Associations Between Triglycerides and Walking Capacity in Community-Dwelling Older Adults with Metabolic Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Demographic, Anthropometric, and Metabolic Assessment
2.3. Functional Assessments
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Associations Between Triglyceride Levels and Physiological-Functional Outcomes
3.3. Predictors of Six-Minute Walk Distance
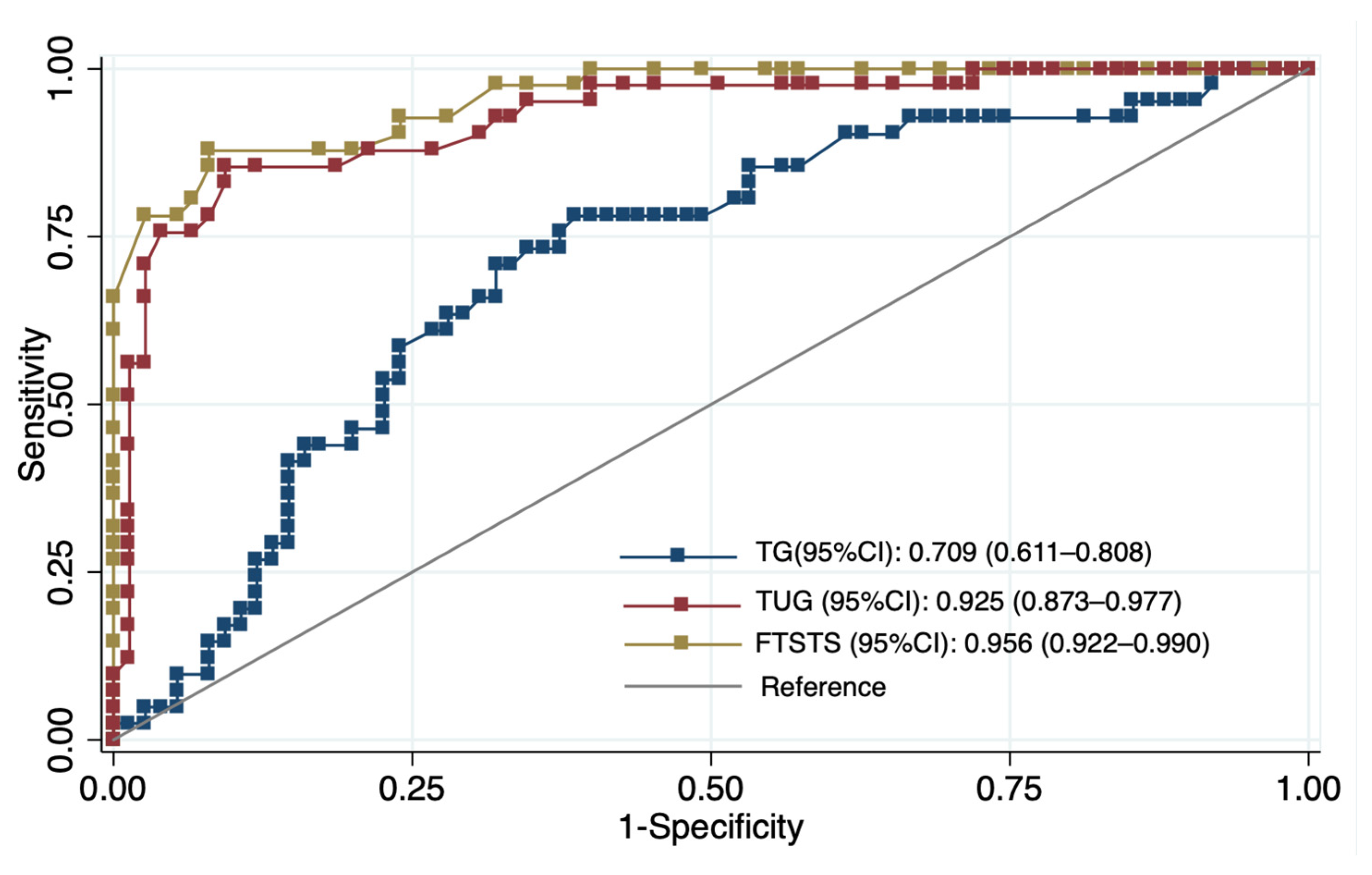
3.4. Discriminatory Accuracy for Identifying Low Walking Capacity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 6MWD | Six-Minute Walk Distance |
| 6MWT | Six-Minute Walk Test |
| AUC | Area Under the Curve |
| BMI | Body Mass Index |
| DBP | Diastolic Blood Pressure |
| FBG | Fasting Blood Glucose |
| FTSST | Five-Times-Sit-to-Stand Test |
| GPAQ | Global Physical Activity Questionnaire |
| HDL-C | High-Density Lipoprotein Cholesterol |
| HR | Heart Rate |
| MET | Metabolic Equivalent of Task |
| MetS | Metabolic Syndrome |
| SBP | Systolic Blood Pressure |
| SpO2 | Peripheral Oxygen Saturation |
| TG | Triglycerides |
| TG/HDL-C | Triglyceride-to-HDL Cholesterol Ratio |
| TUG | Timed-Up-and-Go Test |
| VO2max | Maximal Oxygen Uptake |
| WC | Waist Circumference |
References
- Ricardo, S.; Araujo, M.; Santos, L.; Romanzini, M.; Fernandes, R.; Turi-Lynch, B.; Codogno, J. Burden of metabolic syndrome on primary healthcare costs among older adults: A cross-sectional study. Sao Paulo Med. J. 2024, 142, e2023215. [Google Scholar] [CrossRef]
- Limon, V.M.; Lee, M.; Gonzalez, B.; Choh, A.C.; Czerwinski, S.A. The impact of metabolic syndrome on mental health-related quality of life and depressive symptoms. Qual. Life Res. 2020, 29, 2063–2072. [Google Scholar] [CrossRef]
- Hamooya, B.M.; Siame, L.; Muchaili, L.; Masenga, S.K.; Kirabo, A. Metabolic syndrome: Epidemiology, mechanisms, and current therapeutic approaches. Front. Nutr. 2025, 12, 1661603. [Google Scholar] [CrossRef]
- Devesa, A.; Delgado, V.; Valkovic, L.; Lima, J.A.C.; Nagel, E.; Ibanez, B.; Raman, B. Multiorgan Imaging for Interorgan Crosstalk in Cardiometabolic Diseases. Circ. Res. 2025, 136, 1454–1475. [Google Scholar] [CrossRef]
- Vesa, C.M.; Zaha, D.C.; Bungău, S.G. Molecular Mechanisms of Metabolic Syndrome. Int. J. Mol. Sci. 2024, 25, 5452. [Google Scholar] [CrossRef]
- Tahir, U.A.; Gerszten, R.E. Molecular Biomarkers for Cardiometabolic Disease: Risk Assessment in Young Individuals. Circ. Res. 2023, 132, 1663–1673. [Google Scholar] [CrossRef] [PubMed]
