Advanced Practice Providers as Leaders of a Rapid Response Team: A Prospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Population
2.3. Power Analysis
2.4. Ethical Considerations
2.5. Data Collection
2.6. Study Outcomes
2.6.1. Primary Outcome
2.6.2. Secondary Outcomes
2.6.3. Statistical Analysis
3. Results
3.1. Participants and RRT Calls
3.2. Patient-Related Outcomes
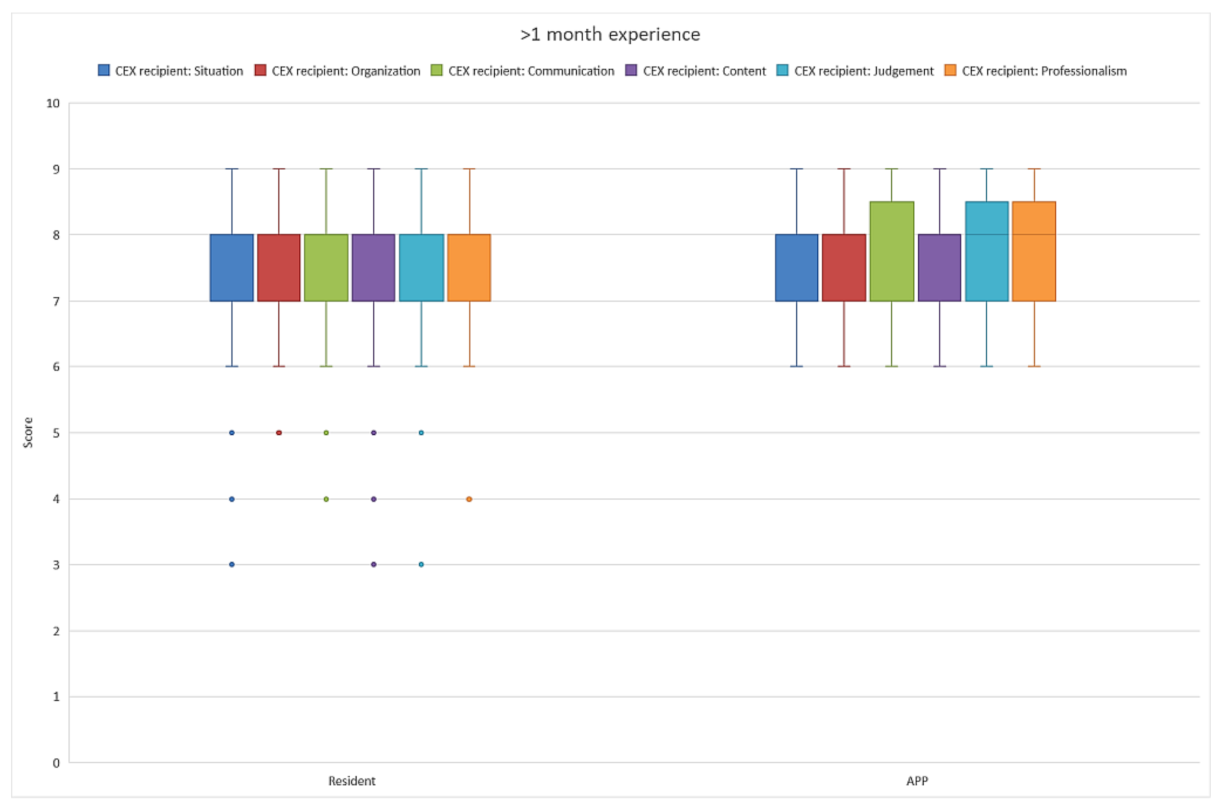
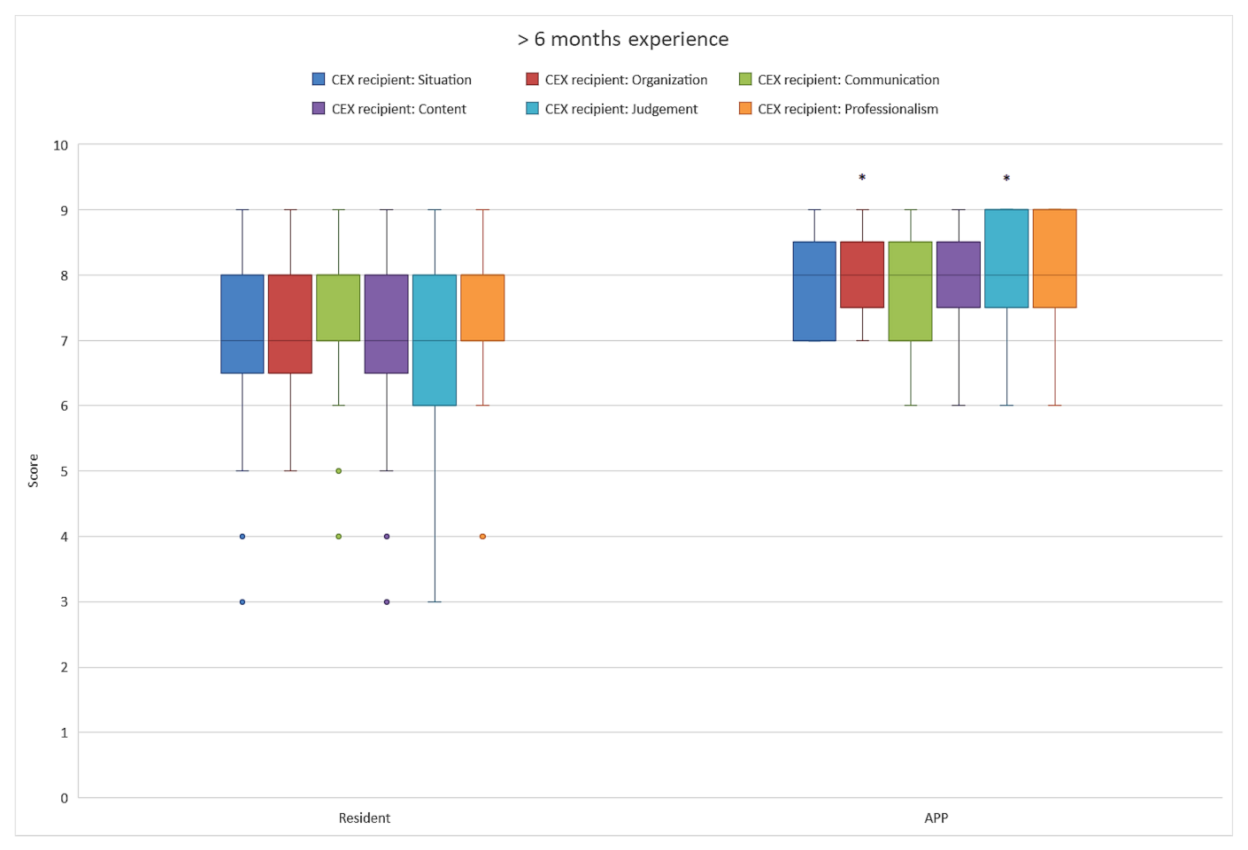
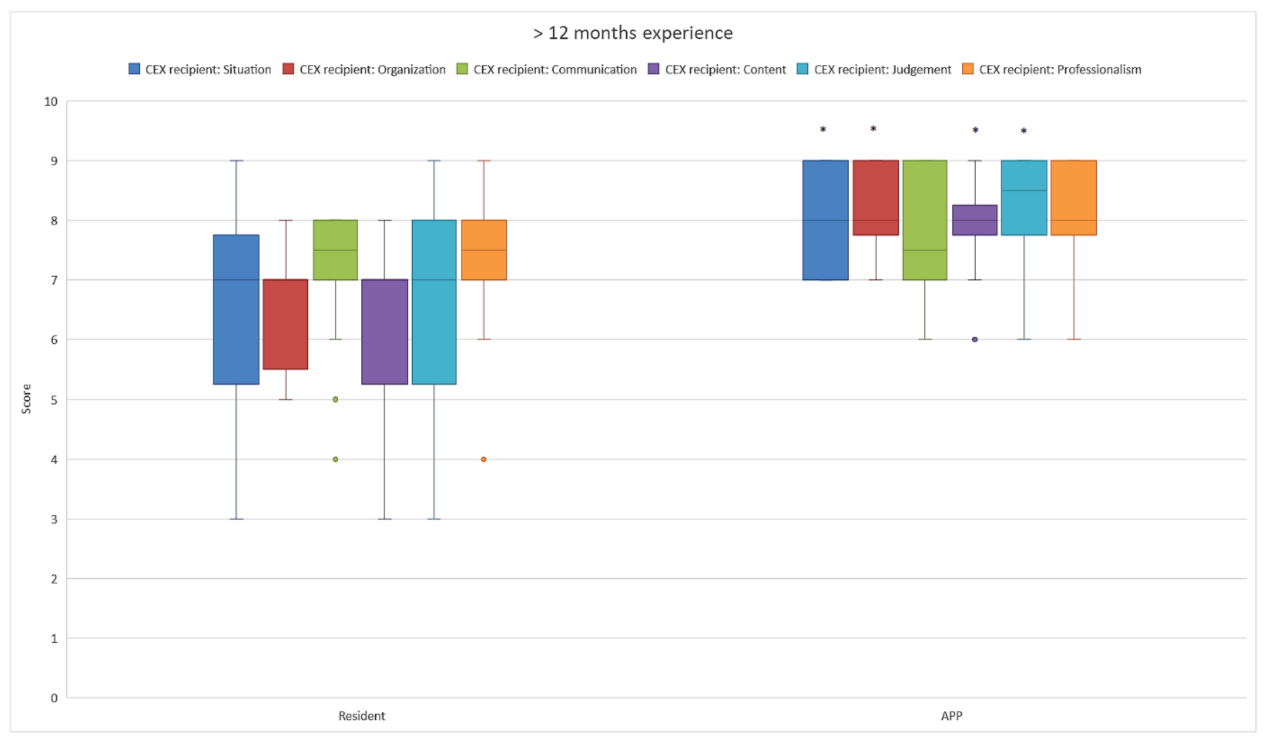
3.3. Team-Related Outcomes
4. Discussion
Strengths and Weaknesses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| APP | Advanced practice provider |
| EWS | Early warning score |
| ICU | Intensive care unit |
| MR | Medical resident |
| RRT | Rapid response team |
References
- Fry, M. Literature review of the impact of nurse practitioners in critical care services. Nurs. Crit. Care. 2011, 16, 58–66. [Google Scholar] [CrossRef]
- Kreeftenberg, H.G.; van Rosmalen, J.; Aarts, J.T.; van der Voort, P.H.J. Physician assistants in intensive care units in the Netherlands: A narrative review with recommendations. Neth. J. Crit. Care 2020, 28, 200–204. [Google Scholar]
- Kleinpell, R.M.; Grabenkort, W.R.; Kapu, A.N.; Constantine, R.; Sicoutris, C. Nurse Practitioners and Physician Assistants in Acute and Critical Care: A Concise Review of the Literature and Data 2008-2018. Crit. Care Med. 2019, 47, 1442–1449. [Google Scholar] [CrossRef]
- Kreeftenberg, H.G.; Pouwels, S.; Bindels, A.; de Bie, A.; van der Voort, P.H.J. Impact of the Advanced Practice Provider in Adult Critical Care: A Systematic Review and Meta-Analysis. Crit. Care Med. 2019, 47, 722–730. [Google Scholar] [CrossRef]
- Alexandrou, E.; Spencer, T.R.; Frost, S.A.; Mifflin, N.; Davidson, P.M.; Hillman, K.M. Central venous catheter placement by advanced practice nurses demonstrates low procedural complication and infection rates--a report from 13 years of service*. Crit. Care Med. 2014, 42, 536–543. [Google Scholar] [CrossRef]
