Different Effects of Perceived Social Support on the Relationship between Perceived Stress and Depression among University Students with Borderline Personality Disorder Symptoms: A Multigroup Mediation Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Calculation
2.3. Participants and Setting
2.4. Measurements
2.4.1. Screening Instrument for BPD (SI-Bord)
2.4.2. 10-Item Perceived Stress Scale (PSS-10)
2.4.3. Revised Thai Multi-Dimensional Scales of Perceived Social Support (r-MSPSS)
2.4.4. Patient-Health Questionaire-9 (PHQ-9)
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Implications and Future Research
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Depression. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 30 January 2022).
- El Ansari, W.; Vallentin-Holbech, L.; Stock, C. Predictors of illicit drug/s use among university students in Northern Ireland, Wales and England. Glob. J. Health Sci. 2014, 7, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Yagmaee, F. Eight Weeks of Aerobic Exercise and Prescribed Diet (Low in Carbohydrate and High Protein) Improve Mental Health in Obese Women. Int. J. Sport Stud. Health 2021, 4, e121345. [Google Scholar] [CrossRef]
- Masoomi, H.; Taheri, M.; Irandoust, K.; H’Mida, C.; Chtourou, H. The relationship of breakfast and snack foods with cognitive and academic performance and physical activity levels of adolescent students. Biol. Rhythm Res. 2020, 51, 481–488. [Google Scholar] [CrossRef]
- Banerjee, Y.; Akhras, A.; Khamis, A.H.; Alsheikh-Ali, A.; Davis, D. Investigating the Relationship between Resilience, Stress-Coping Strategies, and Learning Approaches to Predict Academic Performance in Undergraduate Medical Students: Protocol for a Proof-of-Concept Study. JMIR Res. Protoc. 2019, 8, e14677. [Google Scholar] [CrossRef]
- Tosevski, D.L.; Milovancevic, M.P.; Gajic, S.D. Personality and psychopathology of university students. Curr. Opin. Psychiatry 2010, 23, 48–52. [Google Scholar] [CrossRef]
- Wongpakaran, T.; Wongpakaran, N.; Pinyopornpanish, M.; Srisutasanavong, U.; Lueboonthavatchai, P.; Nivataphand, R.; Apisiridej, N.; Petchsuwan, D.; Saisavoey, N.; Wannarit, K.; et al. Baseline characteristics of depressive disorders in Thai outpatients: Findings from the Thai Study of Affective Disorders. Neuropsychiatr. Dis. Treat 2014, 10, 217–223. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Çelik, N.; Ceylan, B.; Ünsal, A.; Çağan, Ö. Depression in health college students: Relationship factors and sleep quality. Psychol. Health Med. 2019, 24, 625–630. [Google Scholar] [CrossRef]
- Li, L.; Lok, G.K.I.; Mei, S.L.; Cui, X.L.; An, F.R.; Cheung, T.; Ungvari, G.S.; Xiang, Y.T. Prevalence of depression and its relationship with quality of life among university students in Macau, Hong Kong and mainland China. Sci. Rep. 2020, 10, 15798. [Google Scholar] [CrossRef]
