Abstract
This study combines innovation resistance theory, the stimulus–organism–response (SOR) framework, and the job demands–resources model to facilitate an in-depth exploration of the barriers faced by healthcare professionals and the psychological responses they exhibit when adopting AI-supported healthcare technologies. We conducted a questionnaire survey and obtained 296 valid responses from healthcare professionals to examine the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. Using the SOR framework as a basis, this study validated a serial mediation model with moderating effects, demonstrating that resistance to AI-supported healthcare technologies influenced AI adoption behavioral intentions through job resource, job demand, and levels of employee engagement. Further, this study sought to validate the relationship between age-moderated job resource and job demand in employees exhibiting resistance to AI-supported healthcare technologies and their associated AI adoption behavioral intentions. The results indicated that job resources, job demands, and employee engagement serially mediated the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. Additionally, age only exhibited significant moderating effects on the relationship between job demands in resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. The findings of this study can aid in promoting the adoption of AI-supported healthcare technologies by healthcare professionals, generating new insights and broadening the scope and vision of existing literature.
1. Introduction
We live in an era of rapid digital transformation, where technology, in its simplest form, aims to drive industry impact and improve work performance [1,2]. Technological advancements over the past few decades have influenced the work and work styles of humans in various ways [3]. Technology has evolved, enabling industrial sectors to transition into Industry 4.0 through artificial intelligence (AI) technologies [4]. In addition, consumers increasingly use smart products such as smartwatches and smart home appliances [5] to enhance both their lifestyles and workstyles. In recent years, the integration of AI into healthcare has become a key focus of innovation and research efforts, driven by rapid technological advances and the urgent need to improve healthcare delivery systems.
The outbreak of the COVID-19 pandemic at the end of 2019 further highlighted the transformative potential of AI, along with the significant challenges associated with its adoption. During the pandemic, AI was applied in various contexts, including predicting virus transmission, accelerating vaccine development, and optimizing medical resources [6]. These applications demonstrate the ability of AI to effectively assist in managing large-scale public health crises. In the healthcare industry, AI can similarly be used to enhance patient diagnosis, improve disease prevention and treatment, increase cost efficiency, and provide universal access to treatment [7]. In addition to enabling machines to provide manual support, AI has also enabled humans to replace manual labor across various industries using superior cognitive abilities and intellectual capacity [8,9]. It is hoped that AI and healthcare can integrate together into the healthcare interface [10]. While AI has the potential to solve many problems, it has not flourished and become widespread to the extent initially expected. Webster (2020) [11] notes that many in the healthcare industry remain wary of AI-supported healthcare innovations, despite the occurrence of the COVID-19 pandemic and AI’s clear benefits during that time.
In fact, digital innovations across most industries face resistance to acceptance or adoption from both public and private users [5], with this resistance posing a significant threat to the digital transformation of the healthcare industry. Scholars have previously noted that the reasons consumers do not adopt AI include a lack of incentives for adoption along with consumer resistance behaviors [12]. While past research has focused on the benefits of AI-supported healthcare technologies, such as automated decision-making [13], process streamlining [14], and performance enhancement [15], less attention has been given to the barriers to achieving digital health innovation [16,17] and the resistance of healthcare professionals to the adoption of digital innovations in the healthcare industry [18]. This is the first motivation for this study, which is based on the theoretical foundation of the innovation resistance theory (IRT).
In the past, most studies on users’ behavioral intentions have relied on the diffusion of innovations theory, the technology acceptance model, and social exchange theory to conduct empirical research. Chong et al. (2022) [19] argue that user behavior is primarily influenced by the experience of using a particular technology. However, this study contends that the IRT alone is insufficient for exploring resistance to AI-supported healthcare technologies. This is because most of the components of IRT focus on resistance factors and fail to address the usage behavior and behavioral intentions of service users adopting the new technologies. Therefore, to better understand resistance to the adoption of AI-supported healthcare technologies, this study argues that using the stimulus–organism–response (SOR) framework [20] can provide a more comprehensive approach for guiding model construction and empirical testing. The SOR model helps to explain the cognitive and emotional processes behind resistance to innovations before the eventual adoption of a behavior or response, wherein intrinsic processes intervene in the stimulus to affect the individual’s internal state [21]. This represents the second motivation for this study, which primarily integrates the SOR framework to construct its empirical model.
IRT is a key framework for exploring the underlying causes of consumer resistance to adoption of technology. In this study, we use IRT to examine value barriers, usage barriers, risk barriers, traditional barriers, and impression barriers as distinct stimuli. Further, the job demands–resources (JD-R) model [22] offers valuable insights into the dynamics of AI adoption in healthcare. Job demands and job resources are key factors in shaping employee well-being and performance [22]. In the context of adopting AI-supported healthcare technologies, job demands may include the requirement to learn new technologies, adapt to changing workflows, and manage the increasing complexity of AI-enhanced healthcare tasks. These demands can be stressful for healthcare professionals, though past research has found that moderate stress is positively associated with innovative work behaviors [23]. In terms of job resources, professional development opportunities, a supportive work environment, and adequate training provided by supervisors can help healthcare professionals to manage the aforementioned demands, leading to positive outcomes and increased innovation adoption behaviors [24]. This serves as the third motivation for this study, which integrates the JD-R model to construct its empirical framework.
This study’s core premise is that innovation adoption behavior arises not only from an individual’s inherent traits but also from their work attitudes. Increasingly, scholars have focused on the attitudinal factors that contribute to fostering innovative behavior. One of these factors is employee engagement, which is “operationalized by the intensity and direction of cognitive, emotional, and behavioral energy” [25] (Shuck et al., 2017, p. 2). This is because individuals require greater energy to navigate the challenging process of innovation. Scholars have emphasized the need for a more in-depth exploration of the various personal and environmental factors that influence employee engagement, particularly in the context of innovative behavior [26]. Additionally, past research highlights the critical role of employee engagement in mediating the relationship between job demands, job resources, and behavioral intentions [27] (Kwon & Kim, 2020). Healthcare professionals who are more engaged in their work are also more likely to embrace new technologies, as job engagement enhances their ability to handle the demands of technological change [28]. Furthermore, scholars recommend incorporating variables such as age, religion, and education level into studies of digital transformation in the healthcare industry [3,29]. This is the fourth motivation for this study, which integrates constructs such as employee engagement to develop an empirical model.
Building on the four research motivations, this study integrates the SOR framework [20] (Jacoby, 2002), IRT [12,30,31], the JD-R model [22], and other related concepts such as employee engagement. This study explores the psychological processes linking the independent variable (resistance to AI-supported healthcare technologies) and the dependent variable (behavioral intention). By examining the cognitive and emotional processes behind innovation resistance through the mechanism of serially mediated variables, this study aims to construct a more rigorous research model. Further, it aims to investigate whether resistance to AI-supported healthcare technologies can influence AI adoption behavioral intentions through the serial mediation mechanism of job resources or job demands, along with employee engagement. Additionally, it seeks to provide a deeper understanding of the factors affecting AI adoption behavioral intentions toward adopting AI-supported healthcare technologies by examining age as a moderating variable. Furthermore, this study’s findings can assist healthcare professionals, technologists, and software vendors in developing effective strategies to promote the widespread adoption of AI-supported technologies in the healthcare industry.
This study aims to solve the following questions:
- What role does the SOR framework play in resistance to AI-supported technologies in healthcare?
- Do job resources and job demands influence healthcare professionals’ AI adoption behavioral intentions toward AI-supported healthcare technologies?
- Does work engagement influence healthcare professionals’ AI adoption behavioral intentions toward AI-supported healthcare technologies?
- Does medical professionals’ resistance to artificial intelligence health care technology increase AI adoption behavioral intentions through the sequential mediation of job resources, job demands, and engagement?
- Does age influence healthcare professionals’ AI adoption behavioral intentions toward AI-supported healthcare technologies?
2. Literature Review
2.1. SOR Framework
The SOR framework, originally proposed by Mehrabian and Russell (1974) [32], provides a model for interpreting the behavior of consumers and individuals in response to environmental stimuli. It posits that extrinsic stimuli (S) (for example, AI tools and technologies) [33] and changes in the healthcare environment [34] influence an individual’s (O) internal state or emotions, such as cognitive responses [35,36] and emotional reactions [37], which in turn trigger specific behavioral responses (R), such as behavioral intentions. Previous research has indicated that healthcare professionals’ intention to adopt AI is often determined by the alignment between AI tools and their perceived job demands and resources [38]. In consumer behavior research, the SOR framework has been extensively applied to explain how environmental factors shape consumer emotions and purchasing behaviors [20]. In this framework, stimuli are often interpreted as external cues or marketing elements, organisms represent the affective or cognitive states of consumers, and responses correspond to consumer behaviors, including behavioral intentions, loyalty, or engagement.
