A Systems Thinking Approach to Designing Clinical Models and Healthcare Services
Abstract
:1. Introduction
1.1. The Changing Needs of Patients: From Treating Acute to Chronic Conditions
1.2. The Current Healthcare Delivery System and Challenges of Conventional Clinical Modeling
1.3. Paper Contribution—Systems Thinking Approach to Tackle Current Clinical Modeling Challenges
1.4. Paper Outline
2. Systems Thinking Approach to Modeling Healthcare Delivery
2.1. Domains Applying Systems Thinking to the Health Field
2.2. Systems Thinking for Healthcare Delivery
2.2.1. System Function
2.2.2. System Form
2.2.3. System Concept
3. Designing Clinical Models Using Systems Thinking and Systems Methodology: An Illustrative Example
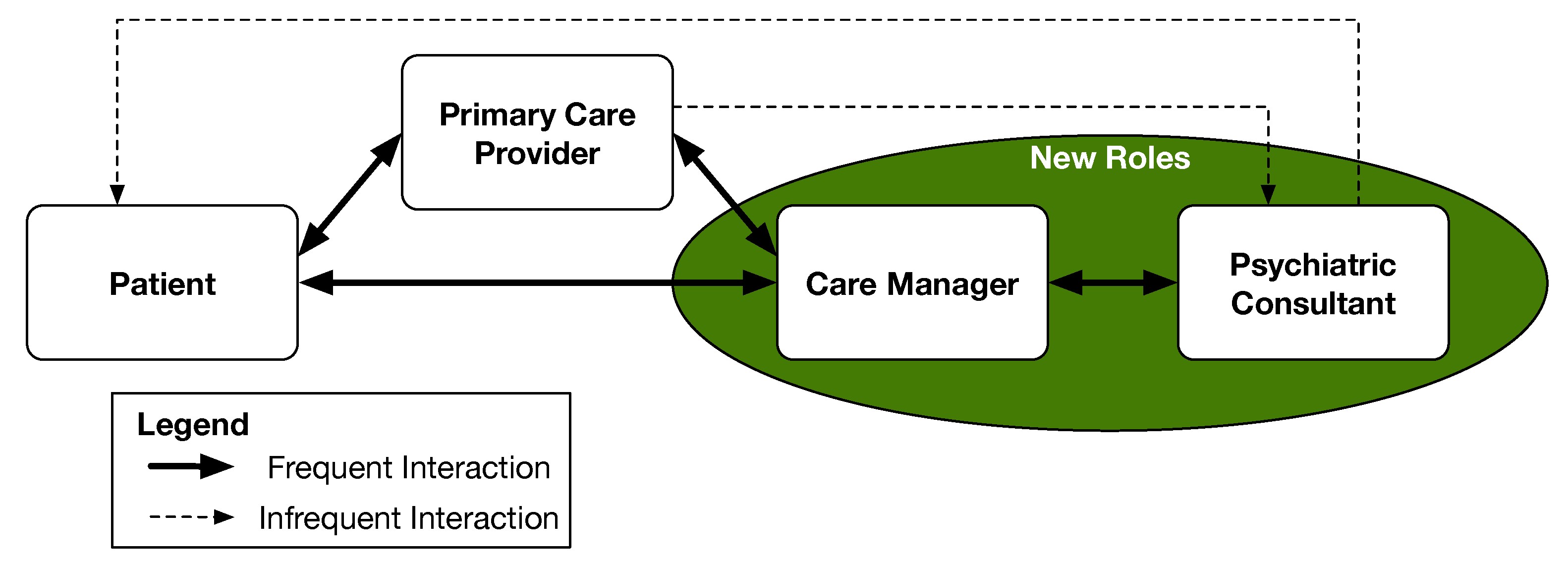
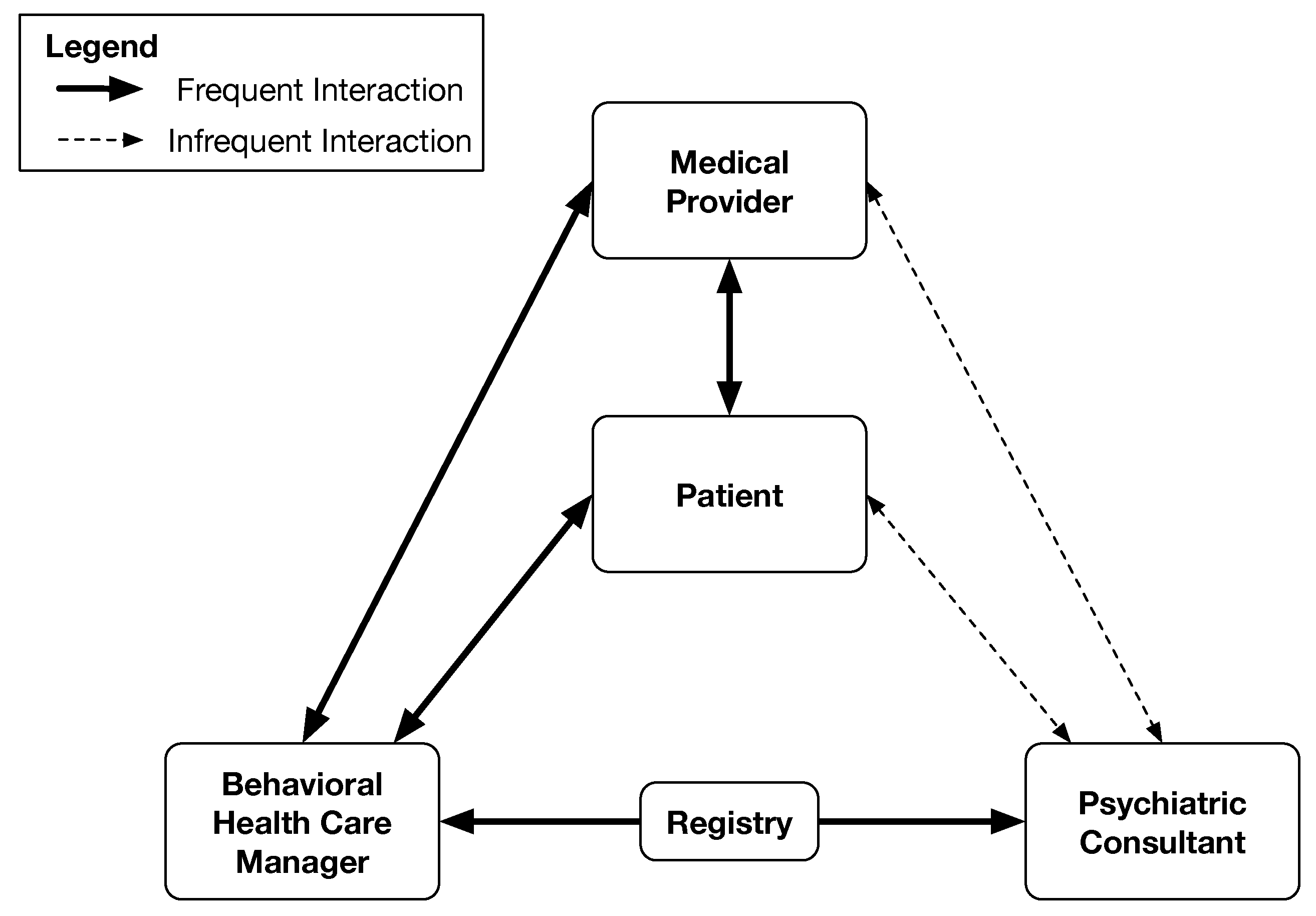
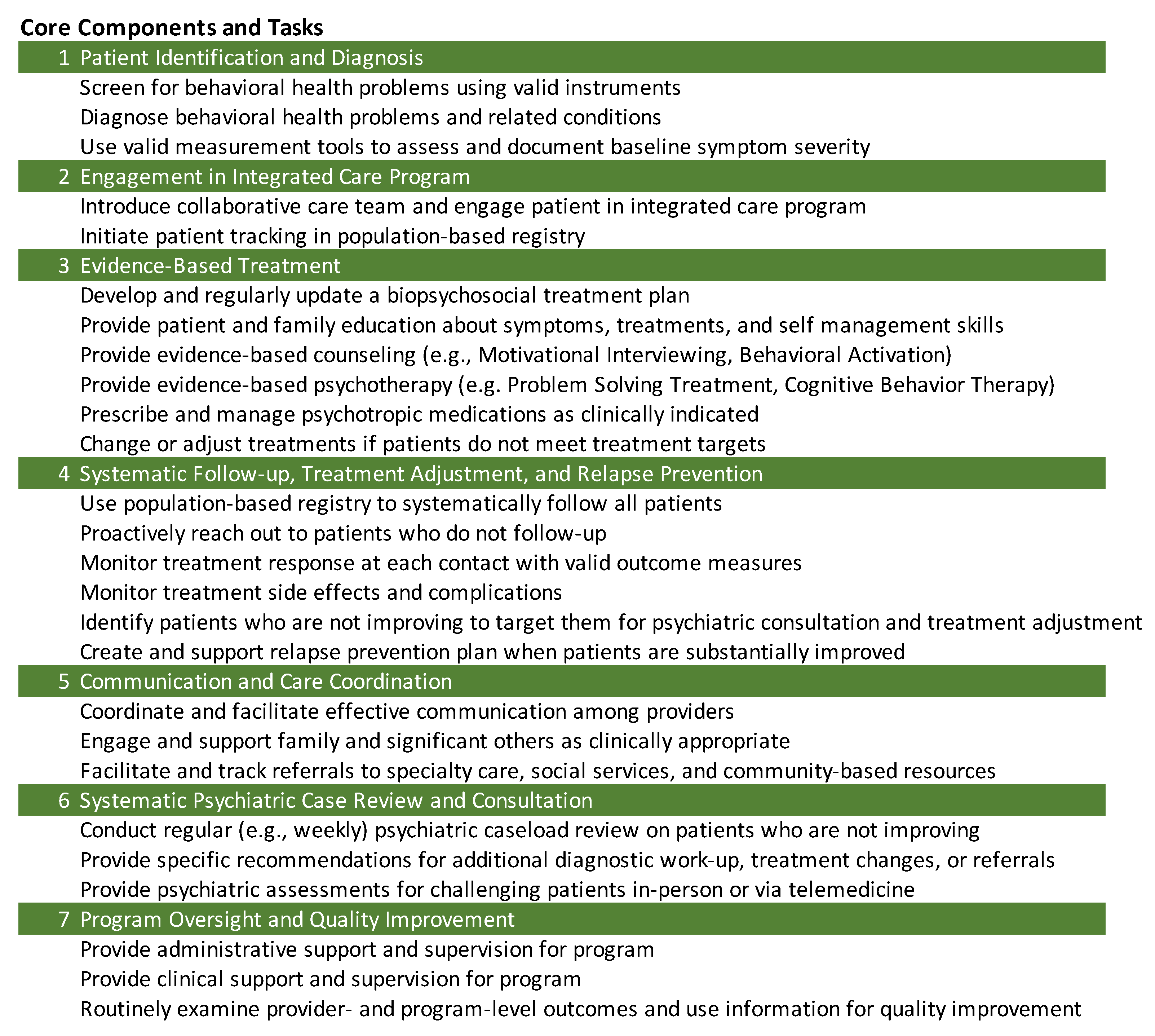
3.1. Clinical Model of Behavioral Health Integration into Primary Care
3.2. Methodology for Developing the System Model
3.3. Description of the System Model
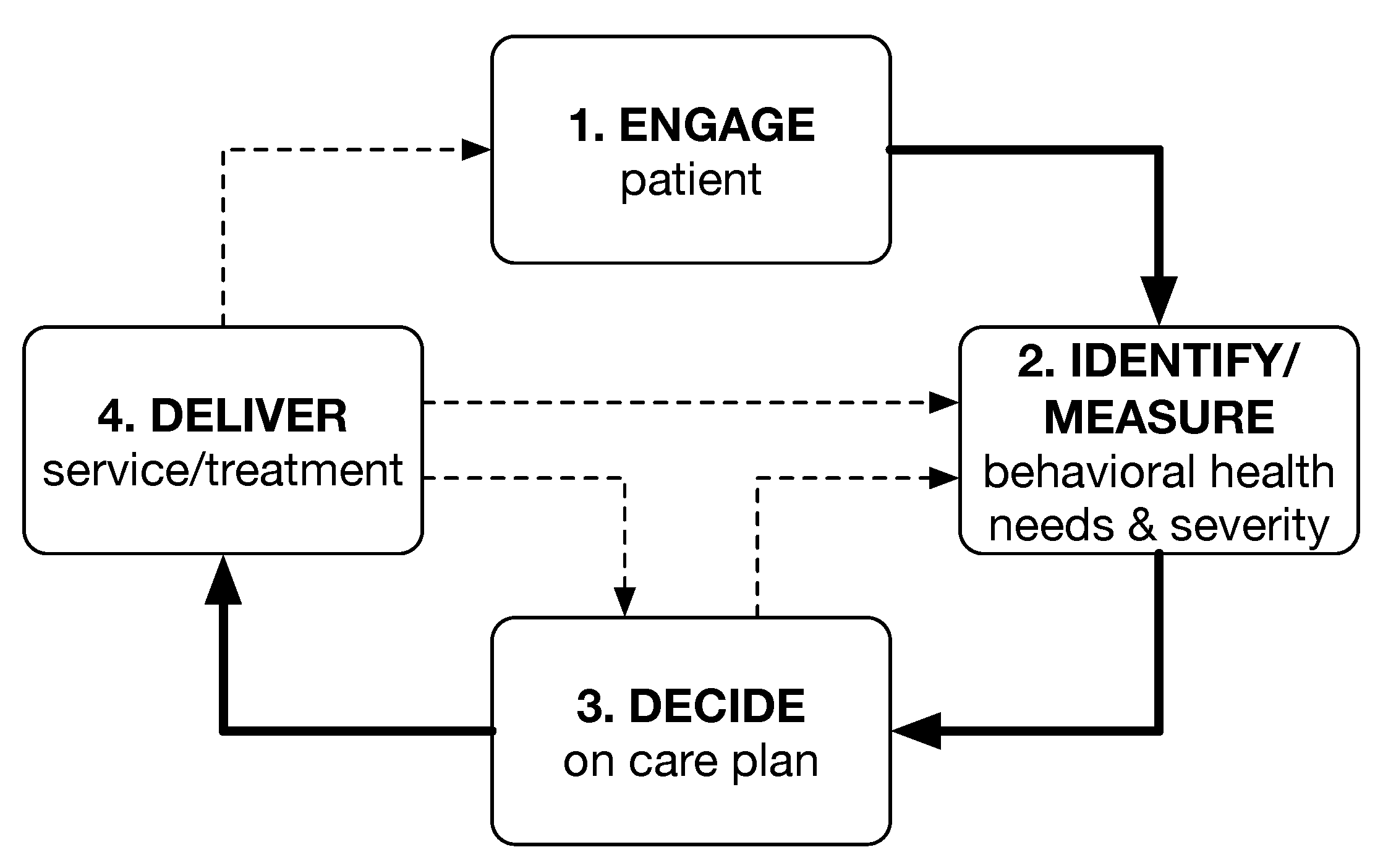
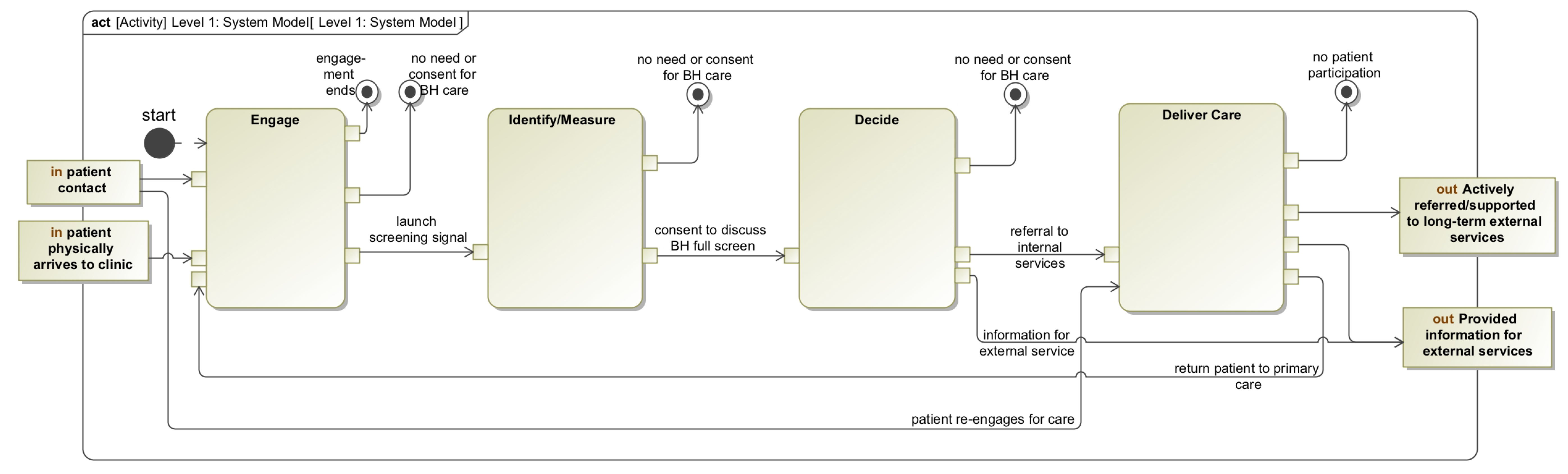
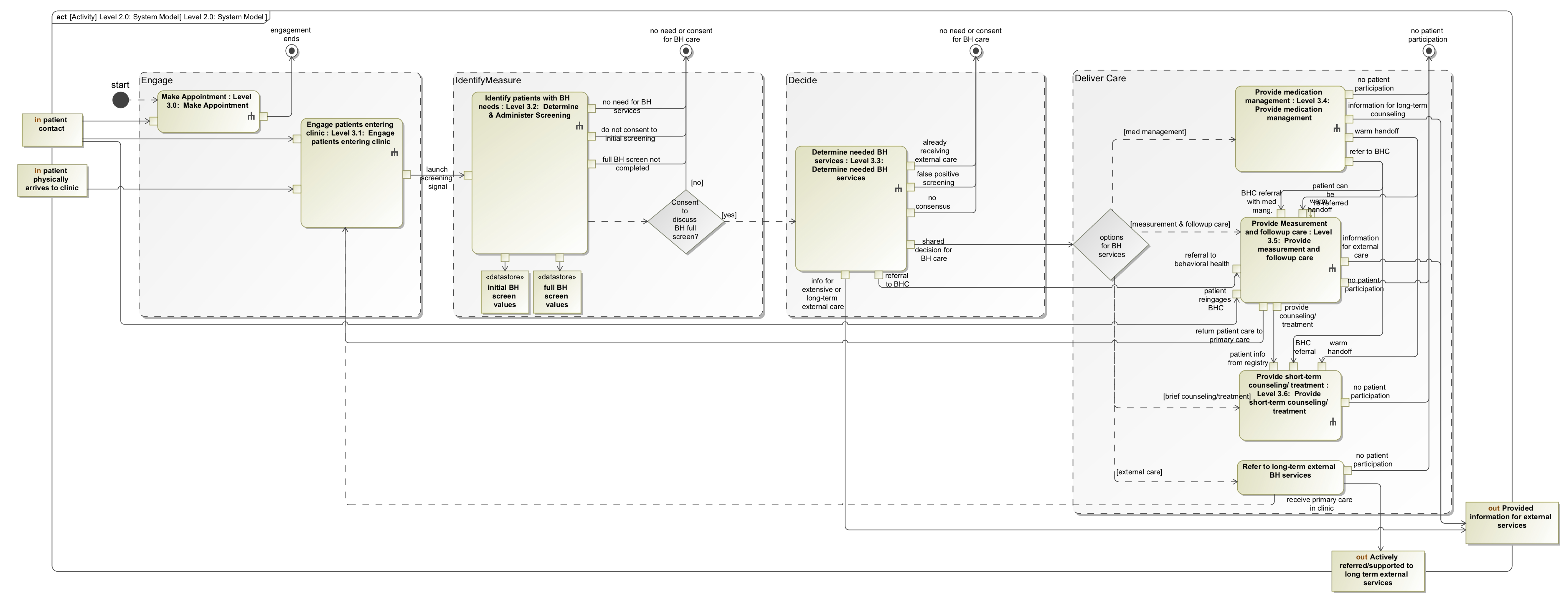
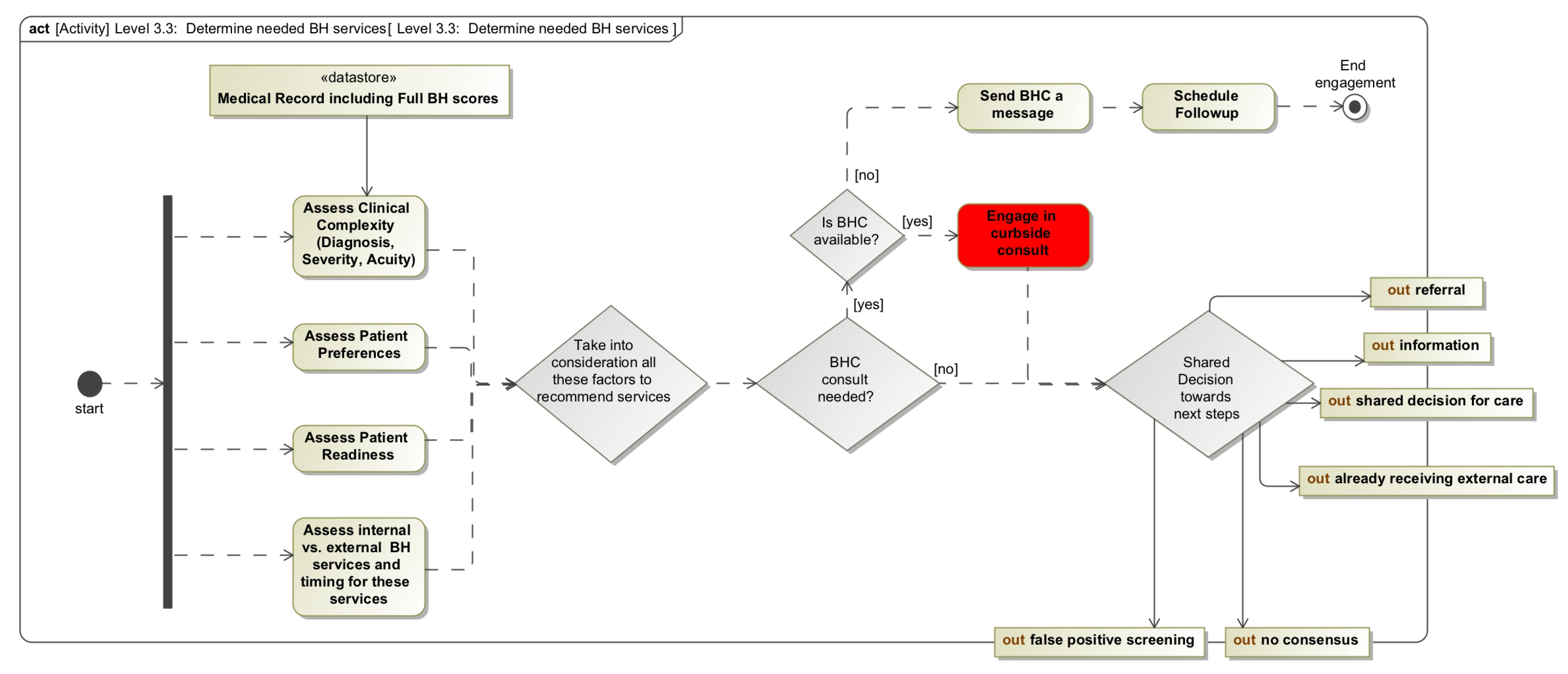
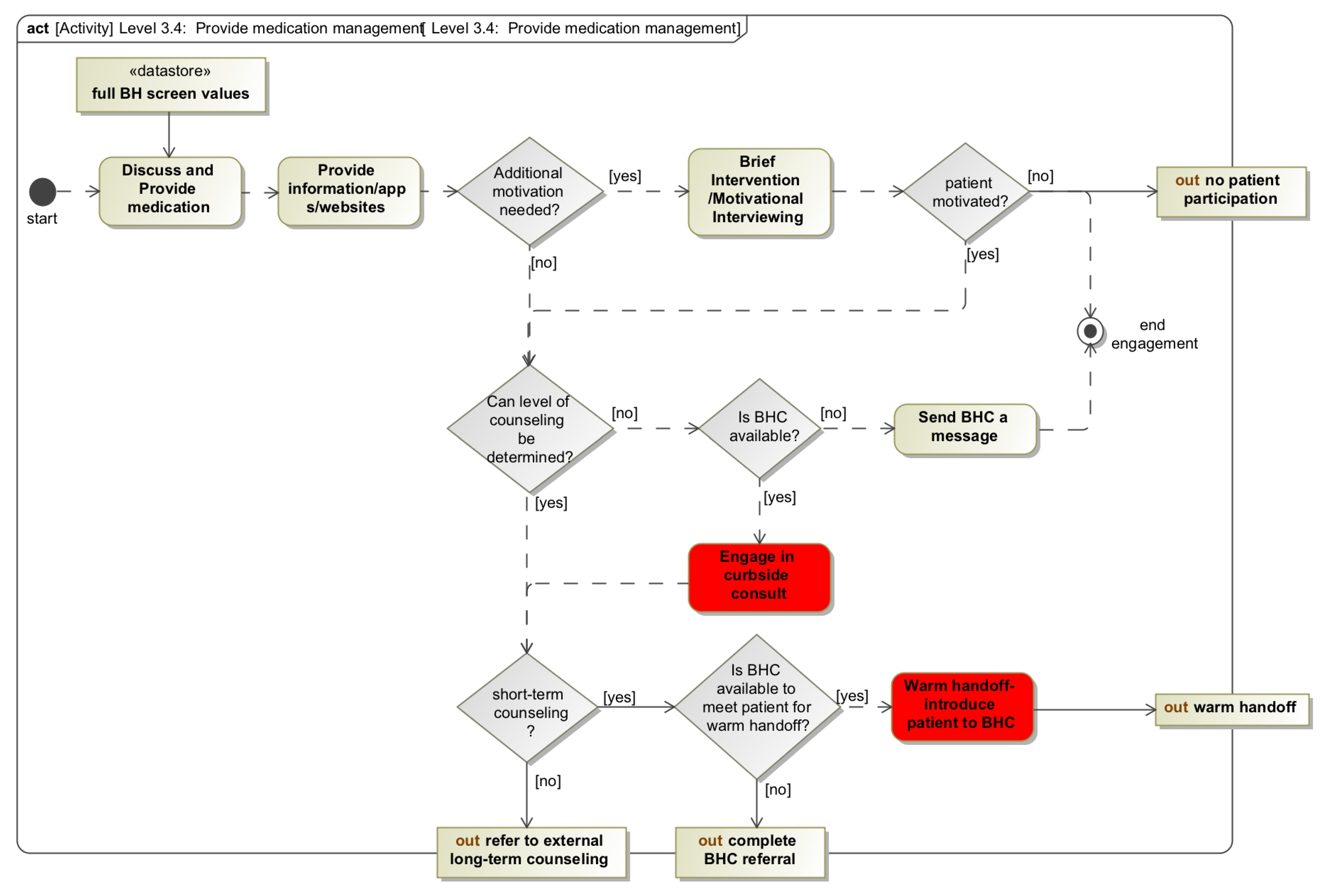
3.3.1. System Function
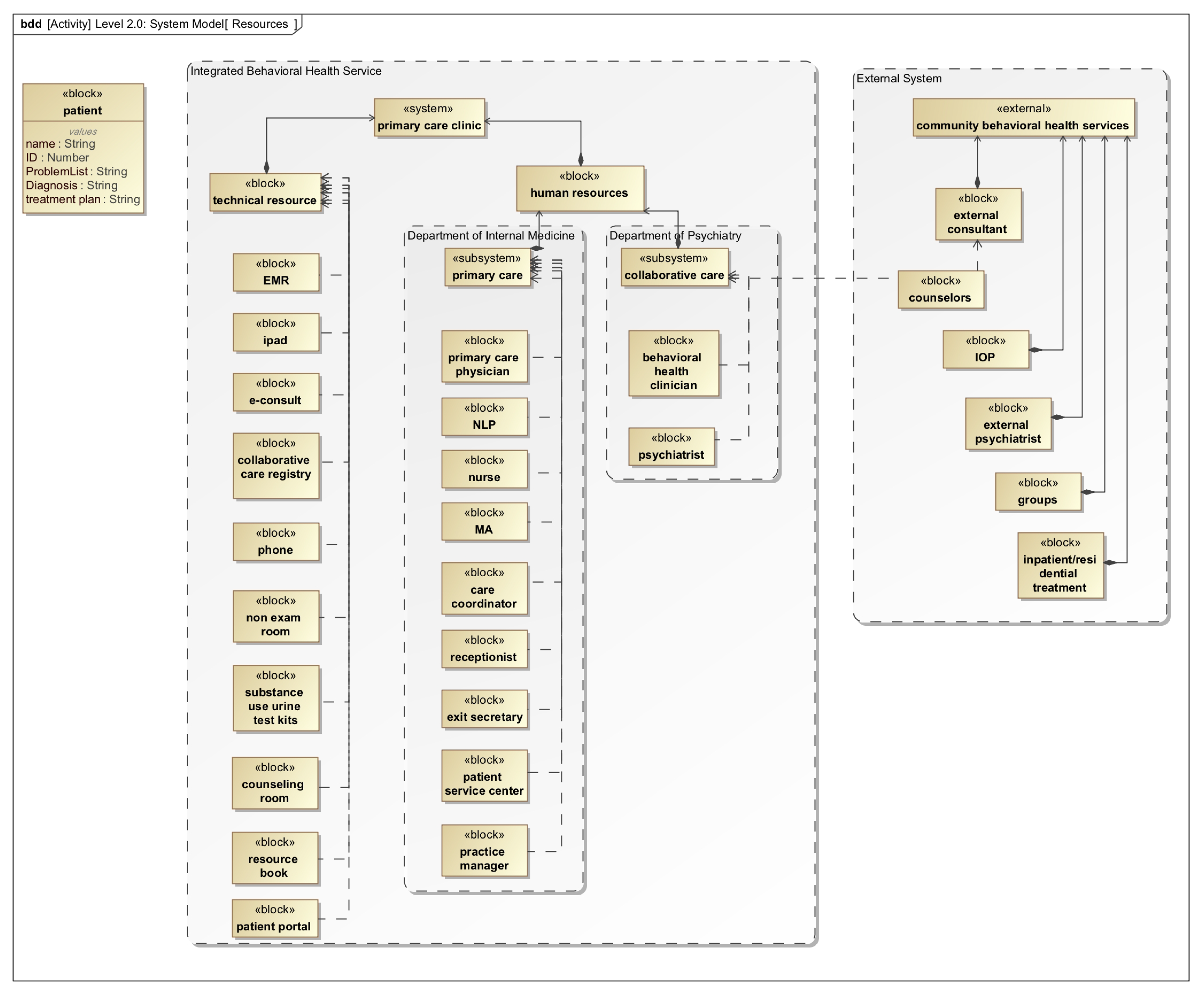
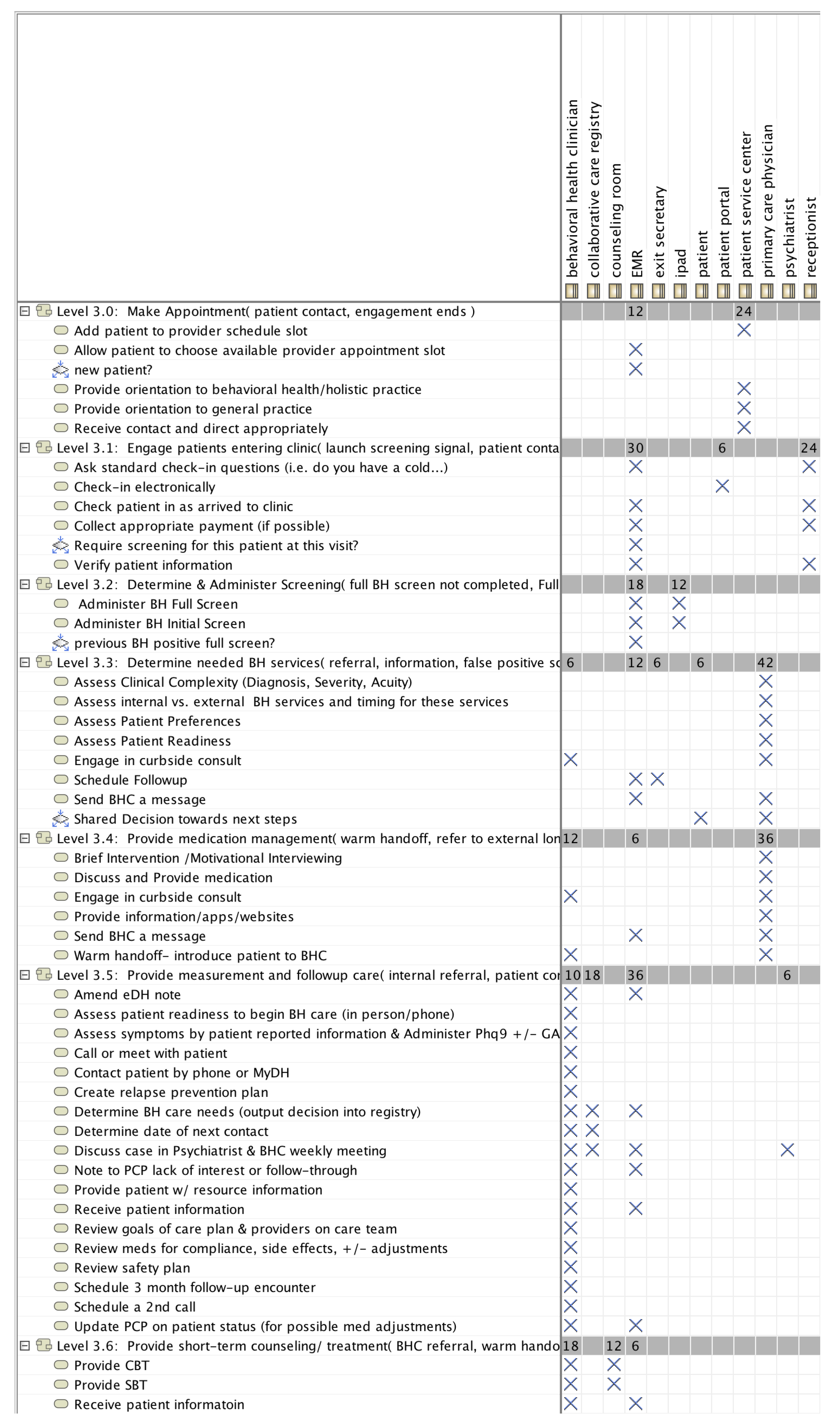
3.3.2. System Form
3.3.3. System Concept
4. Discussion
4.1. Potential Advantages of Systems Thinking Based Modeling
4.2. Limitations of a Systems Thinking Approach in Healthcare Delivery
5. Conclusions and Future Directions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| MD | Medicine Doctor (Doctor of Medicine) |
| BH | Behavioral Health |
References
- Levit, K.; Smith, C.; Cowan, C.; Lazenby, H.; Sensenig, A.; Catlin, A. Trends in US health care spending, 2001. Health Aff. 2003, 22, 154–164. [Google Scholar] [CrossRef]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America; The National Academies Press: Washington, DC, USA, 2013. [Google Scholar]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G. Chronic Conditions: Making the Case for Ongoing Care; Technical Report; Robert Wood Johnson Foundation: Baltimore, MD, USA, 2004. [Google Scholar]
