Pathophysiology and Management of Placenta Accreta Spectrum
Abstract
1. Introduction
- Grade 1: Abnormally adherent placenta (placenta adherenta or creta): attached directly to the myometrium without invasion.
- Grade 2: Abnormal invasion of placenta into the myometrium (placenta increta).
- Grade 3: Abnormal invasion of placenta through the full thickness of the uterine wall to the serosa, or beyond to surrounding pelvic tissues, vessels, and organs (placenta percreta) [3].
1.1. Incidence
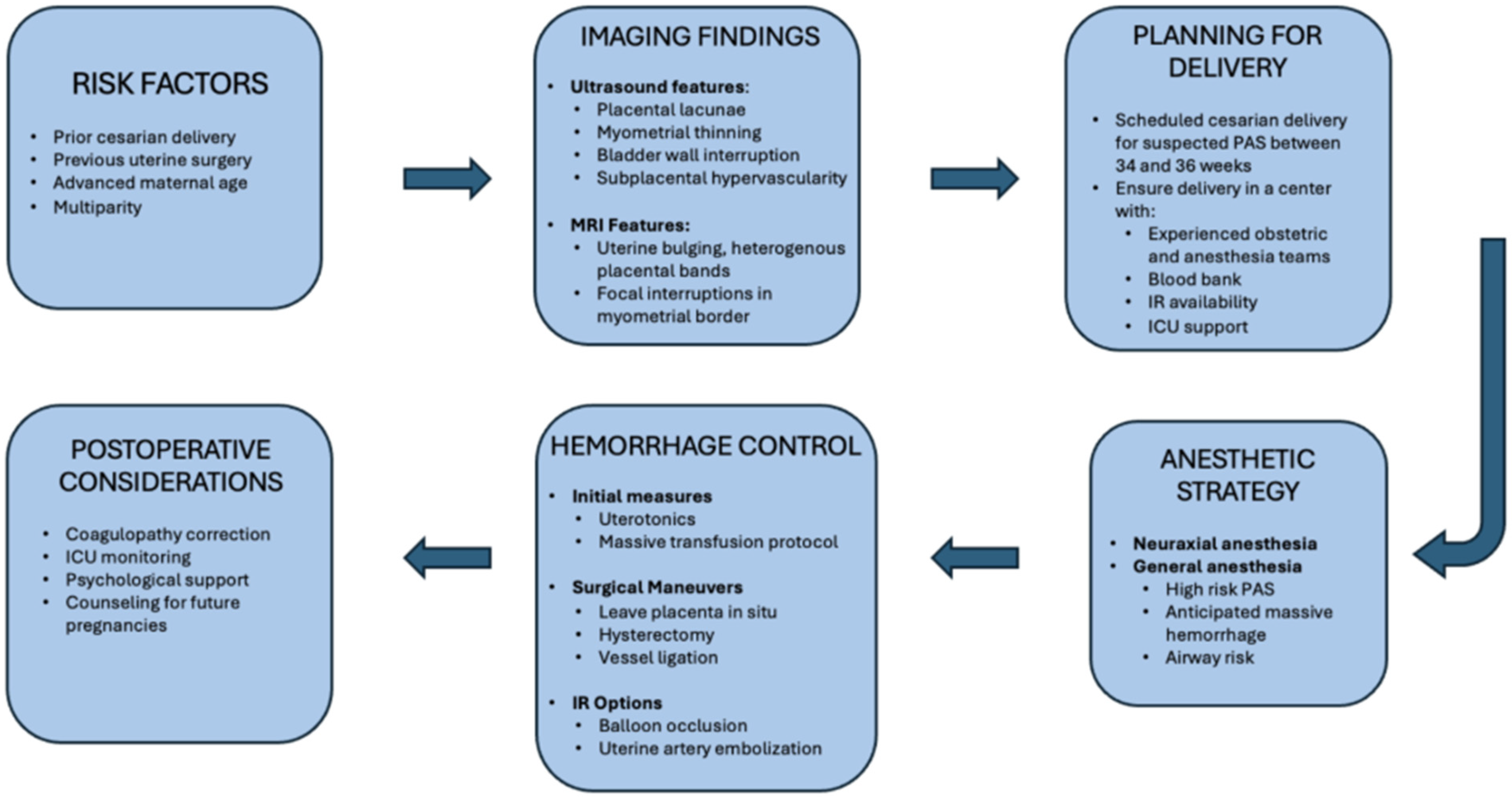
1.2. Risk Factors
1.3. Clinical Significance
1.4. Pathophysiology
1.4.1. Normal Placentation
1.4.2. Developmental Origins of Abnormal Placentation
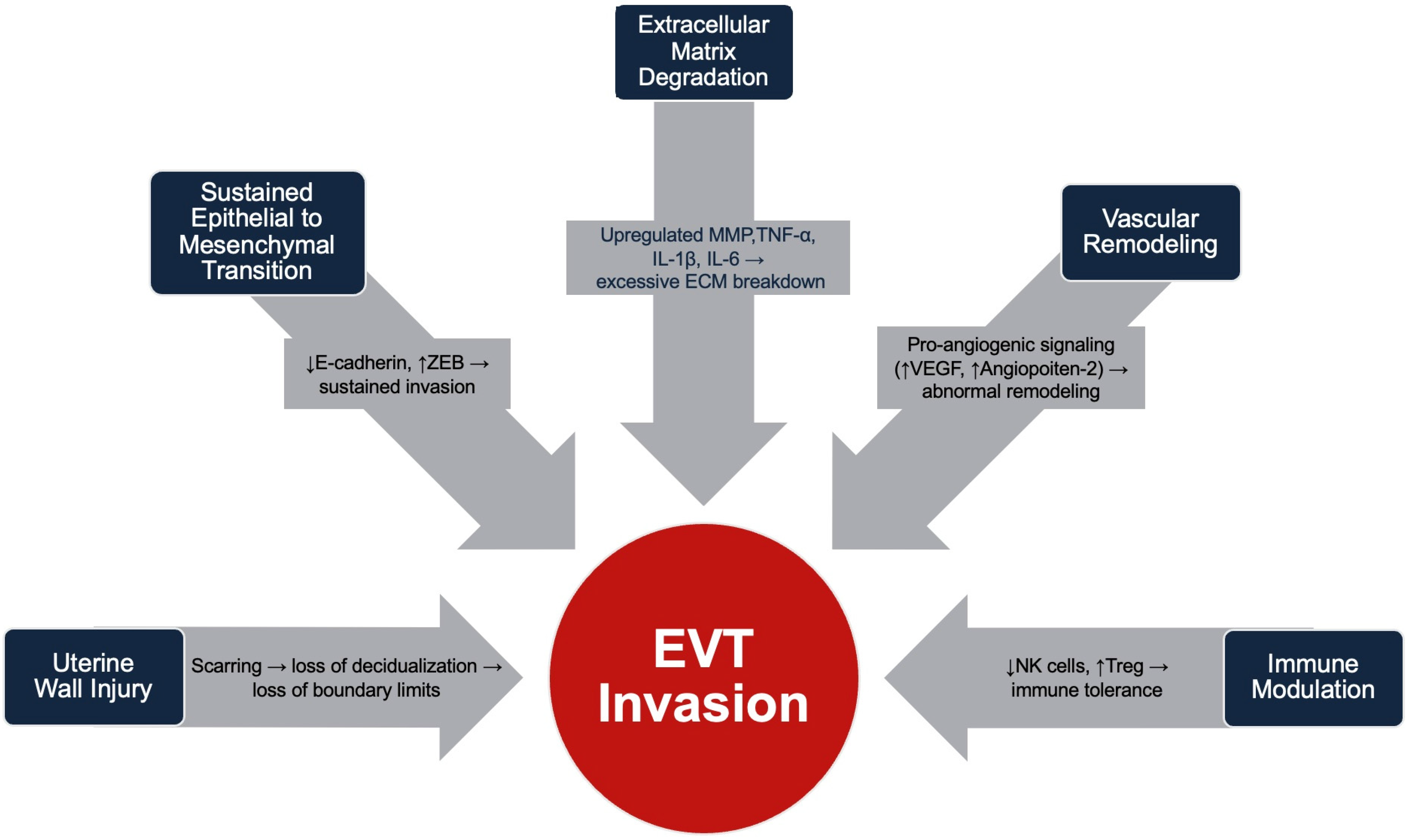
1.4.3. Molecular and Cellular Mechanisms Involved in Trophoblast Invasion and Uterine Wall Remodeling
1.4.4. Implications on Fetal Development
1.5. Diagnosis
The Role of MRI
2. Management and Considerations
2.1. Preoperative
2.1.1. History and Physical Exam
2.1.2. Anesthesia Planning and Maternal Considerations
2.2. Intra-Operative
2.2.1. General Anesthesia
2.2.2. Considerations for Hemorrhage
2.2.3. Conservative and Expectant Management
2.2.4. Interventional Radiology
2.3. Postoperative
3. Unexpected Accreta Discovered Intra-Operatively
4. Future Fertility
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Silver, R.M.; Branch, D.W. Placenta Accreta Spectrum. N. Engl. J. Med. 2018, 378, 1529–1536. [Google Scholar] [CrossRef] [PubMed]
- Marcellin, L.; Delorme, P.; Bonnet, M.P.; Grange, G.; Kayem, G.; Tsatsaris, V.; Goffinet, F. Placenta percreta is associated with more frequent severe maternal morbidity than placenta accreta. Am. J. Obstet. Gynecol. 2018, 219, 193.e1–193.e9. [Google Scholar] [CrossRef] [PubMed]
- Jauniaux, E.; Zheng, W.; Yan, J. Confirming the Diagnosis and Classifying Placenta Accreta Spectrum (PAS) Disorders: Minutes of 2020 Online International Workshop on PAS in Beijing. Matern.-Fetal Med. 2021, 3, 229–231. [Google Scholar] [CrossRef]
- Rac, M.W.; Dashe, J.S.; Wells, C.E.; Moschos, E.; McIntire, D.D.; Twickler, D.M. Ultrasound predictors of placental invasion: The Placenta Accreta Index. Am. J. Obstet. Gynecol. 2015, 212, 343.e1–343.e7. [Google Scholar] [CrossRef]
- Hecht, J.L.; Baergen, R.; Ernst, L.M.; Katzman, P.J.; Jacques, S.M.; Jauniaux, E.; Khong, T.Y.; Metlay, L.A.; Poder, L.; Qureshi, F.; et al. Classification and reporting guidelines for the pathology diagnosis of placenta accreta spectrum (PAS) disorders: Recommendations from an expert panel. Mod. Pathol. 2020, 33, 2382–2396. [Google Scholar] [CrossRef]
- Bailit, J.L.; Grobman, W.A.; Rice, M.M.; Reddy, U.M.; Wapner, R.J.; Varner, M.W.; Leveno, K.J.; Iams, J.D.; Tita, A.T.N.; Saade, G.; et al. Morbidly adherent placenta treatments and outcomes. Obstet. Gynecol. 2015, 125, 683–689. [Google Scholar] [CrossRef]
- Read, J.A.; Cotton, D.B.; Miller, F.C. Placenta accreta: Changing clinical aspects and outcome. Obstet. Gynecol. 1980, 56, 31–34. [Google Scholar]
- Matsuzaki, S.; Mandelbaum, R.S.; Sangara, R.N.; McCarthy, L.E.; Vestal, N.L.; Klar, M.; Matsushima, K.; Amaya, R.; Ouzounian, J.G.; Matsuo, K. Trends, characteristics, and outcomes of placenta accreta spectrum: A national study in the United States. Am. J. Obstet. Gynecol. 2021, 225, 534.e1–534.e38. [Google Scholar] [CrossRef]
- Rau, A.R.; Youssefzadeh, A.C.; Matsuzaki, S.; Mandelbaum, R.S.; Ouzounian, J.G.; Matsuo, K. Unsuspected placenta accreta spectrum at vaginal delivery: Assessment of incidence, characteristics, and maternal morbidity. Am. J. Obstet. Gynecol. MFM 2023, 5, 100805. [Google Scholar] [CrossRef]
- Jauniaux, E.; Bunce, C.; Grønbeck, L.; Langhoff-Roos, J. Prevalence and main outcomes of placenta accreta spectrum: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2019, 221, 208–218. [Google Scholar] [CrossRef] [PubMed]