This study adopts the SOR framework, one of the most widely recognized models for studying consumer behavior [39], to explore user behavior concerning AI-supported healthcare technologies. Previous research highlights the extensive application of the SOR framework in areas such as online interactions [29], mobile applications [40], and online drug delivery platforms [21]. However, much of this research focuses on online platforms, interactions, and purchasing behaviors, with limited attention given to the intrinsic psychological processes that drive behavioral responses to digital healthcare technologies. The SOR framework, therefore, serves as the foundation for this study, as it facilitates an understanding of the complex psychological processes that healthcare professionals experience in their use of digital healthcare technologies, encompassing both emotional and cognitive experiences.
2.2. Innovation Resistance Theory (IRT)
Innovation is viewed as a substantial and meaningful change in a user’s daily activities [41]. Ram and Sheth (1989) [42] highlight that despite the potential benefits innovation offers to individuals and corporations, there remains a significant degree of resistance to adopting new technologies. The extent of this resistance often determines whether the innovation or technology will succeed or fail.
The IRT, developed by Ram and Sheth (1989) [42], offers insights into why users may be reluctant to adopt innovations. The IRT defines resistance behavior as a negative perception toward the adoption and use of an innovation, driven by an individual’s status quo bias toward existing systems and the perceived barriers posed by new technologies. Individuals exhibit two types of resistance: active resistance and passive resistance, both of which define user resistance behavior from a behavioral perspective [43]. Active resistance arises as a result of the specific characteristics of an innovation, with the IRT addressing both active and passive resistance. Functional barriers are primarily associated with active resistance [44], whereas psychological barriers are more commonly linked to passive resistance [9].
Past research on IRT has explored its application in various fields, including mobile payments [30], electric vehicles [45], environmentally friendly products [46], and online food delivery [47], as well as healthcare-related fields such as healthcare technologies [48], telemedicine [49], and online medication delivery [21]. These studies demonstrate that IRT is a suitable framework for understanding users’ responses to digital healthcare technologies. However, most research utilizing IRT has focused on resistance behavior among end-users, without addressing how to influence resistance behavior before it fully manifests. To bridge this gap in existing research, this study applies the SOR framework to examine whether AI digital healthcare technologies, as an extrinsic stimulus, along with the JD-R model and engagement, which represent intrinsic states or emotions, can help to influence resistance behavior and ultimately trigger a behavioral intention response.
2.3. JD-R Model and Employee Engagement
Bakker and Demerouti (2007) [50] introduced the JD-R model, which is established on the premise that every occupation has distinct risk factors associated with job stress. These factors are categorized into two broad groups: job demands and job resources. This comprehensive model can be applied across various occupational environments, including highly skilled professions such as researchers, professors, and medical professionals [51].
Job demands refer to aspects of work that consistently require the expenditure of an individual’s physiological, psychological, social, or organizational resources, often leading to psychological or physical strain [22]. If physical or mental resources are taxed to an excessive degree, performance outcomes can be adversely affected [52]. Previous research on job demands has primarily focused on aspects such as role conflict, time and workload pressures, and quantitative workloads. Job resources are defined as the physical, social, or organizational aspects of work that facilitate the achievement of job goals; alleviate job demands and their associated physical and psychological costs; and foster personal growth, learning, and development [22]. According to the dual-process JD-R model, reducing job demands allows employees to concentrate more effectively on their tasks and minimize idle time, while increasing job resources helps employees to sustain their energy so as to manage work responsibilities [27].
The concept of employee engagement can be traced back to Kahn (1990) [53], who coined the term “personal engagement” to describe an individual’s psychological state. Kahn suggested that the greater an employee’s personal engagement, the more they will channel their physical and mental energy into their work, thereby fully utilizing their abilities on work tasks. Schaufeli et al. (2002) [54] define employee engagement as a positive, fulfilling, and work-related state of mind characterized by energy, dedication, and focus which is not solely dependent upon any specific events, individuals, or personal behaviors.
3. Research Model Hypothesis Development
3.1. The Mediating Role of the Job Resources
According to the JD-R model, job resources, when leveraged as positive psychological motivators, can help individuals to manage the demands of innovation in the workplace, reduce stress, and enhance overall work outcomes. In the healthcare field, where AI technology is becoming increasingly prevalent, healthcare professionals may resist the adoption of said technology owing to concerns over technological complexity, potential job displacement, or a perceived lack of necessary skills. However, past research suggests that even for the creation of new existing ventures, job resources can offset the financial impact of their business impact [9] and that providing adequate job resources, such as training, can enhance the professionalism of healthcare workers and increase the prevalence of innovative behaviors [27], which in turn may positively influence their AI adoption behavioral intentions to adopt AI-supported healthcare technologies. Therefore, this study suggests that AI-supported healthcare technologies enhance behavioral intention through the mediating effect of job resources.
H1:
Job resources mediate the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
3.2. The Mediating Role of the Job Demands
According to the JD-R model, job demands encompass the cognitive, emotional, and physical requirements placed on employees within professional environments [22]. In the healthcare sector, these demands may include learning to use new tools and adjusting workflows to integrate AI systems. For example, the implementation of AI diagnostic tools may require clinicians to adopt new recommendations and workflows, imposing additional demands on their time and cognitive resources [55]. Previous studies have indicated that when job demands align with job resources, resistance is reduced and AI adoption behavioral intentions are enhanced. Organizations that provide educational training and technical support can mitigate resistance to adopting AI tools, fostering a more positive attitude [56]. Additionally, job demands can serve as a bridge between resistance and AI adoption behavioral intentions. For instance, ensuring that AI systems are intuitive and compatible with existing workflows can reduce perceived complexity and increase adoption willingness [55]. Therefore, this study posits that AI-supported healthcare technology enhances behavioral intention through the mediating role of job demands.
H2:
Job demands mediate the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
3.3. The Mediating Role of the Employee Engagement
In past studies, scholars have argued that job engagement is a more effective predictor of performance than job satisfaction, employee engagement, or organizational commitment [57]. With the increasing adoption of AI-supported healthcare technologies in the near future, engagement is likely to become a crucial motivational factor [58]. Employees with high engagement tend to perform better and work more efficiently [59]. Therefore, healthcare professionals who are highly engaged are less likely to resist AI-supported healthcare technologies [60,61], resulting in a stronger behavioral intention to adopt these technologies. Conversely, healthcare professionals with lower levels of engagement may exhibit greater resistance to innovative technologies, leading to weaker AI adoption behavioral intentions to adopt them. Therefore, this study suggests that AI-supported healthcare technologies enhance behavioral intention through the mediating role of employee engagement.
