SARS-CoV-2 Infection in Late Pregnancy and Childbirth from the Perspective of Perinatal Pathology
Abstract
:1. Introduction
2. SARS-CoV-2 Infection and Chronic Placental Pathology
3. Identification of SARS-CoV-2 in Placental and Fetal Tissues
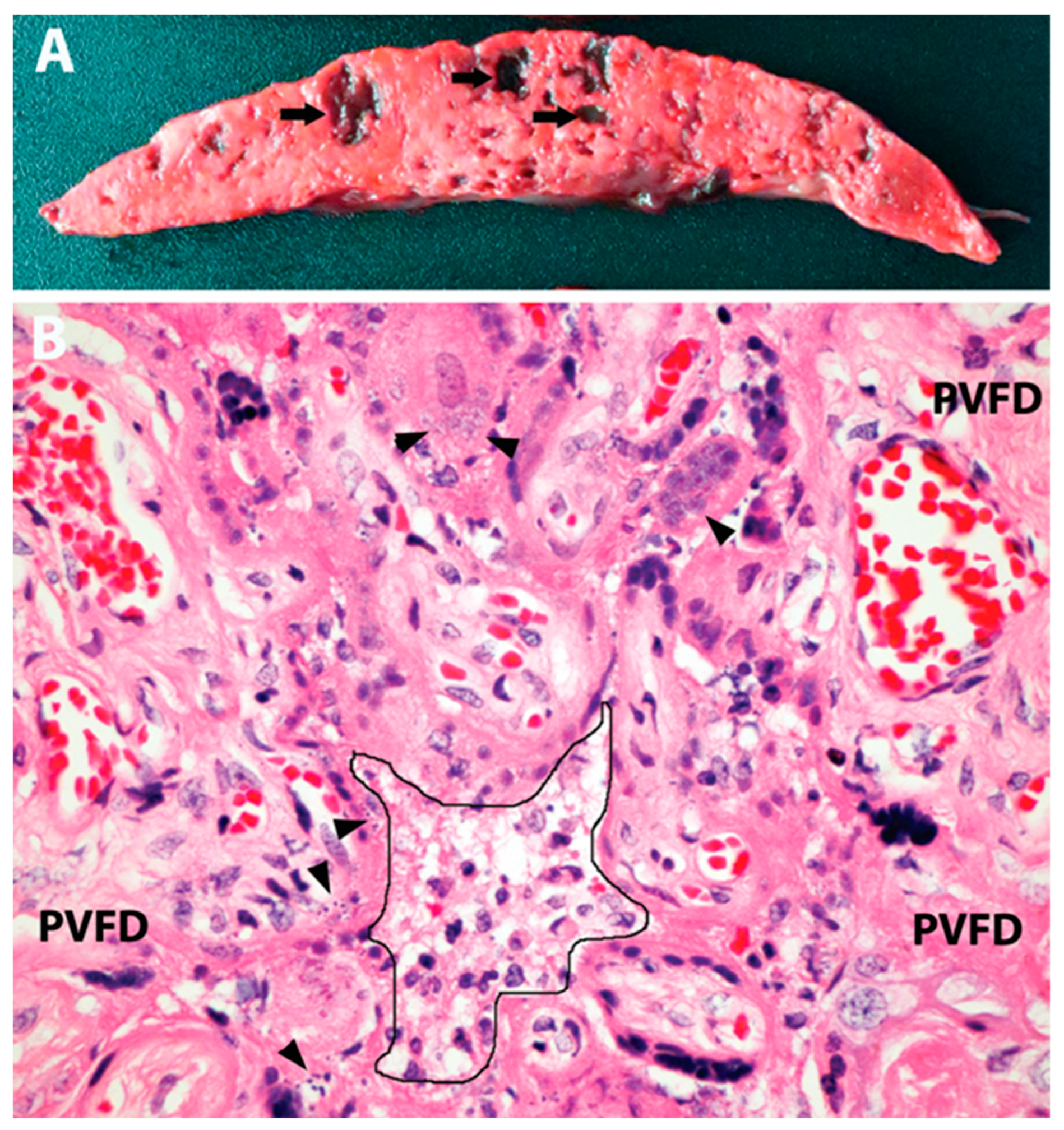
4. SARS-CoV-2 Placentitis
5. Massive Perivillous Fibrin Deposition as an End-Stage SARS-CoV-2 Placentitis Causing Hypoxic–Ischemic Fetal Death
6. Statistics of Increased COVID-19-Related Adverse Pregnancy Outcomes
7. Biology of Placental Response to SARS-CoV-2
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jering, K.S.; Claggett, B.L.; Cunningham, J.W.; Rosenthal, N.; Vardeny, O.; Greene, M.F.; Solomon, S.D. Clinical characteristics and outcomes of hospitalized women civing birth with and without COVID-19. JAMA Intern. Med. 2021, 181, 714–717. [Google Scholar] [CrossRef] [PubMed]
- Chinn, J.; Sedighim, S.; Kirby, K.A.; Hohmann, S.; Hameed, A.B.; Jolley, J.; Nguyen, N.T. Characteristics and Outcomes of Women with COVID-19 Giving Birth at US Academic Centers during the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2120456. [Google Scholar] [CrossRef] [PubMed]
- Gurol-Urganci, I.; Jardine, J.E.; Carroll, F.; Draycott, T.; Dunn, G.; Fremeaux, A.; Harris, T.; Hawdon, J.; Morris, E.; Muller, P.; et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: National cohort study. Am. J. Obstet. Gynecol. 2021, 225, 522.e1–522.e11. [Google Scholar] [CrossRef] [PubMed]
- DeSisto, C.L.; Wallace, B.; Simeone, R.M.; Polen, K.; Ko, J.Y.; Meaney-Delman, D.; Ellington, S.R. Risk for Stillbirth among Women with and without COVID-19 at Delivery Hospitalization—United States, March 2020–September 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Slack, J.C.; Parra-Herran, C. Life After Amsterdam: Placental Pathology Consensus Recommendations and Beyond. Surg. Pathol. Clin. 2022, 15, 175–196. [Google Scholar] [CrossRef]
- Shanes, E.D.; Mithal, L.B.; Otero, S.; Azad, H.A.; Miller, E.S.; Goldstein, J.A. Placental Pathology in COVID-19. Am. J. Clin. Pathol. 2020, 154, 23–32. [Google Scholar] [CrossRef]
- Pijnenborg, R.; Vercruysse, L.; Hanssens, M. The uterine spiral arteries in human pregnancy: Facts and controversies. Placenta 2006, 27, 939–958. [Google Scholar] [CrossRef]
- Baergen, R.N.; Heller, D.S. Placental Pathology in Covid-19 Positive Mothers: Preliminary Findings. Pediatr. Dev. Pathol. 2020, 23, 177–180. [Google Scholar] [CrossRef]
- Smithgall, M.C.; Liu-Jarin, X.; Hamele-Bena, D.; Cimic, A.; Mourad, M.; Debelenko, L.; Chen, X. Third-trimester placentas of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive women: Histomorphology, including viral immunohistochemistry and in-situ hybridization. Histopathology 2020, 77, 994–999. [Google Scholar] [CrossRef]
- Boyraz, B.; James, K.; Hornick, J.L.; Roberts, D.J. Placental pathology from COVID-19-recovered (nonacute) patients. Hum. Pathol. 2022, 125, 18–22. [Google Scholar] [CrossRef]
