The Different Patterns of Over-the-Counter Nonsteroidal Anti-Inflammatory Drugs or Analgesics Use in Patients with Chronic Kidney Disease and the General Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Patient’s Characteristics
3.1.1. CKD Cohort
3.1.2. GP Cohort
3.1.3. Basic Comparison of Study Cohorts
3.2. Comparison between CKD and GP Cohort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. The Questionnaire about OTC NSAIDs and/or Analgesics Use in CKD Patients
| Every Day | Few Times in a Week | Few Times in a Month | Once in a Month | Few Times in a Year | Once in a Year | Less Often than Once in a Year | Never | Hard to Say | |
| painkillers | |||||||||
| physiotherapy | |||||||||
| acupuncture | |||||||||
| massage | |||||||||
| psychotherapy | |||||||||
| herbal medicine | |||||||||
| other |
Appendix B. The Questionnaire about OTC NSAIDs and/or Analgesics Use in GP Population
| a. diarrhea | g. nausea |
| b. abdominal pain | h. kidney damage |
| c. headache | i. bone marrow damage |
| d. peptic ulcer | j. liver damage |
| e. allergic skin reactions such as: rash, asthma | k. blood clotting disorders |
| f. arousal or somnolence |
| doctor | I don’t believe at all 1---2---3---4---5 I believe totally |
| advertisement/media | I don’t believe at all 1---2---3---4---5 I believe totally |
| family/relatives | I don’t believe at all 1---2---3---4---5 I believe totally |
| internet | I don’t believe at all 1---2---3---4---5 I believe totally |
| dosing | unimportant 1---2---3---4---5 very important |
| price | unimportant 1---2---3---4---5 very important |
| previous experience | unimportant 1---2---3---4---5 very important |
| advertised drug efficacy | unimportant 1---2---3---4---5 very important |
Appendix C. The List of OTC NSAIDs and Analgesics Included in the Questionnaire Supplement
| Main Active Substance | Pharmaceutical Formulation (Dose) | Product Name (in Polish) | Product ID |
| acetylsalicylic acid | acidum acetylsalicylicum (300 mg); ethenezamidum (100 mg); coffeinum (50 mg) | Etopiryna | 11 |
| acidum acetylsalicylicum (400 mg); coffeinum (50 mg) | Kopiryna | 18 | |
| acidum acetylsalicylicum (450 mg); coffeinum (50 mg) | Coffepirine | 8 | |
| acidum acetylsalicylicum (500 mg) | Aspirin | 6 | |
| acidum acetylsalicylicum (500 mg); glycinum (200 mg) | Asprocol | 7 | |