H3:
Employee engagement mediates the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
3.4. Serial Mediation of the Job Resources, Job Demands and Employee Engagement
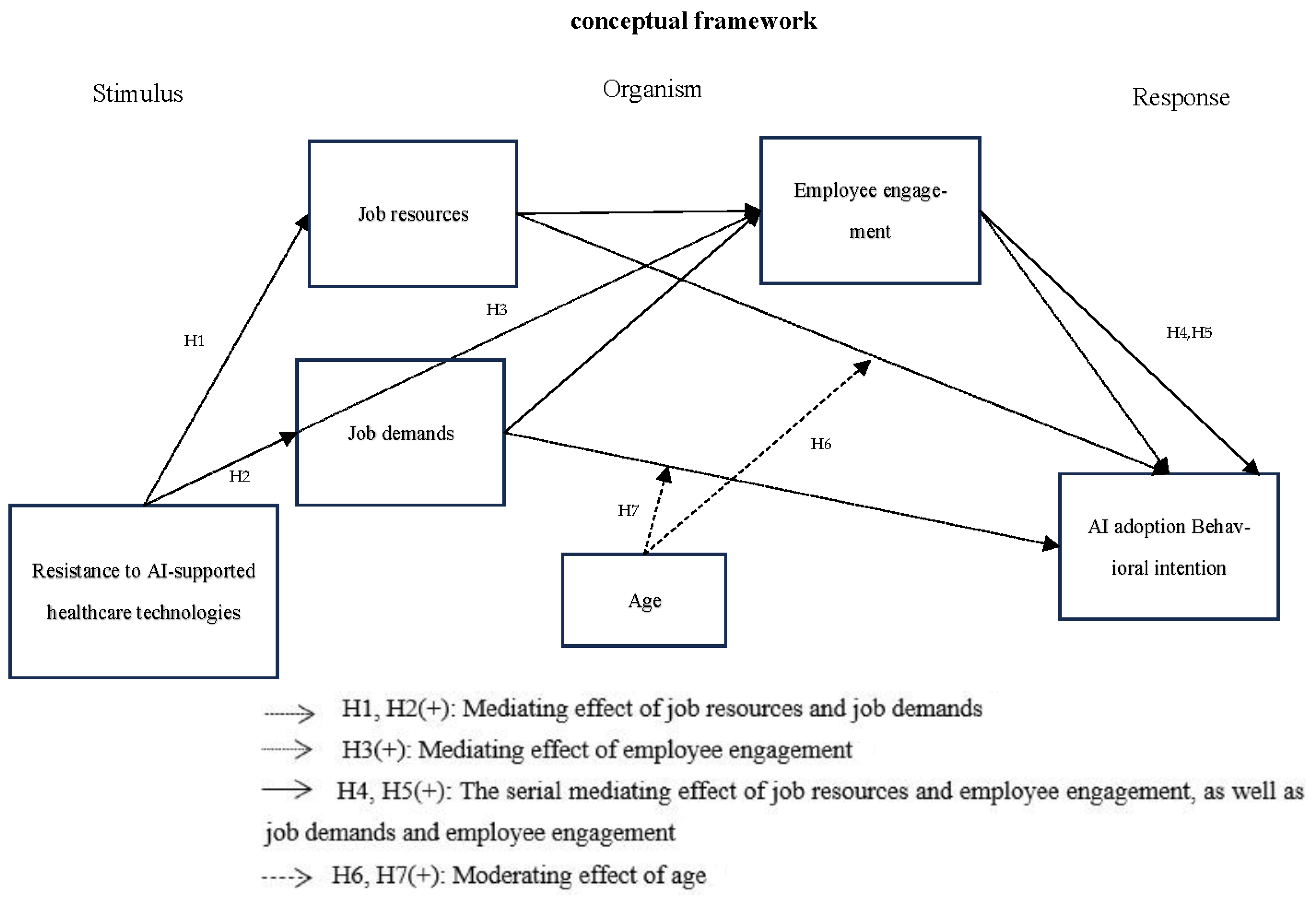
This study integrates the stimulus–organism–response (SOR) framework [20], innovation resistance theory (IRT) [12,30,31], the JD-R model [22], and employee engagement, which are combined with the above three hypotheses (H1~H3) to construct an integrated hypothesis model to further explore the impact of artificial intelligence on health care. Whether technological resistance can improve behavioral intention through the sequential mediation mechanism of job resources or job demands and employee engagement is shown in Figure 1.
Figure 1.
Research framework (Variable’s definition please refer to Appendix A).
This study examines the relationship between job resources, job demands, and engagement, with a focus on their sequential mediating role in the relationship between resistance to AI-enabled medical technologies and behavioral intentions to adopt such innovations. Resistance to AI technologies often manifests through emotional and cognitive barriers which can hinder the adoption of these technologies. However, these barriers can be effectively mitigated through the presence of adequate job resources and manageable job demands, especially when these factors contribute to enhanced employee engagement [62]. The sequential mediation process offers a comprehensive framework to explain how resistance can transform into positive behavioral intentions toward adopting AI technologies.
Previous research has highlighted the critical role of job resources in fostering innovative behaviors. For instance, Kwon and Kim (2020) demonstrated that job resources, such as organizational support, access to learning opportunities, and clear communication, significantly enhance employees’ ability to engage in innovation. Furthermore, an increase in job resources has been shown to directly enhance employee engagement [63], which is characterized by vigor, dedication, and absorption. This heightened engagement ultimately strengthens employees’ behavioral intentions to embrace AI technologies in their professional practices.
Conversely, job demands, such as high workloads or the need to adapt to complex technologies, can induce stress among professionals [23,50]. Despite the potential negative effects of high demands, the job demands–resources (JD-R) model posits that demands, when paired with adequate resources, can function as motivating challenges rather than debilitating stressors [64]. Under such conditions, engagement acts as a psychological mechanism that transforms the perceived burden of job demands into opportunities for professional growth. Hakanen, Schaufeli, and Ahola (2008) [65] demonstrated that the synergy of cognitive, emotional, and physical engagement can mitigate the negative effects of stress and further promote innovative behaviors in high-demand environments.
In this context, engagement plays a pivotal role as a mediating factor. Employees who are deeply engaged are more likely to reinterpret job demands as opportunities for skill enhancement and career development. This reappraisal reduces the negative impact of resistance on their behavioral intentions, fostering a more positive attitude toward AI adoption. By aligning personal and organizational goals, engagement ensures that employees perceive AI technologies as tools that complement their professional responsibilities rather than as threats to their autonomy or job security.
Based on these insights, this study argues that the interplay between job resources, job demands, and engagement is instrumental in reducing resistance to AI-enabled medical technologies. When job resources and demands are managed effectively, they collectively enhance employee engagement, which, in turn, reduces resistance and fosters stronger behavioral intentions to adopt AI technologies. This sequential mediation process underscores the importance of a supportive work environment and the strategic management of demands to ensure the successful integration of AI innovations in healthcare settings.
H4:
Job resources and employee engagement have a serial mediation effect on the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
H5:
Job demands and employee engagement have a serial mediation effect on the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
3.5. The Moderating Effect of Age
Job resources and job demands are crucial for healthcare professionals in adopting AI-supported healthcare technologies. However, one significant factor that has yet to be validated is age [66]. When job resources, such as educational training, are provided, older healthcare professionals may exhibit greater resistance to the adoption of AI-supported healthcare technologies owing to work stress arising from job demands [67]. This resistance could stem from a perceived incompatibility with established work practices and the challenge of quickly adapting to AI technologies and learning new system tools [68,69]. Furthermore, AI adoption behavioral intentions are affected by age-related differences [70]. Therefore, this study argues that age plays a moderating role between job resources, job demands, and the adoption of AI-supported healthcare technologies, influencing AI adoption behavioral intentions toward innovative AI technologies.
H6:
Age moderates the role of job resources in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
H7:
Age moderates the role of job demands in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
Based on the above discussion, this study proposes that there exists a mutual relationship between job resources, job demands, and employee engagement. It also suggests that the link between AI-supported healthcare technologies and AI adoption behavioral intentions should be mediated through a serial mediation model involving job resources, job demands, and employee engagement. In this model, job resources and job demands enhance engagement, which in turn influences healthcare professionals’ AI adoption behavioral intentions toward adopting AI-supported healthcare technologies. Additionally, it is proposed that age moderates the relationship between job resources, job demands, and resistance to AI-supported healthcare technologies, ultimately affecting AI adoption behavioral intentions. This is illustrated in Figure 1, with hypotheses H1 to H7 used as the proposed models.
4. Research Methods
This study examines whether resistance to AI-supported healthcare technologies can enhance AI adoption behavioral intentions when serially mediated through job resources, job demands, and employee engagement, with age serving as a moderating variable. In this study, an online questionnaire was conducted using purposive sampling. Past research has indicated that innovative medical technologies are more commonly implemented in medical institutions, particularly in large healthcare organizations, specialty hospitals, and teaching hospitals. These medical institutions typically have better resources, expertise, and research support, enabling them to introduce and apply the latest medical technologies more quickly [71,72]. Additionally, the healthcare professionals who use AI-supported healthcare technologies are typically physicians [73], pharmacists [74], and registered nurses [75]. Therefore, the target population for this study consists of healthcare professionals practicing in medical institutions, with the following principles implemented for sampling: 1. Healthcare professionals shall be the subjects of this study, including physicians, registered nurses, and pharmacists; 2. Participants shall have achieved an educational level of university/college graduate or higher. Based on the above, this study focused on the online question-and-answer method, with a total of 334 questions and answers. A total of 190 questionnaires were sent and telephone reminders were made. A total of 152 valid question questionnaires were collected (effective collection rate 80%, are shown in Table 1.

Table 1.
Demographic information of the valid study subject sample.
The questionnaire content was designed using items adapted from previous research to measure the constructs in this study’s model. Participants rated each item on a six-point Likert scale.
Job resources and job demands: This study used Scholze and Hecker’s (2024) [76] 24-item questionnaire to measure the job resources (M = 4.01, SD = 1.02, Cronbach’s α = 0.869) and job demands (M = 4.29, SD = 0.7, Cronbach’s α = 0.945) of healthcare professionals. Respondents rated their level of agreement with each statement on a six-point scale, ranging from 1 to 6 (e.g., How often do you not have enough time to complete all your tasks?; I am free to organize my work in terms of time).