- Edlow, A.G.; Li, J.Z.; Collier, A.Y.; Atyeo, C.; James, K.E.; Boatin, A.A.; Gray, K.J.; Bordt, E.A.; Shook, L.L.; Yonker, L.M.; et al. Assessment of Maternal and Neonatal SARS-CoV-2 Viral Load, Transplacental Antibody Transfer, and Placental Pathology in Pregnancies During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2030455. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Skaria, P.; Kreutz, K.; Chen, L.; Hagemann, I.S.; Carter, E.B.; Mysorekar, I.U.; Nelson, D.M.; Pfeifer, J.; Dehner, L.P. Histopathology of Third Trimester Placenta from SARS-CoV-2-Positive Women. Fetal Pediatr. Pathol. 2022, 41, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Hecht, J.L.; Quade, B.; Deshpande, V.; Mino-Kenudson, M.; Ting, D.T.; Desai, N.; Dygulska, B.; Heyman, T.; Salafia, C.; Shen, D.; et al. SARS-CoV-2 can infect the placenta and is not associated with specific placental histopathology: A series of 19 placentas from COVID-19-positive mothers. Mod. Pathol. 2020, 33, 2092–2103. [Google Scholar] [CrossRef] [PubMed]
- Gulersen, M.; Prasannan, L.; Tam, H.T.; Metz, C.N.; Rochelson, B.; Meirowitz, N.; Shan, W.; Edelman, M.; Millington, K.A. Histopathological evaluation of placentas after diagnosis of maternal SARS-CoV-2 infection. Am. J. Obstet. Gynecol. 2020, 2, 100211. [Google Scholar] [CrossRef]
- Zhang, P.; Salafia, C.; Heyman, T.; Salafia, C.; Lederman, S.; Dygulska, B. Detection of severe acute respiratory syndrome coronavirus 2 in placentas with pathology and vertical transmission. Am. J. Obstet. Gynecol. 2020, 2, 100197. [Google Scholar] [CrossRef]
- Debelenko, L.; Katsyv, I.; Chong, A.M.; Peruyero, L.; Szabolcs, M.; Uhlemann, A.C. Trophoblast damage with acute and chronic intervillositis: Disruption of the placental barrier by severe acute respiratory syndrome coronavirus 2. Hum. Pathol. 2021, 109, 69–79. [Google Scholar] [CrossRef]
- Lin, R.; Forquer, H.; Cviko-Pajt, A.; Schauer, G.M.; Abellar, R.G.; Hedderson, M.; Kuzniewicz, M.W.; Greenberg, M.B. Placental Histopathologic Findings of a Large Cohort of Patients with SARS-CoV-2 Infection During Pregnancy. Int. J. Gynecol. Pathol. 2023, 42, 589–596. [Google Scholar] [CrossRef]
- Roberts, J.M.; Gammill, H.S. Preeclampsia: Recent insights. Hypertension 2005, 46, 1243–1249. [Google Scholar] [CrossRef]
- Yagel, S.; Cohen, S.M.M.; Admati, I.M.; Skarbianskis, N.M.; Solt, I.; Zeisel, A.; Beharier, O.; Goldman-Wohl, D. Expert Review: Preeclampsia Type I and Type II. Am. J. Obstet. Gynecol. 2023, 5, 101203. [Google Scholar] [CrossRef]
- Papageorghiou, A.T.; Deruelle, P.; Gunier, R.B.; Rauch, S.; García-May, P.K.; Mhatre, M.; Usman, M.A.; Abd-Elsalam, S.; Etuk, S.; Simmons, L.E.; et al. Preeclampsia and COVID-19: Results from the INTERCOVID prospective longitudinal study. Am. J. Obstet. Gynecol. 2021, 225, 289.e1–289.e17. [Google Scholar] [CrossRef]
