AI-Supported Healthcare Technology Resistance and Behavioral Intention: A Serial Mediation Empirical Study on the JD-R Model and Employee Engagement
Abstract
1. Introduction
- What role does the SOR framework play in resistance to AI-supported technologies in healthcare?
- Do job resources and job demands influence healthcare professionals’ AI adoption behavioral intentions toward AI-supported healthcare technologies?
- Does work engagement influence healthcare professionals’ AI adoption behavioral intentions toward AI-supported healthcare technologies?
- Does medical professionals’ resistance to artificial intelligence health care technology increase AI adoption behavioral intentions through the sequential mediation of job resources, job demands, and engagement?
- Does age influence healthcare professionals’ AI adoption behavioral intentions toward AI-supported healthcare technologies?
2. Literature Review
2.1. SOR Framework
2.2. Innovation Resistance Theory (IRT)
2.3. JD-R Model and Employee Engagement
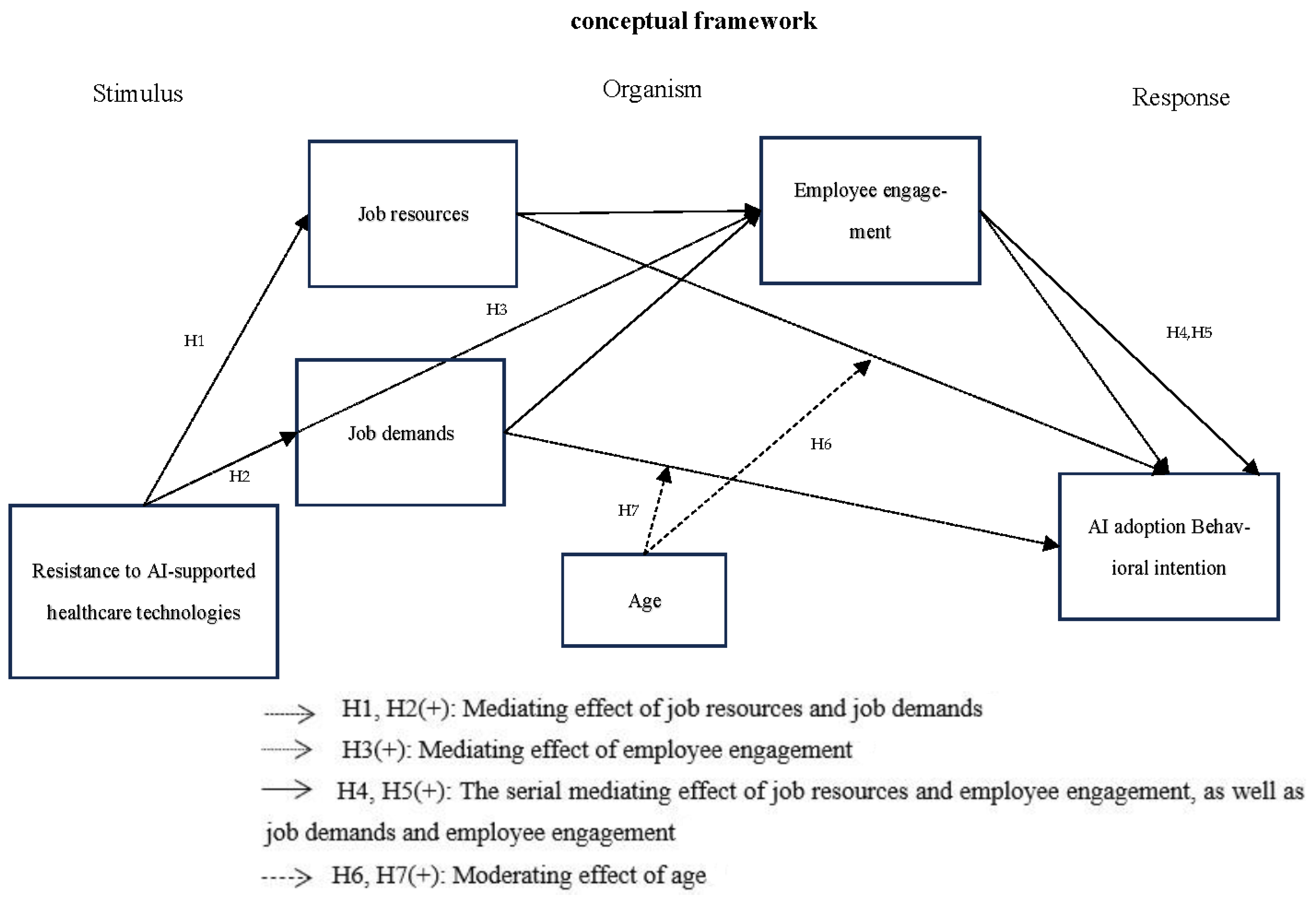
3. Research Model Hypothesis Development
3.1. The Mediating Role of the Job Resources
3.2. The Mediating Role of the Job Demands
3.3. The Mediating Role of the Employee Engagement
3.4. Serial Mediation of the Job Resources, Job Demands and Employee Engagement
3.5. The Moderating Effect of Age
4. Research Methods
5. Results
6. Discussion
- (i)
- The mediating effect of job resources and job demands
- (ii)
- The mediating effect of employee engagement
- (iii)
- The serial mediation of job resources, job demands, and employee engagement
- (iv)
- The moderating effect of age
- (v)
- Theoretical implications
7. Conclusions and Recommendations
- (i)
- Management Implications
- (ii)
- Research Limitations and Directions for Future Research
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A
| Variable | Label | Definition | Source |
|---|---|---|---|
| Independent variable | AI-supported healthcare technologies | Refers to the creation of new knowledge, tools, and ideas using human-like intelligence (e.g., artificial intelligence, including machine learning, deep learning, neural networks, and reinforcement learning) that is programmed to think like humans and imitate their behavior. | Du Plessis, M. (2007) [88] |
| Dependent variable | AI adoption behavioral intention | Behavioral intention refers to an individual’s readiness to adopt AI technology based on perceived benefits, feasibility, and motivation | Huang, Y.C. (2023) [89] |
| Mediator variable | job demands | Job resources refer to job related attributes that positively influence an employee’s work achievement, physical and psychological well-being, and learning and growth; personal resources refer to an individual’s sense of his or her ability to successfully control and impact circumstances. | Hobfoll, 2001 [90] |
| job resources | Job demands refer to job-related characteristics that require significant physical and psychological investment and if overwhelming, hinder performance outcomes. | Hakanen & Roodt, 2010 [51] | |
| employee engagement | Personal engagement, satisfaction, and enthusiasm for work | Kang, J. et al. (2020) [91] |
References
- Del Giudice, M.; Scuotto, V.; Papa, A.; Tarba, S.Y.; Bresciani, S.; Warkentin, M. A self-tuning model for smart manufacturing SMEs: Effects on digital innovation. J. Prod. Innov. Manag. 2021, 38, 68–89. [Google Scholar] [CrossRef]