Employee engagement: This study measured the level of engagement of healthcare professionals using the 15-item questionnaire developed by Shuck, Adelson, and Reio Jr. (2017) [25] (M = 4.59, SD = 0.77, Cronbach’s α = 0.934). Respondents rated their level of agreement with each statement on a six-point scale, ranging from 1 to 6 (e.g., I am really focused on my job when I am working; I work harder than expected to help my company be successful).
Resistance to innovation: This study used Kautish et al.’s (2023) [77] 21-item questionnaire (M = 4.13, SD = 0.66, Cronbach’s α = 0.911) to measure healthcare professionals’ resistance to AI-supported healthcare technologies, with statements encompassing use (6-item), value (5-item), risk (2-item), tradition (6-item), and impression-related barriers (2-item). Respondents rated their level of agreement with each statement on a six-point scale, ranging from 1 to 6 (e.g., telemedicine apps are convenient as they are accessible through my phone; I believe using telemedicine apps helps save time; I fear that using telemedicine apps may not ensure privacy and confidentiality).
AI adoption behavioral intentions: This study used Edo et al.’s (2023) [78] four-item questionnaire to measure the AI adoption behavioral intentions of healthcare professionals (M = 4.35, SD = 0.87, Cronbach’s α = 0.955). Respondents rated their level of agreement with each statement on a six-point scale, ranging from 1 to 6 (e.g., I intend to use AI health information technology in the future).
This study conducted a Confirmatory Factor Analysis (CFA) using AMOS. The overall model fit was acceptable (χ²/df = 387.033/98 = 3.949, RMSEA = 0.1, NFI = 0.902, CFI = 0.924, IFI = 0.925, SRMR = 0.106, GFI = 0.855, PNFI = 0.736).
The CMV problem was assessed following the commonly used Harman’s one-factor test (Fuller, Simmering, Atinc, Atinc, & Babin, 2016) [79] during data collection. Single factor analysis was an exploratory factor analysis (EFA) of all the measured indicators of the five research institutions together without factor transformation to determine how many individual factors were needed to explain the changes between the indicators [80]. Therefore, it was estimated that the CMV in this study was not too severe.
The descriptive statistics of the main variables of this study, including CR value, Cronbach’s α, AVE value, and discriminant validity testing, are shown in Table 2.

Table 2.
Descriptive statistics of the main variables.
In this study, serial mediation analysis was conducted to examine the mediating role of job resources, job demands, and employee engagement in the relationship between resistance to AI-supported healthcare technology innovation and AI adoption behavioral intentions. Barriers resulting in resistance to technological innovation in AI-supported healthcare technologies served as the independent variable, with job resources and job demands acting as first-stage mediators, employee engagement as a second-stage mediator, and AI adoption behavioral intentions as the dependent variable [81] (PROCESS Model 6). Finally, this study conducted an analysis of moderating variables to examine the moderating role of job resources and job demands in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions, with age as the moderating variable [81] (PROCESS Model 14). For the statistical analysis using PROCESS Model 14, this study applied the bootstrapping method to generate a 95% confidence interval based on 5000 samples.
5. Results
This study examines whether the serial mediation of job resources, job demands, and employee engagement influences the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions, analyzed using the PROCESS statistical model.
H1 assumes that job resources mediate the relationship between resistance to AI-supported healthcare technology and behavioral intentions to adopt AI. The mediation analysis indicates that resistance to AI-supported healthcare technology has a significant positive impact on job resources (B = 0.48, SE = 0.54, CI = 0.40, 0.62); in turn, job resources significantly increase AI adoption behavioral intentions (B = 0.23, SE = 0.07, CI = 0.13, 0.42). These findings support the existence of a significant indirect effect of resistance to AI-supported healthcare technologies on AI adoption behavioral intentions through job resources (B = 0.14, SE = 0.04, CI = 0.05, 0.24), shown in Table 3, thus validating H1.

Table 3.
Research framework (job resources as mediating factor).
H2 assumes that job demands mediate the relationship between resistance to AI-supported healthcare technologies and behavioral intention to adopt AI. Mediation analysis showed that resistance to artificial intelligence medical technology had a significant positive impact on job demands (B = 0.45, SE = 0.79, CI = 0.54, 0.86); in turn, job demands significantly increase AI adoption behavioral intentions (B = 0.28, SE = 0.04, CI = 0.15, 0.32). These findings support the existence of a significant indirect effect of resistance to AI-supported healthcare technologies on behavioral intention through job demands (B = 0.12, SE = 0.03, CI = 0.07, 0.18), shown in Table 4, thus validating H2.

Table 4.
Research Framework (Job demands as mediating factor).
H3 assumes that employee engagement mediates the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. The mediation analysis results indicate that resistance to AI-supported healthcare technologies significantly increases employee engagement (B = 0.26, SE = 0.60, CI = 0.19, 0.43; B = 0.41, SE = 0.06, CI = 0.35, 0.61); further, employee engagement significantly increases AI adoption behavioral intentions (B = 0.40, SE = 0.06, CI = 0.32, 0.58; B = 0.46, SE = 0.05, CI = 0.40, 0.63). These results support the finding that resistance to AI-supported healthcare technologies has a significant indirect effect on AI adoption behavioral intentions through employee engagement (B = 0.14, SE = 0.03, CI = 0.07, 0.21; B = 0.19, SE = 0.03, CI = 0.12, 0.27), shown in Table 3 and Table 4, thus validating H3.
H4 assumes that the mediators of H1 and H3, namely job resources and employee engagement, have a serial mediation effect on the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. The results of the serial mediation analyses indicate that resistance to AI-supported healthcare technologies significantly increases job resources (B = 0.48, SE = 0.54, CI = 0.40, 0.62) and, in a serial manner, significantly increases both employee engagement (B = 0.45, SE = 0.56, CI = 0.39, 0.61) and AI adoption behavioral intentions (B = 0.40, SE = 0.06, CI = 0.32, 0.58). Furthermore, resistance to AI-supported healthcare technologies has a significant indirect effect on AI adoption behavioral intentions through job resources and employee engagement (B = 0.11, SE = 0.02, CI = 0.06, 0.18), shown in Table 3, thus validating H4.
H5 assumes that the mediators of H2 and H3, namely job demands and employee engagement, have a serial mediation effect on the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. The results of the serial mediation analyses indicate that resistance to AI-supported healthcare technologies significantly increases job demands (B = 0.45, SE = 0.79, CI = 0.54, 0.86) and, in a serial manner, significantly increases both employee engagement (B = 0.15, SE = 0.04, CI = 0.03, 0.20) and AI adoption behavioral intentions (B = 0.46, SE = 0.05, CI = 0.40, 0.63). Additionally, resistance to AI-supported healthcare technologies has a significant indirect effect on AI adoption behavioral intentions through job demands and employee engagement (B = 0.03, SE = 0.01, CI = 0.05, 0.06), shown in Table 3 and Table 4, thus supporting H5.