- Mira, A.R.; De Pinho, A.; Calado-Araújo, M.; Ferreira, C.; David, D.; Enes, M.; Vaz-de-Macedo, C. COVID-19 and Hypertensive Disorders of Pregnancy (HDP): A Portuguese Multicentric Retrospective Cohort Study of HDP in SARS-CoV-2 Infected Patients. Cureus 2023, 15, e36483. [Google Scholar] [CrossRef] [PubMed]
- Örtqvist, A.K.; Magnus, M.C.; Dahlqvist, E.; Söderling, J.; Johansson, K.; Sandström, A.; Håberg, S.E.; Stephansson, O. Association between SARS-CoV-2 infection and newly diagnosed hypertension during pregnancy: Prospective, population based cohort study. BMJ Med. 2023, 2, e000465. [Google Scholar] [CrossRef] [PubMed]
- Serrano, B.; Bonacina, E.; Garcia-Ruiz, I.; Mendoza, M.; Garcia-Manau, P.; Garcia-Aguilar, P.; Gil, J.; Armengol-Alsina, M.; Fernández-Hidalgo, N.; Sulleiro, E.; et al. Confirmation of preeclampsia-like syndrome induced by severe COVID-19: An observational study. Am. J. Obstet. Gynecol. 2023, 5, 100760. [Google Scholar] [CrossRef] [PubMed]
- Redline, R.W.; Ravishankar, S.; Bagby, C.; Saab, S.; Zarei, S. Diffuse and Localized SARS-CoV-2 Placentitis: Prevalence and Pathogenesis of an Uncommon Complication of COVID-19 Infection During Pregnancy. Am. J. Surg. Pathol. 2022, 46, 1036–1047. [Google Scholar] [CrossRef]
- Penfield, C.A.; Brubaker, S.G.; Limaye, M.A.; Lighter, J.; Ratner, A.J.; Thomas, K.M.; Meyer, J.A.; Roman, A.S. Detection of severe acute respiratory syndrome coronavirus 2 in placental and fetal membrane samples. Am. J. Obstet. Gynecol. 2020, 2, 100133. [Google Scholar] [CrossRef]
- Valk, J.E.; Chong, A.M.; Uhlemann, A.C.; Debelenko, L. Detection of SARS-CoV-2 in placental but not fetal tissues in the second trimester. J. Perinatol. 2021, 41, 1184–1186. [Google Scholar] [CrossRef]
- Patanè, L.; Morotti, D.; Giunta, M.R.; Sigismondi, C.; Piccoli, M.G.; Frigerio, L.; Mangili, G.; Arosio, M.; Cornolti, G. Vertical transmission of coronavirus disease 2019: Severe acute respiratory syndrome coronavirus 2 RNA on the fetal side of the placenta in pregnancies with coronavirus disease 2019-positive mothers and neonates at birth. Am. J. Obstet. Gynecol. 2020, 2, 100145. [Google Scholar] [CrossRef]
- Hosier, H.; Farhadian, S.F.; Morotti, R.A.; Deshmukh, U.; Lu-Culligan, A.; Campbell, K.H.; Yasumoto, Y.; Vogels, C.B.; Casanovas-Massana, A.; Vijayakumar, P.; et al. SARS-CoV-2 infection of the placenta. J. Clin. Investig. 2020, 130, 4947–4953. [Google Scholar] [CrossRef]
- Sisman, J.; Jaleel, M.A.; Moreno, W.; Rajaram, V.; Collins, R.R.J.; Savani, R.C.; Rakheja, D.; Evans, A.S. Intrauterine Transmission of SARS-CoV-2 Infection in a Preterm Infant. Pediatr. Infect. Dis. J. 2020, 39, e265–e267. [Google Scholar] [CrossRef]
- Vivanti, A.J.; Vauloup-Fellous, C.; Prevot, S.; Zupan, V.; Suffee, C.; Do Cao, J.; Benachi, A.; De Luca, D. Transplacental transmission of SARS-CoV-2 infection. Nat. Commun. 2020, 11, 3572. [Google Scholar] [CrossRef]