- Stanton, M.W.; Rutherford, M. The High Concentration of US Health Care Expenditures; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2006. [Google Scholar]
- Gerteis, J.; Izrael, D.; Deitz, D.; LeRoy, L.; Ricciardi, R.; Miller, T.; Basu, J. Multiple Chronic Conditions Chartbook; AHRQ Publications No, Q14-0038; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2014. [Google Scholar]
- Warshaw, G. Introduction: Advances and challenges in care of older people with chronic illness. Generations 2006, 30, 5–10. [Google Scholar]
- Friedman, B.; Jiang, H.J.; Elixhauser, A. Costly hospital readmissions and complex chronic illness. Inq. J. Health Care Organ. Provis. Financ. 2008, 45, 408–421. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. Multiple Chronic Conditions: A Strategic Framework–Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions; US Department of Health and Human Services: Washington, DC, USA, 2010.
- Anderson, G.F. ChRonic Care: Making the Case for Ongoing Care; Robert Wood Johnson Foundation: Baltimore, MD, USA, 2010. [Google Scholar]
- Ahn, A.C.; Tewari, M.; Poon, C.S.; Phillips, R.S. The limits of reductionism in medicine: Could systems biology offer an alternative? PLoS Med. 2006, 3, 709–713. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, D.; Ryan, J.; Klein, S. Models of care for high-need, high-cost patients: An evidence synthesis. Issue Brief (Commonw Fund) 2015, 31, 1–19. [Google Scholar] [PubMed]
- Milstein, A.; Gilbertson, E. American medical home runs. Health Aff. 2009, 28, 1317–1326. [Google Scholar] [CrossRef] [PubMed]
- Khayal, I.; Farid, A. Architecting a System Model for Personalized Healthcare Delivery and Managed Individual Health Outcomes. Complexity 2018, 2018, 8457231. [Google Scholar] [CrossRef]
