Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort
Abstract
1. Introduction
2. Materials and Methods
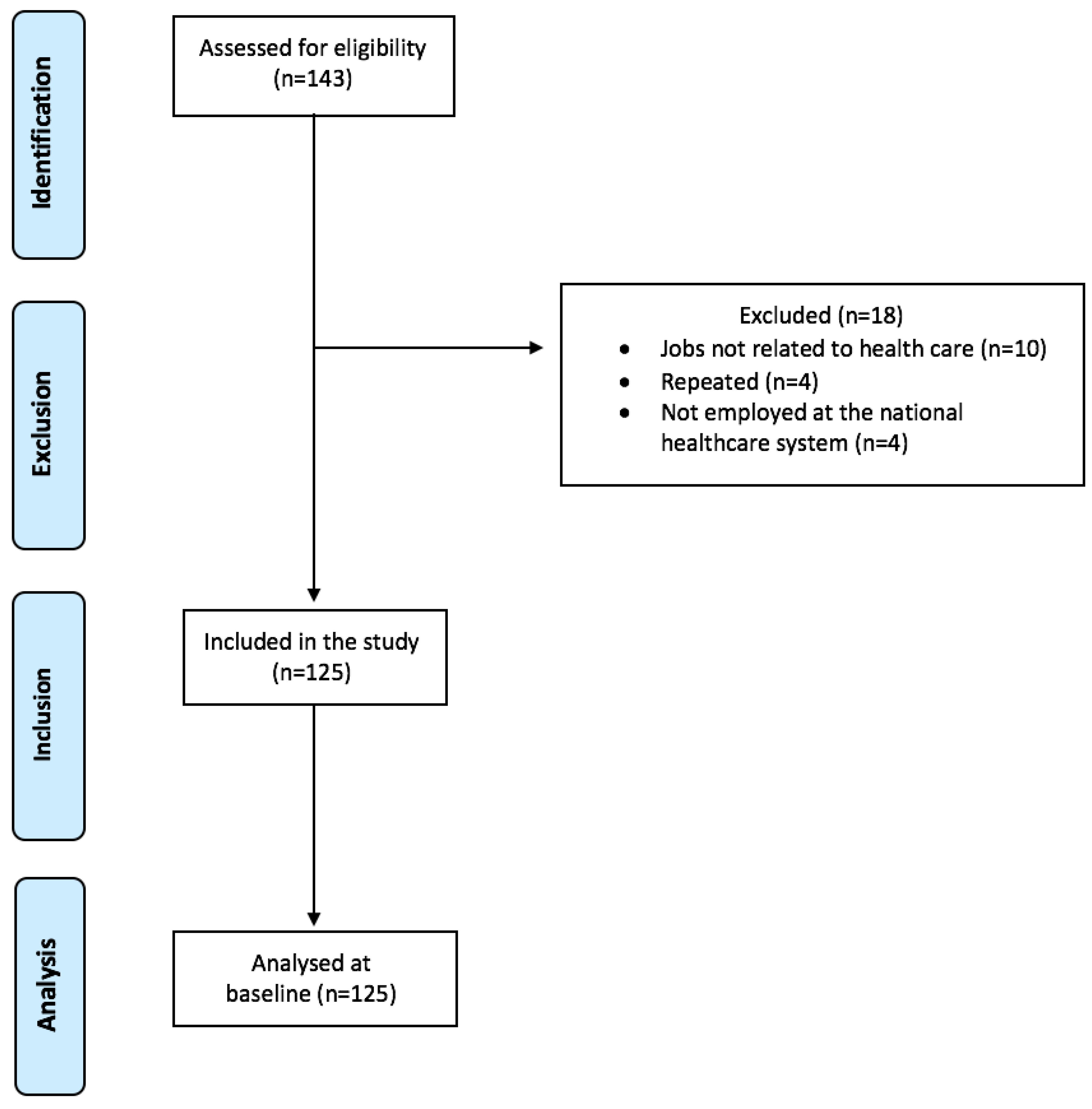
2.1. Study Design
2.2. Recruitment Process
2.3. Ethical Aspects
2.4. Participants
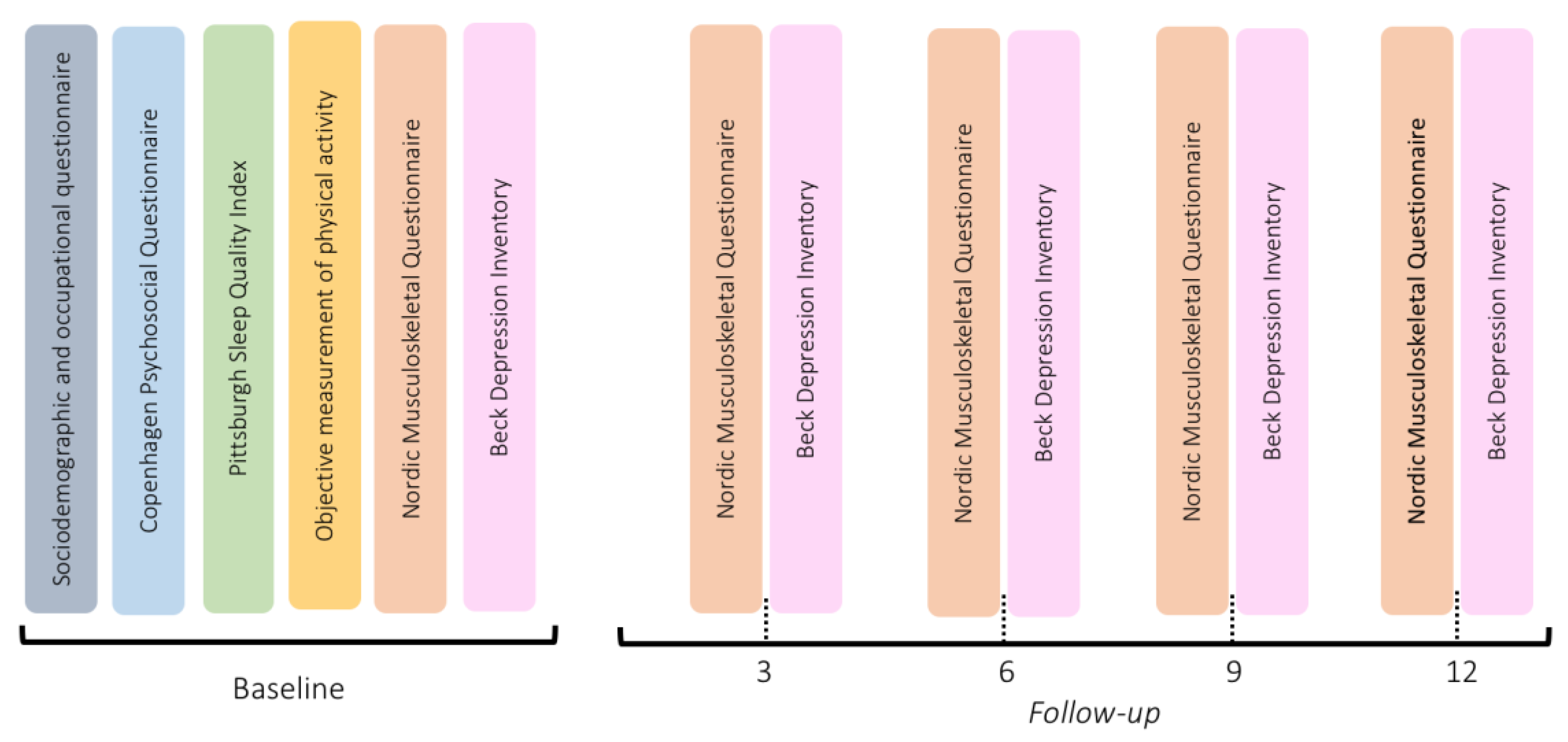
2.5. Data Collection
2.5.1. Baseline Measurements
2.5.2. Follow-Up
2.6. Procedures
2.7. Data Analysis
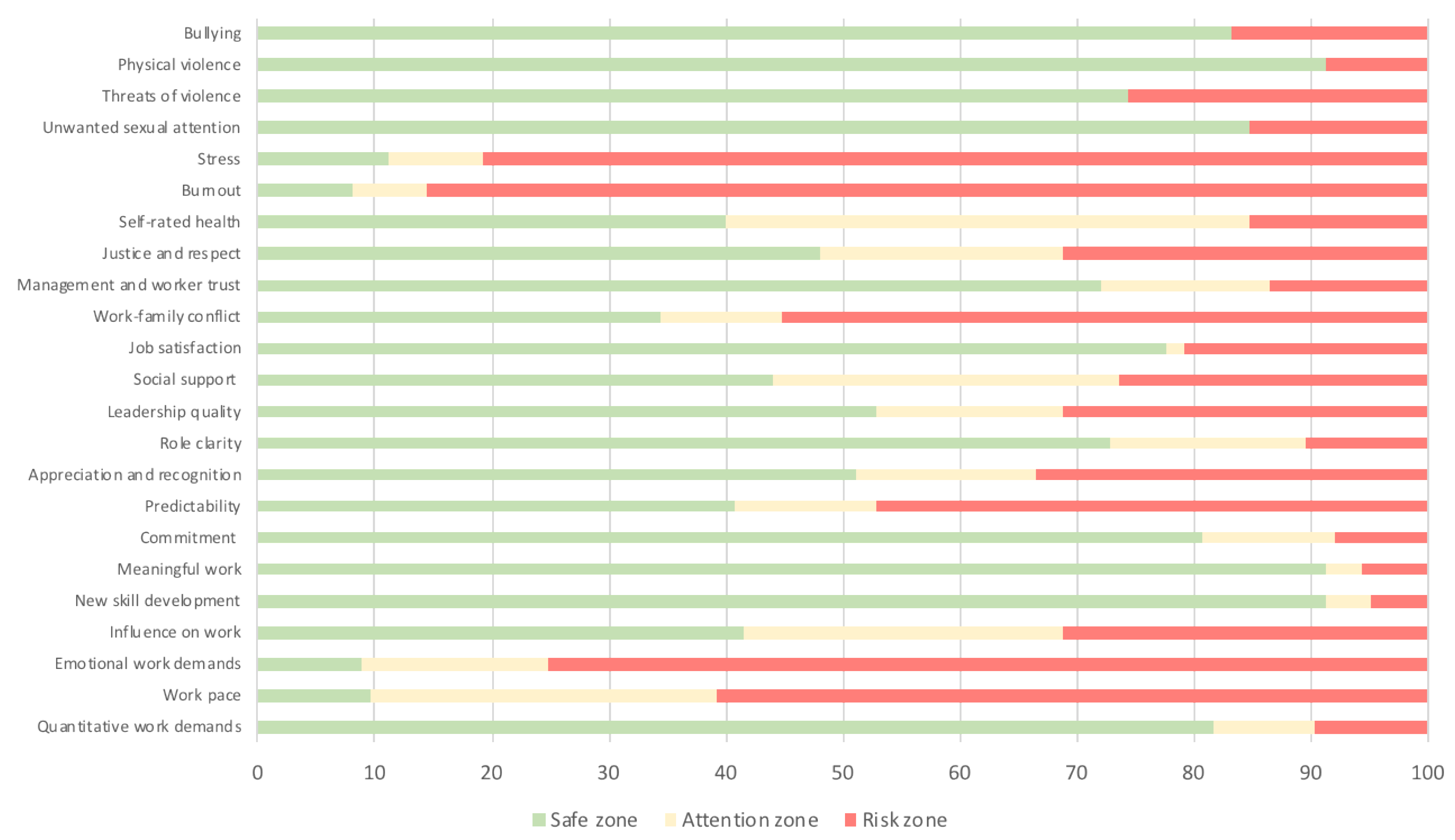
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Castellucci, H.I.; Altamirano, I. Changing the shift system in a mining company: An intervention study. Hum. Factors Ergon. Manuf. Serv. Ind. 2017, 28, 81–89. [Google Scholar] [CrossRef]
- Hittle, B.M.; Gillespie, G.L. Identifying shift worker chronotype: Implications for health. Ind. Health 2018, 56, 512–523. [Google Scholar] [CrossRef] [PubMed]
- Boden, L.I.; Sembajwe, G.; Tveito, T.H.; Hashimoto, D.; Hopcia, K.; Ms, C.K.; Stoddard, A.M.; Sorensen, G. Occupational injuries among nurses and aides in a hospital setting. Am. J. Ind. Med. 2011, 55, 117–126. [Google Scholar] [CrossRef]
- Ministério da Previdência Social. Boletim Quadrimestral Sobre Benefícios por Incapacidade de 2017. Adoecimento Mental e Trabalho: A Concessão de Benefícios por Incapacidade Relacionados a Transtornos Mentais e Comportamentais Entre 2012 e 2016. 2017. Available online: http://sa.previdencia.gov.br/site/2017/04/1oboletim-quadrimestral.pdf (accessed on 13 June 2020).