- Westerman, G.; Bonnet, D.; McAfee, A. Leading Digital: Turning Technology into Business Transformation; Harvard Business Press: Boston, MA, USA, 2014. [Google Scholar]
- Iyanna, S.; Kaur, P.; Ractham, P.; Talwar, S.; Islam, A.N. Digital transformation of healthcare sector. What is impeding adop-tion and continued usage of technology-driven innovations by end-users? J. Bus. Res. 2022, 153, 150–161. [Google Scholar] [CrossRef]
- Kapletia, D.; Phillips, W.; Medcalf, N.; Makatsoris, H.; McMahon, C.; Rich, N. Redistributed manufacturing—Challenges for operations management. Prod. Plan. Control. 2019, 30, 493–495. [Google Scholar] [CrossRef]
- Talwar, S.; Talwar, M.; Tarjanne, V.; Dhir, A. Why retail investors traded equity during the pandemic? An application of artificial neural networks to examine behavioral biases. Psychol. Mark. 2021, 38, 2142–2163. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Sunarti, S.; Rahman, F.F.; Naufal, M.; Risky, M.; Febriyanto, K.; Masnina, R. Artificial intelligence in healthcare: Opportunities and risk for future. Gac. Sanit. 2021, 35, S67–S70. [Google Scholar] [CrossRef]
- Chien, C.F.; Dauzes, S.; Huh, W.T.; Jang, Y.J.; Morrison, J.R. Artificial intelligence in manufacturing and logistics systems: Algorithms, applications, and case studies. Int. J. Prod. Res. 2020, 58, 2730–2731. [Google Scholar] [CrossRef]
- Shankar, A.; Kumar, A.; Yadav, R.; Misra, P.; Pani, S.K. Should I adopt an integrated virtual clinic? A dual-factor theory perspective. J. Consum. Behav. 2024, 23, 357–371. [Google Scholar] [CrossRef]
- Talwar, S.; Dhir, A.; Islam, N.; Kaur, P.; Almusharraf, A. Resistance of multiple stakeholders to e-health innovations: Inte-gration of fundamental insights and guiding research paths. J. Bus. Res. 2023, 166, 114135. [Google Scholar] [CrossRef]
- Webster, P. Virtual health care in the era of COVID-19. Lancet 2020, 395, 1180–1181. [Google Scholar] [CrossRef]
- Talwar, S.; Talwar, M.; Kaur, P.; Dhir, A. Consumers’ resistance to digital innovations: A systematic review and framework development. Australas. Mark. J. 2020, 28, 286–299. [Google Scholar] [CrossRef]
- Woo, Y.; Andres, P.T.C.; Jeong, H.; Shin, C. Classification of diabetic walking through machine learning: Survey targeting senior citizens. In Proceedings of the International Conference on Artificial Intelligence in Information and Communication, Jeju Island, Republic of Korea, 20–23 April 2021; pp. 435–437. [Google Scholar]
- Deebak, B.D.; Al-Turjman, F. Smart mutual authentication protocol for cloud based medical healthcare systems using internet of medical things. IEEE J. Sel. Areas Commun. 2021, 39, 346–360. [Google Scholar]
- Kaur, A.; Garg, R.; Gupta, P. Challenges facing AI and big data for resource poor healthcare system. In Proceedings of the 2nd International Conference on Electronics and Sustainable Communication Systems, Coimbatore, India, 4–6 August 2021; pp. 1426–1433. [Google Scholar]
- Mitchell, M.; Kan, L. Digital technology and the future of health systems. Health Syst. Reform 2019, 5, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, S.; Gandhi, C. Capability-based access control with trust for effective healthcare systems. Int. J. Cloud Appl. Comput. 2022, 12, 1–28. [Google Scholar] [CrossRef]
