Abstract
The objective of this study was to compare the mental well-being of French women who were and were not pregnant during the first COVID-19 pandemic lockdown. We performed a nationwide online quantitative survey including all women between 18 and 45 years of age during the second and third weeks of global lockdown (25 March–7 April 2020). The main outcome measure was mental well-being measured by the Warwick–Edinburgh Mental Well-Being Scale (WEMWBS). This study analysed 275 responses from pregnant women and compared them with those from a propensity score–matched sample of 825 non-pregnant women. In this French sample, the median WEMWBS score was 49.0 and did not differ by pregnancy status. Women living in urban areas reported better well-being, while those with sleep disorders or who spent more than an hour a day watching the news reported poorer well-being. During the first lockdown in France, women had relatively low mental well-being scores, with no significant difference between pregnant and non-pregnant women. More than ever, health-care workers need to find a way to maintain their support for women’s well-being. Minor daily annoyances of pregnancy, such as insomnia, should not be trivialised because they are a potential sign of poor well-being.
1. Introduction
In some Western countries, suicides are one of the main causes of maternal deaths [,]. Long before the COVID-19 pandemic, a systematic review found that between 7 and 13% of women are depressed during pregnancy and 19% have postpartum depression; 7% of these cases were considered major []. We also know that the mental disorders of mothers are strongly associated with their children’s physical and mental well-being [].
At the beginning of the COVID-19 pandemic period, the medical situation was considered much more anxiety inducing for pregnant than for non-pregnant women. In March 2020, no data were available about the potential for a higher risk of severe effects due to this coronavirus during pregnancy, for both mother and child, by possible vertical transmission []. Applying the precautionary principle, pregnant women were considered to be at high risk of medical complications []. The separation of an infected mother from the child at birth was debated [] and many French hospitals prevented women (infected or uninfected) from receiving support from their partners during childbirth []. The lockdown measures, imposed to limit the epidemic’s spread and applied to maternity wards in elsewhere in Europe and in Western countries, have raised concerns among professionals about their psychological impact on pregnant women and mothers []. The reorganisation of hospitals and the community care sector may have generated concern about access to care during pregnancy and childbirth [].
These factors indicate that the current pandemic period, with its repeated lockdowns, is likely to negatively affect the mental well-being of pregnant women [,]. Most of the recently reviewed studies have reported that isolation has negative psychological effects on the population, including anxiety, depression, and post-traumatic and other stress symptoms [,]. While some controlled comparative studies on the lockdown’s impact on depression during the postpartum period are available, to our knowledge, no such data exist for broader outcomes such as mental well-being among pregnant women in Western countries [,,].
We therefore sought to compare the mental well-being level of French pregnant and non-pregnant women during the first COVID-19 lockdown. As a secondary objective, we examined the association between pregnant women’s characteristics and their level of well-being.
2. Materials and Methods
We conducted a nationwide online survey to measure the mental well-being of French women during the second and third weeks of global lockdown during the pandemic. The results of this quantitative study are reported according to the Checklist for Reporting Results of Internet E-Surveys (cf. Table S1: CHERRIES) [].
2.1. Screening and Recruitment
The LockUwell survey was an open French e-survey. Recruitment took place by sending the survey link through various online announcements on social networks (Facebook, Twitter and LinkedIn, the authors’ individual and institutional accounts) and national newspaper websites. It directed those interested in participating to this survey, created with open-source software (LimeSurvey). Individual consent was obtained from all women. In accordance with current French legislation on health research, no ethics committee approval was required because data collection was anonymous. We obtained a convenience sample through voluntary participation, without any incentives or rewards. The survey was open throughout the first nationwide lockdown period. The analysis presented here studies data collected from 25 March to 7 April (week 2 and week 3 of this first national lockdown in France). We used cookies to ensure we collected only one set of answers per participant.
The LockUwell survey targeted all French-speakers. This analysis includes pregnant and non-pregnant women aged between 18 and 45 years. We thus excluded all men, women older or younger than the selected age group, as well as women locked down outside France and those who did not know their pregnancy status. The completion rate was defined by the ratio of users who finished the survey divided by the number who agreed to participate.