- Ibrahim, A.K.; Kelly, S.J.; Adams, C.E.; Glazebrook, C. A systematic review of studies of depression prevalence in university students. J. Psychiatr. Res. 2013, 47, 391–400. [Google Scholar] [CrossRef]
- Akhtar, P.; Ma, L.; Waqas, A.; Naveed, S.; Li, Y.; Rahman, A.; Wang, Y. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 2020, 274, 911–919. [Google Scholar] [CrossRef]
- Crispim, M.O.; Santos, C.; Frazão, I.D.S.; Frazão, C.; Albuquerque, R.C.R.; Perrelli, J.G.A. Prevalence of suicidal behavior in young university students: A systematic review with meta-analysis. Rev. Lat. Am. Enferm. 2021, 29, e3495. [Google Scholar] [CrossRef] [PubMed]
- Rotenstein, L.S.; Ramos, M.A.; Torre, M.; Segal, J.B.; Peluso, M.J.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation among Medical Students: A Systematic Review and Meta-Analysis. JAMA 2016, 316, 2214–2236. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.H.; Hsiao, R.C.; Liu, T.L.; Yen, C.F. Predicting effects of borderline personality symptoms and self-concept and identity disturbances on internet addiction, depression, and suicidality in college students: A prospective study. Kaohsiung J. Med. Sci. 2019, 35, 508–514. [Google Scholar] [CrossRef]
- Dalbudak, E.; Evren, C.; Aldemir, S.; Evren, B. The severity of Internet addiction risk and its relationship with the severity of borderline personality features, childhood traumas, dissociative experiences, depression and anxiety symptoms among Turkish university students. Psychiatry Res. 2014, 219, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Wongpakaran, N.; Oon-Arom, A.; Karawekpanyawong, N.; Lohanan, T.; Leesawat, T.; Wongpakaran, T. Borderline Personality Symptoms: What Not to Be Overlooked When Approaching Suicidal Ideation among University Students. Healthcare 2021, 9, 1399. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T.; Kittipodjanasit, A.; Chompoosri, P.; Kuntawong, P.; Wedding, D. Predictive factors for suicidal attempts: A case-control study. Perspect. Psychiatr. Care 2019, 55, 667–672. [Google Scholar] [CrossRef]
- Ball, J.S.; Links, P.S. Borderline personality disorder and childhood trauma: Evidence for a causal relationship. Curr. Psychiatry Rep. 2009, 11, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Broadbear, J. Borderline personality disorder and depressive disorder. Australas. Psychiatry 2019, 27, 573–577. [Google Scholar] [CrossRef]
- Weinberg, A.; Klonsky, E.D.; Hajcak, G. Autonomic impairment in borderline personality disorder: A laboratory investigation. Brain Cogn. 2009, 71, 279–286. [Google Scholar] [CrossRef]