- Guy, M.E.; Newman, M.A. Women’s Jobs, Men’s Jobs: Sex Segregation and Emotional Labor. Public Adm. Rev. 2004, 64, 289–298. [Google Scholar] [CrossRef]
- Meeks, T.W.; Vahia, I.V.; Lavretsky, H.; Kulkarni, G.; Jeste, D.V. A tune in “a minor” can “b major”: A review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J. Affect. Disord. 2011, 129, 126–142. [Google Scholar] [CrossRef] [PubMed]
- Cheung, T.; Yip, P.S. Lifestyle and Depression among Hong Kong Nurses. Int. J. Environ. Res. Public Health 2016, 13, 135. [Google Scholar] [CrossRef]
- Ibrahim, M.E.; Cheval, B.; Cullati, S.; Mongin, D.; Lauper, K.; Pihl-Thingvad, J.; Chopard, P.; Genevay, S.; Courvoisier, D.S. Back pain occurrence and treatment-seeking behavior among nurses: The role of work-related emotional burden. Qual. Life Res. 2020, 29, 1301–1310. [Google Scholar] [CrossRef]
- Tanaka, H.; Sasazawa, Y.; Suzuki, S.; Nakazawa, M.; Koyama, H. Health status and lifestyle factors as predictors of depression in middle-aged and elderly Japanese adults: A seven-year follow-up of the Komo-Ise cohort study. BMC Psychiatry 2011, 11, 20. [Google Scholar] [CrossRef]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef]
- Theorell, T.; Hammarström, A.; Aronsson, G.; Bendz, L.T.; Grape, T.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Hall, C. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015, 15, 1–14. [Google Scholar] [CrossRef]
- Wang, J.; Patten, S.B.; Currie, S.; Sareen, J.; Schmitz, N. A Population-based Longitudinal Study on Work Environmental Factors and the Risk of Major Depressive Disorder. Am. J. Epidemiol. 2012, 176, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Han, T.; Chen, W.; Dib, H.; Yang, G.; Zhuang, R.; Chen, Y.; Tong, X.; Yin, X.; Lu, Z. Prevalence of Anxiety and Depressive Symptoms and Related Risk Factors among Physicians in China: A Cross-Sectional Study. PLoS ONE 2014, 9, e103242. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, A.M.; Silva, M.T.; Galvão, T.F.; Lopes, L.C. The relationship between job satisfaction, burnout syndrome and depressive symptoms. Medicine 2018, 97, e13364. [Google Scholar] [CrossRef] [PubMed]
- De Vasconcelos, E.M.; De Martino, M.M.F.; França, S.P.D.S. Burnout and depressive symptoms in intensive care nurses: Relationship analysis. Rev. Bras. Enferm. 2018, 71, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Weigl, M.; Stab, N.; Herms, I.; Angerer, P.; Hacker, W.; Glaser, J. The associations of supervisor support and work overload with burnout and depression: A cross-sectional study in two nursing settings. J. Adv. Nurs. 2016, 72, 1774–1788. [Google Scholar] [CrossRef]
- Bitencourt, S.M.; Andrade, C.B. Trabalhadoras da saúde face à pandemia: Por uma análise sociológica do trabalho de cuidado. Ciência Saúde Coletiva 2021, 26, 1013–1022. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for reporting results of internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Gonçalves, J.S.; Moriguchi, C.S.; Chaves, T.C.; Sato, T.D.O. Cross-cultural adaptation and psychometric properties of the short version of COPSOQ II-Brazil. Rev. Saude Publica 2021, 55, 69. [Google Scholar] [CrossRef]