| ibuprofen | dexibuprofenum (200 mg) | Seractil | 29 |
| ibuprofenum (200 mg) | Ibupar | 13 | |
| ibuprofenum (200 mg) | Ibuprofen | 14 | |
| ibuprofenum (200 mg) | Ibum | 15 | |
| ibuprofenum (200 mg) | Ibuprom Sprint Caps | 16 | |
| ibuprofenum (200 mg); codeini pfosphas (128 mg) | Nurofen Plus | 23 | |
| ibuprofenum (200 mg); pseudoephedrini hydrochloridum (30 mg) | Modafen | 19 | |
| ibuprofenum (400 mg) | Ibuprom Max | 17 | |
| ibuprofenum (400 mg) | Nurofen Ultra Forte | 22 | |
| metamizol | metamizolum natricum (500 mg) | Pyralginum | 26 |
| naproxen | naproxenum (200 mg) | Naproxen | 20 |
| naproxenum (200 mg) | Natrax 200 | 21 | |
| naproxenum natricum (200 mg) | Aleve | 2 | |
| paracetamol | paracetamolum (250 mg); propyphenazonum (150 mg); coffeinum (50 mg) | Saridon | 28 |
| paracetamolum (300 mg) | Acenol | 1 | |
| paracetamolum (500 mg) | Apap | 5 | |
| paracetamolum (500 mg) | Codipar | 9 | |
| paracetamolum (500 mg) | Efferalgan | 10 | |
| paracetamolum (500 mg) | Panadol | 25 | |
| paracetamolum (500 mg) | Paracetamol | 27 | |
| paracetamolum (500 mg); codeini phosphas (15 mg) | Antidol 15 | 3 | |
| paracetamolum (500 mg); coffeinum (30 mg); kodeine (8 mg) | Solpadeine | 30 | |
| paracetamolum (500 mg); coffeinum (65 mg) | Apap EXTRA | 4 | |
| propyhenazone | propyphenazonum (200 mg); noramidopyrine methanosulfones (300 mg) | Gardan P | 12 |
| propyphenazonum (220 mg); allobarbitalum (220 mg) | Pabialgin P | 24 |
Appendix D. Merged Questionnaires
| Figure | CKD—Questionnaire | GP—Questionnaire | ||
| Question | Answer | Question | Answer | |
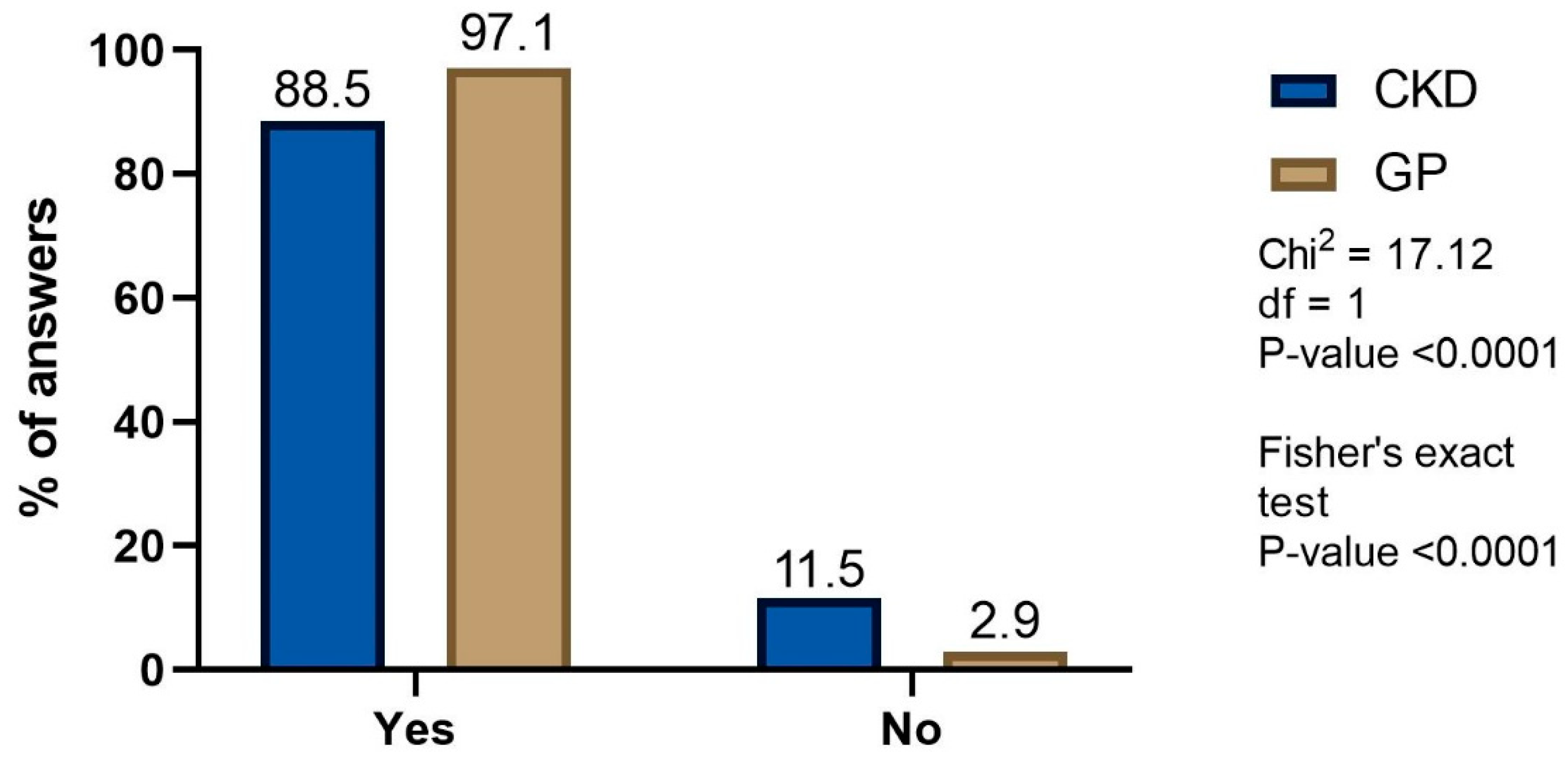
| Figure 1 | Do you use drugs for pain relief? | a. yes b. no | Do you use drugs sold over-the-counter for pain relief? | a. yes b. no |
| Figure 2 | Which of the listed drugs are you taking? (Please indicate from the most used) | a…. b… c… | Please provide the names of analgetic drugs you used?(from the most to the least frequently used) | a…. b… c… d… * c and d were merged in calculations |
| Figure 3 | You take them (painkillers) because of: (Select all appropriate variants of the answer, please) * | a. toothache c. headache d. joint pain e. menstrual pain f. back pain g. other……………….? * according to patient’s answers in variant ‘other’ we categorized the data as follow: joint and muscle pain; fever/infection; headache; spinal pain; toothache; abdominal pain; other | You take them (painkillers) because of: (you may select more than one answer) * | a. abdominal pain c. back pain d. joint pain e. toothache f. fever g. to improve the well-being h. other…………? |