- Silver, R.M.; Landon, M.B.; Rouse, D.J.; Leveno, K.J.; Spong, C.Y.; Thom, E.A.; Moawad, A.H.; Caritis, S.N.; Harper, M.; Wapner, R.J.; et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet. Gynecol. 2006, 107, 1226–1232. [Google Scholar] [CrossRef]
- Bowman, Z.S.; Eller, A.G.; Bardsley, T.R.; Greene, T.; Varner, M.W.; Silver, R.M. Risk factors for placenta accreta: A large prospective cohort. Am. J. Perinatol. 2014, 31, 799–804. [Google Scholar]
- Kayem, G.; Seco, A.; Vendittelli, F.; Crenn Hebert, C.; Dupont, C.; Branger, B.; Huissoud, C.; Fresson, J.; Winer, N.; Langer, B.; et al. Risk factors for placenta accreta spectrum disorders in women with any prior cesarean and a placenta previa or low lying: A prospective population-based study. Sci. Rep. 2024, 14, 6564. [Google Scholar] [CrossRef]
- Umezurike, C.C.; Feyi-Waboso, P.A. Placenta accreta and the developing world—A review. East. Afr. Med. J. 2010, 87, 513–520. [Google Scholar] [PubMed]
- Carusi, D.A.; Gopal, D.; Cabral, H.J.; Racowsky, C.; Stern, J.E. A risk factor profile for placenta accreta spectrum in pregnancies conceived with assisted reproductive technology. F S Rep. 2023, 4, 279–285. [Google Scholar] [CrossRef] [PubMed]
- You, H.; Wang, Y.; Han, R.; Gu, J.; Zeng, L.; Zhao, Y. Risk factors for placenta accreta spectrum without prior cesarean section: A case-control study in China. Int. J. Gynaecol. Obstet. 2024, 166, 1092–1099. [Google Scholar] [CrossRef]
- Keag, O.E.; Norman, J.E.; Stock, S.J. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018, 15, e1002494. [Google Scholar] [CrossRef]
- Iacovelli, A.; Liberati, M.; Khalil, A.; Timor-Trisch, I.; Leombroni, M.; Buca, D.; Milani, M.; Flacco, M.E.; Manzoli, L.; Fanfani, F.; et al. Risk factors for abnormally invasive placenta: A systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2020, 33, 471–481. [Google Scholar] [CrossRef]
- Shamshirsaz, A.A.; Fox, K.A.; Erfani, H.; Clark, S.L.; Hui, S.K.; Shamshirsaz, A.A.; Rezaei, A.; Nassr, A.A.; Lake, Y.N.; Teruya, J.; et al. Coagulopathy in surgical management of placenta accreta spectrum. Eur. J. Obs. Gynecol. Reprod. Biol. 2019, 237, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Clausen, C.; Lönn, L.; Langhoff-Roos, J. Management of placenta percreta: A review of published cases. Acta Obstet. Gynecol. Scand. 2014, 93, 138–143. [Google Scholar] [CrossRef]
- Washecka, R.; Behling, A. Urologic complications of placenta percreta invading the urinary bladder: A case report and review of the literature. Hawaii Med. J. 2002, 61, 66–69. [Google Scholar]
- Vinograd, A.; Wainstock, T.; Mazor, M.; Beer-Weisel, R.; Klaitman, V.; Dukler, D.; Hamou, B.; Novack, L.; Ben-Shalom Tirosh, N.; Vinograd, O.; et al. Placenta accreta is an independent risk factor for late pre-term birth and perinatal mortality. J. Matern. Fetal Neonatal Med. 2015, 28, 1381–1387. [Google Scholar] [CrossRef]
- Jauniaux, E.; Jurkovic, D. Placenta accreta: Pathogenesis of a 20th century iatrogenic uterine disease. Placenta 2012, 33, 244–251. [Google Scholar] [CrossRef]
- Gómez, E.; Ruíz-Alonso, M.; Miravet, J.; Simón, C. Human Endometrial Transcriptomics: Implications for Embryonic Implantation. Cold Spring Harb. Perspect. Med. 2015, 5, a022996. [Google Scholar] [CrossRef]
- Coulam, C. What about superfertility, decidualization, and natural selection? J. Assist. Reprod. Genet. 2016, 33, 577–580. [Google Scholar] [CrossRef]
- Ji, L.; Brkić, J.; Liu, M.; Fu, G.; Peng, C.; Wang, Y.L. Placental trophoblast cell differentiation: Physiological regulation and pathological relevance to preeclampsia. Mol. Aspects Med. 2013, 34, 981–1023. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, P.; Black, S.; Huppertz, B. Endovascular trophoblast invasion: Implications for the pathogenesis of intrauterine growth retardation and preeclampsia. Biol. Reprod. 2003, 69, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Knöfler, M. Critical growth factors and signalling pathways controlling human trophoblast invasion. Int. J. Dev. Biol. 2010, 54, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Lyall, F. Mechanisms regulating cytotrophoblast invasion in normal pregnancy and pre-eclampsia. Aust. N. Z. J. Obstet. Gynaecol. 2006, 46, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Meakin, C.; Barrett, E.S.; Aleksunes, L.M. Extravillous trophoblast migration and invasion: Impact of environmental chemicals and pharmaceuticals. Reprod. Toxicol. 2022, 107, 60–68. [Google Scholar] [CrossRef]
