Abstract
Health information systems (HISs) are instrumental in improving the efficiency and effectiveness of hospital operations, from managing patient data to enhancing decision-making processes. This study, which holds significant implications for the healthcare industry, aimed to identify the factors that influence users’ intentions to use HISs. The research involved interviews with healthcare professionals licensed to use the HIS of a public hospital. The survey, conducted in 2020, received 113 responses. Statistical methods of descriptive analysis, correlation, and multiple linear regression were used. Two models were examined. The first model investigated the relationship between the dependent variable of the intention to use an HIS and the independent variables of perceived time savings and perceived privacy protection. The second model explored the impact of age and education as control variables in the connection between the intention to use an HIS and time savings and privacy protection. A significant moderate positive correlation was found between the intention to use an HIS and perceived time savings, while a significant weak positive correlation was detected between the intention to use an HIS and education. Regression analysis in the first model revealed a significant connection between the intention to use an HIS and perceived time savings. However, the perceived privacy protection variable did not show a significant relationship with the dependent variable. The second model showed statistical significance in the relationship between the intention to use an HIS and education, but not with the second control variable, age. It can be concluded that education strengthens the positive impact of perceived time savings on the intention to use a health information system (HIS), a finding that has immediate and practical implications for healthcare professionals and researchers in the field of health information systems and healthcare management, underlining the importance of this research in advancing the understanding and adoption of HISs in healthcare settings.
1. Introduction
Technological progress has transformed hospital operations, especially as hospitals have increasingly required information systems that meet both medical and administrative needs in a straightforward, digital manner, increasing the efficiency of hospital management [1,2]. For that purpose, many hospitals, polyclinics, and other health institutions use a hospital information system (HIS) to support the medical diagnostics, care, and treatment of patients, along with invoicing services provided to users of the system [3]. In addition, HISs are used to monitor work, the consumption of drugs and materials, and procurement efficiency, and to conduct other management tasks. HISs enable efficient management, rational use of pharmaceuticals and consumables, streamlined and automated administration, a reduction in the number of non-medical staff needed, direct inclusion in international medical databases, facilitated professional and scientific work based on comprehensive patient data, and telemedicine connections between clinical institutions [1]. Moreover, enhancing the hospital system with digital advancements boosts employees’ confidence and motivation, fosters a sense of modern and efficient operation, and instils vital confidence in both patients and the wider community [4], leading to more efficient interorganizational alliances undergoing digitalisation [5].
Furthermore, the development of the HIS has become an important tool for building the reputation of hospitals, retaining existing ones, and attracting new employees [6]. The trust that patients or users of the HIS have in such a system is a very important determinant of the implementation itself, and thus, the intention to use it. This is reflected in the importance of protecting the privacy of user information, which the system should ensure in its operation. In this way, trust is built, which later enables an ever-increasing intention to use the HIS and, ultimately, the frequency of using it.
Finally, the HIS has an important function in rationalising resources and managing the hospital’s staff, thus supporting the efficiency of the hospital’s management in managing and organising the business. This certainly affects the system’s productivity, which results in significant time savings [7,8].
Over the past decade, research models such as the Technology Acceptance Model (TAM) have identified key factors influencing the adoption of information technologies in healthcare, including perceived usefulness, ease of use, and data confidentiality [9,10]. However, the TAM’s predictive power is debated due to socio-organizational and cultural influences [11]. Importantly, perceived privacy and security are critical determinants of HIS adoption, directly impacting user trust [12,13]. Perceived time savings are a vital factor, as they can streamline processes and reduce the time required for administrative tasks, thus enhancing productivity and allowing healthcare workers to focus on more complex activities [14,15]. At the same time, age and education significantly impact the use of HISs. Younger users and those with higher education levels tend to adopt the HIS more readily due to greater familiarity with technology and higher comfort levels with navigating digital systems [16]. Conversely, older adults and those with lower educational attainment may face barriers to HIS adoption, often requiring additional training and support to build confidence and proficiency in using these systems [17].