- Talayero, B.G.; Sacks, F.M. The role of triglycerides in atherosclerosis. Curr. Cardiol. Rep. 2011, 13, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Buring, J.E.; Cook, N.R.; Rifai, N. C-Reactive Protein, the Metabolic Syndrome, and Risk of Incident Cardiovascular Events. Circulation 2003, 107, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Morgado, F.; Valado, A.; Metello, J.; Pereira, L. Laboratory markers of metabolic syndrome. Explor. Cardiol. 2024, 2, 114–133. [Google Scholar] [CrossRef]
- Chait, A.; den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7, 522637. [Google Scholar] [CrossRef]
- Finelli, C.; Tarantino, G. What is the role of adiponectin in obesity related non-alcoholic fatty liver disease? World J. Gastroenterol. 2013, 19, 802–812. [Google Scholar] [CrossRef]
- Shen, J.; Poole, J.C.; Topel, M.L.; Bidulescu, A.; Morris, A.A.; Patel, R.S.; Binongo, J.G.; Dunbar, S.B.; Phillips, L.; Vaccarino, V.; et al. Subclinical Vascular Dysfunction Associated with Metabolic Syndrome in African Americans and Whites. J. Clin. Endocrinol. Metab. 2015, 100, 4231–4239. [Google Scholar] [CrossRef]
- Kim, M.; Kobori, T. Nutrient deficiency and physical inactivity in middle-aged adults with dynapenia and metabolic syndrome: Results from a nationwide survey. Nutr. Metab. 2025, 22, 88. [Google Scholar] [CrossRef]
- Zeng, P.; Li, M.; Cao, J.; Zeng, L.; Jiang, C.; Lin, F. Association of metabolic syndrome severity with frailty progression among Chinese middle and old-aged adults: A longitudinal study. Cardiovasc. Diabetol. 2024, 23, 302. [Google Scholar] [CrossRef]
- Penninx, B.W.; Nicklas, B.J.; Newman, A.B.; Harris, T.B.; Goodpaster, B.H.; Satterfield, S.; de Rekeneire, N.; Yaffe, K.; Pahor, M.; Kritchevsky, S.B. Metabolic syndrome and physical decline in older persons: Results from the Health, Aging And Body Composition Study. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Farias, D.L.; Tibana, R.A.; Teixeira, T.G.; Vieira, D.C.; Tarja, V.; Nascimento Dda, C.; Silva Ade, O.; Funghetto, S.S.; Coura, M.A.; Valduga, R.; et al. Elderly women with metabolic syndrome present higher cardiovascular risk and lower relative muscle strength. Einstein 2013, 11, 174–179. [Google Scholar] [CrossRef]
- Vieira, D.C.; Tibana, R.A.; Tajra, V.; Nascimento Dda, C.; de Farias, D.L.; Silva Ade, O.; Teixeira, T.G.; Fonseca, R.M.; de Oliveira, R.J.; Mendes, F.A.; et al. Decreased functional capacity and muscle strength in elderly women with metabolic syndrome. Clin. Interv. Aging 2013, 8, 1377–1386. [Google Scholar] [CrossRef]