- Bevis, L.C.; Berg-Copas, G.M.; Thomas, B.W.; Vasquez, D.G.; Wetta-Hall, R.; Brake, D.; Lucas, E.; Toumeh, K.; Harrison, P. Outcomes of tube thoracostomies performed by advanced practice providers vs trauma surgeons. Am. J. Crit. Care. 2008, 17, 357–363. [Google Scholar] [CrossRef]
- Rayo, M.F.; Mount-Campbell, A.F.; O’Brien, J.M.; White, S.E.; Butz, A.; Evans, K.; Patterson, E.S. Interactive questioning in critical care during handovers: A transcript analysis of communication behaviours by physicians, nurses and nurse practitioners. BMJ Qual. Saf. 2014, 23, 483–489. [Google Scholar] [CrossRef]
- Burns, S.M.; Earven, S.; Fisher, C.; Lewis, R.; Merrell, P.; Schubart, J.R.; Truwit, J.D.; Bleck, T.P. Implementation of an institutional program to improve clinical and financial outcomes of mechanically ventilated patients: One-year outcomes and lessons learned. Crit. Care Med. 2003, 31, 2752–2763. [Google Scholar] [CrossRef]
- Collins, N.; Miller, R.; Kapu, A.; Martin, R.; Morton, M.; Forrester, M.; Atkinson, S.; Evans, B.; Wilkinson, L. Outcomes of adding acute care nurse practitioners to a Level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction. J. Trauma Acute Care Surg. 2014, 76, 353–357. [Google Scholar] [CrossRef]
- Sirleaf, M.; Jefferson, B.; Christmas, A.B.; Sing, R.F.; Thomason, M.H.; Huynh, T.T. Comparison of procedural complications between resident physicians and advanced clinical providers. J. Trauma Acute Care Surg. 2014, 77, 143–147. [Google Scholar] [CrossRef]
- Landsperger, J.S.; Semler, M.W.; Wang, L.; Byrne, D.W.; Wheeler, A.P. Outcomes of Nurse Practitioner-Delivered Critical Care: A Prospective Cohort Study. Chest 2016, 149, 1146–1154. [Google Scholar] [CrossRef] [PubMed]
- Gershengorn, H.B.; Xu, Y.; Chan, C.W.; Armony, M.; Gong, M.N. The Impact of Adding a Physician Assistant to a Critical Care Outreach Team. PLoS ONE 2016, 11, e0167959. [Google Scholar]