For the above reasons, in our work, we focus on perceived time savings and perceived privacy as the determinants of the intention to use an HIS. Therefore, the objectives of this study are as follows: (1) to examine the relationship between the user’s perception of time savings and the intention to use an HIS, (2) to examine the relationship between perceived privacy protection and the intention to use an HIS, (3) to examine the impact of age and education to the intention to use an HIS, and (4) to investigate if age and education strengthen the positive impact of perceived time savings on the intention to use a health information system (HIS). To investigate these relationships, a survey of the sample of HIS users in one public hospital was conducted. Research instruments were used to measure the perceived time savings, perceived privacy protection, and intention to use an HIS. The validity and reliability of the research instrument were tested using confirmatory factor analysis and Cronbach’s alpha. The relationship between the examined variables was tested using regression analysis. Results indicated that the perceived time savings and educational level of the users positively impact their intent to use an HIS.
The paper is organised as follows. After the introduction, a literature review is given, with a focus on the factors influencing the intention to use an HIS. The research model is elaborated in the Section 3 of the study, focusing on developing the research propositions (RPs). The research methodology is presented in the Section 4 of the study, starting with the presentation of the research instrument and data collection, followed by a detailed description of the data analysis. The results section (Section 5) begins with a validity and reliability analysis and then focuses on model fit assessment and research proposition testing. The Section 6 presents the study’s conclusion, with its theoretical and practical contributions.
2. Literature Review
2.1. Hospital Information Systems
Nowadays, most sectors struggle with the design and maintenance of technological tools [18], including the health sector. HISs significantly enhance the efficiency, accuracy, and quality of healthcare delivery by integrating various administrative and clinical functions. Therefore, the adoption of HISs is indispensable in modern healthcare. An HIS can consist of several modules, with extensions depending on which specialised hospital activity is performed [19]. The most common specialised HIS implementations are radiology information systems, laboratory information systems, policy and procedure management systems, and picture archiving and communication systems [20]. There are many ways in which the HIS ensures internal and external communication between healthcare providers; hence, portable devices such as tablets and smartphones can be used at the hospital bedside.
To plan and make sure that the workforce is fully supported and equipped with the required tools, equipment, resources, and policies to deliver services, health systems need high-quality data from the HIS [6,21]. In terms of program creation and improvement, policy formation, strategic planning, or advocacy, available data are frequently underutilised. The process’s breakdown is partially attributable to HISs’ intrinsic complexity and the fact that their outputs are not immediately related to better service delivery. For instance, increases in the quality of services and coverage are strongly tied to advances in the health workforce, while better information systems produce better-quality and more timely data [21].
A breakdown in the causal pathway and underuse of data in decision making are both caused by the complexity of how hospitals use and contribute to HISs, including the decision-making process, information flow, the delay between data availability and use, and eventual changes in services and health outcomes [22]. By including all staff, clinical and non-clinical, in the tasks of managing and overseeing the various activities of the hospital, the implementation of new information systems in the hospital represents a potential method of changing the “de facto” power structure into a different, more formal type of power structure [7,23]. Information control is sometimes used to legitimise and maintain the power structures that exist in an organisation [24]. Hospitals are being forced to abandon their conventional forms and methods to focus on integrating information technology into all aspects of their operations and services due to the high demand for ever-more-complex goods and services [8,25].
Under the digital transformation of the healthcare system, the physical interaction between the patient and the healthcare worker becomes less important [26]. For that reason, health systems require quality data from the HIS to plan and ensure that the workforce is fully funded and equipped with the necessary commodities, infrastructure, resources, and policies to deliver services [27]. In that direction, the benefits of the HIS are mainly referring to the provision of a common source of information about the patient’s health history [28]. Therefore, one of the most important functions of HISs is the protection and control of the data that are stored, which improves the ability of all healthcare professionals to better coordinate the process of providing information about the patient’s health status and history. At the same time, all the information about the patients becomes vulnerable to the common information security risk. Therefore, better data privacy protection influences the decision or intention to use it [13].
The potential advantages of an HIS based on its implementation may include more efficient management of resources; first of all, this means saving time, finances, and materials and strengthening the distribution capacity in exchange for medical assistance [29]. Time rationalisation is a key factor influencing the intention to use an HIS. It ensures the management of the time needed to perform a specific activity and organisation for other business tasks [15]. However, the impact of information systems on administrative tasks in public organisations can be both positive and negative. On the positive side, these systems streamline processes, reduce errors, and enhance productivity, particularly in routine tasks [30]. They improve service delivery by making data more accessible and processes more efficient [31]. However, the initial implementation can increase administrative workload due to the need for staff training and system adjustments [32]. Thus, while they offer long-term efficiency, they may temporarily increase administrative burdens [33].