- Collins, K.H.; Herzog, W.; MacDonald, G.Z.; Reimer, R.A.; Rios, J.L.; Smith, I.C.; Zernicke, R.F.; Hart, D.A. Obesity, metabolic syndrome, and musculoskeletal disease: Common inflammatory pathways suggest a central role for loss of muscle integrity. Front. Physiol. 2018, 9, 112. [Google Scholar] [CrossRef] [PubMed]
- Harridge, S.D.R.; Lazarus, N.R. Physical activity, aging, and physiological function. Physiology 2017, 32, 152–161. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Bautmans, I.; Lambert, M.; Mets, T. The six-minute walk test in community dwelling elderly: Influence of health status. BMC Geriatr. 2004, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Rasekaba, T.; Lee, A.L.; Naughton, M.T.; Williams, T.J.; Holland, A.E. The six-minute walk test: A useful metric for the cardiopulmonary patient. Intern. Med. J. 2009, 39, 495–501. [Google Scholar] [CrossRef]
- Enright, P.; McBurnie, M.A.; Bittner, V.; Tracy, R.; McNamara, R.; Arnold, A.; Newman, A. The 6-min Walk Test: A quick measure of functional status in elderly adults. Chest 2003, 123, 387–398. [Google Scholar] [CrossRef]
- Strath, S.; Swartz, A.; Parker, S.; Miller, N.; Cieslik, L. Walking and metabolic syndrome in older adults. J. Phys. Act. Health 2007, 4, 397–410. [Google Scholar] [CrossRef] [PubMed]
- Ubuane, P.; Animasahun, B.; Ajiboye, O.; Kayode-Awe, O.; Ajayi, O.; Njokanma, F. The historical evolution of the six-minute walk test as a measure of functional exercise capacity: A narrative review. J. Xiangya Med. 2018, 3, 40. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Son, K.Y.; Shin, D.W.; Lee, J.E.; Kim, S.H.; Yun, J.M.; Cho, B. Association of metabolic syndrome with mobility in the older adults: A Korean nationwide representative cross-sectional study. Sci. Rep. 2021, 11, 6605. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef]
- Jaturapatporn, D.; Hathirat, S.; Manataweewat, B.; Dellow, A.C.; Leelaharattanarak, S.; Sirimothya, S.; Dellow, J.; Udomsubpayakul, U. Reliability and validity of a Thai version of the General Practice Assessment Questionnaire (GPAQ). J. Med. Assoc. Thai 2006, 89, 1491–1496. [Google Scholar]
- Muñoz-Bermejo, L.; Adsuar, J.C.; Mendoza-Muñoz, M.; Barrios-Fernández, S.; Garcia-Gordillo, M.A.; Pérez-Gómez, J.; Carlos-Vivas, J. Test-retest reliability of five times sit to stand test (FTSST) in adults: A systematic review and meta-analysis. Biology 2021, 10, 510. [Google Scholar] [CrossRef]
- Herman, T.; Giladi, N.; Hausdorff, J.M. Properties of the ‘timed up and go’ test: More than meets the eye. Gerontology 2011, 57, 203–210. [Google Scholar] [CrossRef]