- Kumari, P.; Shankar, A.; Behl, A.; Pereira, V.; Yahiaoui, D.; Laker, B.; Gupta, B.B.; Arya, V. Investigating the barriers towards adoption and implementation of open innovation in healthcare. Technol. Forecast. Soc. Change 2024, 200, 123100. [Google Scholar] [CrossRef]
- Chong, A.Y.L.; Blut, M.; Zheng, S. Factors influencing the acceptance of healthcare information technologies: A meta-analysis. Inf. Manag. 2022, 59, 103604. [Google Scholar] [CrossRef]
- Jacoby, J. Stimulus-organism-response reconsidered: An evolutionary step in modeling (consumer) behavior. J. Consum. Psychol. 2002, 12, 51–57. [Google Scholar] [CrossRef]
- Chakraborty, D.; Singu, H.B.; Kar, A.K.; Biswas, W. From fear to faith in the adoption of medicine delivery application: An integration of SOR framework and IRT theory. J. Bus. Res. 2023, 166, 114140. [Google Scholar]
- Demerouti, E.; Bakker, A.B. The job demands-resources model: Challenges for future research. SA J. Ind. Psychol. 2011, 37, 1–9. [Google Scholar]
- Anjum, A.; Zhao, Y. The impact of stress on innovative work behavior among medical healthcare professionals. Behav. Sci. 2022, 12, 340. [Google Scholar] [CrossRef]
- Koroglu, Ş.; Ozmen, O. The mediating effect of work engagement on innovative work behavior and the role of psychological well-being in the job demands–resources (JD-R) model. Asia-Pac. J. Bus. Adm. 2022, 14, 124–144. [Google Scholar]
- Shuck, B.; Adelson, J.L.; Reio, T.G., Jr. The employee engagement scale: Initial evidence for construct validity and implications for theory and practice. Hum. Resour. Manag. 2017, 56, 953–977. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Perhoniemi, R.; Toppinen-Tanner, S. Positive gain spirals at work: From job resources to work engagement, personal initiative and work-unit innovativeness. J. Vocat. Behav. 2008, 73, 78–91. [Google Scholar]
- Kwon, K.; Kim, T. An integrative literature review of employee engagement and innovative behavior: Revisiting the JD-R model. Hum. Resour. Manag. Rev. 2020, 30, 100704. [Google Scholar]
- Shamsi, M.; Iakovleva, T.; Olsen, E.; Bagozzi, R.P. Employees’ work-related well-being during COVID-19 pandemic: An integrated perspective of technology acceptance model and JD-R theory. Int. J. Environ. Res. Public Health 2021, 18, 11888. [Google Scholar] [CrossRef]
- Lee, C.H.; Chen CW, D.; Huang, S.F.; Chang, Y.T.; Demirci, S. Exploring consumers’ impulse buying behavior on online apparel websites: An empirical investigation on consumer perceptions. Int. J. Electron. Commer. Stud. 2021, 12, 119–142. [Google Scholar]
- Kaur, P.; Dhir, A.; Singh, N.; Sahu, G.; Almotairi, M. An innovation resistance theory perspective on mobile payment solutions. J. Retail. Consum. Serv. 2020, 55, 102059. [Google Scholar] [CrossRef]
- Talwar, S.; Dhir, A.; Khalil, A.; Mohan, G.; Islam AK, M.N. Point of adoption and beyond. Initial trust and mobile-payment continuation intention. J. Retail. Consum. Serv. 2020, 55, 102086. [Google Scholar]
- Mehrabian, A.; Russell, J.A. An Approach to Environmental Psychology; The MIT Press: Cambridge, MA, USA, 1974. [Google Scholar]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, e000101. [Google Scholar] [CrossRef]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar]