| Figure 4 | When did you take over-the counter painkiller for the last time? (Mark one answer, please) | a. today b. yesterday c. this week d. this month e. during the last 6 months f. I didn’t take analgesic drugs in the last 6 months g. hard to say, I don’t remember * answer ‘g’ was not included in calculations | When was the last time you took over-the-counter painkiller? | a. today b. yesterday c. this week d. in the last month e. during the last 6 months f. I didn’t take analgesic drugs in the last 6 months |
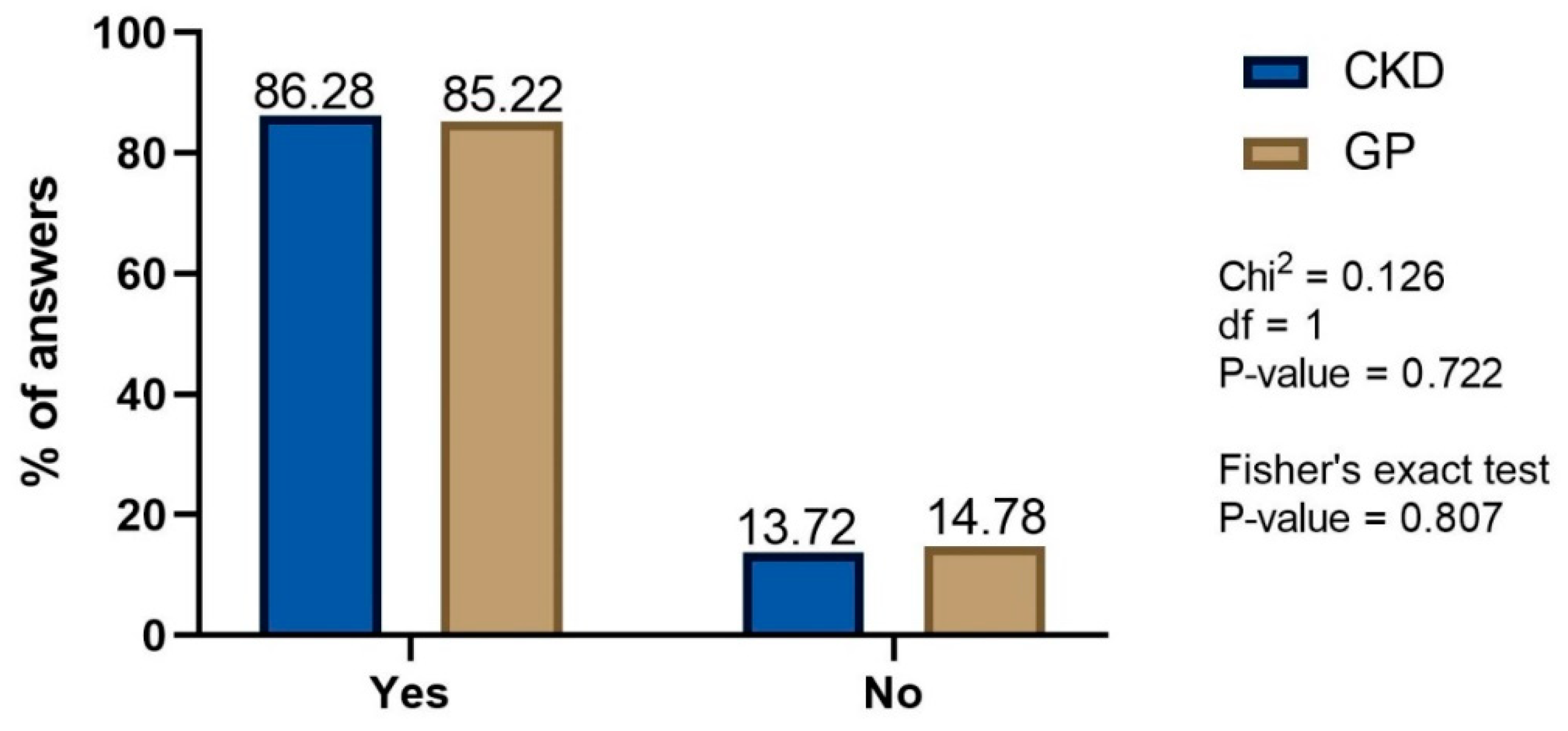
| Figure 5 | Do you think that the painkillers may cause side effects? (Mark one answer, please) | a. definitely yes b. rather yes c. sometimes d. rather no e. certainly not f. hard to say, I don’t know * a, b, c and d, e, f were merged separately in calculations | Do you think that the painkillers may cause side effects? | a. yes b. no |
| Figure 6 | Do you think that advertisement of painkillers reliably informs you about the effectiveness of the drug? (Mark one answer, please) | a. yes, always b. yes, often c. sometimes d. no, never e. hard to say * only definitive answers were compared | How strong do you believe in different sources of information * (advertisement/media) about analgesic drugs? Please grade your answers from 1 to 5. | 1—I do not believe at all 2—I believe a little 3—I believe quite a lot 4—I believe very much 5—I believe totally |
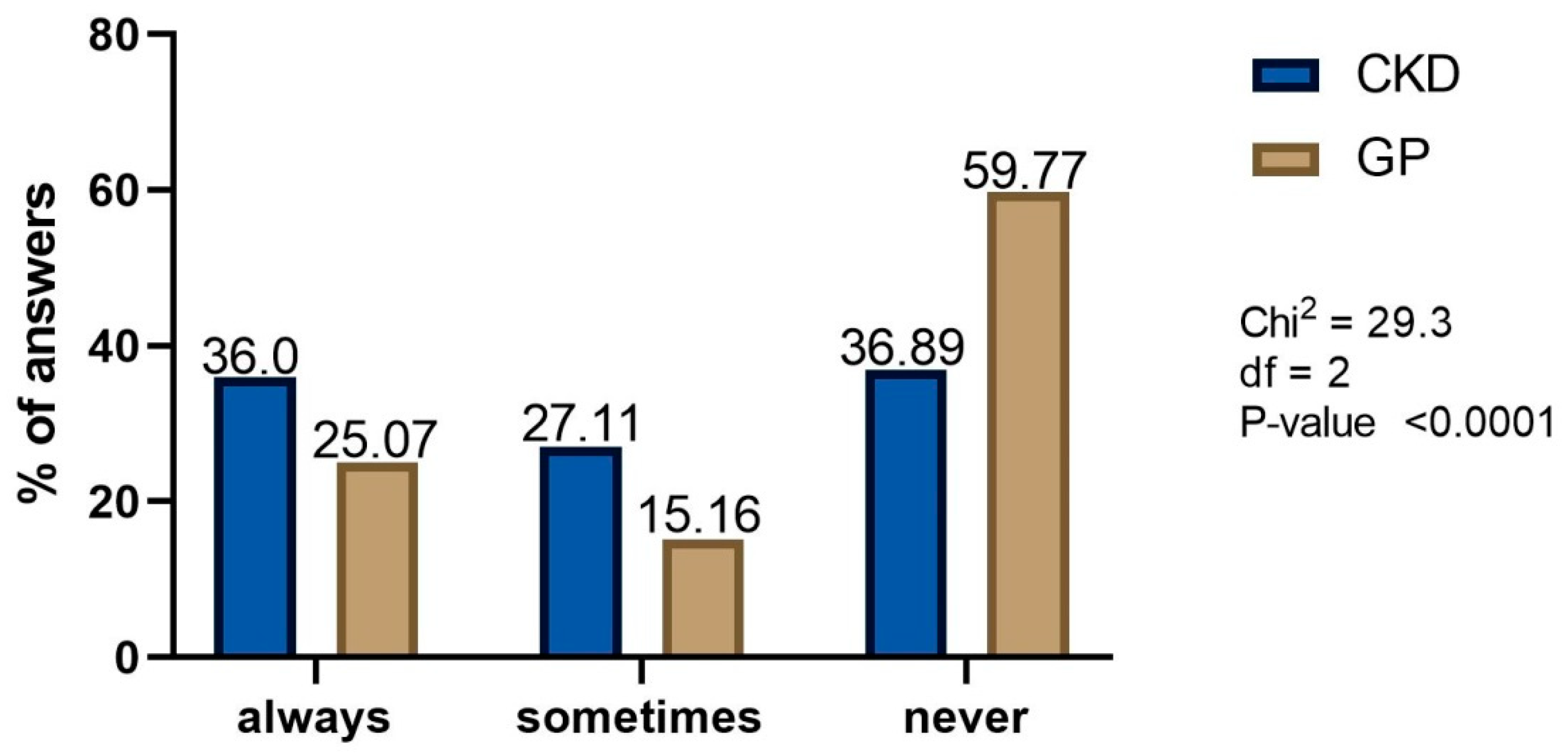
| Figure 7 | Do you consult the choice of painkiller with your doctor? (Mark one answer, please) | a. yes, always b. yes, often c. occasionally d. no, never * a and b were merged in calculations | Do you consult the choice of painkiller with your doctor? | a. always b. sometimes c. never |
| Table 1, Table 2, Table 3 and Table 4 | Metrics | |||
| Gender | a. F b. M | Please, indicate your gender | a. F b. M | |
| Date of birth (day/month/year) | …….. | Please, provide your birth date (day/month/year) | …….. | |