- Hsu, A.L.; Guan, M.; Johannesen, E.; Stephens, A.J.; Khaleel, N.; Kagan, N.; Tuhlei, B.C.; Wan, X.F. Placental SARS-CoV-2 in a pregnant woman with mild COVID-19 disease. J. Med. Virol. 2021, 93, 1038–1044. [Google Scholar] [CrossRef] [PubMed]
- Linehan, L.; O’Donoghue, K.; Dineen, S.; White, J.; Higgins, J.R.; Fitzgerald, B. SARS-CoV-2 placentitis: An uncommon complication of maternal COVID-19. Placenta 2021, 104, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Roberts, D.J.; Edlow, A.G.; Romero, R.J.; Coyne, C.B.; Ting, D.T.; Hornick, J.L.; Zaki, S.R.; Das Adhikari, U.; Serghides, L.; Gaw, S.L.; et al. A standardized definition of placental infection by SARS-CoV-2, a consensus statement from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development SARS-CoV-2 Placental Infection Workshop. Am. J. Obstet. Gynecol. 2021, 225, 593.e1–593.e9. [Google Scholar] [CrossRef] [PubMed]
- Labarrere, C.; Mullen, E. Fibrinoid and trophoblastic necrosis with massive chronic intervillositis: An extreme variant of villitis of unknown etiology. Am. J. Reprod. Immunol. Microbiol. 1987, 15, 85–91. [Google Scholar] [CrossRef]
- Watkins, J.C.; Torous, V.F.; Roberts, D.J. Defining Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Placentitis. Arch. Pathol. Lab. Med. 2021, 145, 1341–1349. [Google Scholar] [CrossRef]
- Fitzgerald, B.; O’Donoghue, K.; McEntagart, N.; Gillan, J.E.; Kelehan, P.; O’Leary, J.; Downey, P.; Dean, J.; De Gascun, C.F.; Bermingham, J.; et al. Fetal Deaths in Ireland Due to SARS-CoV-2 Placentitis Caused by SARS-CoV-2 Alpha. Arch. Pathol. Lab. Med. 2022, 146, 529–537. [Google Scholar] [CrossRef]
- Stenton, S.; McPartland, J.; Shukla, R.; Turner, K.; Marton, T.; Hargitai, B.; Bamber, A.; Pryce, J.; Peres, C.L.; Burguess, N.; et al. SARS-CoV-2 placentitis and pregnancy outcome: A multicentre experience during the Alpha and early Delta waves of coronavirus pandemic in England. eClinicalMedicine 2022, 47, 101389. [Google Scholar] [CrossRef]
- Konstantinidou, A.E.; Angelidou, S.; Havaki, S.; Paparizou, K.; Spanakis, N.; Chatzakis, C.; Sotiriadis, A.; Theodora, M.; Donoudis, C.; Daponte, A.; et al. Stillbirth due to SARS-CoV-2 placentitis without evidence of intrauterine transmission to fetus: Association with maternal risk factors. Ultrasound Obstet. Gynecol. 2022, 59, 813–822. [Google Scholar] [CrossRef]
- Nielsen, S.Y.; Hvidman, L.E.; Aabakke, A.J.M.; Olsen, T.E.; Johnsen, I.B.G.; Bogaard, P.W.; Petersen, A.; Westergaard, H.B.; Sørensen, A.; Hedermann, G.; et al. SARS-CoV-2 placentitis and severe pregnancy outcome after maternal infection: A Danish case series. Acta Obstet. Gynecol. Scand. 2023, 102, 567–576. [Google Scholar] [CrossRef]
- Delle Chiaie, L.; Stolpner, I.; Dettmer, M.S.; Baltz-Ghahremanpour, K. Acute placental insufficiency two weeks after an asymptomatic COVID-19 maternal infection: The deleterious effects of the SARS-CoV-2 placentitis. Arch. Gynecol. Obstet. 2023, 308, 1–4. [Google Scholar] [CrossRef]