2.2. Measures and Definitions
The questionnaire of the LockUwell survey was constructed through an iterative testing process that included revisions by epidemiologists, psychiatrists in several subspecialties, mental-health service users, and citizens, as described elsewhere []. The survey included sociodemographic data (Section 1), an evaluation of well-being (validated French version of the Warwick–Edinburgh Mental Well-Being Scale, WEMWBS) (Section 2), stress evaluations (Section 3), medical, psychiatric, lockdown and isolation, and social contact history (Section 4), personal situation (infection or exposure of self or family, friends, and co-workers) regarding COVID-19 (Section 5), as well as personal and environmental conditions during lockdown including watching news, physical exercise and sports activities, and sleep disorders (Section 6) [,]. The items were not randomised. Respondents were able to review and change their answers through a back button. The estimated duration of the questionnaire was 15 to 30 min.
2.3. Statistical Analysis
All statistical analyses were performed with R software, version 4.0.3 []. Inescapably, if only for their age, non-pregnant women who responded to our survey did not have the same characteristics as the pregnant women who responded to it. Therefore, we used a propensity score approach to control for confounding factors that might influence our result on their mental well-being levels. We included all pregnant women but selected non-pregnant women by stratification by a propensity score []. We analysed only questionnaires with sufficient information to calculate this score. A woman’s propensity score was defined as her probability of being pregnant based on the individual covariates we measured. This score was calculated by applying a generalised linear model with current pregnancy as the dependent variable and considering the following characteristics: age range, marital status, living alone or with someone else, psychiatric (including addictions) history, parity, local extent of pandemic area during weeks 2–3 of lockdown, educational level, and occupation. We distributed the propensity scores obtained for each woman into five classes. Finally, we matched non-pregnant women (controls) on a three-for-one basis, class by class. The early/late pandemic area was determined retrospectively as early or late by the respondents’ postcodes. Districts with a ratio of more than 2 deaths per 100,000 residents on 23 March 2020, were classified as early pandemic areas by the French national public health agency, Santé Publique France (https://www.data.gouv.fr/ accessed on 5 September 2021).
Quantitative variables with normal distributions according to the Shapiro–Wilk test were described by their means and standard deviations (SD), and then compared with a Welch two-sample t-test. When distributions were not normal, variables were described according to their medians, with their 25th and 75th percentiles (Q1–Q3), and then compared by a Wilcoxon rank sum test. Qualitative variables were described as the number of individuals and percentages and then compared with Fisher’s exact test. The denominator is reported when it comprises less than 95% of the total sample size. A multiple regression analysis then assessed the association of pregnant women’s characteristics with their WEMWBS score. This score was entered as a dependent variable in the model and all their other characteristics as independent variables.
3. Results
Of the 23,709 questionnaires started, only 16,963 provided sufficient responses for analysis, for a completion rate of 71.55%. Of these 16,963 participants, 291 women were pregnant, a figure consistent with the around 800 000 annual births in France for a population of 67 million persons. After exclusion of women without minimal data to calculate the propensity score, 275 pregnant women and 825 non-pregnant women were included and analysed (Figure 1). These pregnant women had a mean age of 31 years (SD = 4.1), and 97% were in a relationship. Most were nulliparous (59%), with a high educational level (63%) and no history of psychiatric disorder, including addiction (83%) (Table 1). These pregnant women had a median WEMWBS score of 49 (Q1–Q3 43.0–54.0), as did the non-pregnant women (Q1–Q3 44.0–54.0) (p = 0.720).
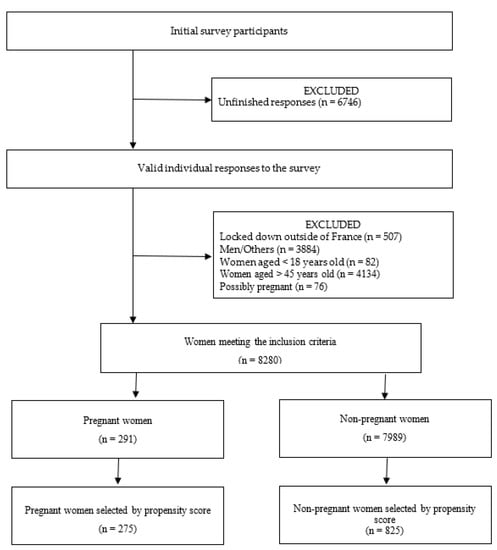
Figure 1.
Study flow.

Table 1.
Characteristics of study participants by pregnancy status.
Among pregnant women, suburban living was significantly associated with a lower level of well-being (47 vs. 50 for urban living). Sleep disorders were similarly significantly associated with poorer well-being (45.5 WEMBWS median), as was watching the news for more than an hour a day (47 WEMBWS median; Table 2). Pregnant women who were in relationships, or had a high level of education, or who worked alternately at home and at the office, tended to report higher levels of mental well-being, although these differences were not statistically significant.