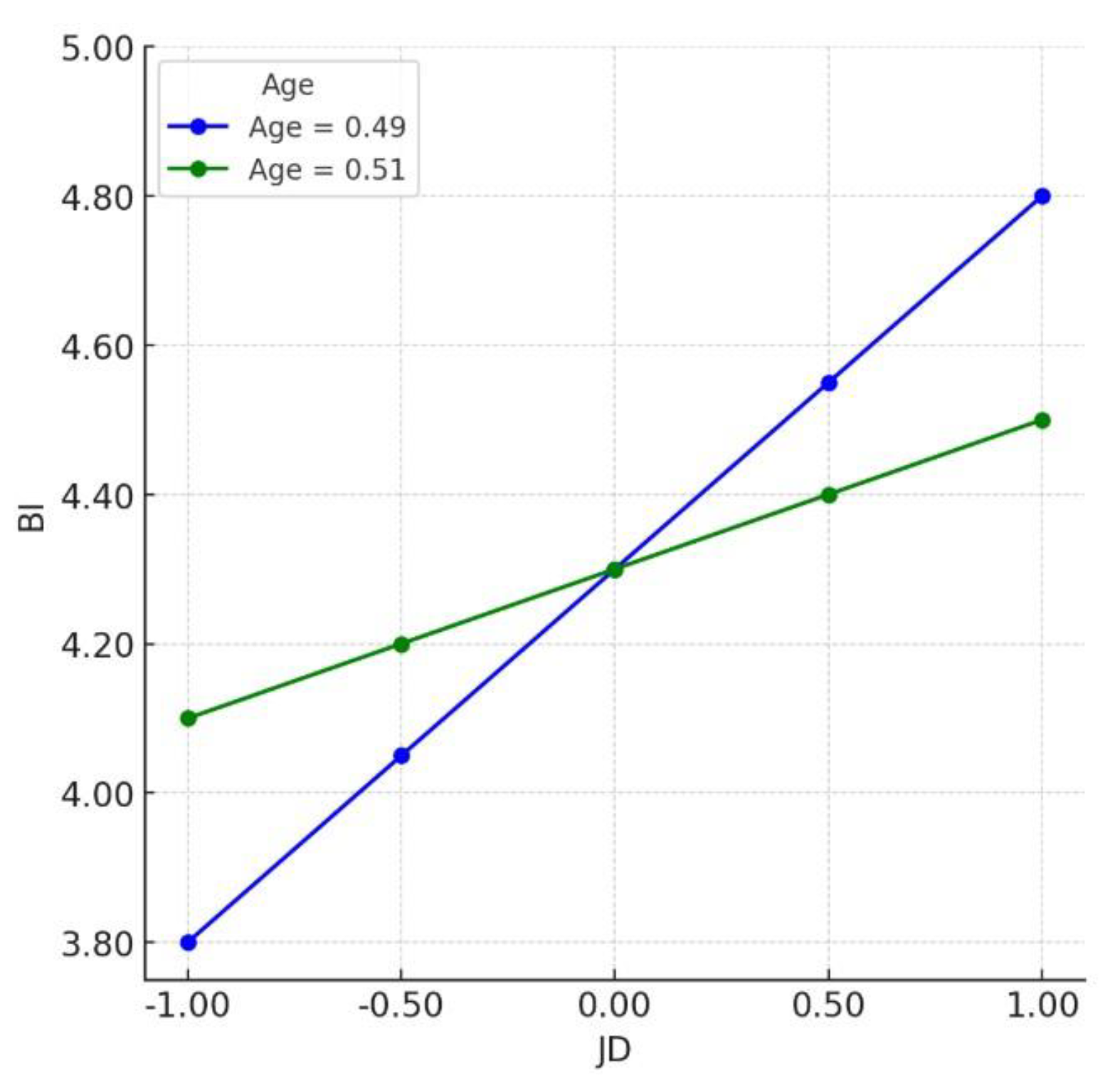
H6 and H7 assume that age moderates the role of job resources and job demands in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. The analysis of the results indicates that job resources and job demands exhibit indirect effects on resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. The moderating influence of job resources on the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions is not significant with the moderation of age (B = −0.093, SE = 0.067, CI = −0.23, 0.031). Thus, H6 is not supported. However, there is a significant negative moderating influence of job demands on the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions with the moderation of age (B = −0.158, SE = 0.07, CI = −0.297, −0.021), shown in Table 5 and Figure 2. Thus, H7 is supported.

Table 5.
Table of moderating effects.
Figure 2.
Age moderation.
6. Discussion
This study utilized the SOR framework to examine the relationships between relevant constructs and investigate the AI adoption behavioral intentions of healthcare professionals regarding resistance to AI-supported healthcare technologies. This model facilitated the investigation of seven mediating and moderating relationships within the research framework, providing insights into the AI adoption behavioral intentions of healthcare professionals regarding AI-supported healthcare technologies. We first examined the mediating role of job resources, job demands, and employee engagement in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. Additionally, we identified the significant moderating effect of age on the relationships between resistance to AI-supported healthcare technologies, job demands, and AI adoption behavioral intentions.
- (i)
- The mediating effect of job resources and job demands
Past research has indicated that job resources can alleviate resistance to AI-supported healthcare technologies by fostering work engagement and reducing the perceived stress or increased workload associated with said technologies [64,82]. These resources tend to enhance employee adaptability and cultivate positive attitudes toward adopting new technologies [60], which is aligned with the findings of this study.
However, regarding job demands, past research suggests that increased demands can heighten resistance by amplifying stress and reducing engagement, thereby lowering the likelihood of adopting innovations such as AI technologies [69,83]. Studies suggest that when the introduction of AI technologies increases employee workload or task complexity, job demands may heighten resistance. However, these findings differ from the results of the current study.
This study suggests that appropriate job demands can still mitigate healthcare professionals’ resistance to AI-supported healthcare technologies, owing to factors such as a higher perceived usefulness of said technologies [84], employee adherence to professional norms and role expectations [85], and a strong prioritization of patient well-being [86] when considering new technologies.
- (ii)
- The mediating effect of employee engagement
Employee engagement, characterized by a strong focus on one’s work, significantly influences behavioral intentions to adopt innovations. Past scholars have noted that higher engagement increases employees’ willingness to adopt AI-supported healthcare technologies [42]. Furthermore, highly engaged employees are more likely to embrace the changes introduced by AI technologies [60]. These results align with the findings of the present study, suggesting that employee engagement mitigates resistance to the introduction of new technologies in the workplace. Healthcare professionals with higher levels of engagement are more inclined to perceive AI-supported healthcare technologies as tools to enhance patient care, benefiting both themselves and their patients, and thereby have a greater willingness to learn and adopt these technologies. Thus, employee engagement mediates the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions.
- (iii)
- The serial mediation of job resources, job demands, and employee engagement
The results of this study demonstrate that job resources, job demands, and employee engagement can all mediate the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. Using the SOR framework, resistance to AI-supported healthcare technologies serves as the stimulus, while job resources, job demands, and engagement act as positive influences on AI adoption behavioral intentions through initiating a response. This framework effectively explains how the serial mediation of job resources, job demands, and engagement mitigate resistance to innovation among healthcare professionals, thereby enhancing their AI adoption behavioral intentions to adopt AI-supported healthcare technologies.
- (iv)
- The moderating effect of age
This study identified differences in the results when age was considered a moderator. Specifically, age demonstrated a significant negative moderating effect on job demands in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. However, age did not exhibit a significant moderating effect in the context of job resources. We believe that when healthcare professionals are in the process of adopting AI-supported healthcare technologies, older employees perceive the associated job demands to be a greater challenge, which negatively impacts their AI adoption behavioral intentions. Younger employees, however, may view these job demands as opportunities for career progression and skill development, leading to more positive AI adoption behavioral intentions.
Age does not have a significant moderating effect on job resources. This study suggests that this is because job resources, such as supportive training, benefit all employees. Regardless of age, the effect of training and resource support in helping employees cope with the introduction of AI in the healthcare field may not change significantly.
- (v)
- Theoretical implications
This study contributes to the field of research on the digital healthcare industry, as past scholars have emphasized the importance of understanding consumer resistance to the adoption of digital healthcare technologies [86] (Li et al., 2022). This study also addresses three gaps in the existing research on this topic. Gap 1: While IRT [42] provides a theoretical framework for understanding healthcare professionals’ resistance to new technologies and explains the factors contributing to resistance, it lacks specificity regarding the underlying cognitive and affective mechanisms that link resistance to behavioral outcomes, such as adoption intentions. By incorporating the SOR framework, this study explores how job resources, job demands, and employee engagement influence AI adoption behavioral intentions. In this context, resistance to AI-supported healthcare technologies is viewed as a stimulus that ultimately alters AI adoption behavioral intentions through the mediation of job resources, job demands, and employee engagement. The above findings enrich our understanding of various aspects of technology adoption and provide a more comprehensive model for understanding the adoption of AI technology in the healthcare industry. Gap 2: Kwon and Kim’s (2020) model, which refined the JD-R model to include the concept of engagement, lacked empirical evidence to support this change. This study fills the gap in evidence by confirming that employee engagement plays an indispensable role as a serial mediator between innovation resistance and AI adoption behavioral intentions, specifically through job resources and job demands. The empirical results provide new insights into how best to reduce resistance to AI-supported healthcare technologies in the healthcare field. Gap 3: Past scholars have suggested that when studying digital transformation in the healthcare industry, variables such as age, religion, and education should be included [3,29]. This study addresses this gap by confirming that age significantly moderates job demands in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. However, age exhibited no significant moderating effect on job resources in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions. This suggests that the effect of job demands on resistance to adoption is more pronounced among older healthcare professionals, whereas job resources exert a more universally positive influence across age groups [87]. These findings highlight the importance of incorporating demographic factors into analysis when examining the adoption of innovative digital technologies.
As mentioned above, this study’s empirical findings make a significant contribution to enhancing our understanding of how job resources, job demands, and employee engagement affect healthcare professionals’ resistance to AI-supported healthcare technologies through three theoretical constructs: IRT, the SOR framework, and the JD-R model. In addition, by incorporating age as a moderator, this study provides new insights into how individual and contextual factors interact to influence resistance to the adoption of AI-supported healthcare technologies and to shape AI adoption behavioral intentions. The aforementioned theoretical contributions offer valuable directions for future research, particularly regarding the role of the work environment and demographic factors in influencing the adoption of technologies in the healthcare industry.