- Khayal, I.; Farid, A. An Architecture for a Cyber-Physical Healthcare Delivery System with Human Agents. In Proceedings of the 2017 IEEE International Summer School on Smart Cities (IEEE S3C), Natal, Brazil, 6–11 August 2017. [Google Scholar]
- Weiner, J.P. Expanding the US medical workforce: Global perspectives and parallels. BMJ Br. Med. J. 2007, 335, 236–238. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality AHRQ Publishing and Communications Guidelines Section 6: Toolkit Guidance. Available online: http://www.ahrq.gov/research/publications/pubcomguide/index.html (accessed on 24 March 2019).
- Hauk, O.; Davis, M.H.; Ford, M.; Pulvermüller, F.; Marslen-Wilson, W.D. The time course of visual word recognition as revealed by linear regression analysis of ERP data. Neuroimage 2006, 30, 1383–1400. [Google Scholar] [CrossRef]
- Potter, M.C.; Wyble, B.; Hagmann, C.E.; McCourt, E.S. Detecting meaning in RSVP at 13 ms per picture. Atten. Percept. Psychophys. 2014, 76, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Rouse, W.B.; Cortese, D.A. (Eds.) Engineering the System of Healthcare Delivery; Chapter Engineering Healthcare as a Service System; IOS Press: Amsterdam, The Netherlands, 2010; Volume 153. [Google Scholar]
- Croskerry, P. Achieving quality in clinical decision making: Cognitive strategies and detection of bias. Acad. Emerg. Med. 2002, 9, 1184–1204. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, B.H.; Emler, A.C. Rationality in medical decision making: A review of the literature on doctors’ decision-making biases. J. Eval. Clin. Pract. 2001, 7, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Edwards, A.; Elwyn, G. Shared Decision-Making in Health Care: Achieving Evidence-Based Patient Choice; Oxford University Press: New York, NY, USA, 2009. [Google Scholar]