- Koenig, J.; Kemp, A.H.; Feeling, N.R.; Thayer, J.F.; Kaess, M. Resting state vagal tone in borderline personality disorder: A meta-analysis. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2016, 64, 18–26. [Google Scholar] [CrossRef]
- Duesenberg, M.; Wolf, O.T.; Metz, S.; Roepke, S.; Fleischer, J.; Elias, V.; Renneberg, B.; Otte, C.; Wingenfeld, K. Psychophysiological stress response and memory in borderline personality disorder. Eur. J. Psychotraumatol. 2019, 10, 1568134. [Google Scholar] [CrossRef] [PubMed]
- Rausch, J.; Flach, E.; Panizza, A.; Brunner, R.; Herpertz, S.C.; Kaess, M.; Bertsch, K. Associations between age and cortisol awakening response in patients with borderline personality disorder. J. Neural Transm. 2021, 128, 1425–1432. [Google Scholar] [CrossRef] [PubMed]
- Banjongrewadee, M.; Wongpakaran, N.; Wongpakaran, T.; Pipanmekaporn, T.; Punjasawadwong, Y.; Mueankwan, S. The role of perceived stress and cognitive function on the relationship between neuroticism and depression among the elderly: A structural equation model approach. BMC Psychiatry 2020, 20, 25. [Google Scholar] [CrossRef] [PubMed]
- Candrian, M.; Schwartz, F.; Farabaugh, A.; Perlis, R.H.; Ehlert, U.; Fava, M. Personality disorders and perceived stress in major depressive disorder. Psychiatry Res. 2008, 160, 184–191. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Guo, S.-E. Stress, perceived support, resourcefulness and depressive symptoms in Taiwanese adolescents. J. Clin. Nurs. 2009, 18, 3271–3279. [Google Scholar] [CrossRef]
- Heinen, I.; Bullinger, M.; Kocalevent, R.D. Perceived stress in first year medical students—Associations with personal resources and emotional distress. BMC Med. Educ. 2017, 17, 4. [Google Scholar] [CrossRef]
- Karyotaki, E.; Cuijpers, P.; Albor, Y.; Alonso, J.; Auerbach, R.P.; Bantjes, J.; Bruffaerts, R.; Ebert, D.D.; Hasking, P.; Kiekens, G.; et al. Sources of Stress and Their Associations with Mental Disorders among College Students: Results of the World Health Organization World Mental Health Surveys International College Student Initiative. Front. Psychol. 2020, 11, 1759. [Google Scholar] [CrossRef]
- Racic, M.; Todorovic, R.; Ivkovic, N.; Masic, S.; Joksimovic, B.; Kulic, M. Self-Perceived Stress in Relation to Anxiety, Depression and Health-related Quality of Life among Health Professions Students: A Cross-sectional Study from Bosnia and Herzegovina. Slov. J. Public Health 2017, 56, 251–259. [Google Scholar] [CrossRef]
- Worku, D.; Dirriba, A.B.; Wordofa, B.; Fetensa, G. Perceived Stress, Depression, and Associated Factors among Undergraduate Health Science Students at Arsi University in 2019 in Oromia, Ethiopia. Psychiatry J. 2020, 2020, 4956234. [Google Scholar] [CrossRef]