- Zou, X.; Na, Y.; Lai, K.; Liu, G. Unpacking public resistance to health Chatbots: A parallel mediation analysis. Front. Psychol. 2024, 15, 1276968. [Google Scholar] [CrossRef] [PubMed]
- Ye, T.; Xue, J.; He, M.; Gu, J.; Lin, H.; Xu, B.; Cheng, Y. Psychosocial factors affecting artificial intelligence adoption in health care in China: Cross-sectional study. J. Med. Internet Res. 2019, 21, e14316. [Google Scholar] [CrossRef] [PubMed]
- Jarrahi, M.H. Artificial intelligence and the future of work: Human-AI symbiosis in organizational decision making. Bus. Horiz. 2018, 61, 577–586. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Stocchi, L.; Pourazad, N.; Michaelidou, N.; Tanusondjaja, A.; Harrigan, P. Marketing research on Mobile apps: Past, present and future. J. Acad. Mark. Sci. 2022, 50, 195–225. [Google Scholar] [CrossRef]
- Bhandari, U.; Neben, T.; Chang, K.; Chua, W.Y. Effects of interface design factors on affective responses and quality evalua-tions in mobile applications. Comput. Hum. Behav. 2017, 72, 525–534. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Balakrishnan, J.; Das, R.; Dutot, V. Resistance to innovation: A dynamic capability model based enquiry into retailers’ resistance to blockchain adaptation. J. Bus. Res. 2023, 157, 113632. [Google Scholar] [CrossRef]
- Ram, S.; Sheth, J.N. Consumer resistance to innovations: The marketing problem and its solutions. J. Consum. Mark. 1989, 6, 5–14. [Google Scholar] [CrossRef]
- Heidenreich, S.; Handrich, M. What about passive innovation resistance? Investigating adoption-related behavior from a resistance perspective. J. Prod. Innov. Manag. 2015, 32, 878–903. [Google Scholar] [CrossRef]
- Chen, H.S.; Tsai, B.K.; Hsieh, C.M. The effects of perceived barriers on innovation resistance of hydrogen-electric motorcycles. Sustainability 2018, 10, 1933. [Google Scholar] [CrossRef]
- Sadiq, M.; Adil, M.; Paul, J. An innovation resistance theory perspective on purchase of eco-friendly cosmetics. J. Retail. Consum. Serv. 2021, 59, 102369. [Google Scholar] [CrossRef]
- Khalil, A.; Shankar, A.; Bodhi, R.; Behl, A.; Ferraris, A. Why do people resist drone food delivery services? An innovation resistance theory perspective. IEEE Trans. Eng. Manag. 2022, 71, 13038–13048. [Google Scholar] [CrossRef]
- Chen, P.T.; Lin, C.L.; Wu, W.N. Big data management in healthcare: Adoption challenges and implications. Int. J. Inf. Manag. 2020, 53, 102078. [Google Scholar] [CrossRef]
- Tsai, J.M.; Cheng, M.J.; Tsai, H.H.; Hung, S.W.; Chen, Y.L. Acceptance and resistance of telehealth: The perspective of du-al-factor concepts in technology adoption. Int. J. Inf. Manag. 2019, 49, 34–44. [Google Scholar] [CrossRef]
- Galanakis, M.D.; Tsitouri, E. Positive psychology in the working environment. Job demands-resources theory, work en-gagement and burnout: A systematic literature review. Front. Psychol. 2022, 13, 1022102. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job demands–resources theory: Taking stock and looking forward. J. Occup. Health Psychol. 2017, 22, 273. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Roodt, G. Using the job demands-resources model to predict engagement: Analyzing a conceptual model. In Work Engagement: A Handbook of Essential Theory and Research; Bakker, A.B., Leiter, M.P., Eds.; Psychology Press: New York, NY, USA, 2010; pp. 85–101. [Google Scholar]