| What diseases do you have? (Select all appropriate variants of the answer, please) | a. hypertension b. diabetes mellitus c. gastric ulcers disease and/or duodenal ulcer d. cardiovascular diseases (ischemic heart disease, myocardial infarction) e. kidney failure f. other ………? | Which of the following diseases do you suffer from? (you may indicate more than one answer) | a. hypertension b. diabetes c. gastric and/or duodenal ulcer disease d. cardiovascular diseases (coronary disease, myocardial infarction) e. chronic renal disease f. chronic liver disease g. other ………? | |
| * do not need any explanation, this is information from author about how the questionnaires were interpreted. | ||||
References
- Available online: https://www.fortunebusinessinsights.com/non-steroidal-anti-inflammatory-drugs-nsaids-market-102823 (accessed on 18 February 2022).
- French, D.P.; James, D.H. Reasons for the use of mild analgesics among English students. Pharm. World Sci. 2008, 30, 79–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sostres, C.; Gargallo, C.J.; Arroyo, M.T.; Lanas, A. Adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs, aspirin and coxibs) on upper gastrointestinal tract. Best Pract. Res. Clin. Gastroenterol. 2010, 24, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Mulka-Gierek, M.; Foroncewicz, B.; Florczak, M.; Pączek, L.; Krawczyk, M.; Mucha, K. The use of nonsteroidal anti-inflammatory drugs and analgesics by liver transplant recipients. J. Clin. Nurs. 2016, 25, 1001–1005. [Google Scholar] [CrossRef]
- Mulka-Gierek, M.; Foroncewicz, B.; Pączek, L.; Wawiórko, E.; Kamińska, J.; Kosieradzki, M.; Małkowski, P.; Małczuk, B.; Nazarewski, S.; Mucha, K. Nonsteroidal Anti-Inflammatory Drugs and Analgesics Use by Kidney Transplant Recipients. Ann. Transplant. 2018, 23, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Bindu, S.; Mazumder, S.; Bandyopadhyay, U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective. Biochem. Pharmacol. 2020, 180, 114147. [Google Scholar] [CrossRef]
- Cairns, R.; Brown, J.A.; Buckley, N.A. The impact of codeine re-scheduling on misuse: A retrospective review of calls to Australia’s largest poisons centre. Addiction 2016, 111, 1848–1853. [Google Scholar] [CrossRef]
- Chatterjee, S.; Dureja, G.P.; Kadhe, G.; Mane, A.; Phansalkar, A.A.; Sawant, S.; Kapatkar, V. Cross-Sectional Study for Prevalence of Non-Steroidal Anti-Inflammatory Drug-Induced Gastrointestinal, Cardiac and Renal Complications in India: Interim Report. Gastroenterol. Res. 2015, 8, 216–221. [Google Scholar] [CrossRef] [Green Version]