- Dunkley, D.M.; Lewkowski, M.; Lee, I.A.; Preacher, K.J.; Zuroff, D.C.; Berg, J.L.; Foley, J.E.; Myhr, G.; Westreich, R. Daily Stress, Coping, and Negative and Positive Affect in Depression: Complex Trigger and Maintenance Patterns. Behav. Ther. 2017, 48, 349–365. [Google Scholar] [CrossRef]
- Lee, C.S.; Goldstein, S.E.; Dik, B.J.; Rodas, J.M. Sources of social support and gender in perceived stress and individual adjustment among Latina/o college-attending emerging adults. Cult. Divers. Ethn. Minor. Psychol. 2020, 26, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef] [PubMed]
- Hupcey, J.E. Clarifying the social support theory-research linkage. J. Adv. Nurs. 1998, 27, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
- Mackin, D.M.; Perlman, G.; Davila, J.; Kotov, R.; Klein, D.N. Social support buffers the effect of interpersonal life stress on suicidal ideation and self-injury during adolescence. Psychol. Med. 2017, 47, 1149–1161. [Google Scholar] [CrossRef] [PubMed]
- Zerach, G.; Elklit, A. Attachment and social support mediate associations between Polyvictimization and psychological distress in early adolescence. Int. J. Psychol. 2020, 55, 380–391. [Google Scholar] [CrossRef]
- Nazzal, F.I.; Cruz, O.; Neto, F. Psychological predictors of loneliness among Palestinian university students in the West Bank. Transcult. Psychiatry 2020, 57, 688–697. [Google Scholar] [CrossRef]
- Dong, Y.; Li, H. The relationship between social support and depressive symptoms among the college students of Liaoning, China: A moderated mediated analysis. Psychol. Health Med. 2020, 25, 368–378. [Google Scholar] [CrossRef]
- Jibeen, T. Perceived Social Support and Mental Health Problems among Pakistani University Students. Community Ment. Health J. 2016, 52, 1004–1008. [Google Scholar] [CrossRef] [PubMed]
- Khallad, Y.; Jabr, F. Effects of perceived social support and family demands on college students’ mental well-being: A cross-cultural investigation. Int. J. Psychol. 2016, 51, 348–355. [Google Scholar] [CrossRef]
- Adams, T.R.; Rabin, L.A.; Da Silva, V.G.; Katz, M.J.; Fogel, J.; Lipton, R.B. Social Support Buffers the Impact of Depressive Symptoms on Life Satisfaction in Old Age. Clin. Gerontol. 2016, 39, 139–157. [Google Scholar] [CrossRef]
- Choi, N.G.; Ha, J.H. Relationship between spouse/partner support and depressive symptoms in older adults: Gender difference. Aging Ment. Health 2011, 15, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Hadebe, N.F.; Ramukumba, T.S. Resilience and social support of young adults living with mental illness in the city of Tshwane, Gauteng province, South Africa. Curationis 2020, 43, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Harrison, K.E.; Dombrovski, A.Y.; Morse, J.Q.; Houck, P.; Schlernitzauer, M.; Reynolds, C.F.; Szanto, K. Alone? Perceived social support and chronic interpersonal difficulties in suicidal elders. Int. Psychogeriatr. 