- Nelson, E.C.; Landgraf, J.M.; Hays, R.D.; Wasson, J.H.; Kirk, J.W. The functional status of patients: How can it be measured in physicians’ offices? Med. Care 1990, 28, 1111–1126. [Google Scholar] [CrossRef]
- Khayal, I.S.; Farid, A.M. The Need for Systems Tools in the Practice of Clinical Medicine. Syst. Eng. 2017, 20, 3–20. [Google Scholar] [CrossRef]
- Kitano, H. Systems Biology: A Brief Overview. Science 2002, 295, 1662–1664. [Google Scholar] [CrossRef]
- Ideker, T.; Galitski, T.; Hood, L. A New Approach to Decoding Life: Systems Biology. Annu. Rev. Genom. Hum. Genet. 2001, 2, 343–372. [Google Scholar] [CrossRef]
- Hood, L. Systems biology: Integrating technology, biology, and computation. Mech. Ageing Dev. 2003, 124, 9–16. [Google Scholar] [CrossRef]
- Westerhoff, H.V.; Palsson, B.O. The evolution of molecular biology into systems biology. Nat. Biotechnol. 2004, 22, 1249–1252. [Google Scholar] [CrossRef]
- O’Malley, M.a.; Dupré, J. Fundamental issues in systems biology. BioEssays 2005, 27, 1270–1276. [Google Scholar] [CrossRef]
- Boogerd, F.; Bruggeman, F.J.; Hofmeyr, J.H.S.; Westerhoff, H.V. Systems Biology: Philosophical Foundations; Elsevier: Oxford, UK, 2007. [Google Scholar]
- Bruggeman, F.J.; Westerhoff, H.V. The nature of systems biology. Trends Microbiol. 2007, 15, 45–50. [Google Scholar] [CrossRef]
- Gatherer, D. So what do we really mean when we say that systems biology is holistic? BMC Syst. Biol. 2010, 4, 22. [Google Scholar] [CrossRef]
- De Backer, P.; de Waele, D.; van Speybroeck, L. Ins and outs of systems biology vis-a-vis molecular biology: Continuation or clear cut? Acta Biotheor. 2010, 58, 15–49. [Google Scholar] [CrossRef] [PubMed]
- Bizzarri, M.; Cucina, A.; Palombo, A. The Conceptual Foundations of Systems Biology: An Introduction. In Systems Biology—Theory, Techniques and Applications; Nova Science Publishers, Inc.: New York, NY, USA, 2014; pp. 1–18. [Google Scholar]