- Shin, S.J.; Noh, C.K.; Lim, S.G.; Lee, K.M.; Lee, K.J. Non-steroidal anti-inflammatory drug-induced enteropathy. Intest. Res. 2017, 15, 446–455. [Google Scholar] [CrossRef] [Green Version]
- Maiden, L.; Thjodleifsson, B.; Theodors, A.; Gonzalez, J.; Bjarnason, I. A quantitative analysis of NSAID-induced small bowel pathology by capsule enteroscopy. Gastroenterology 2005, 128, 1172–1178. [Google Scholar] [CrossRef]
- Roumie, C.L.; Choma, N.N.; Kaltenbach, L.; Mitchel, E.F., Jr.; Arbogast, P.G.; Griffin, M.R. Non-aspirin NSAIDs, cyclooxygenase-2 inhibitors and risk for cardiovascular events-stroke, acute myocardial infarction, and death from coronary heart disease. Pharmacoepidemiol. Drug Saf. 2009, 18, 1053–1063. [Google Scholar] [CrossRef]
- Rane, M.A.; Gitin, A.; Fiedler, B.; Fiedler, L.; Hennekens, C.H. Risks of Cardiovascular Disease and Beyond in Prescription of Nonsteroidal Anti-Inflammatory Drugs. J. Cardiovasc. Pharmacol. Ther. 2020, 25, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Alajbegovic, A.; Gomes, A.V. NSAIDs and Cardiovascular Diseases: Role of Reactive Oxygen Species. Oxid. Med. Cell. Longev. 2015, 2015, 536962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schjerning, A.M.; McGettigan, P.; Gislason, G. Cardiovascular effects and safety of (non-aspirin) NSAIDs. Nat. Rev. Cardiol. 2020, 17, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Schink, T.; Kollhorst, B.; Varas Lorenzo, C.; Arfè, A.; Herings, R.; Lucchi, S.; Romio, S.; Schade, R.; Schuemie, M.J.; Straatman, H.; et al. Risk of ischemic stroke and the use of individual non-steroidal anti-inflammatory drugs: A multi-country European database study within the SOS Project. PLoS ONE 2018, 13, e0203362. [Google Scholar] [CrossRef] [Green Version]
- Goetz, D.W.; Jacobson, J.M.; Murnane, J.E.; Reid, M.J.; Repperger, D.W.; Goodyear, C.; Martin, M.E. Prolongation of simple and choice reaction times in a double-blind comparison of twice-daily hydroxyzine versus terfenadine. J. Allergy Clin. Immunol. 1989, 84, 316–322. [Google Scholar] [CrossRef]
- Potamianos, G.; Kellett, J.M. Anti-cholinergic drugs and memory: The effects of benzhexol on memory in a group of geriatric patients. Br. J. Psychiatry 1982, 140, 470–472. [Google Scholar] [CrossRef]