2010, 22, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Thadani, B.; Pérez-García, A.M.; Bermúdez, J. Functional Impairment in Borderline Personality Disorder: The Mediating Role of Perceived Social Support. Front. Psychol. 2022, 13, 883833. [Google Scholar] [CrossRef]
- Held, M.L.; First, J.M.; Huslage, M.; Holzer, M. Policy stress and social support: Mental health impacts for Latinx Adults in the Southeast United States. Soc. Sci. Med. 2022, 307, 115172. [Google Scholar] [CrossRef]
- Zhang, M.; Wu, Y.; Ji, C.; Wu, J. The Role of Perceived Social Support and Stress in the Relationship between Hope and Depression among Chinese Shadow Education Tutors: A Serial Mediation Model. Int. J. Environ. Res. Public Health 2022, 19, 3348. [Google Scholar] [CrossRef]
- Hu, J.; Huang, Y.; Liu, J.; Zheng, Z.; Xu, X.; Zhou, Y.; Wang, J. COVID-19 Related Stress and Mental Health Outcomes 1 Year after the Peak of the Pandemic Outbreak in China: The Mediating Effect of Resilience and Social Support. Front. Psychiatry 2022, 13, 828379. [Google Scholar] [CrossRef]
- Leonard, K.S.; Evans, M.B.; Kjerulff, K.H.; Downs, D.S. Postpartum Perceived Stress Explains the Association between Perceived Social Support and Depressive Symptoms. Womens Health Issues 2020, 30, 231–239. [Google Scholar] [CrossRef]
- Zamanian, H.; Amini-Tehrani, M.; Jalali, Z.; Daryaafzoon, M.; Ala, S.; Tabrizian, S.; Foroozanfar, S. Perceived social support, coping strategies, anxiety and depression among women with breast cancer: Evaluation of a mediation model. Eur. J. Oncol. Nurs. 2021, 50, 101892. [Google Scholar] [CrossRef]
- Lim, A.Y.; Lee, S.H.; Jeon, Y.; Yoo, R.; Jung, H.Y. Job-Seeking Stress, Mental Health Problems, and the Role of Perceived Social Support in University Graduates in Korea. J. Korean Med. Sci. 2018, 33, e149. [Google Scholar] [CrossRef]
- Bedaso, A.; Adams, J.; Peng, W.; Sibbritt, D. The mediational role of social support in the relationship between stress and antenatal anxiety and depressive symptoms among Australian women: A mediational analysis. Reprod. Health 2021, 18, 250. [Google Scholar] [CrossRef] [PubMed]
- Lohanan, T.; Leesawat, T.; Wongpakaran, T.; Wongpakaran, N.; Karawekpanyawong, N.; Oon-Arom, A.; Kuntawong, P. Development and validation of a screening instrument for borderline personality disorder (SI-Bord) for use among university students. BMC Psychiatry 2020, 20, 479. [Google Scholar] [CrossRef] [PubMed]