- Okada, H.; Tsuzuki, T.; Murata, H. Decidualization of the human endometrium. Reprod. Med. Biol. 2018, 17, 220–227. [Google Scholar] [CrossRef]
- Anacker, J.; Segerer, S.E.; Hagemann, C.; Feix, S.; Kapp, M.; Bausch, R.; Kämmerer, U. Human decidua and invasive trophoblasts are rich sources of nearly all human matrix metalloproteinases. Mol. Hum. Reprod. 2011, 17, 637–652. [Google Scholar] [CrossRef]
- Kashani-Ligumsky, L.; Scott, O.; Martinez, G.; Jeong, A.; Yin, O.; Shah, S.; Wang, A.; Zhu, Y.; Afshar, Y. Updates and Knowledge Gaps in Placenta Accreta Spectrum Biology. Clin. Obstet. Gynecol. 2025, 68, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Afshar, Y.; Yin, O.; Jeong, A.; Martinez, G.; Kim, J.; Ma, F.; Jang, C.; Tabatabaei, S.; You, S.; Tseng, H.R.; et al. Placenta accreta spectrum disorder at single-cell resolution: A loss of boundary limits in the decidua and endothelium. Am. J. Obstet. Gynecol. 2024, 230, 443.e1–443.e18. [Google Scholar] [CrossRef] [PubMed]
- Imafuku, H.; Tanimura, K.; Shi, Y.; Uchida, A.; Deguchi, M.; Terai, Y. Clinical factors associated with a placenta accreta spectrum. Placenta 2021, 112, 180–184. [Google Scholar] [CrossRef]
- Garg, P.; Semwal, S.; Bansal, R. Unexpected placenta accreta spectrum in an unscarred uterus causing catastrophic post-partum hemorrhage: A case report and review of the literature. BMC Pregnancy Childbirth 2025, 25, 14. [Google Scholar] [CrossRef] [PubMed]
- Pegu, B.; Thiagaraju, C.; Nayak, D.; Subbaiah, M. Placenta accreta spectrum-a catastrophic situation in obstetrics. Obstet. Gynecol. Sci. 2021, 64, 239–247. [Google Scholar] [CrossRef]
- Hakimi, H.M.H.; Ramli, N.; Napes, M.M.; Wahab, W.N.N.; Abdul Rohim, R.A. Placenta Accreta Spectrum in Normal Situated Placenta and Unscarred Uterus. Oman Med. J. 2024, 39, e618. [Google Scholar] [CrossRef]
- Kharisma, Y.; Rachmawati, M.; Hassan, A.H.; Nur, I.M.; Agustina, H.; Suryanti, S. Association between Chronic Inflammation of Basal Plate and Decidua Existences with Placenta Accreta Spectrum. Glob. Med. Health Commun. (GMHC) 2022, 10, 111–116. [Google Scholar] [CrossRef]
- Einerson, B.D.; Comstock, J.; Silver, R.M.; Branch, D.W.; Woodward, P.J.; Kennedy, A. Placenta Accreta Spectrum Disorder: Uterine Dehiscence, Not Placental Invasion. Obstet. Gynecol. 2020, 135, 1104–1111. [Google Scholar] [CrossRef]
- Rosen, T. Placenta Accreta and Cesarean Scar Pregnancy: Overlooked Costs of the Rising Cesarean Section Rate. Clin. Perinatol. 2008, 35, 519–529. [Google Scholar] [CrossRef]
- Afshar, Y.; Kashani Ligumsky, L.; Bartels, H.C.; Krakow, D. Biology and Pathophysiology of Placenta Accreta Spectrum Disorder. Obstet. Gynecol. 2025, 145, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Wenqiang, D.; Novin, A.; Liu, Y.; Afzal, J.; Suhail, Y.; Liu, S.; Gavin, N.R.; Jorgensen, J.R.; Morosky, C.M.; Figueroa, R.; et al. Scar matrix drives Piezo1 mediated stromal inflammation leading to placenta accreta spectrum. Nat. Commun. 2024, 15, 8379. [Google Scholar] [CrossRef]
- Bartels, H.C.; Postle, J.D.; Downey, P.; Brennan, D.J. Placenta Accreta Spectrum: A Review of Pathology, Molecular Biology, and Biomarkers. Dis. Markers 2018, 2018, 1507674. [Google Scholar] [CrossRef]
- Illsley, N.P.; DaSilva-Arnold, S.C.; Zamudio, S.; Alvarez, M.; Al-Khan, A. Trophoblast invasion: Lessons from abnormally invasive placenta (placenta accreta). Placenta 2020, 102, 61–66. [Google Scholar] [CrossRef]