- Corn, M.; Pham, T.; Kemp, W. Adverse Fetal Outcomes and Histopathology of Placentas Affected by COVID-19: A Report of Four Cases. Cureus 2023, 15, e44402. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Pontnou, M.; Navarro, A.; Camacho, J.; Crispi, F.; Alguacil-Guillén, M.; Moreno-Baró, A.; Hernandez-Losa, J.; Sesé, M.; Cajal, S.R.Y.; Garcia Ruíz, I.; et al. Diffuse trophoblast damage is the hallmark of SARS-CoV-2-associated fetal demise. Mod. Pathol. 2021, 34, 1704–1709. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A.; Avvad-Portari, E.; Babál, P.; Baldewijns, M.; Blomberg, M.; Bouachba, A.; Camacho, J.; Collardeau-Frachon, S.; Colson, A.; Dehaene, I.; et al. Placental Tissue Destruction and Insufficiency From COVID-19 Causes Stillbirth and Neonatal Death From Hypoxic-Ischemic Injury. Arch. Pathol. Lab. Med. 2022, 146, 660–676. [Google Scholar] [CrossRef] [PubMed]
- Horn, L.C.; Krücken, I.; Hiller, G.G.R.; Niedermair, M.; Perac, K.; Pietsch, C.; Höhn, A.K. Placental pathology in sudden intrauterine death (SIUD) in SARS-CoV-2-positive oligosymptomatic women. Arch. Gynecol. Obstet. 2023, 307, 1811–1822. [Google Scholar] [CrossRef] [PubMed]
- Mourad, M.; Jacob, T.; Sadovsky, E.; Bejerano, S.; Simone, G.S.; Bagalkot, T.R.; Zucker, J.; Yin, M.T.; Chang, J.Y.; Liu, L.; et al. Placental response to maternal SARS-CoV-2 infection. Sci. Rep. 2021, 11, 14390. [Google Scholar] [CrossRef]
- Thomas, J.; Sun, Y.; Debelenko, L. Infrequent Placental and Fetal Involvement in SARS-CoV-2 Infection: Pathology Data from a Large Medical Center. J. Dev. Biol. 2021, 9, 45. [Google Scholar] [CrossRef]
- Nkobetchou, M.; Leruez-Ville, M.; Guilleminot, T.; Roux, N.; Petrilli, G.; Guimiot, F.; Saint-Frison, M.H.; Deryabin, I.; Ville, Y.; Faure Bardon, V. Assessing importance of SARS-CoV2 infection as cause of in utero fetal death: Regional retrospective cohort study. Ultrasound Obstet. Gynecol. 2023, 62. [Google Scholar] [CrossRef]
- Schwartz, D.A.; Morotti, D.; Beigi, B.; Moshfegh, F.; Zafaranloo, N.; Patanè, L. Confirming Vertical Fetal Infection with Coronavirus Disease 2019: Neonatal and Pathology Criteria for Early Onset and Transplacental Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 from Infected Pregnant Mothers. Arch. Pathol. Lab. Med. 2020, 144, 1451–1456. [Google Scholar] [CrossRef]
- Schwartz, D.A.; Mulkey, S.B.; Roberts, D.J. SARS-CoV-2 placentitis, stillbirth, and maternal COVID-19 vaccination: Clinical-pathologic correlations. Am. J. Obstet. Gynecol. 2023, 228, 261–269. [Google Scholar] [CrossRef]
- King, A. Doctors Investigate Several Stillbirths among Moms with COVID-19. 2021. Available online: https://www.the-scientist.com/news-opinion/doctors-investigate-several-stillbirths-among-moms-with-covid-19-68703 (accessed on 25 September 2023).
