Effect of Household Type on the Prevalence of Metabolic Syndrome in Korea: Using Propensity Score Matching
Abstract
:1. Introduction
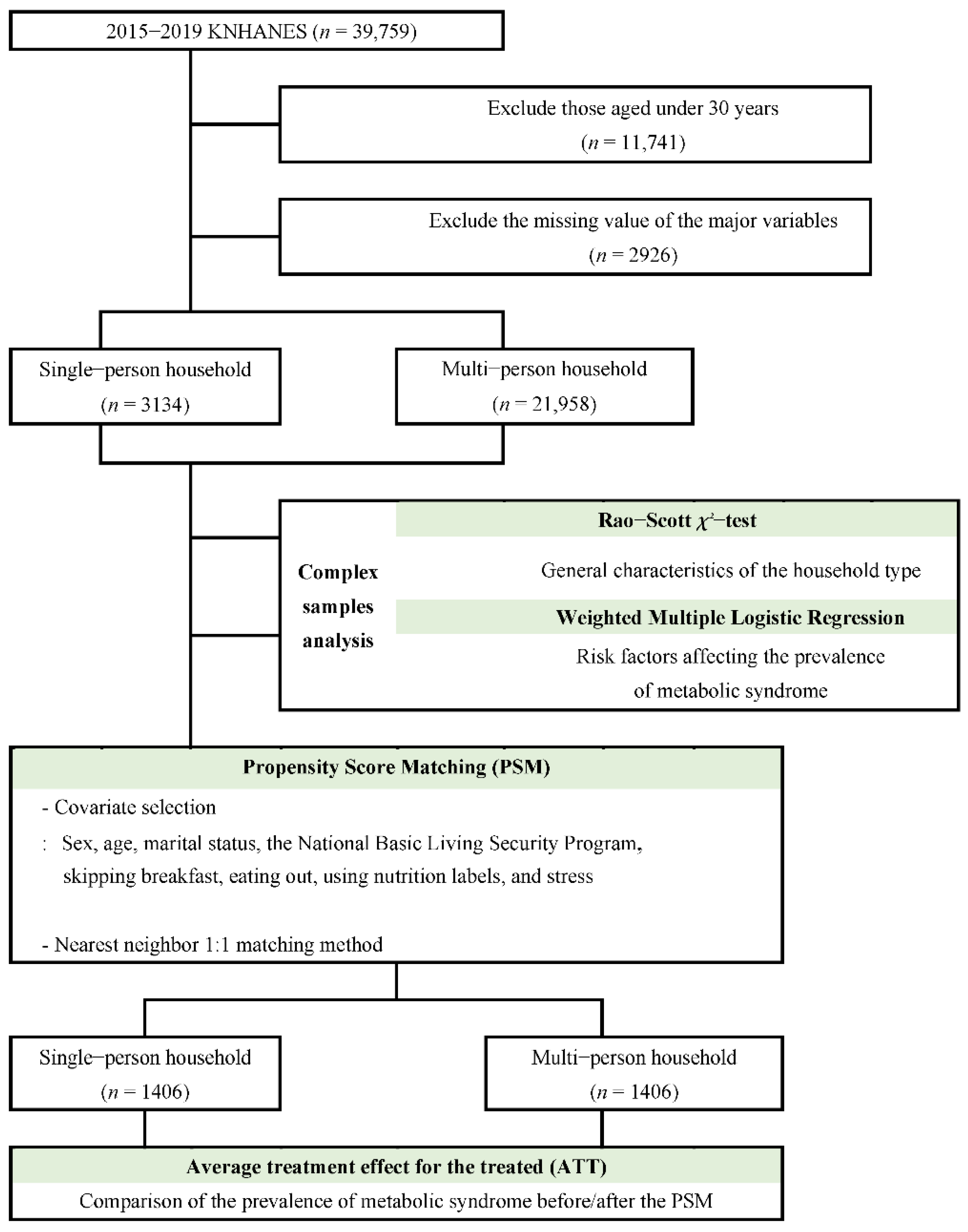
2. Materials and Methods
2.1. Subjects and Data Collection
2.2. Research Variables
2.3. Statistical Analysis
3. Results
3.1. General Characteristics of the Subjects
3.2. Analysis of the Factors Affecting the Prevalence of the Metabolic Syndrome
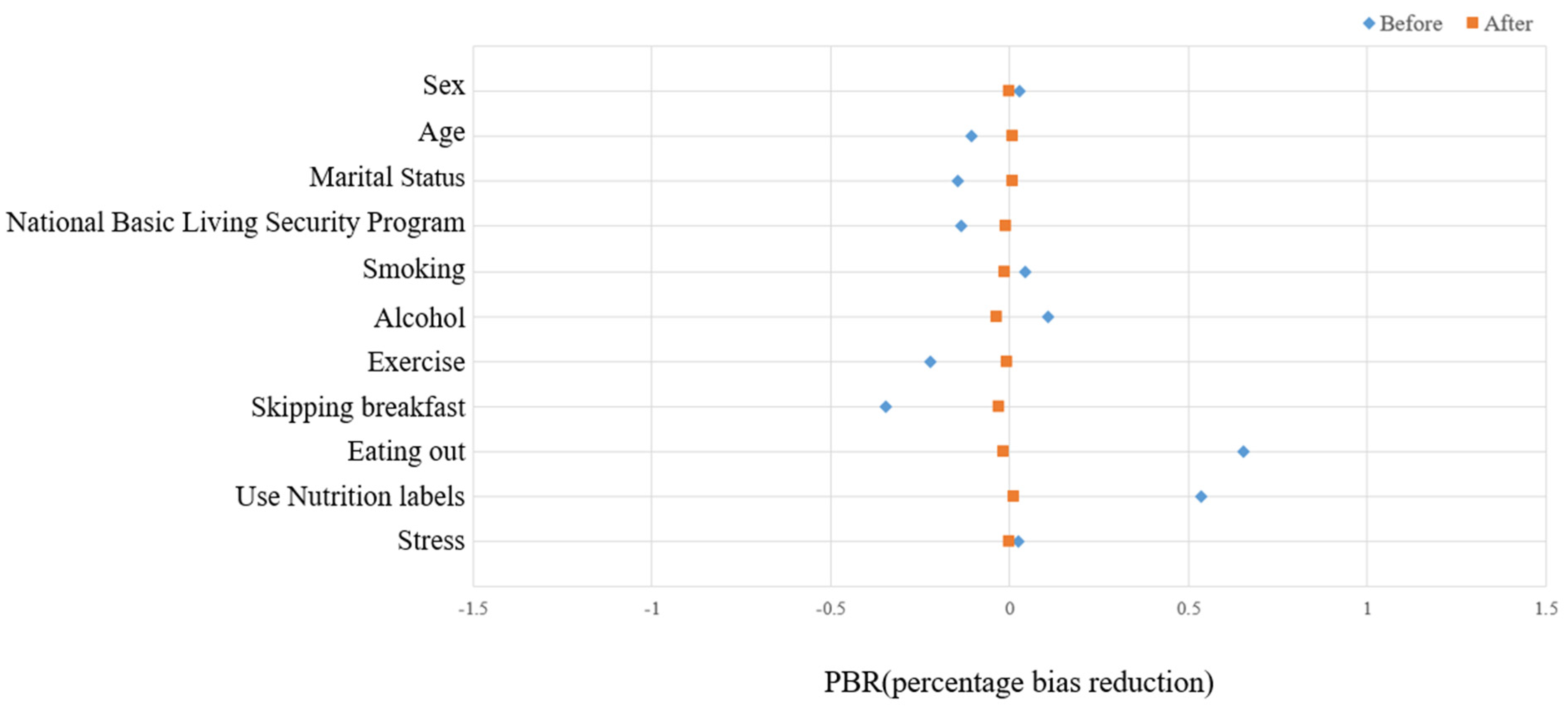
3.3. Propensity Score Matching
3.4. Analysis of the Difference in the Prevalence of Metabolic Syndrome by Household Type before and after PSM
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Korean Statistical Information Service (KOSIS). Population and Housing Census 2020; KOSIS: Daejeon, Korea, 2020. [Google Scholar]
- Korean Statistical Information Service (KOSIS). Household Projections 2020; KOSIS: Daejeon, Korea, 2020. [Google Scholar]
- Organization for Economic Cooperation and Development (OECD). OECD Family Database; OECD Publishing: Paris, France, 2013. [Google Scholar]
- Lee, M.J. Policy trends on one-person household in European countries. Glob. Soc. Secur. Rev. 2019, 11, 16–26. [Google Scholar] [CrossRef]
- Jung, S.H. The Latest Trends of Single-person Households Related Policy in U.S.A. Glob. Soc. Secur. Rev. 2019, 11, 37–49. [Google Scholar] [CrossRef]
- Oh, Y.J. Considering single households for new health vulnerable groups. Wkly. Issue 2017, 4, 1–8. [Google Scholar]
- Berkman, L.F. Social support, social networks, social cohesion and health. Soc. Work Health Care 2000, 31, 3–14. [Google Scholar] [CrossRef]
- Lee, M.H.; Kang, E.N. Single-Person Households in South Korea and Their Policy Implications. Health Commun. Welf Policy Forum 2016, 234, 47–56. [Google Scholar]
- Song, E.G.; Yoon, Y.S.; Yang, Y.J.; Lee, E.S.; Lee, J.H.; Lee, J.Y.; Park, W.J.; Park, S.Y. Factors associated with eating alone in Korean adults: Findings from the sixth Korea National Health and Nutrition Examination Survey, 2014. Korean J. Fam. Pract. 2017, 7, 698–706. [Google Scholar] [CrossRef]
- Lee, M.K.; Han, K.D.; Kim, M.K.; Koh, E.S.; Kim, E.S.; Nam, G.E.; Kwon, H.S. Changes in metabolic syndrome and its components and the risk of type 2 diabetes: A nationwide cohort study. Sci. Rep. 2020, 10, 2313. [Google Scholar] [CrossRef]
- Felix, F.L.; John, D.L.; Ewgenij, P. Multi-Target Approaches in Metabolic Syndrome. Front. Pharmacol. 2021, 11, 554961. [Google Scholar] [CrossRef]