Finally, the hospital system is the most intricately organised and managed component of the entire healthcare system. As a result, it takes up the biggest portion of the overall healthcare budget. Hospitals aim to establish an HIS to provide accurate, timely, comprehensive, and conveniently accessible information in an integrated manner [34]. The HIS enables the effective provision of data on patients’ health information to enable better healthcare decisions [35].
2.2. Determinants of Intention to Use HIS
Over the past 10 years, several research models have been developed to identify the determinants of user acceptance of information technologies in healthcare [9, 36].
The Technology Acceptance Model (TAM) has been widely used to understand the adoption of information systems in healthcare settings. Studies have identified factors such as data confidentiality, perceived usefulness, ease of use, and quality of the system as key influencers of information systems in healthcare adoption [10]. However, the predictive capabilities of the TAM in healthcare have been questioned, with socio-organizational and cultural factors also playing a significant role [11]. Despite its limitations, the TAM has been found to predict a substantial portion of information systems in healthcare use, and its application in specific healthcare contexts has been recommended [37]. The model has been extended to fit dynamic health service environments, with variables such as subjective norms and self-efficacy being added [9]. Other factors influencing the adoption of health information technologies include ease of use, usefulness, social impact, and the attitudes and behaviour of users [38]. The importance of e-collaboration services in healthcare and the need for a new model to explain their adoption has also been highlighted [39]. Lastly, a modified version of the TAM has been proposed to better understand health professionals’ support for information systems in healthcare, with perceived ease of use and relevance being key predictors [40].
One of the essential elements of the TAM is perceived ease of use. From the aspect of the health system, perceived ease of use, simplicity, and the variety of features and products offered have a positive impact on the perceived value to users [14]. Simplicity and ease of use are important because they ensure that the time and effort required to manage finances are kept to a minimum [15,41]. By itself, simplicity in use leads to rationalisation of time, i.e., the productivity of work, which is connected with saving time when using the HIS and the possibility for healthcare workers to focus more on more complex processes. To our knowledge, we are not aware of research investigating the relationship between time savings and intention to use an HIS, although time is the most critical element in hospital management due not only to the shortage of staff, but also the nature of the work, which often is characterised by a health crisis in which timely actions are vital for the benefit of the patient.
The adoption of new technologies should consider the estimated cost, risk, benefits, and compliance [7,42]. Some studies show that security and risk issues are some of the main concerns that clients feel towards HISs and harm the intention to use the HIS. Potentially greater security creates trust in HISs, leading to greater user perception of the protection of patients’ private data in healthcare facilities [12]. The security of the service is crucial for users, and the perception of risk and security becomes an important feature that affects the intention of HIS use [13].
Perceived privacy is a crucial determinant of the intention to use an HIS. Privacy concerns are paramount in healthcare due to the sensitive nature of patient data. When users feel confident that their personal and medical information is secure, they are more likely to adopt and utilise the HIS [12,13]. Studies have shown that perceived privacy directly impacts trust in the system, which in turn influences the intention to use the HIS. Users’ belief in the system’s ability to protect their information from unauthorised access and breaches increases their willingness to engage with the system [43,44]. Furthermore, ensuring robust privacy measures can mitigate fears and resistance towards the adoption of new technologies in healthcare settings. Therefore, healthcare providers must prioritise privacy features in HISs to foster user acceptance and trust [45].
For the above reasons, in the research proposition development section (Section 3) following, we focus on perceived time savings and perceived privacy.
3. Research Proposition Development
HIS services are crucial for optimising patient care, improving efficiency, ensuring data security and privacy, complying with regulations, and ultimately, enhancing the overall healthcare experience for both healthcare professionals and patients [34]. Hospitals need to align their HIS modules with the specific needs and objectives of their users, resulting in better healthcare outcomes.
For this research, a model was constructed according to determinants from the set factors of trust and perceived ease of use, which, according to previous findings, have a significant influence on the intention to use an HIS. However, in our work, we focus on perceived time-spending as a specific aspect of perceived ease of use and on perceived privacy protection as a specific aspect of perceived trust. The perceived time savings refers to the ease of using the HIS due to the rationalisation of time, i.e., the effect of reducing the time required to perform a specific activity using the HIS [41]. Information systems, on the one hand, save time because they shorten and simplify several processes, such as patient registration. However, on the other hand, they may increase the time needed for administrative tasks [30]. Furthermore, privacy protection is a security factor that affects the trust in the HIS, which can increase the intention to use the system itself [12].