- Zaigham, M.; Gisselsson, D.; Sand, A.; Wikström, A.K.; von Wowern, E.; Schwartz, D.A.; Iorizzo, L.; Nelander, M.; Blomberg, M.; Papadogiannakis, N.; et al. Clinical-pathological features in placentas of pregnancies with SARS-CoV-2 infection and adverse outcome: Case series with and without congenital transmission. BJOG 2022, 129, 1361–1374. [Google Scholar] [CrossRef]
- Katzman, P.J.; Genest, D.R. Maternal floor infarction and massive perivillous fibrin deposition: Histological definitions, association with intrauterine fetal growth restriction, and risk of recurrence. Pediatr. Dev. Pathol. 2002, 5, 159–164, Erratum in Pediatr. Dev. Pathol. 2003, 6, 102. [Google Scholar] [CrossRef]
- Reagan-Steiner, S.; Bhatnagar, J.; Martines, R.B.; Milligan, N.S.; Gisondo, C.; Williams, F.B.; Lee, E.; Estetter, L.; Bullock, H.; Goldsmith, C.S.; et al. Detection of SARS-CoV-2 in Neonatal Autopsy Tissues and Placenta. Emerg. Infect. Dis. 2022, 28, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Vercoutere, A.; Zina, M.J.; Benoit, K.; Costa, E.; Derisbourg, S.; Boulvain, M.; Roelens, K.; Vandenberghe, G.; Daelemans, C.; B. OSS Collaborating Group. Late miscarriage and stillbirth in asymptomatic and symptomatic hospitalised pregnant women in Belgium during the first and second waves of COVID-19: A prospective nationwide population-based study. BMC Pregnancy Childbirth 2023, 23, 356. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Chen, L.; Zhang, J.; Xiong, C.; Li, X. The SARS-CoV-2 receptor ACE2 expression of maternal-fetal interface and fetal organs by single-cell transcriptome study. PLoS ONE 2020, 15, e0230295. [Google Scholar] [CrossRef]
- Ouyang, Y.; Bagalkot, T.; Fitzgerald, W.; Sadovsky, E.; Chu, T.; Martínez-Marchal, A.; Brieño-Enríquez, M.; Su, E.J.; Margolis, L.; Sorkin, A.; et al. Term Human Placental Trophoblasts Express SARS-CoV-2 Entry Factors ACE2, TMPRSS2, and Furin. mSphere 2021, 6, e00250-21. [Google Scholar] [CrossRef]
- Lyu, T.; Liang, C.; Liu, J.; Hung, P.; Zhang, J.; Campbell, B.; Ghumman, N.; Olatosi, B.; Hikmet, N.; Zhang, M.; et al. Risk for stillbirth among pregnant individuals with SARS-CoV-2 infection varied by gestational age. Am. J. Obstet. Gynecol. 2023, 229, 288.e1–288.e13. [Google Scholar] [CrossRef]
- Chen, J.; Neil, J.A.; Tan, J.P.; Rudraraju, R.; Mohenska, M.; Sun, Y.B.Y.; Walters, E.; Bediaga, N.G.; Sun, G.; Zhou, Y.; et al. A placental model of SARS-CoV-2 infection reveals ACE2-dependent susceptibility and differentiation impairment in syncytiotrophoblasts. Nat. Cell Biol. 2023, 25, 1223–1234. [Google Scholar] [CrossRef]
- Lu-Culligan, A.; Chavan, A.R.; Vijayakumar, P.; Irshaid, L.; Courchaine, E.M.; Milano, K.M.; Tang, Z.; Pope, S.D.; Song, E.; Vogels, C.B.F.; et al. Maternal respiratory SARS-CoV-2 infection in pregnancy is associated with a robust inflammatory response at the maternal-fetal interface. Med 2021, 2, 591–610.e10. [Google Scholar] [CrossRef]