- Schoemann, A.M.; Boulton, A.J.; Short, S.D. Determining Power and Sample Size for Simple and Complex Mediation Models. Soc. Psychol. Personal. Sci. 2017, 8, 379–386. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 386–396. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T. The Thai version of the PSS-10: An Investigation of its psychometric properties. BioPsychoSocial Med. 2010, 4, 6. [Google Scholar] [CrossRef]
- Zimet, G.D.; Powell, S.S.; Farley, G.K.; Werkman, S.; Berkoff, K.A. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1990, 55, 610–617. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Lotrakul, M.; Sumrithe, S.; Saipanish, R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry 2008, 8, 46. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; The Guilford Press: New York, NY, USA, 2018; pp. 507–517. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; The Guilford Press: New York, NY, USA, 2022. [Google Scholar]
- Agrawal, H.R.; Gunderson, J.; Holmes, B.M.; Lyons-Ruth, K. Attachment studies with borderline patients: A review. Harv. Rev. Psychiatry 2004, 12, 94–104. [Google Scholar] [CrossRef]
- Barnow, S.; Stopsack, M.; Grabe, H.; Meinke, C.; Spitzer, C.; Kronmüller, K.; Sieswerda, S. Interpersonal evaluation bias in borderline personality disorder. Behav. Res. Ther. 2009, 47, 359–365. [Google Scholar] [CrossRef]
- Schulze, A.; Biermann, M.; Atanasova, K.; Unterseher, F.; Winkler, L.; Bohus, M.; Lis, S. Social Touch, Social Isolation, and Loneliness in Borderline Personality Disorder during the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 876413. [Google Scholar] [CrossRef] [PubMed]
- Steele, K.R.; Townsend, M.L.; Grenyer, B.F.S. Parenting and personality disorder: An overview and meta-synthesis of systematic reviews. PLoS ONE 2019, 14, e0223038. [Google Scholar] [CrossRef] [PubMed]
- Guilé, J.M.; Boissel, L.; Alaux-Cantin, S.; de La Rivière, S.G. Borderline personality disorder in adolescents: Prevalence, diagnosis, and treatment strategies. Adolesc. Health Med. Ther. 2018, 9, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Kantojärvi, L.; Hakko, H.; Riipinen, P.; Riala, K. Who is becoming personality disordered? A register-based follow-up study of 508 inpatient adolescents. Eur. Psychiatry 2016, 31, 52–59. [Google Scholar] [CrossRef]
- Kantojärvi, L.; Hakko, H.; Mukka, M.; Käyhkö, A.; Riipinen, P.; Riala, K. Psychotropic medication use among personality disordered young adults. A follow-up study among former adolescent psychiatric inpatients. Psychiatry Res. 2020, 293, 113449. [Google Scholar] [CrossRef]
- Wongpakaran, N.; Wongpakaran, T.; Boonyanaruthee, V.; Pinyopornpanish, M.; Intaprasert, S. Comorbid personality disorders among patients with depression. Neuropsychiatr. Dis. Treat. 2015, 11, 1091–1096. [Google Scholar] [CrossRef]