- He, H.; Pan, L.; Wang, D.; Liu, F.; Du, J.; Pa, L.; Wang, X.; Cui, Z.; Ren, X.; Wang, H.; et al. Normative values of hand grip strength in a large unselected Chinese population: Evidence from the China National Health Survey. J. Cachexia Sarcopenia Muscle 2023, 14, 1312–1321. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E. Measuring functional. J. Act. Aging 2002, 1, 24–30. [Google Scholar]
- Kim, B.; Ku, M.; Kiyoji, T.; Isobe, T.; Sakae, T.; Oh, S. Cardiorespiratory fitness is strongly linked to metabolic syndrome among physical fitness components: A retrospective cross-sectional study. J. Physiol. Anthr. 2020, 39, 30. [Google Scholar] [CrossRef] [PubMed]
- Babb, T.G. Obesity: Challenges to ventilatory control during exercise—A brief review. Respir. Physiol. Neurobiol. 2013, 189, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Green, S.; Egaña, M.; Baldi, J.C.; Lamberts, R.; Regensteiner, J.G. Cardiovascular control during exercise in type 2 diabetes mellitus. J. Diabetes Res. 2015, 2015, 654204. [Google Scholar] [CrossRef]
- Rhynehart, A.; Dunlevy, C.; Hayes, K.; O’Connell, J.; O’Shea, D.; O’Malley, E. The Association of Physical Function Measures with Frailty, Falls History, and Metabolic Syndrome in a Population with Complex Obesity. Front. Rehabil. Sci. 2021, 2, 716392. [Google Scholar] [CrossRef]
- Chen, M.Z.; Wong, M.W.K.; Lim, J.Y.; Merchant, R.A. Frailty and Quality of Life in Older Adults with Metabolic Syndrome—Findings from the Healthy Older People Everyday (HOPE) Study. J. Nutr. Health Aging 2021, 25, 637–644. [Google Scholar] [CrossRef]
- Muollo, V.; D’Emanuele, S.; Ghiotto, L.; Rudi, D.; Schena, F.; Tarperi, C. Evaluating handgrip strength and functional tests as indicators of gait speed in older females. Front. Sports Act. Living 2025, 7, 1497546. [Google Scholar] [CrossRef]
- Baer, M.; Klemetson, B.; Scott, D.; Murtishaw, A.S.; Navalta, J.W.; Kinney, J.W.; Landers, M.R. Effects of Fatigue on Balance in Individuals with Parkinson Disease: Influence of Medication and Brain-Derived Neurotrophic Factor Genotype. J. Neurol. Phys. Ther. 2018, 42, 61–71. [Google Scholar] [CrossRef]
- Huang, Y.; Liao, J.; Liu, Y. Triglyceride to high-density lipoprotein cholesterol ratio was negatively associated with relative grip strength in older adults: A cross-sectional study of the NHANES database. Front. Public Health 2023, 11, 1222636. [Google Scholar] [CrossRef]
- Lu, H.; Liang, W.; Huang, H.; Huang, K.; Zeng, L.; Yang, L. Association of metabolic syndrome components and their combinations with functional disability among older adults in a longevity-associated ethnic minority region of Southwest China. Front. Public Health 2025, 13, 1635390. [Google Scholar] [CrossRef]