Table 2.
Linear regression for total WEMWBS scores of pregnant women (n = 275).
4. Discussion
4.1. Main Findings
The COVID-19 lockdown appeared to affect the well-being of pregnant and non-pregnant women equally. Our study identified important characteristics of pregnant women that appears to be associated with poorer mental well-being. These included suburban residence, sleep disorders, and spending more than one hour a day watching the news. Midwives should explore these warning signs.
4.2. Strengths and Limitations
The originality of this study is its approach based on women’s well-being scores. Well-being is a key determinant of health-related behaviours []. The scale used in our study combines the hedonic approach (positive emotions, satisfaction with one’s life) with the eudemonic approach that includes the perception of usefulness and confidence in the future, which may be particularly questionable in the current context of media gloom-mongering. Most of the other tools published so far have assessed negative psychological reactions such as anxiety and stress, or even pathological reactions such as depression and/or post-traumatic stress disorder. The main strengths of our study are that the results are based on a voluntary general population survey with the control group selected by a propensity score as a representative sample of our source sample. Thus, this study is based on a convenience sample with overrepresentation of high educational and socioeconomic levels with stable partner situations, who are at lower risk of stress. A noteworthy limitation of our study is due to the selection bias inherent in any population-based survey []. Indeed, on the one hand, our study was only accessible to women with access to the internet and, on the other hand, our study shows that access to information (especially available on the internet) was associated with the level of well-being. Nevertheless, one the one hand, more than 98% of the French women from which our sample emerged have access to the internet []. One the other hand, our method balances the selection bias between the groups and therefore provides some confidence in our results regarding the main objective of comparing well-being according to pregnancy [].
4.3. Interpretation
Given that previous studies have reported similar levels of well-being between men and women, pregnant or not, we hypothesised that the specific official measures affecting pregnant women compared with non-pregnant women based on the precautionary principle might have compromised their well-being [,]. We were surprised that we did not observe any difference in well-being between pregnant and non-pregnant women. This may be explained in part by the fact that work is also a major source of stress, from which some pregnant women are protected []. This hypothesis was also suggested to explain the decrease in the preterm birth rate during the lockdown []. During the French lockdown, many pregnant women, especially among those working as caregivers, were declared temporarily unavailable for work to protect them. Our study showed a lower level of well-being among women in general and pregnant women in particular during than before lockdown: 49 for the WEMSBS total score for both groups during lockdown in our study vs. 53 among the French general population in 2014 (not of women, but identical in the one group primarily female, and the one primarily male) [] and 54 among British women pregnant with their first child in 2016–2017 []. These results are in line with those recently published about a population recruited in the United States, the United Kingdom and Ireland []. However, our results should be seen in the French context. Indeed, there are large cultural and policy differences between European countries that are reflected, for example, in large differences in sick leave rates []. Lastly, let us consider that, apart from the specific restrictions for pregnant women, the main restriction of confinement that applied to all women may have been particularly burdensome for non-pregnant mothers who were working at home while caring for their child(ren) (more so than for pregnant women without children). A recent Irish study also shows a lower perceived level of social support among pregnant women []. The lack of a significant association between the presence of psychiatric history or addiction and well-being could be related to a selection bias in our sample but suggests the importance of caring for the well-being of all pregnant women, regardless of their history. Contrary to results from a Chinese study, living in urban-based environments appears to be a protective factor for well-being []. Recent studies have showed a negative impact of rural living on mental health in Turkey and Italy [,]. However, fear of contracting the virus and being locked down are legitimate factors that may affect women’s well-being.
4.4. Research Recommendation
Further studies should be conducted to assess the impact of repeated lockdowns on pregnant women, and indeed on mothers, especially those who work. We expect that further research with a similar methodology and better control of selection bias will confirm our results. It will also be important to study women’s well-being by designs appropriate for recruiting residents with low literacy levels. Last but not least, this pandemic seems to have led to the population losing confidence in the future, resulting in a fall in the birth rate. The increase that followed remained well below the rates of previous years [].