- Rekowska, A.K.; Obuchowska, K.; Bartosik, M.; Kimber-Trojnar, Ż.; Słodzińska, M.; Wierzchowska-Opoka, M.; Leszczyńska-Gorzelak, B. Biomolecules Involved in Both Metastasis and Placenta Accreta Spectrum-Does the Common Pathophysiological Pathway Exist? Cancers 2023, 15, 2618. [Google Scholar] [CrossRef]
- Lizárraga-Verdugo, E.; Beltrán-Ontiveros, S.A.; Gutiérrez-Grijalva, E.P.; Montoya-Moreno, M.; Gutiérrez-Arzapalo, P.Y.; Avendaño-Félix, M.; Gutiérrez-Castro, K.P.; Cuén-Lazcano, D.E.; González-Quintero, P.; Mora-Palazuelos, C.E. The Underlying Molecular Mechanisms of the Placenta Accreta Spectrum: A Narrative Review. Int. J. Mol. Sci. 2024, 25, 9722. [Google Scholar] [CrossRef]
- Bartels, H.C.; Hameed, S.; Young, C.; Nabhan, M.; Downey, P.; Curran, K.M.; McCormack, J.; Fabre, A.; Kolch, W.; Zhernovkov, V.; et al. Spatial proteomics and transcriptomics of the maternal-fetal interface in placenta accreta spectrum. Transl. Res. 2024, 274, 67–80. [Google Scholar] [CrossRef]
- Detlefs, S.E.; Carusi, D.A.; Modest, A.M.; Einerson, B.D.; Lyell, D.; Grace, M.R.; Shrivastava, V.K.; Khandelwal, M.; Salmanian, B.; Shainker, S.A.; et al. The Association between Placenta Accreta Spectrum Severity and Incidence of Small for Gestational Age Neonates. Am. J. Perinatol. 2023, 40, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, N.; Papanna, R.; Sibai, B.M.; Garcia, A.; Lai, D.; Soto Torres, E.E.; Amro, F.H.; Blackwell, S.C.; Hernandez-Andrade, E. Evaluation of fetal growth and birth weight in pregnancies with placenta previa with and without placenta accreta spectrum. J. Perinat. Med. 2025, 53, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Bartels, H.C.; Walsh, J.M.; O’Connor, C.; McParland, P.; Carroll, S.; Higgins, S.; Mulligan, K.M.; Downey, P.; Brophy, D.; Colleran, G.; et al. Placenta accreta spectrum ultrasound stage and fetal growth. Int. J. Gynaecol. Obstet. 2023, 160, 955–961. [Google Scholar]
- Toussia-Cohen, S.; Castel, E.; Friedrich, L.; Mor, N.; Ohayon, A.; Levin, G.; Meyer, R. Neonatal outcomes in pregnancies complicated by placenta accreta- a matched cohort study. Arch. Gynecol. Obstet. 2024, 310, 269–275. [Google Scholar] [CrossRef]
- Tikkanen, M.; Paavonen, J.; Loukovaara, M.; Stefanovic, V. Antenatal diagnosis of placenta accreta leads to reduced blood loss. Acta Obstet. Gynecol. Scand. 2011, 90, 1140–1146. [Google Scholar] [CrossRef]
- Wong, H.S.; Hutton, J.; Zuccollo, J.; Tait, J.; Pringle, K.C. The maternal outcome in placenta accreta: The significance of antenatal diagnosis and non-separation of placenta at delivery. N. Z. Med. J. 2008, 121, 30–38. [Google Scholar]
- Hall, T.; Wax, J.R.; Lucas, F.L.; Cartin, A.; Jones, M.; Pinette, M.G. Prenatal sonographic diagnosis of placenta accreta—Impact on maternal and neonatal outcomes. J. Clin. Ultrasound 2014, 42, 449–455. [Google Scholar]
- Roca, L.E., 2nd; Hoffman, M.C.; Gaitan, L.F.; Burkett, G. Placenta percreta masquerading as an acute abdomen. Obs. Gynecol 2009, 113, 512–514. [Google Scholar] [CrossRef]
- Innes, G.; Rosen, P. An unusual cause of abdominal pain and shock in pregnancy: Case report and review of the literature. J. Emerg. Med. 1985, 2, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Jauniaux, E.; Bhide, A.; Kennedy, A.; Woodward, P.; Hubinont, C.; Collins, S.; FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: Prenatal diagnosis and screening. Int. J. Gynaecol. Obstet. 2018, 140, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Adu-Bredu, T.K.; Rijken, M.J.; Nieto-Calvache, A.J.; Stefanovic, V.; Aryananda, R.A.; Fox, K.A.; Collins, S.L.; International Society of Placenta Accreta Spectrum Low- and Middle-Income Countries Working Group. A simple guide to ultrasound screening for placenta accreta spectrum for improving detection and optimizing management in resource limited settings. Int. J. Gynaecol. Obstet. 2023, 160, 732–741. [Google Scholar] [PubMed]