- Green, D.J.; Hopman, M.T.; Padilla, J.; Laughlin, M.H.; Thijssen, D.H. Vascular adaptation to exercise in humans: Role of hemodynamic stimuli. Physiol. Rev. 2017, 97, 495–528. [Google Scholar] [CrossRef] [PubMed]
- Meex, R.C.R.; Blaak, E.E.; van Loon, L.J.C. Lipotoxicity plays a key role in the development of both insulin resistance and muscle atrophy in patients with type 2 diabetes. Obes. Rev. 2019, 20, 1205–1217. [Google Scholar] [CrossRef]
- Ramos, S.V.; Distefano, G.; Lui, L.-Y.; Cawthon, P.M.; Kramer, P.; Sipula, I.J.; Bello, F.M.; Mau, T.; Jurczak, M.J.; Molina, A.J.; et al. Role of Cardiorespiratory Fitness and Mitochondrial Oxidative Capacity in Reduced Walk Speed of Older Adults with Diabetes. Diabetes 2024, 73, 1048–1057. [Google Scholar] [CrossRef] [PubMed]
- Itani, S.I.; Ruderman, N.B.; Schmieder, F.; Boden, G. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IkappaB-alpha. Diabetes 2002, 51, 2005–2011. [Google Scholar] [CrossRef]
- Kolka, C.M. The Skeletal Muscle Microvasculature and Its Effects on Metabolism. In Microcirculation Revisited—From Molecules to Clinical Practice; Lenasi, H., Ed.; IntechOpen: London, UK, 2016. [Google Scholar]
- Barazzoni, R.; Bischoff, S.; Boirie, Y.; Busetto, L.; Cederholm, T.; Dicker, D.; Toplak, H.; Van Gossum, A.; Yumuk, V.; Vettor, R. Sarcopenic obesity: Time to meet the challenge. Obes. Facts 2018, 11, 294–305. [Google Scholar] [CrossRef]
- Brun, J.; Connes, P.; Varlet-Marie, E. Alterations of blood rheology during and after exercise are both consequences and modifiers of body’s adaptation to muscular activity. Sci. Sports 2007, 22, 251–266. [Google Scholar] [CrossRef]
- Fiorentino, T.V.; Prioletta, A.; Zuo, P.; Folli, F. Hyperglycemia-induced oxidative stress and its role in diabetes mellitus related cardiovascular diseases. Curr. Pharm. Des. 2013, 19, 5695–5703. [Google Scholar] [CrossRef]
- Gaur, K.; Mohapatra, L.; Wal, P.; Parveen, A.; Kumar, S.; Gupta, V. Deciphering the mechanisms and effects of hyperglycemia on skeletal muscle atrophy. Metab. Open 2024, 24, 100332. [Google Scholar] [CrossRef]
- Sarvestan, J.; Kovacikova, Z.; Linduska, P.; Gonosova, Z.; Svoboda, Z. Contribution of lower limb muscle strength to walking, postural sway and functional performance in elderly women. Isokinet. Exerc. Sci. 2021, 29, 49–57. [Google Scholar] [CrossRef]
- Wu, R.; Zhang, Y.; Bai, J.-J.; Sun, J.; Bao, Z.-J.; Wang, Z. Impact of lower limb muscle strength on walking function beyond aging and diabetes. J. Int. Med. Res. 2020, 48, 030006052092882. [Google Scholar] [CrossRef]