4.5. Practical Recommendation
With the pandemic still active as we go from lockdown to lockdown, the first implication for clinical practice is the importance of maintaining contact with pregnant women, especially those in suburban areas. New ways must be found to maintain this supportive contact. The postponement or cancellation of consultations deemed non-essential by midwives has limited the support available to women during lockdown [,]. Remote video consultation is an innovative approach that has already shown its effectiveness in reducing antenatal distress and pregnancy-related anxiety; it also raises questions in terms of accessibility and literacy []. A second implication for clinical practice is that midwives should be especially observant of women’s sleep disorders. A Finnish study showed that although the lockdown was not associated with total sleep time, daily rhythms changed, and pregnant women overall fell asleep later and woke up later []. Another study found a correlation between COVID-related stress and sleep disturbances []. Although sleep disorders are common during pregnancy, they must never be considered insignificant. They constantly affect women’s well-being and quality of life [,]. Sleep psychoeducation is another approach to helping these women [].
Finally, we can suggest that might be useful for health-care workers, especially for midwives, to communicate clearly and visibly with women about the impact of the pandemic on pregnancy to counterbalance the negative effect of the media.
5. Conclusions
In this survey, the level of mental well-being of pregnant women was similar to that of non-pregnant women during the first lockdown. More than ever, clinicians need to find a way to maintain support for women’s well-being and to screen for potential symptoms of mental distress.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10101855/s1, Table S1: Checklist for Reporting Results of Internet E-Surveys (CHERRIES).
Author Contributions
Conceptualization, L.G., C.B., C.D. and J.H.; methodology, J.H.; validation, J.H.; formal analysis, L.G.; investigation, F.H.; resources, N.F.; data curation, L.G.; writing—original draft preparation, L.G.; writing—review and editing, C.R., S.P., E.L., M.C. and S.V.-S.; supervision, J.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Individual consent was obtained from all women. In accordance with current French legislation on health research, no ethics committee approval was required because data collection was anonymous. The study adheres to the Ethical Principles for Medical Research Involving Human Subjects of the Declaration of Helsinki (64th World Medical Association General Assembly, Fortaleza, Brazil, October 2013).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We thank Jo Ann Cahn for her careful proofreading and editing services.
Conflicts of Interest
All authors have completed the ICMJE uniform disclosure form. F.H. has received personal fees and/or non-financial support outside of the submitted work from Janssen, Lundbeck and Otsuka. J.H. has received personal fees and/or non-financial support outside of the submitted work from Janssen. The others authors certify that they have NO affiliation with or involvement in any organisation or entity with any financial or non-financial interest in the subject matter of this article.
References
- Deneux-Tharaux, C.; Saucedo, M. Les Morts Maternelles en France: Mieux Comprendre Pour Mieux Prévenir. 6e Rapport de l’Enquête Nationale Confidentielle sur Les Morts Maternelles (ENCMM) 2013–2015; Santé Publique France: Paris, France, 2021; p. 237. [Google Scholar]
- Oates, M. Perinatal Psychiatric Disorders: A Leading Cause of Maternal Morbidity and Mortality. Br. Med. Bull. 2003, 67, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Gavin, N.I.; Gaynes, B.N.; Lohr, K.N.; Meltzer-Brody, S.; Gartlehner, G.; Swinson, T. Perinatal Depression: A Systematic Review of Prevalence and Incidence. Obstet. Gynecol. 2005, 106, 1071–1083. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.; Pearson, R.M.; Goodman, S.H.; Rapa, E.; Rahman, A.; McCallum, M.; Howard, L.M.; Pariante, C.M. Effects of Perinatal Mental Disorders on the Fetus and Child. Lancet 2014, 384, 1800–1819. [Google Scholar] [CrossRef]
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q.; et al. Clinical Characteristics and Intrauterine Vertical Transmission Potential of COVID-19 Infection in Nine Pregnant Women: A Retrospective Review of Medical Records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef]
- Favre, G.; Pomar, L.; Qi, X.; Nielsen-Saines, K.; Musso, D.; Baud, D. Guidelines for Pregnant Women with Suspected SARS-CoV-2 Infection. Lancet Infect. Dis. 2020, 20, 652–653. [Google Scholar] [CrossRef]
- Coronavirus (COVID-19) Infection in Pregnancy. Information for Healthcare Professionals; The Royal College of Midweves, Royal College of Obstetrcians & Gynaecologists. 2020. Available online: https://www.rcog.org.uk/media/xsubnsma/2022-03-07-coronavirus-covid-19-infection-in-pregnancy-v15.pdf (accessed on 7 March 2022).