- Baker, M.; Perazella, M.A. NSAIDs in CKD: Are They Safe? Am. J. Kidney Dis. 2020, 76, 546–557. [Google Scholar] [CrossRef]
- Stosic, R.; Dunagan, F.; Palmer, H.; Fowler, T.; Adams, I. Responsible self-medication: Perceived risks and benefits of over-the-counter analgesic use. Int. J. Pharm. Pract. 2011, 19, 236–245. [Google Scholar] [CrossRef]
- Axmon, A.; Ahlstrom, G.; Westergren, H. Pain and Pain Medication among Older People with Intellectual Disabilities in Comparison with the General Population. Healthcare 2018, 6, 67. [Google Scholar] [CrossRef] [Green Version]
- Perpetuo, C.; Placido, A.I.; Aperta, J.; Herdeiro, M.T.; Roque, F. Profile of Prescription Medication in an Internal Medicine Ward. Healthcare 2021, 9, 704. [Google Scholar] [CrossRef]
- Hamilton, K.; Davis, C.; Falk, J.; Singer, A.; Bugden, S. High risk use of OTC NSAIDs and ASA in family medicine: A retrospective chart review. Int. J. Risk Saf. Med. 2015, 27, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.C.; Mohajir, N.; Meltzer, D.O. Consumers’ perceptions about risk of and access to nonprescription medications. J. Am. Pharm. Assoc. 2005, 45, 363–370. [Google Scholar] [CrossRef] [PubMed]




| Demographic Data | ||
| Age | mean (SD) | 60.5 (16.0) |
| range | 19.0–91 | |
| median (IQR) | 63.0 (50–72) | |
| Gender, n (%) | Female | 141 (62.4) |
| Male | 85 (37.6) | |
| BMI | mean (SD) | 28.0 (4.7) |
| range | 17.1–39.9 | |
| median (IQR) | 63 (24.9–31.1) | |
| Employment status, n (%) | Active | 80 (35.4) |
| Unemployed or retired | 146 (64.6) | |
| Clinical Data | ||
| Disease etiology, n (%) | Unknown etiology | 65 (30.7) |
| IgA nephropathy/HSP Nephritis | 24 (10.6) | |
| Diabetic kidney disease | 22 (9.7) | |
| Focal segmental glomerulosclerosis | 21 (9.3) | |
| Polycystic kidney disease | 21 (9.3) | |
| Nephrectomy | 17 (7.5) | |
| Systemic lupus erythematosus | 14 (6.2) | |
| Urinary tract infections | 14 (6.2) | |
| Membranous nephropathy | 9 (3.9) | |
| Urolithiasis | 8 (3.5) | |
| Membranoproliferative glomerulonephritis | 6 (2.6) | |
| Other glomerulonephritis | 5 (2.2) | |
| Comorbidities, n (%) | Diabetes Mellitus | 67 (29.6) |
| Hypertension | 180 (79.6) | |
| Other | 221 (97.8) | |
| Laboratory Results | ||
| Serum creatinine (mg/dL) | mean (SD) | 1.45 (0.9) |
| eGFR (mL/min/1.73 m2) | mean (SD) | 58.16 (27.9) |