- Newman, A.B.; Haggerty, C.L.; Kritchevsky, S.B.; Nevitt, M.C.; Simonsick, E.M. Walking Performance and Cardiovascular Response: Associations with Age and Morbidity—The Health, Aging and Body Composition Study. J. Gerontol. Ser. A 2003, 58, M715–M720. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.; Collier, Z.; Reisman, D.S. Beyond steps per day: Other measures of real-world walking after stroke related to cardiovascular risk. J. Neuroeng. Rehabil. 2022, 19, 111. [Google Scholar] [CrossRef] [PubMed]
- Joyner, M.J.; Casey, D.P. Regulation of increased blood flow (hyperemia) to muscles during exercise: A hierarchy of competing physiological needs. Physiol. Rev. 2015, 95, 549–601. [Google Scholar] [CrossRef]
- Endukuru, C.K.; Gaur, G.S.; Yerrabelli, D.; Sahoo, J.; Vairappan, B. Impaired baroreflex sensitivity and cardiac autonomic functions are associated with cardiovascular disease risk factors among patients with metabolic syndrome in a tertiary care teaching hospital of South-India. Diabetes Metab. Syndr. 2020, 14, 2043–2051. [Google Scholar] [CrossRef]
- Okada, Y.; Galbreath, M.M.; Shibata, S.; Jarvis, S.S.; VanGundy, T.B.; Meier, R.L.; Vongpatanasin, W.; Levine, B.D.; Fu, Q. Relationship Between Sympathetic Baroreflex Sensitivity and Arterial Stiffness in Elderly Men and Women. Hypertension 2012, 59, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Monahan, K.D. Effect of aging on baroreflex function in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 293, R3–R12. [Google Scholar] [CrossRef]
- Parhofer, K.G.; Laufs, U. The diagnosis and treatment of hypertriglyceridemia. Dtsch. Arztebl. Int. 2019, 116, 825–832. [Google Scholar] [CrossRef]
- Garg, R.; Aggarwal, S.; Kumar, R.; Sharma, G. Association of atherosclerosis with dyslipidemia and co-morbid conditions: A descriptive study. J. Nat. Sci. Biol. Med. 2015, 6, 163–168. [Google Scholar] [CrossRef]
- Bonen, A.; Parolin, M.L.; Steinberg, G.R.; Calles-Escandon, J.; Tandon, N.N.; Glatz, J.F.; Luiken, J.J.; Heigenhauser, G.J.; Dyck, D.J. Triacylglycerol accumulation in human obesity and type 2 diabetes is associated with increased rates of skeletal muscle fatty acid transport and increased sarcolemmal FAT/CD36. FASEB J. 2004, 18, 1144–1146. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.L. Arterial stiffness and hypertension. Clin. Hypertens. 2023, 29, 31. [Google Scholar] [CrossRef]
- Albalwi, A.A.; Alharbi, A.A. Optimal procedure and characteristics in using five times sit to stand test among older adults: A systematic review. Medicine 2023, 102, e34160. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta- analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Chun, H.; Kim, Y.-S.; Jung, H.-W.; Jang, I.-Y.; Cha, H.-M.; Son, K.Y.; Cho, B.; Kwon, I.S.; Yoon, J.L. Association between Timed Up and Go Test and subsequent functional dependency. J. Korean Med. Sci. 2020, 35, e25. [Google Scholar] [CrossRef] [PubMed]