In this research, an attempt is made to set up a model that aims to determine the influence of perceived timesaving in hospital services and privacy protection factors in the intention of using the HIS. Moreover, we compare the strength and reliability of the influence of both variables by inserting the influence of education and the age of the user.
3.1. Time Savings
Digital technology has the effect of saving valuable time by facilitating documentation and reducing repetitive tasks through automation [46]. Healthcare professionals gain important value from timesaving impacts in hospital services, which also help to deliver healthcare more effectively, lower costs, improve patient outcomes, and boost staff satisfaction [47]. The perception of HIS users, which is the result of the simpler and easier use of more sophisticated systems, achieves great rationalisation of time when organising and managing business activities. In this way, the effect of a greater intention to use the HIS is created [15,41]. On the other hand, higher time demands placed on physicians reduce their use of the HIS and heighten their resistance, which reduces the likelihood of attaining quality improvement [30]. This is why initial time-spending is regarded as a significant barrier to obtaining advantages. Instead of focusing on their work to personalise, adjust, and complement the HIS product and reap the benefits of this new technology, doctors and other healthcare professionals must perform many difficult and time-consuming tasks, which often creates a barrier towards its usage [48]. Therefore, special emphasis should be placed on the long-term benefits of using the same system while optimising the user requirements and capabilities of the system [49]. Based on the above stated, we develop the first research proposition:
Proposition 1. (RP1)
The perception of time savings with the hospital information system impacts the intention to use it.
3.2. Privacy Protection
When using HIS services, patients and healthcare professionals have specific expectations, and privacy protection is essential to ensure that these expectations are honoured [50]. Hospitals and healthcare facilities that place a high priority on privacy security are better able to meet these demands and promote the secure and efficient use of HIS services [51]. Healthcare professionals are more likely to use the HIS when they trust that sensitive medical information is adequately protected, because it contributes to better security in the whole health system [13]. A robust privacy protection framework builds trust and confidence in the system [12], and privacy protection ensures that this information remains confidential, aligning with patients’ intentions for privacy when discussing medical issues [52]. This said, we developed the second research proposition:
Proposition 2. (RP2)
The perception of privacy protection with the hospital information system impacts the intention to use it.
3.3. Demographic Characteristics
To some extent, demographic characteristics can be related to the intention to use hospital information systems (HISs) and can provide insights into user behaviour and preferences [48]. However, they should not be used in isolation to determine the intention to use an HIS. In terms of age, for example, younger individuals may be more comfortable with technology and more inclined to use digital healthcare services, including HISs, but older individuals may also use the HIS, especially if they perceive the benefits and ease of use [53]. Considering the education level, hospital workers with higher education are often associated with a greater intention to use the HIS [54]. As well, users with more education may have better digital literacy skills and a greater understanding of the benefits of healthcare technology [55]. Therefore, healthcare organisations should consider a user-centred approach that considers both demographic characteristics and user experiences when designing and implementing an HIS [56]. Based on the above, we develop the third and fourth research propositions:
Proposition 3. (RP3)
Demographic characteristics are related to the intention to use hospital information systems.
- a.
- Age is related to the intention to use hospital information systems.
- b.
- Education is related to the intention to use hospital information systems.
Proposition 4. (RP4)
Demographic characteristics (age and education) moderate the relationship between time savings and privacy protection with the intention to use hospital information systems.
Based on the developed research propositions, the research model is presented in Figure 1.
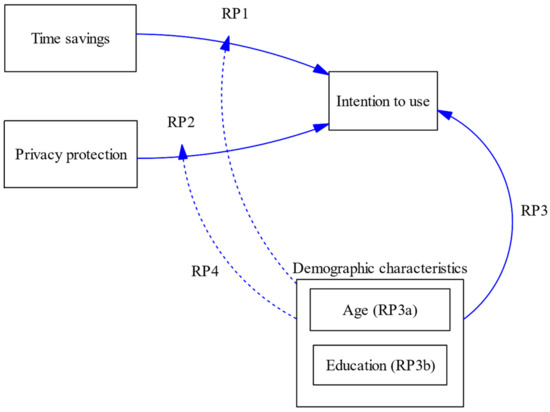
Figure 1.