- Silva, C.; Amaral, V.; Pereira, A.; Bem-haja, P.; Pereira, A.; Rodrigues, V.; Patrone Cotrim, T.; Silvério, J.; Nossa, P. Copenhagen Psychosocial Questionnaire: Portugal e Países Africanos de Língua Oficial Portuguesa; Departamento de Educação, Universidade de Aveiro: Aveiro, Portugal, 2011. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Bertolazi, A.N.; Fagondes, S.C.; Hoff, L.S.; Dartora, E.G.; Miozzo, I.C.D.S.; de Barba, M.E.F.; Barreto, S.S.M. Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011, 12, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, F.A.; Tróccoli, B.T.; De Carvalho, C.V. Validação do Questionário Nórdico de Sintomas Osteomusculares como medida de morbidade. Rev. Saude Publica 2002, 36, 307–312. [Google Scholar] [CrossRef] [PubMed]
- De Barros, E.N.; Alexandre, N.M. Cross-cultural adaptation of the Nordic musculoskeletal questionnaire. Int. Nurs. Rev. 2003, 50, 101–108. [Google Scholar] [CrossRef]
- Gomes-Oliveira, M.H.; Gorenstein, C.; Lotufo Neto, F.; Andrade, L.H.; Wang, Y.P. Validation of the Brazilian Portuguese Version of the Beck Depression Inventory-II in a community sample. Rev. Bras. Psiquiatr. 2012, 34, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Varghese, A.; George, G.; Kondaguli, S.V.; Naser, A.Y.; Khakha, D.C.; Chatterji, R. Decline in the mental health of nurses across the globe during COVID-19: A systematic review and meta-analysis. J. Glob. Health 2021, 11, 05009. [Google Scholar] [CrossRef] [PubMed]
- Busch, I.M.; Moretti, F.; Mazzi, M.; Wu, A.W.; Rimondini, M. What We Have Learned from Two Decades of Epidemics and Pandemics: A Systematic Review and Meta-Analysis of the Psychological Burden of Frontline Healthcare Workers. Psychother. Psychosom. 2021, 90, 178–190. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 38, 3286–3302. [Google Scholar] [CrossRef]
- Pai, D.D.; Sturbelle, I.C.S.; Dos Santos, C.; Tavares, J.P.; Lautert, L. Violência física e psicológica perpetrada no trabalho em saúde. Texto Context.-Enferm. 2018, 27, e2420016. [Google Scholar] [CrossRef]
- De Vasconcellos, I.R.R.; Griep, R.H.; Lisboa, M.T.L.; Rotenberg, L. Violence in daily hospital nursing work. Acta Paul. Enferm. 2012, 25, 40–47. [Google Scholar] [CrossRef]
- Trindade, L.D.L.; Ribeiro, S.T.; Zanatta, E.A.; Vendruscolo, C.; Pai, D.D. Agressão verbal no trabalho da Enfermagem na área hospitalar. Rev. Eletrônica Enferm. 2019, 21, 54333. [Google Scholar] [CrossRef]
- Cotrin, P.; Moura, W.; Gambardela-Tkacz, C.M.; Pelloso, F.C.; Dos Santos, L.; de Barros Carvalho, M.D.; Pelloso, S.M.; Freitas, K.M.S. Healthcare Workers in Brazil during the COVID-19 Pandemic: A Cross-Sectional Online Survey. Inquiry 2020, 57, 46958020963711. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.A.; Alhaj, O.A.; Humood, A.M.; Alenezi, A.F.; Fekih-Romdhane, F.; AlRasheed, M.M.; Saif, Z.Q.; Bragazzi, N.L.; Pandi-Perumal, S.R.; BaHammam, A.S.; et al. Sleep disturbances during the COVID-19 pandemic: A systematic review, meta-analysis, and meta-regression. Sleep Med. Rev. 2022, 62, 101591. [Google Scholar] [CrossRef] [PubMed]