| Variable | All (n = 116) | Non-MetS (n = 58) | MetS (n = 58) | p-Value |
|---|---|---|---|---|
| Demographic and anthropometrics | ||||
| Female sex, n (%) | 76 (65.5%) | 31 (53.4%) | 45 (77.6%) | 0.006 * |
| Age (years) | 68.46 ± 5.48 | 68.74 ± 5.52 | 68.17 ± 5.48 | 0.586 |
| BMI (kg/m2) | 22.49 ± 3.56 | 21.73 ± 3.70 | 23.25 ± 3.28 | 0.021 * |
| WC (cm) | 84.07 ± 9.11 | 82.09 ± 8.65 | 86.05 ± 9.20 | 0.018 * |
| GPAQ (MET-min/wk) | 1359.15 ± 1119.49 | 1411.76 ± 1434.44 | 1306.53 ± 682.07 | 0.594 |
| Cardiometabolic and clinical parameters | ||||
| SBP (mmHg) | 129.87 ± 17.04 | 123.71 ± 13.99 | 136.03 ± 17.68 | <0.001 * |
| DBP (mmHg) | 71.47 ± 9.17 | 70.10 ± 8.99 | 72.83 ± 9.22 | 0.110 |
| FBG (mg/dL) | 117.55 ± 28.65 | 105.55 ± 19.11 | 129.55 ± 31.58 | <0.001 * |
| HDL-C (mg/dL) | 44.79 ± 12.33 | 48.41 ± 13.68 | 41.17 ± 9.63 | 0.007 * |
| TG (mg/dL) | 150.47 ± 71.21 | 120.16 ± 57.56 | 180.79 ± 71.05 | <0.001 * |
| TG/HDL-C ratio | 3.60 ± 1.88 | 2.66 ± 1.55 | 4.55 ± 1.71 | <0.001 * |
| Functional and physiological performance † | ||||
| 6MWD (m) | 334.97 ± 60.28 | 364.44 ± 53.33 | 305.51 ± 52.15 | <0.001 * |
| FTSST (s) | 15.12 ± 1.96 | 14.48 ± 1.62 | 15.75 ± 2.08 | 0.005 * |
| TUG (s) | 13.15 ± 1.85 | 12.34 ± 1.64 | 13.96 ± 1.69 | <0.001 * |
| Handgrip strength (kg) | 21.89 ± 4.88 | 22.85 ± 5.17 | 20.93 ± 4.41 | 0.388 |
| Dyspnea (Borg 0–10) | 2.91 ± 1.58 | 2.54 ± 1.58 | 3.28 ± 1.50 | 0.017 * |
| Leg fatigue (Borg 0–10) | 2.21 ± 1.40 | 2.29 ± 1.43 | 2.13 ± 1.38 | 0.520 |
| Variables | rho (p-Value) | β Standardized (95% CI) | p-Value |
|---|---|---|---|
| Metabolic and Behavioral profile | |||
| WC (cm) | 0.20 (0.029) * | 0.059 (−0.102, 0.220) | 0.465 |
| HDL-C (mg/dL) | −0.01 (0.939) | −0.049 (−0.249, 0.151) | 0.625 |
| FBG (mg/dL) | 0.05 (0.622) | −0.036 (−0.214, 0.142) | 0.705 |
| Physiological responses (6MWT) | |||
| ΔSBP (mmHg) | −0.27 (0.004) * | −0.286 (−0.467, −0.105) | 0.003 * |
| ΔHR (bpm) | 0.09 (0.331) | 0.102 (−0.077, 0.281) | 0.261 |
| ΔSpO2 (%) | 0.17 (0.074) | 0.224 (0.037, 0.411) | 0.019 * |
| Functional capacity | |||
| 6MWD (m) | −0.49 (<0.001) ** | −0.382 (−0.556, −0.207) | <0.001 ** |
| Handgrip strength (kg) | −0.11 (0.244) | −0.038 (−0.063, −0.013) | <0.001 ** |
| FTSST (s) | 0.41 (<0.001) ** | 0.291 (0.122, 0.460) | 0.001 ** |
| TUG (s) | 0.47 (<0.001) ** | 0.316 (0.152, 0.480) | <0.001 ** |