- Abu Hashim, H.; Shalaby, E.M.; Hussien, M.H.; El Rakhawy, M. Diagnostic accuracy of the placenta accreta index for placenta accreta spectrum: A prospective study. Int. J. Gynaecol. Obstet. 2022, 156, 71–76. [Google Scholar]
- Tinari, S.; Buca, D.; Cali, G.; Timor-Tritsch, I.; Palacios-Jaraquemada, J.; Rizzo, G.; Lucidi, A.; Di Mascio, D.; Liberati, M.; D’Antonio, F. Risk factors, histopathology and diagnostic accuracy in posterior placenta accreta spectrum disorders: Systematic review and meta-analysis. Ultrasound Obs. Gynecol 2021, 57, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Baughman, W.C.; Corteville, J.E.; Shah, R.R. Placenta accreta: Spectrum of US and MR imaging findings. Radiographics 2008, 28, 1905–1916. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Xie, L.; Song, W. Comparing the diagnostic value of ultrasound and magnetic resonance imaging for placenta accreta: A systematic review and meta-analysis. Ultrasound Med. Biol. 2013, 39, 1958–1965. [Google Scholar] [CrossRef] [PubMed]
- Warshak, C.R.; Eskander, R.; Hull, A.D.; Scioscia, A.L.; Mattrey, R.F.; Benirschke, K.; Resnik, R. Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. Obs. Gynecol 2006, 108, 573–581. [Google Scholar] [CrossRef]
- D’Antonio, F.; Iacovella, C.; Bhide, A. Prenatal identification of invasive placentation using ultrasound: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2013, 42, 509–517. [Google Scholar] [CrossRef]
- Philips, J.; Gurganus, M.; DeShields, S.; Cunningham, T.; Sinkovskaya, E.; Kanaan, C.; Porche, L.; Abuhamad, A. Prevalence of Sonographic Markers of Placenta Accreta Spectrum in Low-Risk Pregnancies. Am. J. Perinatol. 2019, 36, 733–780. [Google Scholar] [CrossRef]
- Cali, G.; Forlani, F.; Foti, F.; Minneci, G.; Manzoli, L.; Flacco, M.E.; Buca, D.; Liberati, M.; Scambia, G.; D’Antonio, F. Diagnostic accuracy of first-trimester ultrasound in detecting abnormally invasive placenta in high-risk women with placenta previa. Ultrasound Obstet. Gynecol. 2018, 52, 258–264. [Google Scholar] [CrossRef]
- Skupski, D.W.; Duzyj, C.M.; Scholl, J.; Perez-Delboy, A.; Ruhstaller, K.; Plante, L.A.; Hart, L.A.; Palomares, K.T.S.; Ajemian, B.; Rosen, T.; et al. Evaluation of classic and novel ultrasound signs of placenta accreta spectrum. Ultrasound Obstet. Gynecol. 2022, 59, 465–473. [Google Scholar] [CrossRef]
- Jauniaux, E.; Collins, S.; Burton, G.J. Placenta accreta spectrum: Pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am. J. Obstet. Gynecol. 2018, 218, 75–87. [Google Scholar] [CrossRef]
- Robinson, B.K.; Grobman, W.A. Effectiveness of timing strategies for delivery of individuals with placenta previa and accreta. Obstet. Gynecol. 2010, 116, 835–842. [Google Scholar] [CrossRef]
- Shamshirsaz, A.A.; Fox, K.A.; Erfani, H.; Clark, S.L.; Shamshirsaz, A.A.; Nassr, A.A.; Sundgren, N.C.; Jones, J.A.; Anderson, M.L.; Kassir, E.; et al. Outcomes of Planned Compared With Urgent Deliveries Using a Multidisciplinary Team Approach for Morbidly Adherent Placenta. Obstet. Gynecol. 2018, 131, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Lucidi, A.; Janiaux, E.; Hussein, A.M.; Nieto-Calvache, A.; Khalil, A.; D’Amico, A.; Rizzo, G.; D’Antonio, F. Emergency delivery in pregnancies at high probability of placenta accreta spectrum on prenatal imaging: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM 2024, 6, 101432. [Google Scholar] [CrossRef] [PubMed]
- Warrick, C.M.; Markley, J.C.; Farber, M.K.; Balki, M.; Katz, D.; Hess, P.E.; Padilla, C.; Waters, J.H.; Weiniger, C.F.; Butwick, A.J. Placenta Accreta Spectrum Disorders: Knowledge Gaps in Anesthesia Care. Anesth. Analg. 2022, 135, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Ophir, E.; Singer-Jordan, J.; Odeh, M.; Hirch, Y.; Maksimovsky, O.; Shaider, O.; Yvry, S.; Solt, I.; Bornstein, J. Abnormal placental invasion--a novel approach to treatment case report and review. Obstet. Gynecol. Surv. 2009, 64, 811–822. [Google Scholar]