7. Conclusions and Recommendations
- (i)
- Management Implications
This study’s results have significant managerial implications for the healthcare industry, particularly for organizations seeking to facilitate the adoption of AI-supported technologies while addressing potential resistance from healthcare professionals. Senior managers must understand that resistance to AI-supported healthcare technologies is influenced by a variety of factors, including job demands, job resources, and demographic characteristics such as age. Understanding the multitude of factors involved can help managers design strategies that effectively reduce resistance and encourage the adoption of AI-supported healthcare technologies. For example, healthcare organizations can reduce resistance to AI healthcare technologies by strategically increasing job resources (e.g., AI training, leadership support, and workflow integration) and balancing job demands (e.g., cognitive workload and emotional stress).
First, this study’s results demonstrated that age moderates job demands in the relationship between resistance to AI-supported healthcare technologies and AI adoption behavioral intentions, indicating that older healthcare professionals may find it more challenging to adapt to new technologies. Therefore, managers should develop tailored support systems for healthcare professionals of different age groups. For example, customized training for older healthcare professionals can help them adapt to AI technologies and reduce resistance to adoption. In addition, increasing employee engagement is crucial for reducing resistance to AI-supported healthcare technologies. This study empirically demonstrates that engagement mediates the relationship between job resources, job demands, resistance to AI-supported healthcare technologies, and AI adoption behavioral intentions. Senior managers can apply the two-factor theory to enhance healthcare professionals’ satisfaction and, in turn, increase their engagement.
Healthcare institutions can reduce resistance to AI healthcare technologies by strategically increasing job resources (e.g., AI training, leadership support, and workflow integration) and balancing job demands (e.g., cognitive workload and emotional stress). For example, when introducing an AI-powered radiology system, medical professionals resisted its adoption due to concerns about job displacement and increased workload.
To address this, the institution provided specialized AI training, assurances from hospital leadership, and seamless integration of AI with electronic health records (EHRs). Additionally, radiology assistants were assigned to verify AI-generated reports, reducing the workload for radiologists. By implementing these strategies, healthcare institutions can mitigate resistance and foster greater acceptance of AI technologies in clinical practice.
- (ii)
- Research Limitations and Directions for Future Research
Although this study offers valuable insights into healthcare professionals’ resistance to AI-supported healthcare technologies and makes significant contributions to existing literature on this topic, there still exist some limitations. First, this study was conducted solely in Taiwan, which may limit the generalizability of the results to other regions. Similar studies could be conducted in other developing regions to gain a deeper understanding of the factors that may reduce healthcare professionals’ resistance to AI-supported healthcare technologies. Second, this study only considered the moderating effect of a single variable: age. This is despite past research suggesting that more demographic variables should be included in studies of IRT. Therefore, future research could incorporate additional demographic variables to better understand their different effects. Although this study uses the SOR framework as its theoretical basis, it still cannot avoid the problem of endogeneity. Therefore, it is recommended that future research can include an instrumental variable approach that may address such potential endogeneity in the relationship. This study, despite its limitations, offers valuable theoretical and practical insights for healthcare professionals, technologists, and software vendors and acts as a guide for the implementation of AI technologies in the healthcare industry.
Author Contributions
Conceptualization, L.-M.C. and S.-H.H.; methodology, L.-M.C. and S.-H.H.; software L.-M.C. and S.-H.H.; validation, L.-M.C. and S.-H.H.; formal analysis, L.-M.C. and S.-H.H.; investigation, L.-M.C. and S.-H.H.; resources, L.-M.C. and S.-H.H.; data curation, L.-M.C. and S.-H.H.; writing—original draft preparation, L.-M.C. and S.-H.H. These authors contributed equally to this work. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The authors confirm that the data supporting the findings of this study and the original contributions presented are available within the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Variable description.
Table A1.
Variable description.
| Variable | Label | Definition | Source |
|---|---|---|---|
| Independent variable | AI-supported healthcare technologies | Refers to the creation of new knowledge, tools, and ideas using human-like intelligence (e.g., artificial intelligence, including machine learning, deep learning, neural networks, and reinforcement learning) that is programmed to think like humans and imitate their behavior. | Du Plessis, M. (2007) [88] |
| Dependent variable | AI adoption behavioral intention | Behavioral intention refers to an individual’s readiness to adopt AI technology based on perceived benefits, feasibility, and motivation | Huang, Y.C. (2023) [89] |
| Mediator variable | job demands | Job resources refer to job related attributes that positively influence an employee’s work achievement, physical and psychological well-being, and learning and growth; personal resources refer to an individual’s sense of his or her ability to successfully control and impact circumstances. | Hobfoll, 2001 [90] |
| job resources | Job demands refer to job-related characteristics that require significant physical and psychological investment and if overwhelming, hinder performance outcomes. | Hakanen & Roodt, 2010 [51] | |
| employee engagement | Personal engagement, satisfaction, and enthusiasm for work | Kang, J. et al. (2020) [91] |
References
- Del Giudice, M.; Scuotto, V.; Papa, A.; Tarba, S.Y.; Bresciani, S.; Warkentin, M. A self-tuning model for smart manufacturing SMEs: Effects on digital innovation. J. Prod. Innov. Manag. 2021, 38, 68–89. [Google Scholar] [CrossRef]
- Westerman, G.; Bonnet, D.; McAfee, A. Leading Digital: Turning Technology into Business Transformation; Harvard Business Press: Boston, MA, USA, 2014. [Google Scholar]
- Iyanna, S.; Kaur, P.; Ractham, P.; Talwar, S.; Islam, A.N. Digital transformation of healthcare sector. What is impeding adop-tion and continued usage of technology-driven innovations by end-users? J. Bus. Res. 2022, 153, 150–161. [Google Scholar] [CrossRef]
- Kapletia, D.; Phillips, W.; Medcalf, N.; Makatsoris, H.; McMahon, C.; Rich, N. Redistributed manufacturing—Challenges for operations management. Prod. Plan. Control. 2019, 30, 493–495. [Google Scholar] [CrossRef]
- Talwar, S.; Talwar, M.; Tarjanne, V.; Dhir, A. Why retail investors traded equity during the pandemic? An application of artificial neural networks to examine behavioral biases. Psychol. Mark. 2021, 38, 2142–2163. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Sunarti, S.; Rahman, F.F.; Naufal, M.; Risky, M.; Febriyanto, K.; Masnina, R. Artificial intelligence in healthcare: Opportunities and risk for future. Gac. Sanit. 2021, 35, S67–S70. [Google Scholar] [CrossRef]
- Chien, C.F.; Dauzes, S.; Huh, W.T.; Jang, Y.J.; Morrison, J.R. Artificial intelligence in manufacturing and logistics systems: Algorithms, applications, and case studies. Int. J. Prod. Res. 2020, 58, 2730–2731. [Google Scholar] [CrossRef]
- Shankar, A.; Kumar, A.; Yadav, R.; Misra, P.; Pani, S.K. Should I adopt an integrated virtual clinic? A dual-factor theory perspective. J. Consum. Behav. 2024, 23, 357–371. [Google Scholar] [CrossRef]