- Kim, S.H.; Kim, Y.L.; Kim, K.W.; Kim, K.H. The health behavior of single adult households in Korean over 30: The 6th Korean National Health and Nutrition Examination Survey. Korean J. Fam. Pract. 2017, 7, 330–336. [Google Scholar] [CrossRef]
- Park, E.O.; Choi, S.J.; Lee, H.Y. The prevalence of metabolic syndrome and related risk factors based on the KNHANES V 2010. J. Agric. Med. Community Health 2013, 38, 1–13. [Google Scholar] [CrossRef]
- Kim, S.H. The relationship between socioeconomic status and metabolic syndrome, using structural equation modelling. Korean J. Health Promot. 2016, 16, 92–100. [Google Scholar] [CrossRef]
- Park, J.K.; Kweon, S.H.; Kim, Y.H.; Jang, M.J.; Oh, K.W. Dietary behaviors related to metabolic syndrome in Korean adults. Korean J. Community Nutr. 2012, 17, 664–675. [Google Scholar] [CrossRef]
- Kim, C.G.; Kim, Y.G. The prevalence and associated factors of the metabolic syndrome in pre-menopausal housewives: An analysis of the 2010~2015 Korean National Health and Nutrition Examination Survey. J. Korean Acad. Community Health Nurs. 2018, 29, 108–119. [Google Scholar] [CrossRef]
- Chung, T.H.; Kim, M.C.; Choi, C.H.; Kim, C.S. The association between marital status and metabolic syndrome in Korean men. Korean J. Fam. Med. 2010, 31, 208–214. [Google Scholar] [CrossRef]
- Im, M.Y. The effect of stress on prevalence risk of metabolic syndrome among Korean adults. Korean J. Stress Res. 2019, 27, 441–447. [Google Scholar] [CrossRef]
- Oh, E.J.; Joh, H.G.; Lee, R.; Do, H.J.; Oh, S.W.; Lym, Y.L.; Choi, J.K.; Kweon, H.J.; Cho, D.Y. Relations between the dietary habits and components of the metabolic syndrome in premenopausal women. J. Korean Acad. Fam. Med. 2008, 29, 746–761. [Google Scholar]
- Choi, J.H. Assessment of Dietary Behaviors and Nutrient Intakes Levels by a Degree of Metabolic Syndrome Risk for Premenopausal Women. Master’s Thesis, EWHA Women’s University, Seoul, Korea, 2015. [Google Scholar]
- Kim, D.I. The relationship between walking activity per week, metabolic syndrome risk factors, and prevalence of metabolic syndrome in Korean adult population: Data from the fifth Korea National Health and Nutrition Examination Survey. J. Korean Soc. Living Environ. Syst. 2015, 22, 58–65. [Google Scholar] [CrossRef]
- Kim, Y.H. Risk factors related to metabolic syndrome among preparation stage to smoking cessation in men. J. Korean Data Anal. Soc. 2012, 14, 2555–2568. [Google Scholar]
- Jung, C.H.; Park, J.S.; Lee, W.Y.; Kim, S.W. Effects of smoking, alcohol, exercise, level of education, and family history on the metabolic syndrome in Korean adults. Korean J. Med. 2022, 63, 649–659. [Google Scholar]