- Eller, A.G.; Bennett, M.A.; Sharshiner, M.; Masheter, C.; Soisson, A.P.; Dodson, M.; Silver, R.M. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet. Gynecol. 2011, 117, 331–337. [Google Scholar] [CrossRef]
- Butwick, A.J.; Carvalho, B.; El-Sayed, Y.Y. Risk factors for obstetric morbidity in patients with uterine atony undergoing caesarean delivery. Br. J. Anaesth. 2014, 113, 661–668. [Google Scholar] [CrossRef]
- Shin, J. Anesthetic Management of the Pregnant Patient: Part 2. Anesth. Prog. 2021, 68, 119–127. [Google Scholar] [CrossRef]
- Alshehri, K.A.; Ammar, A.A.; Aldhubabian, M.A.; Al-Zanbaqi, M.S.; Felimban, A.A.; Alshuaibi, M.K.; Oraif, A. Outcomes and Complications After Repeat Cesarean Sections Among King Abdulaziz University Hospital Patients. Mater. Sociomed. 2019, 31, 119–124. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Practice Guidelines for Obstetric Anesthesia: An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology 2016, 124, 270–300. [Google Scholar] [CrossRef]
- Takeda, S.; Takeda, J.; Murayama, Y. Placenta Previa Accreta Spectrum: Cesarean Hysterectomy. Surg. J. 2021, 7, S28–S37. [Google Scholar] [CrossRef]
- Tol, I.D.; Yousif, M.; Collins, S.L. Post traumatic stress disorder (PTSD): The psychological sequelae of abnormally invasive placenta (AIP). Placenta 2019, 81, 42–45. [Google Scholar] [CrossRef]
- Bartels, H.C.; Horsch, A.; Cooney, N.; Brennan, D.J.; Lalor, J.G. Living beyond placenta accreta spectrum: Parent’s experience of the postnatal journey and recommendations for an integrated care pathway. BMC Pregnancy Childbirth 2022, 22, 397. [Google Scholar] [CrossRef]
- Collins, S.L.; Alemdar, B.; van Beekhuizen, H.J.; Bertholdt, C.; Braun, T.; Calda, P.; Delorme, P.; Duvekot, J.J.; Gronbeck, L.; Kayem, G.; et al. Evidence-based guidelines for the management of abnormally invasive placenta: Recommendations from the International Society for Abnormally Invasive Placenta. Am. J. Obstet. Gynecol. 2019, 220, 511–526. [Google Scholar] [CrossRef]
- Paping, A.; Bluth, A.; Al Naimi, A.; Mhallem, M.; Kolak, M.; Jaworowski, A.; Huras, H.; Morlando, M.; Daskalakis, G.; Pinto, P.V.; et al. Opportunities for, and barriers to, uterus-preserving surgical techniques for placenta accreta spectrum. Acta Obstet. Gynecol. Scand. 2025, 104, 8–19. [Google Scholar]
- Sentilhes, L.; Kayem, G.; Ambroselli, C.; Provansal, M.; Fernandez, H.; Perrotin, F.; Winer, N.; Pierre, F.; Benachi, A.; Dreyfus, M.; et al. Fertility and pregnancy outcomes following conservative treatment for placenta accreta. Hum. Reprod. 2010, 25, 2803–2810. [Google Scholar] [CrossRef] [PubMed]
- Zeybek, B.; Childress, A.M.; Kilic, G.S.; Phelps, J.Y.; Pacheco, L.D.; Carter, M.A.; Borahay, M.A. Management of the Jehovah’s Witness in Obstetrics and Gynecology: A Comprehensive Medical, Ethical, and Legal Approach. Obstet. Gynecol. Surv. 2016, 71, 488–500. [Google Scholar] [PubMed]
- Hudon, L.; Belfort, M.A.; Broome, D.R. Diagnosis and management of placenta percreta: A review. Obstet. Gynecol. Surv. 1998, 53, 509–517. [Google Scholar]
- Snegovskikh, D.; Clebone, A.; Norwitz, E. Anesthetic management of patients with placenta accreta and resuscitation strategies for associated massive hemorrhage. Curr. Opin. Anaesthesiol. 2011, 24, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Kuczkowski, K.M. Anesthesia for the repeat cesarean section in the parturient with abnormal placentation: What does an obstetrician need to know? Arch. Gynecol. Obstet. 2006, 273, 319–321. [Google Scholar]
- Wise, A.; Clark, V. Strategies to manage major obstetric haemorrhage. Curr. Opin. Anaesthesiol. 2008, 21, 281–287. [Google Scholar] [CrossRef]
- Palanisamy, A.; Mitani, A.A.; Tsen, L.C. General anesthesia for cesarean delivery at a tertiary care hospital from 2000 to 2005: A retrospective analysis and 10-year update. Int. J. Obstet. Anesthesia 2011, 20, 10–16. [Google Scholar] [CrossRef]