- Investigators A-CMd; Jones, D.; Drennan, K.; Hart, G.K.; Bellomo, R.; Web, S.A. Rapid Response Team composition, resourcing and calling criteria in Australia. Resuscitation 2012, 83, 563–567. [Google Scholar] [PubMed]
- Moreira, A.A.S.; Ramos, R.O.; Ligorio, A.B.S.; Junqueira, K.D.; Correa, K.S. Rapid response team: What factors interfere with your performance? Invest. Educ. Enferm. 2018, 36. [Google Scholar] [CrossRef]
- Daniele, R.M.; Bova, A.M.; LeGar, M.; Smith, P.J.; Shortridge-Baggett, L.M. Rapid response team composition effects on outcomes for adult hospitalised patients: A systematic review. JBI Libr. Syst. Rev. 2011, 9, 1297–1340. [Google Scholar] [CrossRef]
- Gupta, S.; Balachandran, M.; Bolton, G.; Pratt, N.; Molloy, J.; Paul, E.; Tiruvoipati, R. Comparison of clinical outcomes between nurse practitioner and registrar-led medical emergency teams: A propensity-matched analysis. Crit. Care 2021, 25, 117. [Google Scholar] [CrossRef]
- Kreeftenberg, H.G.; de Bie, A.J.R.; Subbe, C.P.; van der Voort, P.H.J. Advanced practice providers in critical care improve team performances. A post-hoc analysis of the BASIC trial. Resuscitation 2022, 170, 207–208. [Google Scholar] [CrossRef]
- Kreeftenberg, H.G.; De Bie, A.J.R.; Mestrom, E.H.J.; Bindels, A.; van der Voort, P.H.J. Advanced practice providers versus medical residents as leaders of rapid response teams: A 12-month retrospective analysis. PLoS ONE 2022, 17, e0273197. [Google Scholar] [CrossRef]
- Sidani, S.; Doran, D.; Porter, H.; LeFort, S.; O’Brien-Pallas, L.; Zahn, C.; Sarkissian, S. Outcomes of nurse practitioners in acute care: An exploration. Internet J. Adv. Nurs. Pr. 2005, 8, 1–7. [Google Scholar]
- Ludikhuize, J.; Brunsveld-Reinders, A.H.; Dijkgraaf, M.G.; Smorenburg, S.M.; de Rooij, S.E.; Adams, R.; de Maaijer, P.F.; Fikkers, B.G.; Tangkau, P.; de Jonge, E. Outcomes Associated With the Nationwide Introduction of Rapid Response Systems in The Netherlands. Crit. Care Med. 2015, 43, 2544–2551. [Google Scholar] [CrossRef]