- Wongpakaran, T.; Wongpakaran, N.; Boonyanaruthee, V.; Pinyopornpanish, M.; Intaprasert, S. The influence of comorbid personality disorders on recovery from depression. Neuropsychiatr. Dis. Treat 2015, 11, 725–732. [Google Scholar] [CrossRef][Green Version]
- Fonagy, P.; Luyten, P.; Allison, E.; Campbell, C. What we have changed our minds about: Part 1. Borderline personality disorder as a limitation of resilience. Bord. Personal. Disord. Emot. Dysregul. 2017, 4, 11. [Google Scholar] [CrossRef]
- Thoma, P.; Friedmann, C.; Suchan, B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci. Biobehav. Rev. 2013, 37, 448–470. [Google Scholar] [CrossRef]
- Du, H.; King, R.B.; Chu, S.K. Hope, social support, and depression among Hong Kong youth: Personal and relational self-esteem as mediators. Psychol. Health Med. 2016, 21, 926–931. [Google Scholar] [CrossRef]
- Mendez, I.; Sintes, A.; Pascual, J.C.; Puntí, J.; Lara, A.; Briones-Buixassa, L.; Nicolaou, S.; Schmidt, C.; Romero, S.; Fernández, M.; et al. Borderline personality traits mediate the relationship between low perceived social support and non-suicidal self-injury in a clinical sample of adolescents. J. Affect. Disord. 2022, 302, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Jia, N.; Sakulsriprasert, C.; Wongpakaran, N.; Suradom, C.; O’ Donnell, R. Borderline Personality Disorder Symptoms and Its Clinical Correlates among Chinese University Students: A Cross-Sectional Study. Healthcare 2022, 10, 1751. [Google Scholar] [CrossRef] [PubMed]
- Meaney, R.; Hasking, P.; Reupert, A. Prevalence of Borderline Personality Disorder in University Samples: Systematic Review, Meta-Analysis and Meta-Regression. PLoS ONE 2016, 11, e0155439. [Google Scholar] [CrossRef] [PubMed]
- Cano, K.; Sumlin, E.; Sharp, C. Screening for borderline personality pathology on college campuses. Personal. Ment. Health 2022, 16, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Irfan, M.; Sethi, M.R.; Abdullah, A.S.; Saleem, U.; Zeeshan, M.F. Assessment of personality disorders in students appearing for medical school entrance examination. J. Pak. Med. Assoc. 2018, 68, 1763–1768. [Google Scholar]

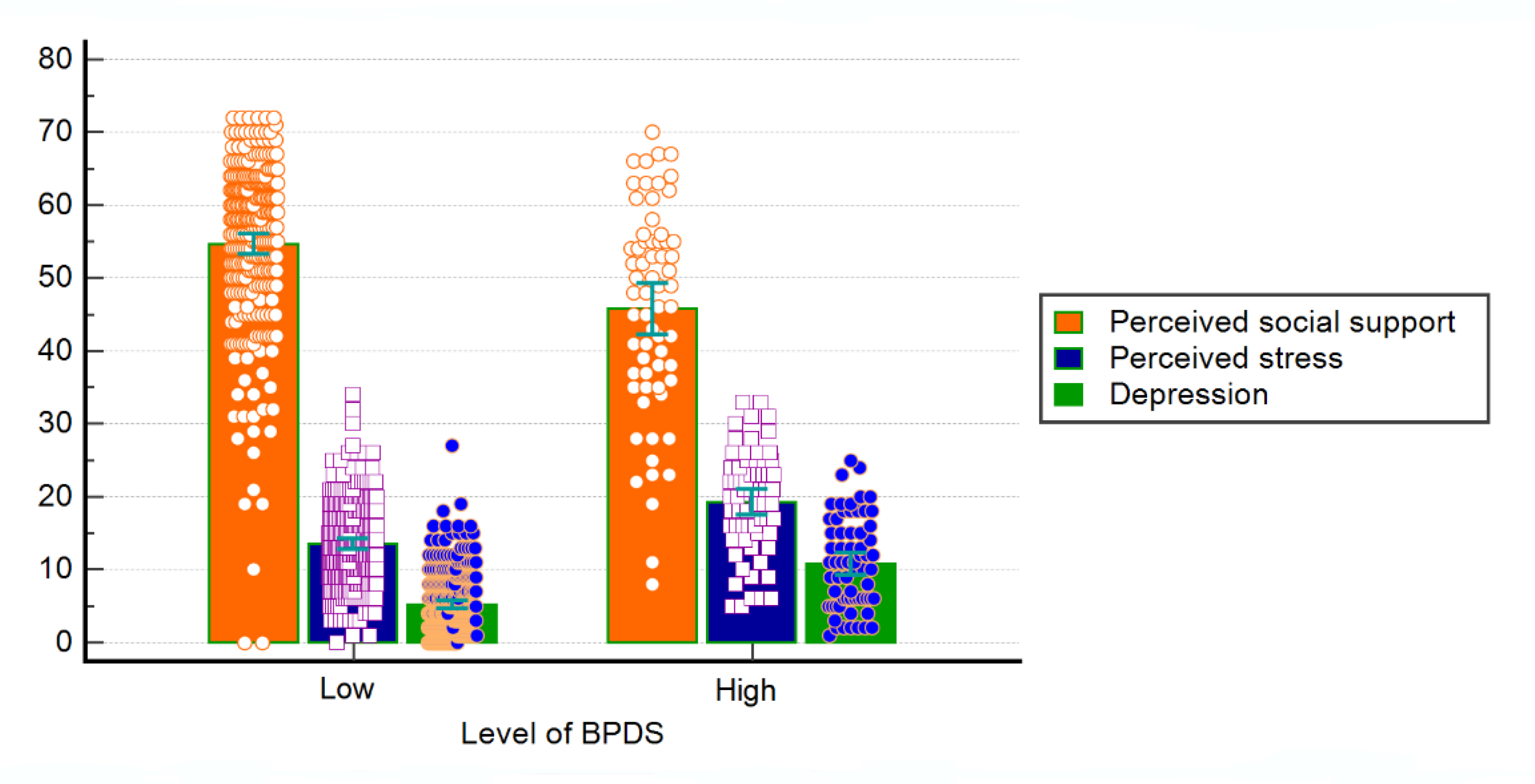
| Variable | All (n = 330) | High Level of BPDS (n = 65) | Low Level of BPDS (n = 265) | Test Difference |
|---|---|---|---|---|
| Age | 20.27 ± 1.4 | 21.05 ± 1.4 | 20.08 ± 1.3 | t = 5.23, p < 0.001 |
| Sex, female | 264 (80.0%) | 43 (66.2%) | 221 (83.4%) | t = 9.70, p < 0.001 |
| Years of studying, median (interquartile range) | 3(2) | 4(2) | 2 (2) | χ2(1) = 31.844, p < 0.001 |
| PSS | MSPSS | PHQ | |
|---|---|---|---|
| PSS | - | −0.395 ** | 0.645 ** |
| MSPSS | −0.428 ** | - | −0.421 ** |
| PHQ | 0.764 ** | −0.589 ** | - |
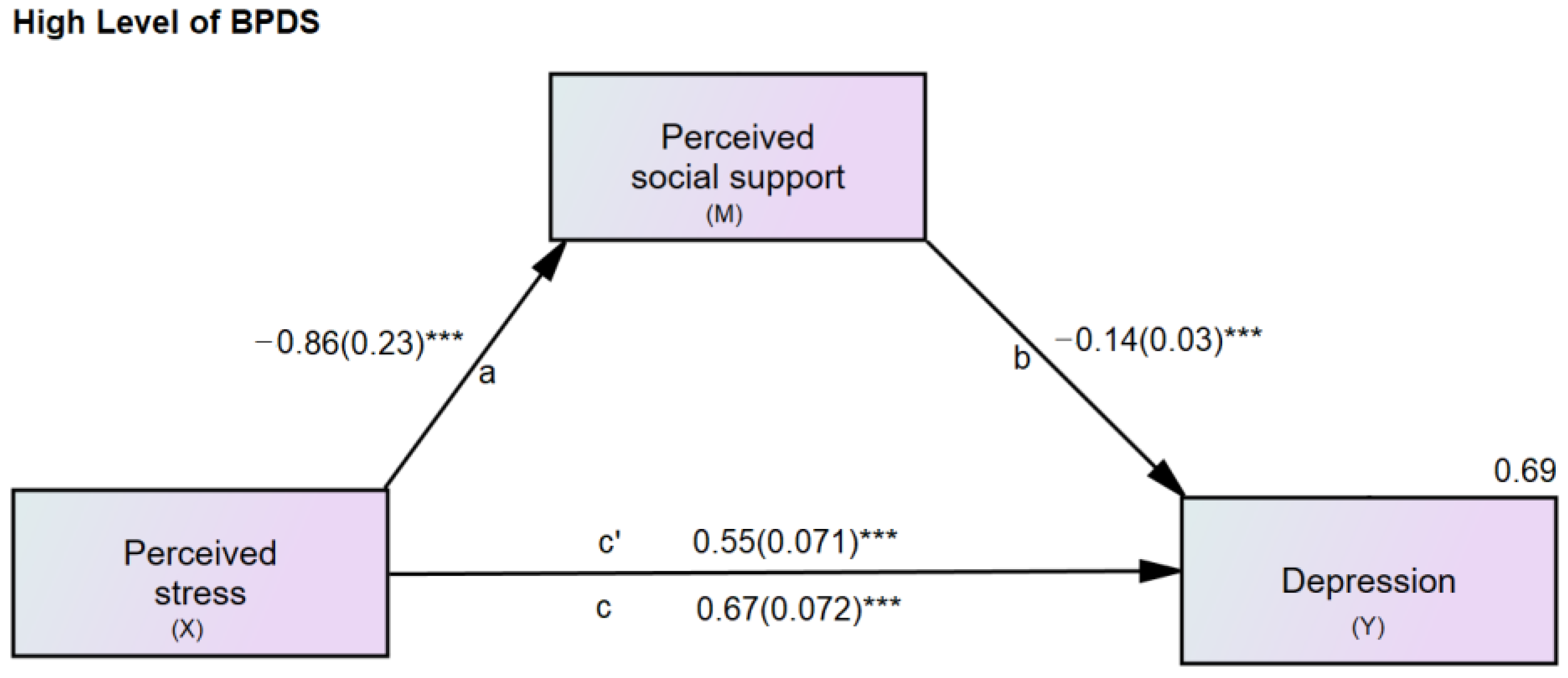
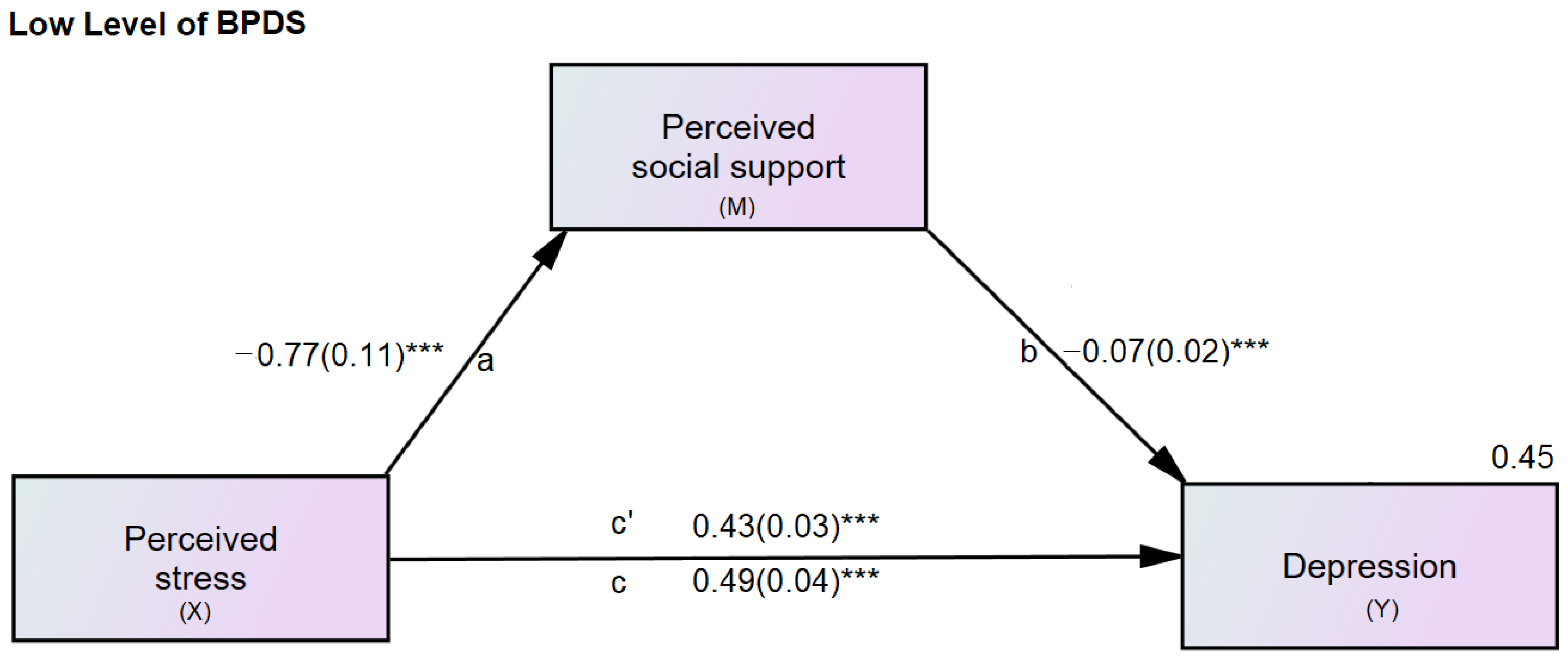