- Proserpio, P.; Zambrelli, E.; Lanza, A.; Dominese, A.; Di Giacomo, R.; Quintas, R.; Tramacere, I.; Rubino, A.; Turner, K.; Colosio, C.; et al. Sleep disorders and mental health in hospital workers during the COVID-19 pandemic: A cross-sectional multicenter study in Northern Italy. Neurol. Sci. 2022, 43, 2241–2251. [Google Scholar] [CrossRef] [PubMed]
- Stewart, N.H.; Koza, A.; Dhaon, S.; Shoushtari, C.; Martinez, M.; Arora, V.M. Sleep Disturbances in Frontline Health Care Workers During the COVID-19 Pandemic: Social Media Survey Study. J. Med. Internet Res. 2021, 23, e27331. [Google Scholar] [CrossRef]
- Moreira, R.F.C.; Sato, T.; Foltran, F.A.; Silva, L.C.C.B.; Coury, H.J.C.G. Prevalence of musculoskeletal symptoms in hospital nurse technicians and licensed practical nurses: Associations with demographic factors. Braz. J. Phys. Ther. 2014, 18, 323–333. [Google Scholar] [CrossRef]
- El Far, H.E.; Albitar, E.A.E.F.; Araby, E.M.; Nabil, N.; Hassan, O.M. Patterns of Work-related Musculoskeletal Disorders among Health Care Workers. Egypt. J. Hosp. Med. 2020, 81, 2325–2334. [Google Scholar] [CrossRef]
- Arca, M.; Dönmezdil, S.; Durmaz, E.D. The effect of the COVID-19 Pandemic on anxiety, depression, and musculoskeletal system complaints in healthcare workers. Work 2021, 69, 47–54. [Google Scholar] [CrossRef]
- Da Silva, F.C.T.; Neto, M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 104, 110057. [Google Scholar] [CrossRef]
- Villela, E.F.D.M.; da Cunha, I.R.; Fodjo, J.N.S.; Obimpeh, M.; Colebunders, R.; Van Hees, S. Impact of COVID-19 on Healthcare Workers in Brazil between August and November 2020: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 6511. [Google Scholar] [CrossRef]
- David, H.M.S.L.; Rafael, R.M.R.; Alves, M.G.D.M.; Breda, K.L.; Faria, M.G.D.A.; Neto, M.; de Souza, R.C.; Persegona, M.F.M.; da Silva, M.C.N. Infection and mortality of nursing personnel in Brazil from COVID-19: A cross-sectional study. Int. J. Nurs. Stud. 2021, 124, 104089. [Google Scholar] [CrossRef] [PubMed]
- Correia, R.F.; da Costa, A.C.C.; Moore, D.C.B.C.; Junior, S.C.G.; de Oliveira, M.P.C.; Zuma, M.C.C.; Galvani, R.G.; Savino, W.; Bonomo, A.C.; Vasconcelos, Z.F.M.; et al. SARS-CoV-2 seroprevalence and social inequalities in different subgroups of healthcare workers in Rio de Janeiro, Brazil. Lancet Reg. Health-Am. 2021, 7, 100170. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n | % |
|---|---|---|
| Sex | ||
| Female | 104 | 83.2 |
| Male | 21 | 16.8 |
| Age | ||
| 18 to 30 years | 25 | 20.0 |
| 31 to 40 years | 58 | 46.4 |
| 41 to 60 years | 42 | 33.6 |
| Skin colour | ||
| White | 89 | 71.2 |
| Black/brown | 35 | 28.0 |
| Yellow | 1 | 0.8 |
| Marital status | ||
| Single | 41 | 32.8 |
| Married | 71 | 56.8 |
| Widower/divorced | 13 | 10.4 |
| Number of children | ||
| None | 65 | 52.0 |
| One | 30 | 24.0 |
| Two or more | 30 | 24.0 |
| Educational level | ||
| Primary school education | 2 | 1.6 |
| High school education | 23 | 18.4 |
| University | 100 | 80.0 |
| Body mass index (BMI) | ||
| Underweight | 1 | 0.8 |
| Normal weight | 50 | 40.0 |
| Overweight | 41 | 32.8 |
| Obese | 33 | 26.4 |
| Smoke | 14 | 11.2 |
| Alcohol use more than 2 times/week | 20 | 16.0 |
| Physical activity during leisure time | 69 | 55.2 |