- Van Galen, L.S.; Dijkstra, C.C.; Ludikhuize, J.; Kramer, M.H.; Nanayakkara, P.W. A Protocolised Once a Day Modified Early Warning Score (MEWS) Measurement Is an Appropriate Screening Tool for Major Adverse Events in a General Hospital Population. PLoS ONE 2016, 11, e0160811. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Neilipovitz, D.; Cardinal, P.; Chiu, M. A comparison of global rating scale and checklist scores in the validation of an evaluation tool to assess performance in the resuscitation of critically ill patients during simulated emergencies (abbreviated as “CRM simulator study IB”). Simul. Healthc. 2009, 4, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Malec, J.F.; Torsher, L.C.; Dunn, W.F.; Wiegmann, D.A.; Arnold, J.J.; Brown, D.A.; Phatak, V. The mayo high performance teamwork scale: Reliability and validity for evaluating key crew resource management skills. Simul. Healthc. 2007, 2, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.; Owen, H.M.; Jones, K.; Hartin, J.; Welch, J.; Subbe, C.P. Objective patient-related outcomes of rapid-response systems—A pilot study to demonstrate feasibility in two hospitals. Crit. Care Resusc. 2013, 15, 33–39. [Google Scholar]
- Horwitz, L.I.; Dombroski, J.; Murphy, T.E.; Farnan, J.M.; Johnson, J.K.; Arora, V.M. Validation of a handoff assessment tool: The Handoff CEX. J. Clin. Nurs. 2013, 22, 1477–1486. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Thomas, E.J.; Sexton, J.B.; Helmreich, R.L. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit. Care Med. 2003, 31, 956–959. [Google Scholar] [CrossRef]
- Kreeftenberg, H.G.; Aarts, J.T.; Bindels, A.; van der Meer, N.J.M.; van der Voort, P.H.J. Procedures Performed by Advanced Practice Providers Compared With Medical Residents in the ICU: A Prospective Observational Study. Crit. Care Explor. 2020, 2, e010. [Google Scholar] [CrossRef]