- Jung, J.W.; Kim, C.H.; Shin, H.C.; Park, Y.W.; Sung, E.J.; Cheong, S.Y. The relationship between metabolic syndrome, stress and depression—Among the 35–64 years old clients of comprehensive medical examination center in one university hospital. Korean J. Health Promot. Dis. Prev. 2004, 4, 10–17. [Google Scholar]
- Kaufman, J.S.; Kaufman, S.; Poole, C. Causal inference from randomized trials in social epidemiology. Soc. Sci. Med. 2003, 57, 2397–2409. [Google Scholar] [CrossRef]
- Byun, G.S.; Lee, H.W. The impact of employment instability on mental health: The case of South Korea. Health Soc. Welf. Rev. 2018, 38, 129–160. [Google Scholar] [CrossRef]
- Kim, A.R.; Choi, M.H. Effects of disability on the prevalence of hypertension and diabetes. Korean Data Anal. Soc. 2018, 20, 1503–1517. [Google Scholar] [CrossRef]
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Lee, D.K. An introduction to propensity score matching methods. Anesth. Pain Med. 2016, 11, 130–148. [Google Scholar] [CrossRef]
- Becker, S.O.; Ichino, A. Estimation of average treatment effects based on propensity scores. Stata J. 2002, 2, 358–377. [Google Scholar] [CrossRef] [Green Version]
- Azadbakht, L.; Mirmiran, P.; Esmaillzadeh, A.; Azizi, T.; Azizi, F. Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome. Diabetes Care 2005, 28, 2823–2831. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.; Ceriello, A.; Esposito, K. The effects of diet on inflammation: Emphasis on the metabolic syndrome. J. Am. Coll. Cardiol. 2006, 48, 677–685. [Google Scholar] [CrossRef]
- Hu, F.B.; Li, T.Y.; Colditz, G.A.; Willett, W.C.; Manson, J.E. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003, 289, 1785–1791. [Google Scholar] [CrossRef] [PubMed]
- Wirfält, E.; Hedblad, B.; Gullberg, B.; Mattisson, I.; Andrén, C.; Rosander, U.; Janzon, L.; Berglund, G. Food patterns and components of the metabolic syndrome in men and women: A cross-sectional study within the Malmӧ diet and cancer cohort. Am. J. Epidemiol. 2001, 154, 1150–1159. [Google Scholar] [CrossRef]
- Henriksen, E.J. Invited review: Effects of acute exercise and exercise training on insulin resistance. J. Appl. Physiol. 2002, 93, 788–796. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Jousilahti, P.; Borodulin, K.; Barengo, N.C.; Lakka, T.A.; Nissinen, A.; Tuomilehto, J. Occupational, commuting and leisure-time physical activity in relation to coronary heart disease among middle-aged Finnish men and women. Atherosclerosis 2007, 194, 490–497. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.Y.; Park, J.S.; Noh, S.Y.; Rhee, E.J.; Kim, S.W.; Zimmet, P.Z. Prevalence of the metabolic syndrome among 40,698 Korean metropolitan subjects. Diabetes Res. Clin. Pract. 2004, 65, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Oh, E.G.; Bang, S.Y.; Hyun, S.S.; Chu, S.H.; Jeon, J.Y.; Kang, M.S. Knowledge, perception and health behavior about metabolic syndrome for an at risk group in a rural community area. J. Korean Acad. Nurs. 2007, 37, 790–800. [Google Scholar] [CrossRef]
- Kim, Y.H.; Yang, Y.O. Effects of walking exercise on metabolic syndrome risk factors and body composition in obese middle school girls. J. Korean Acad. Nurs. 2005, 35, 858–867. [Google Scholar] [CrossRef]
| Factor | Variable | Description |
|---|---|---|
| Dependent variable | Metabolic syndrome | Three or more diagnostic criteria for metabolic syndrome |
| Independent variable | Household type | Single-person household, multi-person household (two or more family members) |
| Demographic characteristics | Gender | Male, female |
| Age | Over 30 years old | |
| Marital status | Married, unmarried | |
| National Basic Living Security Program | Yes (previous or current), No | |
| Health behavior characteristics | Smoking | Smoked 5 packs (100 cigarettes) or more in his/her life and currently smoking |
| Drinking | History of drinking more than once a month in the past year | |
| Aerobic physical activity | Moderate-intensity physical activity for at least 2 h and 30 min, high-intensity physical activity for at least 1 h and 15 min, or a mix of moderate- and high-intensity physical activities for a proportionate amount of time during the week | |
| Skipping breakfast | History of eating breakfast in the past year | |
| Eating out | Eating out more than once a week | |
| Using nutrition labels | Using nutrition labels when buying or choosing processed foods | |
| Mental health | Stress | Stress in daily life |
| Factors | Single-Person Household | Multi-Person Household | Rao–Scott χ² | p- Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | Na | (%) | n | (%) | Na | (%) | |||||
| Total | 3134 | (100.0) | 3,251,512 | (100.0) | 21,958 | (100.0) | 29,052,901 | (100.0) | ||||
| Demographic and social characteristics | Sex | Male | 1131 | (36.1) | 1,469,241 | (45.2) | 9656 | (44.0) | 14,220,000 | (49.0) | 8.17 | <0.0001 |
| Female | 2003 | (63.9) | 1,782,271 | (54.8) | 12,302 | (56.0) | 14,830,000 | (51.1) | ||||