- Searle, R.D.; Lyons, G. Vanishing experience in training for obstetric general anaesthesia: An observational study. Int. J. Obstet. Anesth. 2008, 17, 233–237. [Google Scholar]
- Pather, S.; Strockyj, S.; Richards, A.; Campbell, N.; de Vries, B.; Ogle, R. Maternal outcome after conservative management of placenta percreta at caesarean section: A report of three cases and a review of the literature. Aust. N. Z. J. Obstet. Gynaecol. 2014, 54, 84–87. [Google Scholar] [CrossRef]
- Palacios Jaraquemada, J.M.; Pesaresi, M.; Nassif, J.C.; Hermosid, S. Anterior placenta percreta: Surgical approach, hemostasis and uterine repair. Acta Obstet. Gynecol. Scand. 2004, 83, 738–744. [Google Scholar]
- Clausen, C.; Stensballe, J.; Albrechtsen, C.K.; Hansen, M.A.; Lönn, L.; Langhoff-Roos, J. Balloon occlusion of the internal iliac arteries in the multidisciplinary management of placenta percreta. Acta Obstet. Gynecol. Scand. 2013, 92, 386–391. [Google Scholar] [PubMed]
- Hessami, K.; Kamepalli, S.; Lombaard, H.A.; Shamshirsaz, A.A.; Belfort, M.A.; Munoz, J.L. Conservative management of placenta accreta spectrum is associated with improved surgical outcomes compared to cesarean hysterectomy: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2025, 232, 432–452 e3. [Google Scholar] [CrossRef]
- Sentilhes, L.; Ambroselli, C.; Kayem, G.; Provansal, M.; Fernandez, H.; Perrotin, F.; Winer, N.; Pierre, F.; Benachi, A.; Dreyfus, M.; et al. Maternal outcome after conservative treatment of placenta accreta. Obstet. Gynecol. 2010, 115, 526–534. [Google Scholar] [CrossRef]
- Bretelle, F.; Courbière, B.; Mazouni, C.; Agostini, A.; Cravello, L.; Boubli, L.; Gamerre, M.; D’Ercole, C. Management of placenta accreta: Morbidity and outcome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 133, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Zuckerwise, L.C.; Craig, A.M.; Newton, J.M.; Zhao, S.; Bennett, K.A.; Crispens, M.A. Outcomes following a clinical algorithm allowing for delayed hysterectomy in the management of severe placenta accreta spectrum. Am. J. Obstet. Gynecol. 2020, 222, 179.e1–179.e9. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Lv, B.; He, G.; Liu, X. Internal iliac artery balloon occlusion during cesarean hysterectomy in women with placenta previa accreta. Int. J. Gynaecol. Obstet. 2019, 145, 110–115. [Google Scholar] [CrossRef]
- Liang, D.; Zhao, H.; Liu, D.; Lin, Y. Internal iliac artery balloon occlusion in the management of placenta accreta: A systematic review and meta-analysis. Eur. J. Radiol. 2021, 139, 109711. [Google Scholar] [CrossRef]
- Chen, D.; Xu, J.; Tian, Y.; Ling, Q.; Peng, B. Clinical evaluation of the effect for prophylactic balloon occlusion in pregnancies complicated with placenta accreta spectrum disorder: A systematic review and meta-analysis. Int. J. Gynaecol. Obstet. 2024, 167, 109–127. [Google Scholar]
- Dai, M.; Zhang, F.; Li, K.; Jin, G.; Chen, Y.; Zhang, X. The effect of prophylactic balloon occlusion in patients with placenta accreta spectrum: A Bayesian network meta-analysis. Eur. Radiol. 2022, 32, 3297–3308. [Google Scholar] [CrossRef]
- Alam, B.; Nasir, F.; Akbari, A.R.; Alali, B.; Khalil, Z. A Review and Comparison of the Efficacy of Prophylactic Interventional Radiological Arterial Occlusions in Placenta Accreta Spectrum Patients: A Meta-analysis. Acad. Radiol. 2023, 30, 1443–1455. [Google Scholar] [CrossRef]