- Pirret, A.M. The role and effectiveness of a nurse practitioner led critical care outreach service. Intensive Crit. Care Nurs. 2008, 24, 375–382. [Google Scholar] [CrossRef]
- Van Vught, A.; van den Brink, G.; Hilkens, M.; van Oers, J.A.H. Analysis of the level of clinical skills of physician assistants tested with simulated intensive care patients. J. Eval. Clin. Pract. 2018, 24, 580–584. [Google Scholar] [CrossRef]
| Characteristics | APP | MR |
|---|---|---|
| Experience of the clinician in months * | 5 (1–104) | 6 (2–17) |
| Reason for RRT call | ||
| Respiratory or airway problems | 12 | 11 |
| Hemodynamic instability/sepsis ** | 7 | 21 |
| Electrolyte disorders | 1 | 1 |
| Altered consciousness | 0 | 1 |
| Other | 0 | 6 |
| Specialism | ||
| Surgery | 7 | 6 |
| Internal medicine | 3 | 13 |
| Cardiology | 3 | 3 |
| Pulmonology | 2 | 2 |
| Cardiothoracic surgery | 2 | 1 |
| Gastroenterology | 0 | 3 |
| Neurology | 3 | 1 |
| Other | 0 | 11 |
| Admitted to the ICU | 13 | 25 |
| Patient qSOFA | 0.95 | 1.2 |
| Patient age * | 69 (63–80) | 68 (55–78) |
| Patient gender male | 20 | 26 |
| Patient gender female | 8 | 14 |
| Age-adjusted Charlson comorbidity index * | 7 (3–8.8) | 4.5 (3–6.8) |
| Patient-Related Outcome | APP | MR | p-Value (Chi Square) |
|---|---|---|---|
| Mortality (30 day) | 5/20 (25%) | 7/40 (17.5%) | 0.73 (0.117) |
| MAELOR positive | 17 | 40 | 0.59 (3.55) |
| Admission < 4 h | 13 | 25 | na |
| No admission | 6 | 15 | na |
| Admission > 4 h | 1 | 0 | na |
| Process-Related Outcome * | APP Median (IQR) | MR Median (IQR) | p-Value (u-Value and z-Score) |
| Time between call and arrival (min:sec) | 4:30 (2:45–9:30) | 3:59 (2:00–6:00) | 0.28 (258.5, −1.07) |
| Time until respiratory exam (min:sec) | 0:30 (0:00–1:00) | 0:00 (0:00–1:00) | 0.25 (318.5, −1.14) |