- Chan, E.S.; de Koning, L.; Yu, W.; Chadha, R. C4d Staining Is Present in Normal Placentas from Pregnancies Prior to Pregnancy Loss Associated with Chronic Histiocytic Intervillositis and Is Reduced by Immunomodulatory Therapy in Subsequent Pregnancies. Pediatr. Dev. Pathol. 2023, 26, 10935266231176682. [Google Scholar] [CrossRef]
- Redline, R.W. Extending the Spectrum of Massive Perivillous Fibrin Deposition (Maternal Floor Infarction). Pediatr. Dev. Pathol. 2021, 24, 10–11. [Google Scholar] [CrossRef] [PubMed]
- Mithal, L.B.; Otero, S.; Simons, L.M.; Hultquist, J.F.; Miller, E.S.; Ozer, E.A.; Shanes, E.D.; Goldstein, J.A. Low-level SARS-CoV-2 viremia coincident with COVID placentitis and stillbirth. Placenta 2022, 121, 79–81. [Google Scholar] [CrossRef]
- Shook, L.L.; Atyeo, C.G.; Yonker, L.M.; Fasano, A.; Gray, K.J.; Alter, G.; Edlow, A.G. Durability of Anti-Spike Antibodies in Infants After Maternal COVID-19 Vaccination or Natural Infection. JAMA 2022, 327, 1087–1089. [Google Scholar] [CrossRef] [PubMed]
- Trostle, M.E.; Aguero-Rosenfeld, M.E.; Roman, A.S.; Lighter, J.L. High antibody levels in cord blood from pregnant women vaccinated against COVID-19. Am. J. Obstet. Gynecol. 2021, 3, 100481. [Google Scholar] [CrossRef] [PubMed]

| Publication | Number of Cases | Extent of Placental Involvement by Destructive Pathology (PVFD) | Number of Autopsies Performed | Fetal Hypoxic–Ischemic Injury Identified | SARS-CoV-2 Detected in Fetal or Neonatal Tissues | Duration of Infection and/or Fetal Distress | Maternal SARS-CoV-2 Severity | Associated Conditions |
|---|---|---|---|---|---|---|---|---|
| Fitzgerald et al. [36] | 6 | 80–90% | 5 | Not Reported | 0 | 2–21 days | 5 mild 1 asymptomatic | Thrombocytopenia (3 of 6) |
| Schwartz et al. [43] | 68 | 35–100%, mean 77.7% | 30 | 19 | 16 | ≈2 weeks | No severe COVID-19 reported | Not Reported |
| Konstantinidou et al. [38] | 6 | >75% | 3 | 3 | 0 | 3–5 days | 4 mild 2 asymptomatic | Thrombophilia FGR Multiple Sclerosis |
| Zaigham et al. [51] | 7 | >72% | 4 | 4 | 2 | 2–25 days | 4 mild-to-moderate 3 asymptomatic | No significant reported |
| Nielsen et al. [39] | 10 | 60–90% | 8 | Not Reported | 3 | 12 days on average | 1 severe 8 mild-to-moderate 1 not reported | No significant reported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Debelenko, L. SARS-CoV-2 Infection in Late Pregnancy and Childbirth from the Perspective of Perinatal Pathology. J. Dev. Biol. 2023, 11, 42. https://doi.org/10.3390/jdb11040042
Debelenko L. SARS-CoV-2 Infection in Late Pregnancy and Childbirth from the Perspective of Perinatal Pathology. Journal of Developmental Biology. 2023; 11(4):42. https://doi.org/10.3390/jdb11040042
Chicago/Turabian StyleDebelenko, Larisa. 2023. "SARS-CoV-2 Infection in Late Pregnancy and Childbirth from the Perspective of Perinatal Pathology" Journal of Developmental Biology 11, no. 4: 42. https://doi.org/10.3390/jdb11040042
APA StyleDebelenko, L. (2023). SARS-CoV-2 Infection in Late Pregnancy and Childbirth from the Perspective of Perinatal Pathology. Journal of Developmental Biology, 11(4), 42. https://doi.org/10.3390/jdb11040042