| Age (Mean ± SD) | 63.5 ± 0.4 | 58.8 ± 0.5 | 54.1 ± 0.2 | 51.4 ± 0.2 | 949.29 | <0.0001 | ||||||
| Marital Status | Married | 2529 | (80.7) | 2,299,644 | (70.7) | 20,889 | (95.1) | 27,220,000 | (93.7) | 822.08 | <0.0001 | |
| Unmarried | 605 | (19.3) | 951,868 | (29.3) | 1069 | (4.9) | 1,837,243 | (6.3) | ||||
| National Basic Living Security Program | Yes | 613 | (19.6) | 559,566 | (17.2) | 1112 | (5.1) | 1,395,204 | (4.8) | 411.07 | <0.0001 | |
| No | 2519 | (80.4) | 2,691,069 | (82.8) | 20,843 | (94.9) | 27,650,000 | (95.2) | ||||
| Health behavior characteristics | Smoking | Yes | 618 | (19.9) | 846,511 | (26.2) | 3616 | (16.5) | 5,660,882 | (19.6) | 37.66 | <0.0001 |
| No | 2488 | (80.1) | 2,381,306 | (73.8) | 18,251 | (83.5) | 23,280,000 | (80.4) | ||||
| Alcohol | Yes | 1320 | (42.4) | 1,621,795 | (50.2) | 11,658 | (53.3) | 16,510,000 | (57.0) | 31.88 | <0.0001 | |
| No | 1790 | (57.6) | 1,609,111 | (49.8) | 10,217 | (46.7) | 12,440,000 | (43.0) | ||||
| Exercise | Yes | 1060 | (34.1) | 1,222,139 | (37.8) | 9202 | (42.0) | 12,740,000 | (44.0) | 26.83 | <0.0001 | |
| No | 2051 | (65.9) | 2,010,005 | (62.2) | 12,698 | (58.0) | 16,240,000 | (56.0) | ||||
| Skipping breakfast | No | 2481 | (87.6) | 2,435,469 | (83.9) | 17,259 | (89.4) | 21,910,000 | (87.6) | 17.44 | <0.0001 | |
| Yes | 351 | (12.4) | 465,968 | (16.1) | 2037 | (10.6) | 3,095,662 | (12.4) | ||||
| Eating out | Yes | 1651 | (58.3) | 1,893,088 | (65.3) | 13,728 | (71.2) | 18,950,000 | (75.8) | 93.76 | <0.0001 | |
| No | 1181 | (41.7) | 1,008,349 | (34.8) | 5567 | (28.9) | 6,053,438 | (24.2) | ||||
| Using nutrition labels | Yes | 432 | (29.8) | 554,708 | (32.3) | 4922 | (34.8) | 6,738,336 | (34.9) | 2.32 | 0.1277 | |
| No | 1018 | (70.2) | 1,164,419 | (67.7) | 9232 | (65.2) | 12,560,000 | (65.1) | ||||
| Mental health | Stress | Yes | 758 | (24.4) | 846,513 | (26.2) | 5569 | (25.5) | 7,763,267 | (26.8) | 0.33 | 0.5629 |
| No | 2347 | (75.6) | 2,058,370 | (63.3) | 16,293 | (74.5) | 21,170,000 | (73.2) | ||||
| Disease | Metabolic syndrome | Yes | 1192 | (38.0) | 1,148,837 | (35.3) | 6243 | (28.4) | 7,772,633 | (26.8) | 65.94 | <0.0001 |
| No | 1942 | (62.0) | 2,102,675 | (64.7) | 15,715 | (69.7) | 21,280,000 | (73.3) | ||||
| Factors | MS | |||
|---|---|---|---|---|
| OR a | 95% CI b | |||
| Demographic and social characteristics | Sex | Male (Ref) | 1 | - |
| Female | 0.56 *** | (0.50–0.62) | ||
| Age | 1.51 *** | (1.45–1.57) | ||
| Marital status | Married (Ref) | 1 | - | |
| Unmarried | 1.09 | (0.89–1.33) | ||
| National Basic Living Security Program | Yes | 1.34 ** | (1.09–1.65) | |