| Relationships Perceived Stress → Perceived Social Support → Depression | Level of BPDS | Direct Effect (B) (t-Statistics) | Indirect Effect (B) | Confidence Interval | R2 | |
|---|---|---|---|---|---|---|
| Lower Bound | Higher Bound | |||||
| Total | Low | 0.428(11.38) ** | 0.056 ** | 0.026 | 0.114 | 0.454 |
| High | 0.553 (7.80) *** | 0.120 ** | 0.041 | 0.240 | 0.685 | |
| SO | Low | 0.468 (13.27) ** | 0.016 | −0.001 | 0.043 | 0.429 |
| High | 0.606 (8.98) *** | 0.067 ** | 0.005 | 0.167 | 0.667 | |
| FM | Low | 0.430(11.20) ** | 0.055 ** | 0.016 | 0.111 | 0.449 |
| High | 0.568 (7.79) *** | 0.105 ** | 0.037 | 0.204 | 0.667 | |
| FR | Low | 0.442(11.80) ** | 0.043 ** | 0.010 | 0.090 | 0.446 |
| High | 0.599 (8.06) *** | 0.074 ** | 0.011 | 0.184 | 0.641 | |
| Pairwise Comparison | Total | Significant Others | Family | Friends |
|---|---|---|---|---|
| a1-a2 | 0.304 | 0.484 | −0.069 | 0.252 |
| b1-b2 | 1.641 | 2.278 * | 0.957 | 0.899 |
| c1-c2 | −1.521 | −1.697 | −1.824 | −1.837 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ingkachotivanich, N.; Wongpakaran, T.; Wongpakaran, N.; Oon-Arom, A.; Karawekpanyawong, N.; Lohanan, T.; Leesawat, T. Different Effects of Perceived Social Support on the Relationship between Perceived Stress and Depression among University Students with Borderline Personality Disorder Symptoms: A Multigroup Mediation Analysis. Healthcare 2022, 10, 2212. https://doi.org/10.3390/healthcare10112212
Ingkachotivanich N, Wongpakaran T, Wongpakaran N, Oon-Arom A, Karawekpanyawong N, Lohanan T, Leesawat T. Different Effects of Perceived Social Support on the Relationship between Perceived Stress and Depression among University Students with Borderline Personality Disorder Symptoms: A Multigroup Mediation Analysis. Healthcare. 2022; 10(11):2212. https://doi.org/10.3390/healthcare10112212
Chicago/Turabian StyleIngkachotivanich, Narusorn, Tinakon Wongpakaran, Nahathai Wongpakaran, Awirut Oon-Arom, Nuntaporn Karawekpanyawong, Trustsavin Lohanan, and Thanakorn Leesawat. 2022. "Different Effects of Perceived Social Support on the Relationship between Perceived Stress and Depression among University Students with Borderline Personality Disorder Symptoms: A Multigroup Mediation Analysis" Healthcare 10, no. 11: 2212. https://doi.org/10.3390/healthcare10112212
APA StyleIngkachotivanich, N., Wongpakaran, T., Wongpakaran, N., Oon-Arom, A., Karawekpanyawong, N., Lohanan, T., & Leesawat, T. (2022). Different Effects of Perceived Social Support on the Relationship between Perceived Stress and Depression among University Students with Borderline Personality Disorder Symptoms: A Multigroup Mediation Analysis. Healthcare, 10(11), 2212. https://doi.org/10.3390/healthcare10112212