| Perceptual responses | |||
| Dyspnea (Borg 0–10) | 0.17 (0.064) | 0.186 (−0.008, 0.380) | 0.060 |
| Leg fatigue (Borg 0–10) | −0.00 (0.981) | −0.015 (−0.187, 0.157) | 0.885 |
| Predictors | Model 1 β (95% CI) | Model 2 β (95% CI) | Model 3 β (95% CI) |
|---|---|---|---|
| Demographic and Anthropometric | |||
| Age (years) | −0.93 (−3.15, 1.30) | −2.11 (−4.25, 0.03)) | 0.98 (−0.56, 2.52) |
| Female (ref: male) | −27.88 (−50.64, −4.93) * | −18.39 (−40.02, 3.24) | 15.19 (−0.67, 31.05) |
| BMI (kg/m2) | −2.21 (−5.43, 1.02) | −0.37 (−3.46, 2.71) | −0.02 (−2.10, 2.07) |
| GPAQ (MET-min/wk) | 0.012 (0.0003, 0.023) * | 0.007 (−0.003, 0.018) | 0.01 (−0.00, 0.01) |
| Metabolic biomarkers | |||
| TG (mg/dL) | −0.33 (−0.47, −0.18) ** | −0.09 (−0.20, 0.03) | |
| HDL-C (mg/dL) | 0.02 (−0.79, 0.84) | 0.40 (−0.16, 0.96) | |
| FBG (mg/dL) | −0.34 (−0.71, 0.03) | −0.19 (−0.45, 0.06) | |
| Physiological and Functional (6MWT) | |||
| ΔSBP (mmHg) | 0.76 (0.20, 1.31) * | ||
| ΔHR (bpm) | 0.08 (−0.44, 0.60) | ||
| ΔSpO2 (%) | −0.01 (−5.46, 5.45) | ||
| FTSST (s) | −24.45 (−32.44, −16.45) ** | ||
| Adjusted R2 | 0.05 | 0.213 | 0.657 |
| ΔR2 | - | 0.138 | 0.423 |
| p-value | 0.035 * | <0.001 ** | <0.001 ** |
| Predictor | AUC (95% CI) | Optimal Cut-Off | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| TG (mg/dL) | 0.709 (0.611–0.808) | ≥143 | 70.70 | 68.00 |
| FTSST (s) | 0.956 (0.922–0.990) | ≥15.5 | 90.20 | 76.00 |
| TUG (s) | 0.925 (0.873–0.977) | ≥13.7 | 85.40 | 81.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Kloypan, C.; Promsrisuk, T.; Suwannakul, B.; Kaewjoho, C.; Srithawong, A. Associations Between Triglycerides and Walking Capacity in Community-Dwelling Older Adults with Metabolic Syndrome. Diseases 2026, 14, 18. https://doi.org/10.3390/diseases14010018
Kloypan C, Promsrisuk T, Suwannakul B, Kaewjoho C, Srithawong A. Associations Between Triglycerides and Walking Capacity in Community-Dwelling Older Adults with Metabolic Syndrome. Diseases. 2026; 14(1):18. https://doi.org/10.3390/diseases14010018
Chicago/Turabian StyleKloypan, Chiraphat, Tichanon Promsrisuk, Boonsita Suwannakul, Chonticha Kaewjoho, and Arunrat Srithawong. 2026. "Associations Between Triglycerides and Walking Capacity in Community-Dwelling Older Adults with Metabolic Syndrome" Diseases 14, no. 1: 18. https://doi.org/10.3390/diseases14010018
APA StyleKloypan, C., Promsrisuk, T., Suwannakul, B., Kaewjoho, C., & Srithawong, A. (2026). Associations Between Triglycerides and Walking Capacity in Community-Dwelling Older Adults with Metabolic Syndrome. Diseases, 14(1), 18. https://doi.org/10.3390/diseases14010018