Research model. Source: Authors’ work.
4. Methodology
4.1. Research Instrument
The research instrument was developed based on the defined research propositions about the intention to use the healthcare information system. It included questions about perceived time savings, perceived privacy, and intention to use the information system. All item measures used were based on five-point Likert scales from 1 (strongly disagree) to 5 (strongly agree) and are presented in Table 1. In addition, information about the age and educational level of the healthcare professionals filling out the survey was collected.

Table 1.
Research instrument.
4.2. Data
The primary research was carried out using a structured questionnaire in 2020. The target population of this research was employees of the Bjelovar General Hospital in Croatia. The General Hospital in Bjelovar has 811 employees. However, not all employees are entitled to use the HIS in the hospital. Due to the limited number of licences and nature of the work, licenced users are limited to 237 healthcare professionals engaged in the data management of patients. An online questionnaire was created using Google Forms to conduct the survey. An e-mail message was sent to all licenced users (237 users), and 47.67% (113 users) participated in the survey.
Figure 2 shows the structure of the examined health professionals who have a license to use the HIS. Regarding the age of the respondents in the sample, the largest share of healthcare professionals who are licensed for the HIS is between 31 and 40 years old (29%) and between 51 and 60 years old (28%), while the fewest employees licensed to use the HIS are only 4% aged over 61 years. As far as education is concerned, the most healthcare workers with a license to use the HIS have a high school education (41%), while only 10% of them have a doctorate.
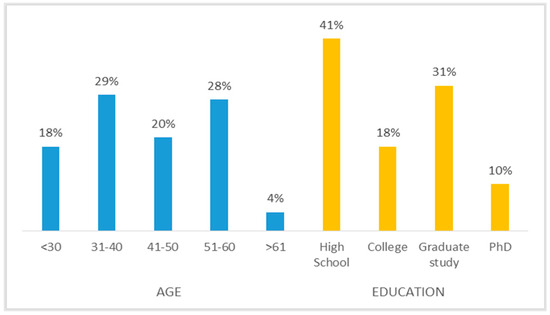
Figure 2.
The respondents’ structure regarding age and education. Source: Authors’ work.
After the data collection was completed, the preparation and verification of the collected data from the survey began. The verification of the collected data was carried out through tests whose purpose was to examine atypical values in the data and to examine the assumption of a normal distribution of the manifest variables.
4.3. Statistical Analysis
Firstly, data analysis using descriptive statistics provides an overview of the frequencies, mean values, and standard deviations of variables, and correlation was used to analyse the relationship between variables and their significance at the level of 1% [57]. Secondly, the data reliability of the research scales was investigated using Cronbach’s alpha [58], and exploratory factor analysis was conducted to ensure the internal consistency of the items [59]. Thirdly, multiple regression was employed to investigate and quantify the associations between the intention to use the HIS and the factors of perceived time savings and perceived privacy protection, controlling for age and education.
Two regression models were created. In Model 1, the dependent variable was the intention to use the HIS, and the independent variables were perceived time savings and perceived privacy protection to test research propositions RP1 and RP2. In Model 2, the dependent variable is the same as in Model 1. In contrast, the control variables age and education were added to the independent variables (perceived time savings and perceived privacy protection) to test research proposition RP3. Model 1 and Model 2 were compared using the F-test to investigate the research proposal for RP4. SPSS v.23 was used to conduct the analysis.
5. Results
5.1. Descriptive Analysis
The analysis of the dataset reveals key insights into the respondents’ attitudes towards hospital information systems (HISs), as presented in Table 2.

Table 2.
Descriptive statistics with Cronbach’s alpha.
The high means for the intention variables indicate a strong overall intention to use an HIS among the participants, which suggests a general positive inclination towards adopting these systems. On the other hand, the means for the privacy variables (ranging from 2.77 to 3.48) are comparatively lower, pointing to moderate to low concerns or satisfaction levels regarding the privacy aspects of HISs. This highlights a potential area of improvement for ensuring users’ confidence in the security and privacy of their information.
The time efficiency variables (TIME1: 4.03, TIME2: 3.60, TIME3: 3.32, TIME4: 3.58) show generally positive perceptions of HISs’ ability to save time, though there is some variability. This indicates that while respondents generally perceive HISs as time-efficient, there is still room for enhancing these perceptions.