- Yang, Y.; Ngai, E.W.; Wang, L. Resistance to artificial intelligence in health care: Literature review, conceptual framework, and research agenda. Inf. Manag. 2024, 61, 103961. [Google Scholar] [CrossRef]
- Kahn, W.A. Psychological conditions of personal engagement and disengagement at work. Acad. Manag. J. 1990, 33, 692–724. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Salanova, M.; González-Romá, V.; Bakker, A.B. The measurement of engagement and burnout: A two sample confirmatory factor analytic approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Achananuparp, P. Perceptions and needs of artificial intelligence in health care to increase adoption: Scoping review. J. Med. Internet Res. 2022, 24, e32939. [Google Scholar] [CrossRef]
- Rich, B.L.; LePine, J.A.; Crawford, E.R. Job engagement: Antecedents and effects on job performance. Acad. Manag. J. 2010, 53, 617–635. [Google Scholar]
- Tims, M.; Bakker, A.B.; Derks, D. Development and validation of the job crafting scale. J. Vocat. Behav. 2012, 80, 173–186. [Google Scholar]
- Kim, W.; Kolb, J.A.; Kim, T. The Relationship between work engagement and performance: A review of empirical literature and a proposed research agenda. Hum. Resour. Dev. Rev. 2013, 12, 248–276. [Google Scholar]
- Wang, W.; Chen, L.; Xiong, M.; Wang, Y. Accelerating AI adoption with responsible AI signals and employee engagement mechanisms in health care. Inf. Syst. Front. 2023, 25, 2239–2256. [Google Scholar] [CrossRef]
- Paul, P.; Singh, B. Healthcare employee engagement using the internet of things: A systematic overview. Adopt. Eff. Artif. Intell. Hum. Resour. Manag. 2023, Part A, 71–97. [Google Scholar]
- Gürbüz, S.; Schaufeli, W.B.; Freese, C.; Brouwers, E.P. Fueling creativity: HR practices, work engagement, personality, and autonomy. Int. J. Hum. Resour. Manag. 2024, 35, 3770–3799. [Google Scholar]
- Rosyafah, S.; Pudjowati, J. What are the Key Determinants of Human Resource Management Effectiveness in Enhancing Organizational Financial Performance? Atestasi J. Ilm. Akunt. 2024, 7, 525–560. [Google Scholar] [CrossRef]
- Rafique, M.A.; Hou, Y.; Chudhery MA, Z.; Waheed, M.; Zia, T.; Chan, F. Investigating the impact of pandemic job stress and transformational leadership on innovative work behavior: The mediating and moderating role of knowledge sharing. J. Innov. Knowl. 2022, 7, 100214. [Google Scholar]
- Khanijahani, A.; Iezadi, S.; Dudley, S.; Goettler, M.; Kroetsch, P.; Wise, J. Organizational, professional, and patient characteristics associated with artificial intelligence adoption in healthcare: A systematic review. Health Policy Technol. 2022, 11, 100602. [Google Scholar]
- Hakanen, J.J.; Schaufeli, W.B.; Ahola, K. The Job Demands-Resources model: A three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work. Stress 2008, 22, 224–241. [Google Scholar]
- Badawy, W.; Shaban, M. Exploring geriatric nurses’ perspectives on the adoption of AI in elderly care a qualitative study. Geriatr. Nurs. 2025, 61, 41–49. [Google Scholar] [PubMed]
- Meyers, M.C.; Kooij, D.; Kroon, B.; de Reuver, R.; van Woerkom, M. Organizational support for strengths use, work en-gagement, and contextual performance: The moderating role of age. Appl. Res. Qual. Life 2020, 15, 485–502. [Google Scholar]