- Palsson, B.O. Systems Biology: Properties of Reconstructed Networks; Cambridge University Press: New York, NY, USA, 2015. [Google Scholar]
- Dekkers, R. Chapter 10 Applications of System Theories. In Applied Systems Theory; Springer International Publishing: Cham, Switzerland, 2015; pp. 221–247. [Google Scholar]
- Brandeau, M.L.; Sainfort, F.; Pierskalla, W.P. Operations Research and Health Care: A Handbook of Methods and Applications; Springer: Norwell, MA, USA, 2004. [Google Scholar]
- Ahmadi-Javid, A.; Jalali, Z.; Klassen, K.J. Outpatient appointment systems in healthcare: A review of optimization studies. Eur. J. Oper. Res. 2017, 258, 3–34. [Google Scholar] [CrossRef]
- Turkcan, A.; Zeng, B.; Lawley, M. Chemotherapy operations planning and scheduling. IIE Trans. Healthc. Syst. Eng. 2012, 2, 31–49. [Google Scholar] [CrossRef]
- Huang, Y.L.; Hancock, W.M.; Herrin, G.D. An alternative outpatient scheduling system: Improving the outpatient experience. IIE Trans. Healthc. Syst. Eng. 2012, 2, 97–111. [Google Scholar] [CrossRef]
- Pérez, E.; Ntaimo, L.; Malavé, C.O.; Bailey, C.; McCormack, P. Stochastic online appointment scheduling of multi-step sequential procedures in nuclear medicine. Health Care Manag. Sci. 2013, 16, 281–299. [Google Scholar] [CrossRef] [PubMed]
- Sir, M.Y.; Dundar, B.; Steege, L.M.B.; Pasupathy, K.S. Nurse–patient assignment models considering patient acuity metrics and nurses’ perceived workload. J. Biomed. Inform. 2015, 55, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Borgman, N.J.; Vliegen, I.M.; Boucherie, R.J.; Hans, E.W. Appointment scheduling with unscheduled arrivals and reprioritization. Flex. Serv. Manuf. J. 2018, 30, 30–53. [Google Scholar] [CrossRef]
- Alvarado, M.M.; Ntaimo, L.; Banerjee, A.; Kianfar, K. Reducing pediatric medication errors: A survey and taxonomy. IIE Trans. Healthc. Syst. Eng. 2012, 2, 142–155. [Google Scholar] [CrossRef]
- Marmor, Y.N.; Golany, B.; Israelit, S.; Mandelbaum, A. Designing patient flow in emergency departments. IIE Trans. Healthc. Syst. Eng. 2012, 2, 233–247. [Google Scholar] [CrossRef]