5.2. Reliability and Validity Analysis
Cronbach’s alpha coefficients were calculated to test the reliability of the variables with the cut-off value (0.70), which implies the internal consistency of the scale items. Research results showed that all of the calculated Cronbach’s alpha coefficients are larger than 0.70, which indicates the internal consistency of the scale’s items (Table 2).
To test the validity of the model, convergent validity analysis was applied using explanatory factor analysis. In measures of rotated factors, the complexity of the factor loading was minimised to have a structure that would be more easily interpreted for the observed models. Three factors were obtained when the iterated primary axis factor and varimax rotation were combined, as shown in Table 3.

Table 3.
Rotated factor matrix for three factors.
According to [60], all of the factor loadings for the three factors that were stated are higher than the crucial value of 0.4. This means that they are considered to be stable and desired, which suggests that they are solid factors. There is no requirement to lower the number of variables in order to keep the greater values of the rotation factor [61]. This is because the sample that was taken into consideration for the study was relatively small.
In compliance with the requirements that have been set, it is recommended that all of the measurement items from the research instrument be kept. The exploratory factor analysis was used to extract three factors: (i) the dependent variable intention to use an HIS (INTENT), (ii) the independent variable perceived time savings (TIME), and (iii) the independent variable perceived privacy protection (PRIVACY).
5.3. Correlation Analysis
A non-parametric Spearman’s correlation coefficient analysis was performed to determine the direction and strength of the extracted factor variables in analysing the correlations between the observed variables. The results of the correlation analysis are given in Table 4. All coefficients of the control variable AGE are not significant at the level of 5%. There is a positive and moderate connection between the variable INTENT and the independent variable TIME, statistically significant at the level of 1%. In contrast, the other independent variable, PRIVACY, in relation to the variable INTENT, is not statistically significant. Furthermore, there is a positive relationship, statistically significant at the 1% level, between the dependent variable INTENT and the control variable EDUCATION. The relationship between the independent variables TIME and PRIVACY is positive and statistically significant at the 5% level. There is also statistical significance at the 1% level in the relationship between the independent variable PRIVACY and the control variable EDUCATION, whose relationship is negative and weak.

Table 4.
Correlation coefficients.
Figure 3 presents a heatmap of the correlation coefficients. In general, Spearman’s correlation coefficients among variables reflect weaker interrelationships. On the heatmap shown in Figure 3, the most positive connections are between the dependent variable INTENT and the independent variable TIME, i.e., the control EDUCATION. Negative relationships are established mainly with the control variable AGE, and the most negative relationship is between the independent variable PRIVACY and the control EDUCATION.
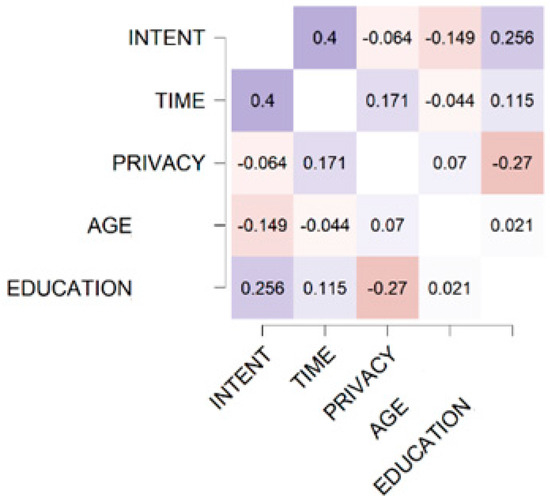
Figure 3.
Heatmap of correlations. Source: Authors’ work.
5.4. Regression Analysis
Table 5 presents the summary results of the regression analyses. Two regression models were estimated.

Table 5.
Estimated linear regression models; dependent variable: intention to use the hospital information system (INTENT).
Model 1 includes the dependent variable intention to use the HIS and two independent variables, protection of privacy and time savings. The independent variable TIME was statistically significant at the 1% level. Furthermore, there was a positive regression coefficient (β = 0.364, p < 0.000) in the relationship between the dependent variable INTENT and the independent variable TIME, which can be explained by the fact that if the users’ time savings when using an HIS by themselves increase, then the users’ intention to use the HIS will increase linearly. Considering the results, PRIVACY has a negative effect on the intention to use an HIS (β = −0.134, p > 0.01), which means that with greater confidence and trust of users in the hospital information system that contains their private data, the intention to use that information system within the hospital organisation would decrease linearly and on average. However, this relationship is not statistically significant in Model 1. Model 1 explains 16.1% of the variance (R2 = 0.161).