- Hassan, M.; Kushniruk, A.; Borycki, E. Barriers to and facilitators of artificial intelligence adoption in health care: Scoping review. JMIR Hum. Factors 2024, 11, e48633. [Google Scholar] [PubMed]
- Venkatesh, V.; Thong, J.Y.; Xu, X. Unified theory of acceptance and use of technology: A synthesis and the road ahead. J. Assoc. Inf. Syst. 2016, 17, 328–376. [Google Scholar] [CrossRef]
- Maleki Varnosfaderani, S.; Forouzanfar, M. The role of AI in hospitals and clinics: Transforming healthcare in the 21st century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef]
- Roppelt, J.S.; Kanbach, D.K.; Kraus, S. Artificial intelligence in healthcare institutions: A systematic literature review on influencing factors. Technol. Soc. 2023, 76, 102443. [Google Scholar]
- Buck, C.; Doctor, E.; Hennrich, J.; Jöhnk, J.; Eymann, T. General practitioners’ attitudes toward artificial intelligence–enabled systems: Interview study. J. Med. Internet Res. 2022, 24, e28916. [Google Scholar]
- Haddad, A.; Habaebi, M.H.; Islam, M.R.; Hasbullah, N.F.; Zabidi, S.A. Systematic review on ai-blockchain based e-healthcare records management systems. IEEE Access 2022, 10, 94583–94615. [Google Scholar]
- Xames, M.D.; Topcu, T.G. A Systematic Literature Review of Digital Twin Research for Healthcare Systems: Research Trends, Gaps, and Realization Challenges. IEEE Access 2024, 12, 4099–4126. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Podsakoff, N.P. Sources of method bias in social science research and recommendations on how to control it. Annu. Rev. Psychol. 2012, 63, 539–569. [Google Scholar]
- Scholze, A.; Hecker, A. The job demands-resources model as a theoretical lens for the bright and dark side of digitization. Comput. Hum. Behav. 2024, 155, 108177. [Google Scholar] [CrossRef]
- Kautish, P.; Siddiqui, M.; Siddiqui, A.; Sharma, V.; Alshibani, S.M. Technology-enabled cure and care: An application of innovation resistance theory to telemedicine apps in an emerging market context. Technol. Forecast. Soc. Change 2023, 192, 122558. [Google Scholar] [CrossRef]
- Edo, O.C.; Ang, D.; Etu, E.E.; Tenebe, I.; Edo, S.; Diekola, O.A. Why do healthcare workers adopt digital health technologies-A cross-sectional study integrating the TAM and UTAUT model in a developing economy. Int. J. Inf. Manag. Data Insights 2023, 3, 100186. [Google Scholar] [CrossRef]
- Fuller, C.M.; Simmering, M.J.; Atinc, G.; Atinc, Y.; Babin, B.J. Common methods variance detection in business research. J. Bus. Res. 2016, 69, 3192–3198. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Bouckenooghe, D.; De Clercq, D.; Naseer, S.; Syed, F. A curvilinear relationship between work engagement and job perfor-mance: The roles of feedback-seeking behavior and personal resources. J. Bus. Psychol. 2022, 37, 353–368. [Google Scholar] [CrossRef]
- Kim, B.J.; Kim, M.J.; Lee, J. Examining the impact of work overload on cybersecurity behavior: Highlighting self-efficacy in the realm of artificial intelligence. Curr. Psychol. 2024, 30, 100704. [Google Scholar] [CrossRef]
- Weinert, C.; Maier, C.; Laumer, S.; Weitzel, T. Repeated IT interruption: Habituation and sensitization of user responses. J. Manag. Inf. Syst. 2022, 39, 187–217. [Google Scholar] [CrossRef]