- Peck, J.S.; Benneyan, J.C.; Nightingale, D.J.; Gaehde, S.A. Characterizing the value of predictive analytics in facilitating hospital patient flow. IIE Trans. Healthc. Syst. Eng. 2014, 4, 135–143. [Google Scholar] [CrossRef]
- Kaner, M.; Gadrich, T.; Dror, S.; Marmor, Y.N. Generating and evaluating simulation scenarios to improve emergency department operations. IIE Trans. Healthc. Syst. Eng. 2014, 4, 156–166. [Google Scholar] [CrossRef]
- Rivera, A.J.; Karsh, B.T. Human factors and systems engineering approach to patient safety for radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, S174–S177. [Google Scholar] [CrossRef] [PubMed]
- Sterman, J.D. Business Dynamics: Systems Thinking and Modeling for a Complex World; Irwin/McGraw-Hill: Boston, MA, USA, 2000; Volume 19. [Google Scholar]
- Newman, M. Networks: An Introduction; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Helbing, D. Agent-based modeling. In Social Self-Organization; Springer: Berlin/Heidelberg, Germany, 2012; pp. 25–70. [Google Scholar]
- Buckingham, J.L.; Donatelle, E.P.; Thomas Jr, A.; Scherger, J.E. Family Medicine: Principles and Practice; Springer: New York, NY, USA, 2013. [Google Scholar]
- De Weck, O.L.; Roos, D.; Magee, C.L. Engineering Systems: Meeting Human Needs in a Complex Technological World; MIT Press: Cambridge, MA, USA, 2011; p. xvi. 213p. [Google Scholar]
- Farid, A.M. Reconfigurability Measurement in Automated Manufacturing Systems. Ph.D. Thesis, University of Cambridge, Cambridge, UK, 2007. [Google Scholar]
- Farid, A.M.; McFarlane, D.C. Production degrees of freedom as manufacturing system reconfiguration potential measures. Proc. Inst. Mech. Eng. Part B J. Eng. Manuf. 2008, 222, 1301–1314. [Google Scholar] [CrossRef]
- Farid, A.M. Product Degrees of Freedom as Manufacturing System Reconfiguration Potential Measures. Int. Trans. Syst. Sci. Appl. 2008, 4, 227–242. [Google Scholar]