- Liu, C.; Yang, D.D.; Qu, H.B.; Guo, Y.; Liu, L.J. Efficacy and safety of prophylactic abdominal aortic balloon occlusion versus internal iliac arterial balloon occlusion for placenta accreta spectrum disorder: A systematic review and meta-analysis. Clin. Imaging 2021, 78, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Fontenelle Ribeiro Junior, M.A.; Salman, S.M.; Al-Qaraghuli, S.M.; Makki, F.; Abu Affan, R.A.; Mohseni, S.R.; Brenner, M. Complications associated with the use of resuscitative endovascular balloon occlusion of the aorta (REBOA): An updated review. Trauma Surg. Acute Care Open 2024, 9, e001267. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Li, J.; Peng, B.; Cao, Y.; Liu, C.; Ye, P.; Li, K.; Zhao, F.; Qu, H.; Liu, L. Prophylactic internal Iliac artery balloon occlusion in placenta accreta spectrum: Evaluating efficacy, risks, and clinical implications. BMC Pregnancy Childbirth 2025, 25, 721. [Google Scholar] [CrossRef]
- Deshmukh, U.; Pabon-Ramos, W.; Ayyagari, R. The Role of Interventional Radiology in Managing Placenta Accreta Spectrum Disorder. Clin. Obstet. Gynecol. 2025, 68, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, J.L. Anesthesia-related maternal mortality. Clin. Obstet. Gynecol. 2003, 46, 679–687. [Google Scholar] [CrossRef]
- McDonnell, N.J.; Paech, M.J.; Clavisi, O.M.; Scott, K.L.; ANZCA Trials Group. Difficult and failed intubation in obstetric anaesthesia: An observational study of airway management and complications associated with general anaesthesia for caesarean section. Int. J. Obstet. Anesth. 2008, 17, 292–297. [Google Scholar]
- Lee, Y.L.; Lim, M.L.; Leong, W.L.; Lew, E. Difficult and failed intubation in Caesarean general anaesthesia: A four-year retrospective review. Singapore Med. J. 2022, 63, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.F.; Kim, D.; Mako, J.; Hand, K.; Brambrink, A.M. A retrospective study of the performance of video laryngoscopy in an obstetric unit. Anesth. Analg. 2012, 115, 904–906. [Google Scholar] [CrossRef] [PubMed]
| Proposed PAS Grade | Invasion Depth | Histologic Findings |
|---|---|---|
| PAS Grade 1 | Noninvasive | Grossly adherent placenta by manual palpation. Myometrial cross sections show a smooth placental-myometrial interface and uniform myometrial thickness without thinning. |
| PAS Grade 2 | Superficial invasion | Cross sections show an irregular placental–myometrial interface without involvement of the outer myometrium (i.e., preservation of >25% of the wall thickness relative to the uninvolved myometrium). |
| PAS Grade 3A | Deep invasion | Cross sections show an irregular placental–myometrial interface with involvement of the outer myometrium (i.e., with preservation of <25% of the wall thickness relative to the uninvolved myometrium). The serosa is intact. |
| PAS Grade 3D | Deep invasion with disruption of serosa | Deeply invasive placenta with disruption of the uterine serosal surface (D = deep invasion). |
| PAS Grade 3E | Deep invasion with adherent extrauterine structures | Placental invasion into adjacent organs or extrauterine fibroadipose tissue, confirmed by microscopy (E = extrauterine invasion). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shteynman, L.; Monanian, G.; Torres, G.; Sabetta, G.; Li, D.M.; Jin, Z.; Angelo, T.; Daoud, B.E.; Factor, M. Pathophysiology and Management of Placenta Accreta Spectrum. J. Dev. Biol. 2025, 13, 45. https://doi.org/10.3390/jdb13040045
Shteynman L, Monanian G, Torres G, Sabetta G, Li DM, Jin Z, Angelo T, Daoud BE, Factor M. Pathophysiology and Management of Placenta Accreta Spectrum. Journal of Developmental Biology. 2025; 13(4):45. https://doi.org/10.3390/jdb13040045
Chicago/Turabian StyleShteynman, Lana, Genevieve Monanian, Gilberto Torres, Giancarlo Sabetta, Deborah M. Li, Zhaosheng Jin, Tiffany Angelo, Bahaa E. Daoud, and Morgane Factor. 2025. "Pathophysiology and Management of Placenta Accreta Spectrum" Journal of Developmental Biology 13, no. 4: 45. https://doi.org/10.3390/jdb13040045
APA StyleShteynman, L., Monanian, G., Torres, G., Sabetta, G., Li, D. M., Jin, Z., Angelo, T., Daoud, B. E., & Factor, M. (2025). Pathophysiology and Management of Placenta Accreta Spectrum. Journal of Developmental Biology, 13(4), 45. https://doi.org/10.3390/jdb13040045