- Baltaxe, E.; Czypionka, T.; Kraus, M.; Reiss, M.; Askildsen, J.E.; Grenkovic, R.; Lindén, T.S.; Pitter, J.G.; Rutten-van Molken, M.; Solans, O.; et al. Digital health transformation of integrated care in Europe: Overarching analysis of 17 integrated care programs. J. Med. Internet Res. 2019, 21, e14956. [Google Scholar] [CrossRef]
- Salanova, M.; Schaufeli, W.B.; Xanthopoulou, D.; Bakker, A.B. The gain spiral of resources and work engagement: Sustaining a positive worklife. In Work Engagement: A Handbook of Essential Theory and Research; Psychology Press: London, UK, 2010; pp. 118–131. [Google Scholar]
- Li, L.; Ye, F.; Zhan, Y.; Kumar, A.; Schiavone, F.; Li, Y. Unraveling the performance puzzle of digitalization: Evidence from manufacturing firms. J. Bus. Res. 2022, 149, 54–64. [Google Scholar] [CrossRef]
- Schroeder, T.; Dodds, L.; Georgiou, A.; Gewald, H.; Siette, J. Older adults and new technology: Mapping review of the factors associated with older adults’ intention to adopt digital technologies. JMIR Aging 2023, 6, e44564. [Google Scholar] [CrossRef]
- Du Plessis, M. The role of knowledge management in innovation. J. Knowl. Manag. 2007, 11, 20–29. [Google Scholar] [CrossRef]
- Huang, Y.C. Integrated concepts of the UTAUT and TPB in virtual reality behavioral intention. J. Retail. Consum. Serv. 2023, 70, 103127. [Google Scholar] [CrossRef]
- Hobfoll, S.E. The influence of culture, community, and the nested-self in the stress process: Advancing conservation of resources theory. Appl. Psychol. 2001, 50, 337–421. [Google Scholar] [CrossRef]
- Kang, J.Y.; Lee, M.K.; Fairchild, E.M.; Caubet, S.L.; Peters, D.E.; Beliles, G.R.; Matti, L.K. Relationships among organizational values, employee engagement, and patient satisfaction in an academic medical center. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 8–20. [Google Scholar] [CrossRef]

| Demographic Category | Items | Sample Size (N = 296) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 170 | 57.2% |
| Female | 126 | 42.6% | |
| Age | Age 55 or below (inclusive) | 151 | 51% |
| Age 56 or above (inclusive) | 145 | 49% | |
| Education level | University | 197 | 66.6% |
| Graduate school | 99 | 33.4% | |
| Job role | Doctor | 109 | 35.9% |
| Registered nurse | 103 | 33.9% | |
| Pharmacist | 84 | 27.6% |
| Cronbach’s α | CR | Job Resources | Job Demands | Employee Engagement | Resistance to Innovation | AI Adoption Behavioral Intentions | |
|---|---|---|---|---|---|---|---|
| Job resources | 0.869 | 0.945 | (0.773) | ||||
| job demands | 0.945 | 0.949 | 0.536 | (0.823) | |||
| Employee engagement | 0.934 | 0.955 | 0.587 | 0.349 | (0.850) | ||
| Resistance to innovation | 0.911 | 0.928 | 0.483 | 0.459 | 0.489 | (0.798) | |
| AI adoption Behavioral intentions | 0.955 | 0.967 | 0.492 | 0.445 | 0.564 | 0.358 | (0.88) |
| Job Resources | Employee Engagement | Behavioral Intention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictive Factor | B | SE | LLCI | ULCI | B | SE | LLCI | ULCI | B | SE | LLCI | ULCI |
| Resistance to AI-supported healthcare technologies | 0.48 | 0.54 | 0.4 | 0.62 | 0.26 | 0.6 | 0.19 | 0.43 | 0.048 | 0.07 | −0.08 | 0.20 |
| Job resources | 0.45 | 0.56 | 0.39 | 0.61 | 0.23 | 0.07 | 0.13 | 0.42 | ||||
| Employee engagement | 0.4 | 0.06 | 0.32 | 0.58 | ||||||||
| Direct effect | B | SE | LLCI | ULCI | ||||||||
| Direct effect: | ||||||||||||