- Farid, A.M. Static Resilience of Large Flexible Engineering Systems: Axiomatic Design Model and Measures. IEEE Syst. J. 2017, 11, 2006–2017. [Google Scholar] [CrossRef]
- Farid, A.M. An Axiomatic Design Approach to Non-Assembled Production Path Enumeration in Reconfigurable Manufacturing Systems. In Proceedings of the 2013 IEEE International Conference on Systems Man and Cybernetics, Manchester, UK, 13–16 October 2013; Volume 1, pp. 1–8. [Google Scholar]
- Farid, A.M.; Ribeiro, L. An Axiomatic Design of a Multi-Agent Reconfigurable Mechatronic System Architecture. IEEE Trans. Ind. Inform. 2015, 11, 1142–1155. [Google Scholar] [CrossRef]
- Schoonenberg, W.C.; Farid, A.M. A Dynamic Energy Management Model for Microgrid-Enabled Production Systems. J. Clean. Prod. 2017, 164, 816–830. [Google Scholar] [CrossRef]
- Davis, M.; Balasubramanian, B.A.; Waller, E.; Miller, B.F.; Green, L.A.; Cohen, D.J. Integrating behavioral and physical health care in the real world: early lessons from advancing care together. J. Am. Board Fam. Med. 2013, 26, 588–602. [Google Scholar] [CrossRef]
- Peek, C.; Council, N. Lexicon for Behavioral Health and Primary Care Integration: Concepts and Definitions Developed by Expert Consensus (AHRQ Publication No. 13-IP001-EF); Technical Report; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2013. [Google Scholar]
- Daniels, A.; England, M.J.; Page, A.K.; Corrigan, J. Crossing the quality chasm: Adaptation for mental health and addictive disorders. Int. J. Ment. Health 2005, 34, 5–9. [Google Scholar] [CrossRef]
- Van Lerberghe, W. The World Health Report 2008: Primary Health Care: Now More Than Ever; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Agency for Healthcare Research and Quality. The Academy: Integrating Behavioral Health and Primary Care. Available online: http://integrationacademy.ahrq.gov (accessed on 2 February 2018).
