda Y, Mizuno R, Miyajima S, Arakawa S, Kabasawa Y. A Case of Oral Health Management for a Patient with Extensive Ulceration of the Oral Mucosa Due to Herpes Zoster. Healthcare. 2022; 10(11):2249. https://doi.org/10.3390/healthcare10112249
Chicago/Turabian StyleMatsuda, Yuhei, Ruriko Mizuno, Saki Miyajima, Shinichi Arakawa, and Yuji Kabasawa. 2022. "A Case of Oral Health Management for a Patient with Extensive Ulceration of the Oral Mucosa Due to Herpes Zoster" Healthcare 10, no. 11: 2249. https://doi.org/10.3390/healthcare10112249
APA StyleMatsuda, Y., Mizuno, R., Miyajima, S., Arakawa, S., & Kabasawa, Y. (2022). A Case of Oral Health Management for a Patient with Extensive Ulceration of the Oral Mucosa Due to Herpes Zoster. Healthcare, 10(11), 2249. https://doi.org/10.3390/healthcare10112249