| Protein (g/24 h urine sample, n = 108) | mean (SD) | 0.82 (1.17) |
| Hemoglobin (mg/dL) | mean (SD) | 14.17 (9.53) |
| Platelets (L/L) | mean (SD) | 244.8 (70.8) |
| Albumin (g/dL), serum | mean (SD) | 5.4 (4.4) |
| Years before the Survey | |||||
|---|---|---|---|---|---|
| −5 | −3 | −1 | Delta (Difference) | p-Value | |
| Serum creatinine, (mg/dL) | 1.35 (0.49) | 1.42 (0.70) | 1.47 (0.71) | +0.12 | 0.35 |
| eGFR, (mL/min/1.73 m2) | 60.6 (27.1) | 57.6 (27.5) | 54.4 (25.3) | −6.2 | 0.21 |
| Demographic and Clinical Data | ||
|---|---|---|
| Age | mean (SD) | 49 (14.8) |
| range | 24–92 | |
| median (IQR) | 47.00 (35–61) | |
| Gender, n (%) | Female | 197 (57.0) |
| Male | 148 (43.0) | |
| Comorbidities, n (%) | Diabetes Mellitus | 43 (12.5) |
| Hypertension | 122 (35.4) | |
| Other | 67 (19.4) | |
| Residence, n (%) | Village | 70 (20.3) |
| Town < 100 k inhabitants | 62 (18.0) | |
| Town >100 k inhabitants | 212 (61.6) | |
| Education, n (%) | High school | 168 (48.8) |
| Bachelor’s or Master’s degree | 83 (24.1) | |
| Primary (8th grade) | 58 (16.9) | |
| Vocational (10th grade) | 35 (10.2) | |
| Demographic and Clinical Data | CKD | GP | p-Value | |
|---|---|---|---|---|
| Age | mean (SD) | 60.5 (16.0) | 49 (14.8) | <0.0001 a |
| range | 19.0–91 | 24–92 | ||
| median (IQR) | 63.0 (50–72) | 47.00 (35–61) | ||
| Gender, n (%) | Female | 141 (62.4) | 197 (57.0) | 0.2986 b |
| Male | 85 (37.6) | 148 (43.0) | ||
| Comorbidities, n (%) | Diabetes Mellitus | 67 (29.6) | 43 (12.5) | <0.0001 b |
| Hypertension | 180 (79.6) | 122 (35.4) | <0.0001 b | |
| Medication | Answer’s Statistics | Frequency | |||||
|---|---|---|---|---|---|---|---|
| A | B | C | |||||
| Group | |||||||
| GP | CKD | GP | CKD | GP | CKD | ||
| paracetamol | Yes, n (%) | 202 (59.6) | 146 (71.57) | 109 (41.44) | 45 (34.09) | 94 (25.68) | 15 (22.39) |
| p-value | 0.0048 a | 0.1575 a | 0.5678 a | ||||
| 0.0055 b | 0.1893 b | 0.6474 b | |||||
| ibuprofen | Yes, n (%) | 113 (33.33) | 16 (7.84) | 117 (44.49) | 40 (30.30) | 201 (54.92) | 15 (22.39) |
| p-value | <0.0001 a | 0.0066 a | <0.0001 a | ||||
| <0.0001 b | 0.0066 b | <0.0001 b | |||||
| acetylsalicylic acid | Yes, n (%) | 4 (1.18) | 28 (13.73) | 11 (4.18) | 31 (23.49) | 26 (7.1) | 15 (22.39) |
| p-value | <0.0001 a | <0.0001 a | <0.0001 a | ||||
| <0.0001 b | <0.0001 b | 0.0004 b | |||||