| Resistance to AI-supported healthcare technologies → Behavioral intentions | 0.35 | 0.07 | 0.32 | 0.6 | ||||||||
| Indirect effect | ||||||||||||
| Indirect effect 1: Resistance to AI-supported healthcare technologies → Job resources → AI adoption behavioral intentions | 0.14 | 0.04 | 0.05 | 0.24 | ||||||||
| Indirect effect 2: Resistance to AI-supported healthcare technologies → Employee engagement → AI adoption behavioral intentions | 0.14 | 0.03 | 0.07 | 0.21 | ||||||||
| Indirect effect 3: Resistance to AI-supported healthcare technologies → Job resources → Employee engagement → AI adoption behavioral intentions | 0.11 | 0.02 | 0.06 | 0.18 | ||||||||
| Job Demands | Employee Engagement | Behavioral Intention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictive Factor | B | SE | LLCI | ULCI | B | SE | LLCI | ULCI | B | SE | LLCI | ULCI |
| Resistance to AI-supported healthcare technologies | 0.45 | 0.79 | 0.54 | 0.86 | 0.41 | 0.06 | 0.35 | 0.61 | 0.0008 | 0.07 | −0.14 | 0.14 |
| Job demands | 0.15 | 0.04 | 0.03 | 0.2 | 0.28 | 0.04 | 0.15 | 0.32 | ||||
| Employee engagement | 0.46 | 0.05 | 0.4 | 0.63 | ||||||||
| Direct effect: | B | SE | LLCI | ULCI | ||||||||
| Direct effect: | ||||||||||||
| Resistance to AI-supported healthcare technologies → AI adoption behavioral intentions | 0.35 | 0.07 | 0.32 | 0.6 | ||||||||
| Indirect effect | ||||||||||||
| Indirect effect 1: Resistance to AI-supported healthcare technologies → Job demands → AI adoption behavioral intentions | 0.12 | 0.03 | 0.07 | 0.18 | ||||||||
| Indirect effect 2: Resistance to AI-supported healthcare technologies → Employee engagement → AI adoption Behavioral intentions | 0.19 | 0.03 | 0.12 | 0.27 | ||||||||
| Indirect effect 3: Resistance to AI-supported healthcare technologies → Job demands → Employee engagement → AI adoption behavioral intentions | 0.03 | 0.01 | 0.05 | 0.06 | ||||||||
| Moderating Factor: Age | ||||
| Path | B | SE | LLCI | ULCI |
| Resistance to AI-supported healthcare technologies → Job resources → AI adoption behavioral intentions | −0.093 | 0.067 | −0.23 | 0.031 |
| Resistance to AI-supported healthcare technologies → Job demands → AI adoption behavioral intentions | −0.158 | 0.07 | −0.297 | −0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuang, L.-M.; Huang, S.-H. AI-Supported Healthcare Technology Resistance and Behavioral Intention: A Serial Mediation Empirical Study on the JD-R Model and Employee Engagement. Systems 2025, 13, 268. https://doi.org/10.3390/systems13040268
Chuang L-M, Huang S-H. AI-Supported Healthcare Technology Resistance and Behavioral Intention: A Serial Mediation Empirical Study on the JD-R Model and Employee Engagement. Systems. 2025; 13(4):268. https://doi.org/10.3390/systems13040268
Chicago/Turabian StyleChuang, Li-Min, and Sheng-Hsuan Huang. 2025. "AI-Supported Healthcare Technology Resistance and Behavioral Intention: A Serial Mediation Empirical Study on the JD-R Model and Employee Engagement" Systems 13, no. 4: 268. https://doi.org/10.3390/systems13040268
APA StyleChuang, L.-M., & Huang, S.-H. (2025). AI-Supported Healthcare Technology Resistance and Behavioral Intention: A Serial Mediation Empirical Study on the JD-R Model and Employee Engagement. Systems, 13(4), 268. https://doi.org/10.3390/systems13040268