| No (Ref) | 1 | - | ||
| Health behavior characteristics | Smoking | Yes | 1.24 ** | (1.10–1.41) |
| No (Ref) | 1 | - | ||
| Alcohol | Yes | 1.04 | (0.94–1.15) | |
| No (Ref) | 1 | - | ||
| Exercise | Yes | 1 | - | |
| No | 1.21 ** | (1.10–1.33) | ||
| Skipping breakfast | No (Ref) | 1 | - | |
| Yes | 1.19 * | (1.03–1.36) | ||
| Eating out | Yes | 0.90 | (0.80–1.01) | |
| No (Ref) | 1 | - | ||
| Using nutrition labels | Yes (Ref) | 1 | - | |
| No | 1.07 | (0.97–1.18) | ||
| Mental health | Stress | Yes | 1.29 *** | (1.16–1.42) |
| No (Ref) | 1 | - | ||
| Household type | One person | 1.02 | (0.87–1.19) | |
| Multi person (Ref) | 1 | - | ||
| Factors | Before Matching (n = 25,092) | SMD b | p- Value | After Matching (n = 2812) | SMD | p- Value | PBR c | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Single-Person Household | Multi-Person Household | Single-Person Household | Multi-Person Household | ||||||||||||
| Na | (%) | Na | (%) | Na | (%) | Na | (%) | ||||||||
| Total | 3,251,512 | (100.0) | 29,052,901 | (100.0) | 1,667,732 | (100.0) | 1,817,642 | (100.0) | |||||||
| Demographic and social characteristics | Sex | Male | 1,469,241 | (45.2) | 14,220,000 | (49.0) | 0.02 | <0.0001 | 832,963 | (50.0) | 832,787 | (45.8) | 0.00 | 0.0757 | 100.0 |
| Female | 1,782,271 | (54.8) | 14,830,000 | (51.1) | 834,768 | (50.1) | 984,855 | (54.2) | |||||||
| Age (Mean ± SD) | 58.8 ± 0.5 | 51.4 ± 0.2 | 0.54 | <0.0001 | 52.8 ± 0.6 | 53.6 ± 0.5 | 0.01 | <0.0001 | 97.7 | ||||||
| Marital status | Married | 2,299,644 | (70.7) | 27,220,000 | (93.7) | 0.65 | <0.0001 | 1,028,450 | (61.7) | 1,181,028 | (65.0) | −0.02 | 0.1735 | 97.6 | |
| Unmarried | 951,868 | (29.3) | 1,837,243 | (6.3) | 1,667,732 | (38.3) | 636,613 | (35.0) | |||||||
| National Basic Living Security Program | Yes | 559,566 | (17.2) | 1,395,204 | (4.8) | −0.35 | <0.0001 | 174,624 | (10.5) | 183,081 | (10.1) | −0.03 | 0.7871 | 91.1 | |
| No | 2,691,069 | (82.8) | 27,650,000 | (95.2) | 1,493,108 | (89.5) | 1,634,560 | (89.9) | |||||||
| Health behavior characteristics | Smoking | Yes | 846,511 | (26.2) | 5,660,882 | (19.6) | −0.22 | <0.0001 | 491,132 | (29.5) | 514,194 | (28.3) | −0.01 | 0.6018 | 95.9 |
| No | 2,381,306 | (73.8) | 23,280,000 | (80.4) | 1,176,599 | (70.6) | 1,303,447 | (71.7) | |||||||
| Alcohol | Yes | 1,621,795 | (50.2) | 16,510,000 | (57.0) | 0.11 | <0.0001 | 949,294 | (56.9) | 859,903 | (47.3) | −0.04 | 0.0669 | 67.1 | |
| No | 1,609,111 | (49.8) | 12,440,000 | (43.0) | 718,437 | (43.1) | 957,739 | (52.7) | |||||||