| naproxen | Yes, n (%) | 15 (4.42) | 2 (0.98) | 24 (9.13) | 3 (2.27) | 33 (9.02) | 1 (1.49) |
| p-value | 0.0256 a | 0.0109 a | 0.0353 a | ||||
| 0.0384 b | 0.0104 b | 0.044 b | |||||
| Medication | CKD | p-Value | GP | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||||
| n (%) | n (%) | |||||||||
| paracetamol | 99 | (75.00) | 47 | (65.28) | 0.141 a | 113 | (57.36) | 94 | (63.51) | 0.248 a |
| 0.148 b | 0.268 b | |||||||||
| acetylsalicylic acid | 10 | (7.58) | 18 | (25.00) | 0.0005 a | 3 | (1.52) | 1 | (0.68) | 0.467 a |
| 0.001 b | 0.638 b | |||||||||
| ibuprofen | 10 | (7.58) | 6 | (8.33) | 0.847 a | 70 | (35.53) | 43 | (29.05) | 0.204 a |
| 0.999 b | 0.246 b | |||||||||
| metamizol | 11 | (8.33) | 1 | (1.39) | 0.044 a | 0 | (0.00) | 0 | (0.00) | n.a. |
| 0.059 b | ||||||||||
| naproxen | 2 | (1.52) | 0 | (0.00) | n.a. | 9 | (4.57) | 6 | (4.05) | 0.817 a |
| 0.999 b | ||||||||||
| propyphenazone | 0 | (0.00) | 0 | (0.00) | n.a. | 2 | (1.02) | 4 | (2.70) | n.a. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mulka-Gierek, M.; Krata, N.; Foroncewicz, B.; Pączek, L.; Mucha, K. The Different Patterns of Over-the-Counter Nonsteroidal Anti-Inflammatory Drugs or Analgesics Use in Patients with Chronic Kidney Disease and the General Population. Healthcare 2022, 10, 2035. https://doi.org/10.3390/healthcare10102035
Mulka-Gierek M, Krata N, Foroncewicz B, Pączek L, Mucha K. The Different Patterns of Over-the-Counter Nonsteroidal Anti-Inflammatory Drugs or Analgesics Use in Patients with Chronic Kidney Disease and the General Population. Healthcare. 2022; 10(10):2035. https://doi.org/10.3390/healthcare10102035
Chicago/Turabian StyleMulka-Gierek, Maria, Natalia Krata, Bartosz Foroncewicz, Leszek Pączek, and Krzysztof Mucha. 2022. "The Different Patterns of Over-the-Counter Nonsteroidal Anti-Inflammatory Drugs or Analgesics Use in Patients with Chronic Kidney Disease and the General Population" Healthcare 10, no. 10: 2035. https://doi.org/10.3390/healthcare10102035
APA StyleMulka-Gierek, M., Krata, N., Foroncewicz, B., Pączek, L., & Mucha, K. (2022). The Different Patterns of Over-the-Counter Nonsteroidal Anti-Inflammatory Drugs or Analgesics Use in Patients with Chronic Kidney Disease and the General Population. Healthcare, 10(10), 2035. https://doi.org/10.3390/healthcare10102035