| Diagnosed disease | 53 | 42.4 |
| Medication use | 83 | 66.4 |
| Occupation | ||
| Nurse | 45 | 36.0 |
| Nursing assistant/technician | 28 | 22.4 |
| Physiotherapist | 26 | 20.8 |
| Physician | 8 | 6.4 |
| Dentist | 4 | 3.2 |
| Other | 14 | 11.2 |
| Job seniority | ||
| Less than 2 years | 37 | 29.6 |
| 2–5 years | 42 | 33.6 |
| More than 5 years | 46 | 36.8 |
| Workplace | ||
| Primary care | 40 | 32.0 |
| Hospital | 61 | 48.8 |
| Emergency care | 12 | 9.6 |
| Ambulatory care | 9 | 7.3 |
| Homecare | 3 | 2.4 |
| Weekly working hours | ||
| Up to 24 h | 6 | 4.8 |
| 30 h | 30 | 24.0 |
| 36 h | 21 | 16.8 |
| 40 h | 60 | 48.0 |
| >40 h | 8 | 6.4 |
| Other employment | 39 | 31.2 |
| Family income (US$) | ||
| >1 to 3 × MMW | 25 | 20.0 |
| >3 to 6 × MMW | 49 | 39.2 |
| >6 to 9 × MMW | 22 | 17.6 |
| >9 × MMW | 25 | 20.0 |
| Not declared | 4 | 3.2 |
| Body Region | 12-Month Symptoms | 12-Month Disability | 12-Month Healthcare Assistance | 7-Day Symptoms |
|---|---|---|---|---|
| Neck | 64.0 (55–72) | 20.0 (14–28) | 18.4 (16–26) | 31.2 (24–40) |
| Shoulders | 62.4 (54–70) | 13.6 (9–21) | 13.6 (9–21) | 26.4 (19–35) |
| Upper back | 58.4 (50–67) | 16.0 (11–23) | 12.8 (8–20) | 29.6 (22–38) |
| Elbow | 9.6 (6–16) | 3.2 (1–8) | 6.4 (3–12) | 5.6 (3–11) |
| Lower back | 60.8 (52–69) | 23.2 (17–31) | 15.2 (10–23) | 39.2 (31–48) |
| Wrist/hand | 42.4 (34–51) | 10.4 (6–17) | 8.8 (5–15) | 13.6 (9–21) |
| Hip/thigh | 29.6 (22–38) | 5.6 (3–11) | 7.2 (4–13) | 12.0 (7–19) |
| Knee | 32.0 (24–41) | 9.6 (6–16) | 8.8 (5–15) | 16.8 (11–24) |
| Ankle/foot | 36.8 (29–46) | 8.0 (4–14) | 9.6 (6–16) | 20.8 (15–29) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sato, T.d.O.; de Faria, B.S.F.; Albuquerque, B.B.; Silva, F.L.d.; Rohwedder, L.S.; de Azevedo, R.T.; Gonçalves, J.S.; Vieira, L.M.S.M.d.A.; Triches, M.I.; de Sousa, R.A.; et al. Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort. Healthcare 2022, 10, 2096. https://doi.org/10.3390/healthcare10102096
Sato TdO, de Faria BSF, Albuquerque BB, Silva FLd, Rohwedder LS, de Azevedo RT, Gonçalves JS, Vieira LMSMdA, Triches MI, de Sousa RA, et al. Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort. Healthcare. 2022; 10(10):2096. https://doi.org/10.3390/healthcare10102096
Chicago/Turabian StyleSato, Tatiana de Oliveira, Beatriz Suelen Ferreira de Faria, Bianca Biason Albuquerque, Fabio Leandro da Silva, Luiza Salvador Rohwedder, Renata Trivelato de Azevedo, Josiane Sotrate Gonçalves, Ludmilla Maria Souza Mattos de Araújo Vieira, Maria Isabel Triches, Rosângela Aparecida de Sousa, and et al. 2022. "Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort" Healthcare 10, no. 10: 2096. https://doi.org/10.3390/healthcare10102096
APA StyleSato, T. d. O., de Faria, B. S. F., Albuquerque, B. B., Silva, F. L. d., Rohwedder, L. S., de Azevedo, R. T., Gonçalves, J. S., Vieira, L. M. S. M. d. A., Triches, M. I., de Sousa, R. A., Cardoso, V. d. F., & Mininel, V. A. (2022). Poor Health Conditions among Brazilian Healthcare Workers: The Study Design and Baseline Characteristics of the HEROES Cohort. Healthcare, 10(10), 2096. https://doi.org/10.3390/healthcare10102096