| Exercise | Yes | 1,222,139 | (37.8) | 12,740,000 | (44.0) | 0.04 | <0.0001 | 755,371 | (45.3) | 804,876 | (44.3) | −0.02 | 0.6516 | 64.6 | |
| No | 2,010,005 | (62.2) | 16,240,000 | (56.0) | 912,360 | (54.7) | 1,012,766 | (55.7) | |||||||
| Skipping breakfast | No | 2,435,469 | (83.9) | 21,910,000 | (87.6) | −0.14 | <0.0001 | 1,341,499 | (80.4) | 1,459,448 | (80.3) | −0.01 | 0.9384 | 92.6 | |
| Yes | 465,968 | (16.1) | 3,095,662 | (12.4) | 326,232 | (19.6) | 358,193 | (19.7) | |||||||
| Eating out | Yes | 1,893,088 | (65.3) | 18,950,000 | (75.8) | −0.15 | <0.0001 | 1,308,435 | (78.5) | 1,395,513 | (76.8) | 0.01 | 0.3419 | 95.5 | |
| No | 1,008,349 | (34.8) | 6,053,438 | (24.2) | 359,297 | (21.5) | 422,129 | (23.2) | |||||||
| Using nutrition labels | Yes | 554,708 | (32.3) | 6,738,336 | (34.9) | −0.11 | 0.1277 | 544,393 | (32.6) | 553,067 | (30.4) | 0.01 | 0.3241 | 91.4 | |
| No | 1,164,419 | (67.7) | 12,560,000 | (65.1) | 1,123,338 | (67.4) | 1,264,574 | (69.6) | |||||||
| Mental health | Stress | Yes | 846,513 | (26.2) | 7,763,267 | (26.8) | 0.03 | 0.5629 | 441,562 | (26.5) | 477,272 | (26.3) | 0.00 | 0.9037 | 94.2 |
| No | 2,380,480 | (73.8) | 21,170,000 | (73.2) | 1,226,169 | (73.5) | 1,340,369 | (73.7) | |||||||
| Diseases | Matching | Mean | Difference (A-B) | 95% CI a of Difference | t- Statistics | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Single-Person Household (A) | Multi-Person Household (B) | Lower Limit | Upper Limit | |||||
| MS | Before | 0.353 | 0.268 | 0.086 | 0.0635 | 0.1081 | 7.56 | <0.0001 |
| After | 0.290 | 0.316 | −0.026 | −0.0648 | 0.0123 | −1.34 | 0.1822 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.; Park, I. Effect of Household Type on the Prevalence of Metabolic Syndrome in Korea: Using Propensity Score Matching. Healthcare 2022, 10, 1894. https://doi.org/10.3390/healthcare10101894
Park J, Park I. Effect of Household Type on the Prevalence of Metabolic Syndrome in Korea: Using Propensity Score Matching. Healthcare. 2022; 10(10):1894. https://doi.org/10.3390/healthcare10101894
Chicago/Turabian StylePark, Jisu, and Ilsu Park. 2022. "Effect of Household Type on the Prevalence of Metabolic Syndrome in Korea: Using Propensity Score Matching" Healthcare 10, no. 10: 1894. https://doi.org/10.3390/healthcare10101894
APA StylePark, J., & Park, I. (2022). Effect of Household Type on the Prevalence of Metabolic Syndrome in Korea: Using Propensity Score Matching. Healthcare, 10(10), 1894. https://doi.org/10.3390/healthcare10101894