- Peyronnet, V.; Sibiude, J.; Deruelle, P.; Huissoud, C.; Lescure, X.; Lucet, J.-C.; Mandelbrot, L.; Nisand, I.; Vayssière, C.; Yazpandanah, Y.; et al. Infection par le SARS-CoV-2 chez les femmes enceintes: État des connaissances et proposition de prise en charge par CNGOF. Gynécologie Obs. Fertil Sénologie 2020, 48, 436–443. [Google Scholar] [CrossRef]
- Viaux, S.; Maurice, P.; Cohen, D.; Jouannic, J. Giving Birth under Lockdown during the COVID-19 Epidemic. J. Gynecol. Obstet. Hum. Reprod. 2020, 49, 101785. [Google Scholar] [CrossRef]
- Baumann, S.; Gaucher, L.; Bourgueil, Y.; Saint-Lary, O.; Gautier, S.; Rousseau, A. Adaptation of Independent Midwives to the COVID-19 Pandemic: A National Descriptive Survey. Midwifery 2021, 94, 102918. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized Anxiety Disorder, Depressive Symptoms and Sleep Quality during COVID-19 Epidemic in China: A Web-Based Cross-Sectional Survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Pope, J.; Olander, E.K.; Leitao, S.; Meaney, S.; Matvienko-Sikar, K. Prenatal Stress, Health, and Health Behaviours during the COVID-19 Pandemic: An International Survey. Women Birth J. Aust. Coll. Midwives 2021, 35, 272–279. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Odriozola-González, P.; Planchuelo-Gómez, Á.; Irurtia, M.J.; de Luis-García, R. Psychological Effects of the COVID-19 Outbreak and Lockdown among Students and Workers of a Spanish University. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef] [PubMed]
- Zanardo, V.; Manghina, V.; Giliberti, L.; Vettore, M.; Severino, L.; Straface, G. Psychological Impact of COVID-19 Quarantine Measures in Northeastern Italy on Mothers in the Immediate Postpartum Period. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2020, 150, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Molgora, S.; Accordini, M. Motherhood in the Time of Coronavirus: The Impact of the Pandemic Emergency on Expectant and Postpartum Women’s Psychological Well-Being. Front. Psychol. 2020, 11, 567155. [Google Scholar] [CrossRef] [PubMed]
- Oskovi-Kaplan, Z.A.; Buyuk, G.N.; Ozgu-Erdinc, A.S.; Keskin, H.L.; Ozbas, A.; Moraloglu Tekin, O. The Effect of COVID-19 Pandemic and Social Restrictions on Depression Rates and Maternal Attachment in Immediate Postpartum Women: A Preliminary Study. Psychiatr. Q. 2020, 92, 675–682. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Haesebaert, F.; Haesebaert, J.; Zante, E.; Franck, N. Who Maintains Good Mental Health in a Locked-down Country? A French Nationwide Online Survey of 11,391 Participants. Health Place 2020, 66, 102440. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Development and UK Validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Trousselard, M.; Steiler, D.; Dutheil, F.; Claverie, D.; Canini, F.; Fenouillet, F.; Naughton, G.; Stewart-Brown, S.; Franck, N. Validation of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) in French Psychiatric and General Populations. Psychiatry Res. 2016, 245, 282–290. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Stranges, S.; Samaraweera, P.C.; Taggart, F.; Kandala, N.-B.; Stewart-Brown, S. Major Health-Related Behaviours and Mental Well-Being in the General Population: The Health Survey for England. BMJ Open 2014, 4, e005878. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. Questionnaire Surveys: Sources of Bias. BMJ 2013, 347, f5265. [Google Scholar] [CrossRef]
- Croutte, P. Baromètre du Numérique 2019; Zenodo: Geneve, Switzerland, 2020. [Google Scholar]
- Adelson, J. Educational Research with Real-World Data: Reducing Selection Bias with Propensity Score Analysis. Pract. Assess. Res. Eval. 2019, 18, 15. [Google Scholar] [CrossRef]