- Talwar, S.; Dhir, A.; Islam, N.; Kaur, P.; Almusharraf, A. Resistance of multiple stakeholders to e-health innovations: Inte-gration of fundamental insights and guiding research paths. J. Bus. Res. 2023, 166, 114135. [Google Scholar] [CrossRef]
- Webster, P. Virtual health care in the era of COVID-19. Lancet 2020, 395, 1180–1181. [Google Scholar] [CrossRef]
- Talwar, S.; Talwar, M.; Kaur, P.; Dhir, A. Consumers’ resistance to digital innovations: A systematic review and framework development. Australas. Mark. J. 2020, 28, 286–299. [Google Scholar] [CrossRef]
- Woo, Y.; Andres, P.T.C.; Jeong, H.; Shin, C. Classification of diabetic walking through machine learning: Survey targeting senior citizens. In Proceedings of the International Conference on Artificial Intelligence in Information and Communication, Jeju Island, Republic of Korea, 20–23 April 2021; pp. 435–437. [Google Scholar]
- Deebak, B.D.; Al-Turjman, F. Smart mutual authentication protocol for cloud based medical healthcare systems using internet of medical things. IEEE J. Sel. Areas Commun. 2021, 39, 346–360. [Google Scholar]
- Kaur, A.; Garg, R.; Gupta, P. Challenges facing AI and big data for resource poor healthcare system. In Proceedings of the 2nd International Conference on Electronics and Sustainable Communication Systems, Coimbatore, India, 4–6 August 2021; pp. 1426–1433. [Google Scholar]
- Mitchell, M.; Kan, L. Digital technology and the future of health systems. Health Syst. Reform 2019, 5, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, S.; Gandhi, C. Capability-based access control with trust for effective healthcare systems. Int. J. Cloud Appl. Comput. 2022, 12, 1–28. [Google Scholar] [CrossRef]
- Kumari, P.; Shankar, A.; Behl, A.; Pereira, V.; Yahiaoui, D.; Laker, B.; Gupta, B.B.; Arya, V. Investigating the barriers towards adoption and implementation of open innovation in healthcare. Technol. Forecast. Soc. Change 2024, 200, 123100. [Google Scholar] [CrossRef]
- Chong, A.Y.L.; Blut, M.; Zheng, S. Factors influencing the acceptance of healthcare information technologies: A meta-analysis. Inf. Manag. 2022, 59, 103604. [Google Scholar] [CrossRef]
- Jacoby, J. Stimulus-organism-response reconsidered: An evolutionary step in modeling (consumer) behavior. J. Consum. Psychol. 2002, 12, 51–57. [Google Scholar] [CrossRef]
- Chakraborty, D.; Singu, H.B.; Kar, A.K.; Biswas, W. From fear to faith in the adoption of medicine delivery application: An integration of SOR framework and IRT theory. J. Bus. Res. 2023, 166, 114140. [Google Scholar]
- Demerouti, E.; Bakker, A.B. The job demands-resources model: Challenges for future research. SA J. Ind. Psychol. 2011, 37, 1–9. [Google Scholar]
- Anjum, A.; Zhao, Y. The impact of stress on innovative work behavior among medical healthcare professionals. Behav. Sci. 2022, 12, 340. [Google Scholar] [CrossRef]
- Koroglu, Ş.; Ozmen, O. The mediating effect of work engagement on innovative work behavior and the role of psychological well-being in the job demands–resources (JD-R) model. Asia-Pac. J. Bus. Adm. 2022, 14, 124–144. [Google Scholar]
- Shuck, B.; Adelson, J.L.; Reio, T.G., Jr. The employee engagement scale: Initial evidence for construct validity and implications for theory and practice. Hum. Resour. Manag. 2017, 56, 953–977. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Perhoniemi, R.; Toppinen-Tanner, S. Positive gain spirals at work: From job resources to work engagement, personal initiative and work-unit innovativeness. J. Vocat. Behav. 2008, 73, 78–91. [Google Scholar]
- Kwon, K.; Kim, T. An integrative literature review of employee engagement and innovative behavior: Revisiting the JD-R model. Hum. Resour. Manag. Rev. 2020, 30, 100704. [Google Scholar]
- Shamsi, M.; Iakovleva, T.; Olsen, E.; Bagozzi, R.P. Employees’ work-related well-being during COVID-19 pandemic: An integrated perspective of technology acceptance model and JD-R theory. Int. J. Environ. Res. Public Health 2021, 18, 11888. [Google Scholar] [CrossRef]
- Lee, C.H.; Chen CW, D.; Huang, S.F.; Chang, Y.T.; Demirci, S. Exploring consumers’ impulse buying behavior on online apparel websites: An empirical investigation on consumer perceptions. Int. J. Electron. Commer. Stud. 2021, 12, 119–142. [Google Scholar]
- Kaur, P.; Dhir, A.; Singh, N.; Sahu, G.; Almotairi, M. An innovation resistance theory perspective on mobile payment solutions. J. Retail. Consum. Serv. 2020, 55, 102059. [Google Scholar] [CrossRef]
- Talwar, S.; Dhir, A.; Khalil, A.; Mohan, G.; Islam AK, M.N. Point of adoption and beyond. Initial trust and mobile-payment continuation intention. J. Retail. Consum. Serv. 2020, 55, 102086. [Google Scholar]
- Mehrabian, A.; Russell, J.A. An Approach to Environmental Psychology; The MIT Press: Cambridge, MA, USA, 1974. [Google Scholar]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, e000101. [Google Scholar] [CrossRef]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar]
- Zou, X.; Na, Y.; Lai, K.; Liu, G. Unpacking public resistance to health Chatbots: A parallel mediation analysis. Front. Psychol. 2024, 15, 1276968. [Google Scholar] [CrossRef] [PubMed]
- Ye, T.; Xue, J.; He, M.; Gu, J.; Lin, H.; Xu, B.; Cheng, Y. Psychosocial factors affecting artificial intelligence adoption in health care in China: Cross-sectional study. J. Med. Internet Res. 2019, 21, e14316. [Google Scholar] [CrossRef] [PubMed]
- Jarrahi, M.H. Artificial intelligence and the future of work: Human-AI symbiosis in organizational decision making. Bus. Horiz. 2018, 61, 577–586. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Stocchi, L.; Pourazad, N.; Michaelidou, N.; Tanusondjaja, A.; Harrigan, P. Marketing research on Mobile apps: Past, present and future. J. Acad. Mark. Sci. 2022, 50, 195–225. [Google Scholar] [CrossRef]
- Bhandari, U.; Neben, T.; Chang, K.; Chua, W.Y. Effects of interface design factors on affective responses and quality evalua-tions in mobile applications. Comput. Hum. Behav. 2017, 72, 525–534. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Balakrishnan, J.; Das, R.; Dutot, V. Resistance to innovation: A dynamic capability model based enquiry into retailers’ resistance to blockchain adaptation. J. Bus. Res. 2023, 157, 113632. [Google Scholar] [CrossRef]
- Ram, S.; Sheth, J.N. Consumer resistance to innovations: The marketing problem and its solutions. J. Consum. Mark. 1989, 6, 5–14. [Google Scholar] [CrossRef]
- Heidenreich, S.; Handrich, M. What about passive innovation resistance? Investigating adoption-related behavior from a resistance perspective. J. Prod. Innov. Manag. 2015, 32, 878–903. [Google Scholar] [CrossRef]
- Chen, H.S.; Tsai, B.K.; Hsieh, C.M. The effects of perceived barriers on innovation resistance of hydrogen-electric motorcycles. Sustainability 2018, 10, 1933. [Google Scholar] [CrossRef]
- Sadiq, M.; Adil, M.; Paul, J. An innovation resistance theory perspective on purchase of eco-friendly cosmetics. J. Retail. Consum. Serv. 2021, 59, 102369. [Google Scholar] [CrossRef]
- Khalil, A.; Shankar, A.; Bodhi, R.; Behl, A.; Ferraris, A. Why do people resist drone food delivery services? An innovation resistance theory perspective. IEEE Trans. Eng. Manag. 2022, 71, 13038–13048. [Google Scholar] [CrossRef]
- Chen, P.T.; Lin, C.L.; Wu, W.N. Big data management in healthcare: Adoption challenges and implications. Int. J. Inf. Manag. 2020, 53, 102078. [Google Scholar] [CrossRef]
- Tsai, J.M.; Cheng, M.J.; Tsai, H.H.; Hung, S.W.; Chen, Y.L. Acceptance and resistance of telehealth: The perspective of du-al-factor concepts in technology adoption. Int. J. Inf. Manag. 2019, 49, 34–44. [Google Scholar] [CrossRef]
- Galanakis, M.D.; Tsitouri, E. Positive psychology in the working environment. Job demands-resources theory, work en-gagement and burnout: A systematic literature review. Front. Psychol. 2022, 13, 1022102. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job demands–resources theory: Taking stock and looking forward. J. Occup. Health Psychol. 2017, 22, 273. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Roodt, G. Using the job demands-resources model to predict engagement: Analyzing a conceptual model. In Work Engagement: A Handbook of Essential Theory and Research; Bakker, A.B., Leiter, M.P., Eds.; Psychology Press: New York, NY, USA, 2010; pp. 85–101. [Google Scholar]