| Time until circulation exam (min:sec) | 2:00 (1:00–4:00) | 1:00 (0:44–3:00) | 0.13 (289, −1.53) |
| Time until EMV exam (min:sec) | 2:00 (1:00–4:00) | 1:00 (0:00–3:00) | 0.91 (336, −0.11) |
| Time until diagnosis (min:sec) | 5:00 (3:00–10:00) | 5:00 (3:00–8:00) | 0.72 (276.5, −0.36) |
| Crisis management skills total | 27 (25–28) | 27 (26–28) | 0.59 (366.5, −0.53) |
| MAYO observer | 22 (22–24) | 23 (22–24) | 0.34 (340.5, −0.95) |
| GRS observer | 6 (6–7) | 6(6–7) | 0.96 (397.5, −0.048) |
| MAYO ICU nurse | 21 (19–24.5) | 24 (20.7–25) | 0.22 (57.5, −1.22) |
| GRS ICU nurse | 6 (6–6.5) | 6 (6–6) | 0.44 (69.5, −0.77) |
| CEX provider | 7 (6–7.25) | 7 (7–8) | 0.04 (233, −2.09) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kreeftenberg, H.G.; de Bie, A.J.R.; Aarts, J.T.; Bindels, A.J.G.H.; van der Meer, N.J.M.; van der Voort, P.H.J. Advanced Practice Providers as Leaders of a Rapid Response Team: A Prospective Cohort Study. Healthcare 2022, 10, 2122. https://doi.org/10.3390/healthcare10112122
Kreeftenberg HG, de Bie AJR, Aarts JT, Bindels AJGH, van der Meer NJM, van der Voort PHJ. Advanced Practice Providers as Leaders of a Rapid Response Team: A Prospective Cohort Study. Healthcare. 2022; 10(11):2122. https://doi.org/10.3390/healthcare10112122
Chicago/Turabian StyleKreeftenberg, Herman G., Ashley J. R. de Bie, Jeroen T. Aarts, Alexander J. G. H. Bindels, Nardo J. M. van der Meer, and Peter H. J. van der Voort. 2022. "Advanced Practice Providers as Leaders of a Rapid Response Team: A Prospective Cohort Study" Healthcare 10, no. 11: 2122. https://doi.org/10.3390/healthcare10112122
APA StyleKreeftenberg, H. G., de Bie, A. J. R., Aarts, J. T., Bindels, A. J. G. H., van der Meer, N. J. M., & van der Voort, P. H. J. (2022). Advanced Practice Providers as Leaders of a Rapid Response Team: A Prospective Cohort Study. Healthcare, 10(11), 2122. https://doi.org/10.3390/healthcare10112122