- Substance Abuse and Mental Health Services Administration. Health Care and Health Systems Integration. Available online: www.samhsa.gov/health-care-health-systems-integration (accessed on 2 February 2018).
- Stewart, J.C.; Perkins, A.J.; Callahan, C.M. Effect of collaborative care for depression on risk of cardiovascular events: Data from the IMPACT randomized controlled trial. Psychosom. Med. 2014, 76, 29. [Google Scholar] [CrossRef] [PubMed]
- University of Washington AIMS Center. Team Structure. Available online: https://aims.uw.edu/collaborative-care/team-structure (accessed on 2 February 2018).
- Brackett, C. Behavioral Health Integration into Adult Primary Care Model Guideline. Available online: http://med.dartmouth-hitchcock.org/documents/behavioral-health-integration-guideline.pdf (accessed on 2 February 2018).
- University of Washington AIMS Center. Stepped Model of Integrated Behavioral Health Care. Available online: https://aims.uw.edu/stepped-model-integrated-behavioral-health-care (accessed on 2 February 2018).
- University of Washington AIMS Center. Collaborative Care: A Step-by-Step Guide to Implementing the Core Model. Available online: https://aims.uw.edu/sites/default/files/CollaborativeCareImplementationGuide.pdf (accessed on 2 February 2018).
- University of Washington AIMS Center. Collaborative Care: Principles and Tasks Checklist. Available online: http://uwaims.org/files/AIMS_Principles_Checklist_final.pdf (accessed on 2 February 2018).
- Crowley, R.A.; Kirschner, N. The integration of care for mental health, substance abuse, and other behavioral health conditions into primary care: Executive summary of an American College of Physicians position paper. Ann. Intern. Med. 2015, 163, 298–299. [Google Scholar] [CrossRef] [PubMed]
- Farid, A.M. An Engineering Systems Introduction to Axiomatic Design. In Axiomatic Design in Large Systems: Complex Products, Buildings and Manufacturing Systems; Farid, A.M., Suh, N.P., Eds.; Springer: Berlin/Heidelberg, Germany, 2016; Chapter 1; pp. 1–47. [Google Scholar]
- Von Bertalanffy, L. General System Theory: Foundations, Development, Applications; George Braziller: New York, NY, USA, 1968; Volume 55. [Google Scholar]
- Buede, D.M. The Engineering Design of Systems: Models and Methods, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2009; Volume 55, 516p. [Google Scholar]
- Wiley. INCOSE Systems Engineering Handbook: A Guide for System Life Cycle Processes and Activities; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Friedenthal, S.; Moore, A.; Steiner, R. A Practical Guide to SysML: The Systems Modeling Language, 2nd ed.; Morgan Kaufmann: Waltham, MA, USA, 2011; p. 640. [Google Scholar]
- Weilkiens, T. Systems Engineering With SysML/UML Modeling, Analysis, Design; Morgan Kaufmann: Burlington, MA, USA, 2011. [Google Scholar]
- Walden, D.D.; Roedler, G.J.; Forsberg, K.; Hamelin, R.D.; Shortell, T.M.; SE Handbook Working Group. Systems Engineering Handbook: A Guide for System Life Cycle Processes and Activities; International Council on Systems Engineering (INCOSE): San Diego, CA, USA, 2015; pp. 1–386. [Google Scholar]
- Wymore, A.W. Model-Based Systems Engineering; CRC Press: Boca Raton, FL, USA, 1993; Volume 3. [Google Scholar]
- Waldman, S.A.; Terzic, A. Clinical and Translational Science: From Bench-Bedside to Global Village. Clin. Transl. Sci. 2010, 3, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Zerhouni, E.A. Translational and Clinical Science—Time for a New Vision. N. Engl. J. Med. 2005, 353, 1621–1623. [Google Scholar] [CrossRef]
- Leischow, S.J.; Best, A.; Trochim, W.M.; Clark, P.I.; Gallagher, R.S.; Marcus, S.E.; Matthews, E. Systems Thinking to Improve the Public’s Health. Am. J. Prev. Med. 2008, 35, S196–S203. [Google Scholar] [CrossRef]
- West, G.B. The importance of quantitative systemic thinking in medicine. Lancet 2012, 379, 1551–1559. [Google Scholar] [CrossRef]
- President’s Council of Advisors on Science and Technology (PCAST). Report to the President, Better Health Care and Lower Costs: Accelerating Improvement Through Systems Engineering; Executive Office of the President, President’s Council of Advisors on Science and Technology: Washington, DC, USA, 2014. [Google Scholar]
- Reid, P.P.; Compton, W.D.; Grossman, J.H.; Fanjiang, G.; Proctor, P.; Compton, W.D.; Grossman, J.H.; Fanjiang, G. Building a Better Delivery System: A New Engineering/Health Care Partnership; National Academies Press: Washington, DC, USA, 2005; p. 276. [Google Scholar]
| Challenge 1: Designed based on single-diagnosis. Generally, not applicable to patients with multiple conditions, |
| Challenge 2: Described at a high-level of abstraction with a focus on human personnel, |
| Challenge 3: Described using text-based toolkits with minimal visuals, |
| Challenge 4: Described with expected paths; qualitatively describes the system and may be biased, and |
| Challenge 5: Described with minimal to no specificity of implementation-level details. |
| Advantage 1: Designed based on specified needs rather than a specific diagnosis, |
| Advantage 2: Described at multiple levels and scales, |
| Advantage 3: Described visually, |
| Advantage 4: Described with comprehensive paths; consequently, quantitatively describing the system, and |
| Advantage 5: Described in multi-level detail, providing a detailed multi-level implementation description. |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khayal, I.S. A Systems Thinking Approach to Designing Clinical Models and Healthcare Services. Systems 2019, 7, 18. https://doi.org/10.3390/systems7010018
Khayal IS. A Systems Thinking Approach to Designing Clinical Models and Healthcare Services. Systems. 2019; 7(1):18. https://doi.org/10.3390/systems7010018
Chicago/Turabian StyleKhayal, Inas S. 2019. "A Systems Thinking Approach to Designing Clinical Models and Healthcare Services" Systems 7, no. 1: 18. https://doi.org/10.3390/systems7010018
APA StyleKhayal, I. S. (2019). A Systems Thinking Approach to Designing Clinical Models and Healthcare Services. Systems, 7(1), 18. https://doi.org/10.3390/systems7010018