- Ginja, S.; Coad, J.; Bailey, E.; Kendall, S.; Goodenough, T.; Nightingale, S.; Smiddy, J.; Day, C.; Deave, T.; Lingam, R. Associations between Social Support, Mental Wellbeing, Self-Efficacy and Technology Use in First-Time Antenatal Women: Data from the BaBBLeS Cohort Study. BMC Pregnancy Childbirth 2018, 18, 441. [Google Scholar] [CrossRef] [PubMed]
- Barone Gibbs, B.; Kline, C.E.; Huber, K.A.; Paley, J.L.; Perera, S. COVID-19 Shelter-at-Home and Work, Lifestyle and Well-Being in Desk Workers. Occup. Med. 2021, 71, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.A.; von Dadelszen, P.; Khalil, A. COVID-19 and Preterm Birth. Lancet Glob. Health 2021, 9, e117. [Google Scholar] [CrossRef]
- Truong, B.T.; Lupattelli, A.; Kristensen, P.; Nordeng, H. Sick Leave and Medication Use in Pregnancy: A European Web-Based Study. BMJ Open 2017, 7, e014934. [Google Scholar] [CrossRef]
- Matvienko-Sikar, K.; Pope, J.; Cremin, A.; Carr, H.; Leitao, S.; Olander, E.K.; Meaney, S. Differences in Levels of Stress, Social Support, Health Behaviours, and Stress-Reduction Strategies for Women Pregnant before and during the COVID-19 Pandemic, and Based on Phases of Pandemic Restrictions, in Ireland. Women Birth 2021, 34, 447–454. [Google Scholar] [CrossRef]
- Liu, L.; Xue, P.; Li, S.X.; Zhang, J.; Zhou, J.; Zhang, W. Urban-Rural Disparities in Mental Health Problems Related to COVID-19 in China. Gen. Hosp. Psychiatry 2020, 69, 119–120. [Google Scholar] [CrossRef]
- Durankuş, F.; Aksu, E. Effects of the COVID-19 Pandemic on Anxiety and Depressive Symptoms in Pregnant Women: A Preliminary Study. J. Matern.-Fetal Neonatal Med. 2020, 35, 205–211. [Google Scholar] [CrossRef]
- Pedrosa, A.L.; Bitencourt, L.; Fróes, A.C.F.; Cazumbá, M.L.B.; Campos, R.G.B.; de Brito, S.B.C.S.; Simões, E.; Silva, A.C. Emotional, Behavioral, and Psychological Impact of the COVID-19 Pandemic. Front. Psychol. 2020, 11, 566212. [Google Scholar] [CrossRef] [PubMed]
- Avril 2021: La Hausse de Mars Se Poursuit; Nombre de Naissances en 2021; Insee: Paris, France, 2021.
- Hagaman, A.; LeMasters, K.; Zivich, P.N.; Sikander, S.; Bates, L.M.; Bhalotra, S.; Chung, E.O.; Zaidi, A.; Maselko, J. Longitudinal Effects of Perinatal Social Support on Maternal Depression: A Marginal Structural Modelling Approach. J. Epidemiol. Community Health 2021, 75, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Aksoy Derya, Y.; Altiparmak, S.; AkÇa, E.; GÖkbulut, N.; Yilmaz, A.N. Pregnancy and Birth Planning during COVID-19: The Effects of Tele-Education Offered to Pregnant Women on Prenatal Distress and Pregnancy-Related Anxiety. Midwifery 2021, 92, 102877. [Google Scholar] [CrossRef] [PubMed]
- Niela-Vilén, H.; Auxier, J.; Ekholm, E.; Sarhaddi, F.; Asgari Mehrabadi, M.; Mahmoudzadeh, A.; Azimi, I.; Liljeberg, P.; Rahmani, A.M.; Axelin, A. Pregnant Women’s Daily Patterns of Well-Being before and during the COVID-19 Pandemic in Finland: Longitudinal Monitoring through Smartwatch Technology. PLoS ONE 2021, 16, e0246494. [Google Scholar] [CrossRef]
- Coiro, M.J.; Asraf, K.; Tzischinsky, O.; Hadar-Shoval, D.; Tannous-Haddad, L.; Wolfson, A.R. Sleep Quality and COVID-19-Related Stress in Relation to Mental Health Symptoms among Israeli and U.S. Adults. Sleep Health 2021, 7, 127–133. [Google Scholar] [CrossRef]
- Garbazza, C.; Hackethal, S.; Riccardi, S.; Cajochen, C.; Cicolin, A.; D’Agostino, A.; Cirignotta, F.; Manconi, M. Polysomnographic Features of Pregnancy: A Systematic Review. Sleep Med. Rev. 2020, 50, 101249. [Google Scholar] [CrossRef]
- Lagadec, N.; Steinecker, M.; Kapassi, A.; Magnier, A.M.; Chastang, J.; Robert, S.; Gaouaou, N.; Ibanez, G. Factors Influencing the Quality of Life of Pregnant Women: A Systematic Review. BMC Pregnancy Childbirth 2018, 18, 455. [Google Scholar] [CrossRef]
- Kempler, L.; Sharpe, L.A.; Marshall, N.S.; Bartlett, D.J. A Brief Sleep Focused Psychoeducation Program for Sleep-Related Outcomes in New Mothers: A Randomized Controlled Trial. Sleep 2020, 43, 11. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).