- Yang, Y.; Ngai, E.W.; Wang, L. Resistance to artificial intelligence in health care: Literature review, conceptual framework, and research agenda. Inf. Manag. 2024, 61, 103961. [Google Scholar] [CrossRef]
- Kahn, W.A. Psychological conditions of personal engagement and disengagement at work. Acad. Manag. J. 1990, 33, 692–724. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Salanova, M.; González-Romá, V.; Bakker, A.B. The measurement of engagement and burnout: A two sample confirmatory factor analytic approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Achananuparp, P. Perceptions and needs of artificial intelligence in health care to increase adoption: Scoping review. J. Med. Internet Res. 2022, 24, e32939. [Google Scholar] [CrossRef]
- Rich, B.L.; LePine, J.A.; Crawford, E.R. Job engagement: Antecedents and effects on job performance. Acad. Manag. J. 2010, 53, 617–635. [Google Scholar]
- Tims, M.; Bakker, A.B.; Derks, D. Development and validation of the job crafting scale. J. Vocat. Behav. 2012, 80, 173–186. [Google Scholar]
- Kim, W.; Kolb, J.A.; Kim, T. The Relationship between work engagement and performance: A review of empirical literature and a proposed research agenda. Hum. Resour. Dev. Rev. 2013, 12, 248–276. [Google Scholar]
- Wang, W.; Chen, L.; Xiong, M.; Wang, Y. Accelerating AI adoption with responsible AI signals and employee engagement mechanisms in health care. Inf. Syst. Front. 2023, 25, 2239–2256. [Google Scholar] [CrossRef]
- Paul, P.; Singh, B. Healthcare employee engagement using the internet of things: A systematic overview. Adopt. Eff. Artif. Intell. Hum. Resour. Manag. 2023, Part A, 71–97. [Google Scholar]
- Gürbüz, S.; Schaufeli, W.B.; Freese, C.; Brouwers, E.P. Fueling creativity: HR practices, work engagement, personality, and autonomy. Int. J. Hum. Resour. Manag. 2024, 35, 3770–3799. [Google Scholar]
- Rosyafah, S.; Pudjowati, J. What are the Key Determinants of Human Resource Management Effectiveness in Enhancing Organizational Financial Performance? Atestasi J. Ilm. Akunt. 2024, 7, 525–560. [Google Scholar] [CrossRef]
- Rafique, M.A.; Hou, Y.; Chudhery MA, Z.; Waheed, M.; Zia, T.; Chan, F. Investigating the impact of pandemic job stress and transformational leadership on innovative work behavior: The mediating and moderating role of knowledge sharing. J. Innov. Knowl. 2022, 7, 100214. [Google Scholar]
- Khanijahani, A.; Iezadi, S.; Dudley, S.; Goettler, M.; Kroetsch, P.; Wise, J. Organizational, professional, and patient characteristics associated with artificial intelligence adoption in healthcare: A systematic review. Health Policy Technol. 2022, 11, 100602. [Google Scholar]
- Hakanen, J.J.; Schaufeli, W.B.; Ahola, K. The Job Demands-Resources model: A three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work. Stress 2008, 22, 224–241. [Google Scholar]
- Badawy, W.; Shaban, M. Exploring geriatric nurses’ perspectives on the adoption of AI in elderly care a qualitative study. Geriatr. Nurs. 2025, 61, 41–49. [Google Scholar] [PubMed]
- Meyers, M.C.; Kooij, D.; Kroon, B.; de Reuver, R.; van Woerkom, M. Organizational support for strengths use, work en-gagement, and contextual performance: The moderating role of age. Appl. Res. Qual. Life 2020, 15, 485–502. [Google Scholar]
- Hassan, M.; Kushniruk, A.; Borycki, E. Barriers to and facilitators of artificial intelligence adoption in health care: Scoping review. JMIR Hum. Factors 2024, 11, e48633. [Google Scholar] [PubMed]
- Venkatesh, V.; Thong, J.Y.; Xu, X. Unified theory of acceptance and use of technology: A synthesis and the road ahead. J. Assoc. Inf. Syst. 2016, 17, 328–376. [Google Scholar] [CrossRef]
- Maleki Varnosfaderani, S.; Forouzanfar, M. The role of AI in hospitals and clinics: Transforming healthcare in the 21st century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef]
- Roppelt, J.S.; Kanbach, D.K.; Kraus, S. Artificial intelligence in healthcare institutions: A systematic literature review on influencing factors. Technol. Soc. 2023, 76, 102443. [Google Scholar]
- Buck, C.; Doctor, E.; Hennrich, J.; Jöhnk, J.; Eymann, T. General practitioners’ attitudes toward artificial intelligence–enabled systems: Interview study. J. Med. Internet Res. 2022, 24, e28916. [Google Scholar]
- Haddad, A.; Habaebi, M.H.; Islam, M.R.; Hasbullah, N.F.; Zabidi, S.A. Systematic review on ai-blockchain based e-healthcare records management systems. IEEE Access 2022, 10, 94583–94615. [Google Scholar]
- Xames, M.D.; Topcu, T.G. A Systematic Literature Review of Digital Twin Research for Healthcare Systems: Research Trends, Gaps, and Realization Challenges. IEEE Access 2024, 12, 4099–4126. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Podsakoff, N.P. Sources of method bias in social science research and recommendations on how to control it. Annu. Rev. Psychol. 2012, 63, 539–569. [Google Scholar]
- Scholze, A.; Hecker, A. The job demands-resources model as a theoretical lens for the bright and dark side of digitization. Comput. Hum. Behav. 2024, 155, 108177. [Google Scholar] [CrossRef]
- Kautish, P.; Siddiqui, M.; Siddiqui, A.; Sharma, V.; Alshibani, S.M. Technology-enabled cure and care: An application of innovation resistance theory to telemedicine apps in an emerging market context. Technol. Forecast. Soc. Change 2023, 192, 122558. [Google Scholar] [CrossRef]
- Edo, O.C.; Ang, D.; Etu, E.E.; Tenebe, I.; Edo, S.; Diekola, O.A. Why do healthcare workers adopt digital health technologies-A cross-sectional study integrating the TAM and UTAUT model in a developing economy. Int. J. Inf. Manag. Data Insights 2023, 3, 100186. [Google Scholar] [CrossRef]
- Fuller, C.M.; Simmering, M.J.; Atinc, G.; Atinc, Y.; Babin, B.J. Common methods variance detection in business research. J. Bus. Res. 2016, 69, 3192–3198. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Bouckenooghe, D.; De Clercq, D.; Naseer, S.; Syed, F. A curvilinear relationship between work engagement and job perfor-mance: The roles of feedback-seeking behavior and personal resources. J. Bus. Psychol. 2022, 37, 353–368. [Google Scholar] [CrossRef]
- Kim, B.J.; Kim, M.J.; Lee, J. Examining the impact of work overload on cybersecurity behavior: Highlighting self-efficacy in the realm of artificial intelligence. Curr. Psychol. 2024, 30, 100704. [Google Scholar] [CrossRef]
- Weinert, C.; Maier, C.; Laumer, S.; Weitzel, T. Repeated IT interruption: Habituation and sensitization of user responses. J. Manag. Inf. Syst. 2022, 39, 187–217. [Google Scholar] [CrossRef]
- Baltaxe, E.; Czypionka, T.; Kraus, M.; Reiss, M.; Askildsen, J.E.; Grenkovic, R.; Lindén, T.S.; Pitter, J.G.; Rutten-van Molken, M.; Solans, O.; et al. Digital health transformation of integrated care in Europe: Overarching analysis of 17 integrated care programs. J. Med. Internet Res. 2019, 21, e14956. [Google Scholar] [CrossRef]
- Salanova, M.; Schaufeli, W.B.; Xanthopoulou, D.; Bakker, A.B. The gain spiral of resources and work engagement: Sustaining a positive worklife. In Work Engagement: A Handbook of Essential Theory and Research; Psychology Press: London, UK, 2010; pp. 118–131. [Google Scholar]
- Li, L.; Ye, F.; Zhan, Y.; Kumar, A.; Schiavone, F.; Li, Y. Unraveling the performance puzzle of digitalization: Evidence from manufacturing firms. J. Bus. Res. 2022, 149, 54–64. [Google Scholar] [CrossRef]
- Schroeder, T.; Dodds, L.; Georgiou, A.; Gewald, H.; Siette, J. Older adults and new technology: Mapping review of the factors associated with older adults’ intention to adopt digital technologies. JMIR Aging 2023, 6, e44564. [Google Scholar] [CrossRef]
- Du Plessis, M. The role of knowledge management in innovation. J. Knowl. Manag. 2007, 11, 20–29. [Google Scholar] [CrossRef]
- Huang, Y.C. Integrated concepts of the UTAUT and TPB in virtual reality behavioral intention. J. Retail. Consum. Serv. 2023, 70, 103127. [Google Scholar] [CrossRef]
- Hobfoll, S.E. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Appl. Psychol. 2001, 50, 337–421. [Google Scholar] [CrossRef]
- Kang, J.Y.; Lee, M.K.; Fairchild, E.M.; Caubet, S.L.; Peters, D.E.; Beliles, G.R.; Matti, L.K. Relationships among organizational values, employee engagement, and patient satisfaction in an academic medical center. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 8–20. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).