In Model 2, two control variables, AGE and EDUCATION, were added to the already existing relationship between the dependent variable INTENT and the independent variables PRIVACY and TIME in order to enhance the internal validity of the research models by limiting the influence of confounding and other extraneous variables. These variables can also establish a correlational relationship in the model and avoid research bias. The addition of control variables in the second model did not significantly change the regression coefficients of the independent variables TIME (β = 0.328, p < 0.000) and PRIVACY (β = −0.077, p > 0.01). The independent variable TIME is statistically significant in Model 2 at the 1% level. At the same time, PRIVACY has no statistical significance in the second model. The control variable AGE negatively affects the intention to use an HIS, but this effect is not statistically significant in Model 2. This means that AGE affects the intention to use an HIS along with other significant variables, such as TIME, in the model. The variable EDUCATION is statistically significant in the model at the 5% level. It has a positive effect, which implies that users of HISs with a certain level of education increase their intention to use the HIS. Model 2 explains 20.5% of the variance (R2 = 0.205).
Overall, the results of the regression analysis for the two observed models showed that the change in the coefficient of determination in the second model was significant (F (113) = 2.944, p = 0.057)) at the level of 10%. In Model 2, the variables time savings and education were significantly associated with the intention to use an HIS (β = 0.328, p = 0.000 and β = 0.265, p = 0.047, respectively). When control variables, such as education and age of respondents, were included in the model, these variables raised the level of variance coverage in the model by 4.4%. Hence, Model 2 became better and statistically significant at the level of 10%. Based on the above, Model 2 explains that the demographic characteristic education alleviates the relationship where greater time savings of HIS users positively affect the intention to use the HIS.
5.5. Research Proposition Testing

Table 6.
Research proposition investigation using linear regression models.
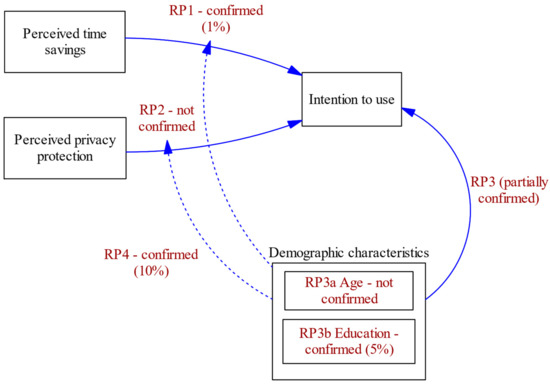
Figure 4.
Research model with research proposition testing.
In Model 1, we observed the relationship between the independent variables, time savings and privacy protection, and the dependent variable, intention to use the HIS. The Model 1 shows acceptance of RP2 and rejection of RP1. The acceptance of RP2 implies that the variable TIME is statistically significant in the model at the 1% level and that an increase in the time savings of HIS users would result in a greater intention to use it. Moreover, the PRIVACY variable is not statistically significant in the model; hence, RP1 was rejected.
By adding the control variables AGE and EDUCATION, an effort was made to determine the influence of these variables on the intention to use HISs and to identify whether the control variables moderate the influence of TIME and PRIVACY on the intention to use HISs. The results suggest that H3 is partially accepted. The variable AGE is not statistically significant in Model 2, which is why H3a is rejected. On the other hand, EDUCATION is statistically significant in the second model at the 5% level, and H3b is accepted, indicating that there is a relationship between the control variable EDUCATION and the intention to use an HIS. In addition, the second model shows a greater coverage of variance deviation by 4.4% compared with the first model. Therefore, the variable EDUCATION moderates the relationship between HIS users’ time savings and intention to use such a system. Hence, H4 is accepted.
6. Conclusions
In this research, the linear multiple regression model was used to test the set hypotheses and determine the influence of the relationship between the independent variables, perceived time savings and perceived privacy protection, with the dependent variable, intention to use an HIS. Furthermore, two control variables measuring the age and educational level of HIS users were added to the model to identify the mitigation of the influence in the connection between the mentioned independent variables and the intention to use an HIS.
Results indicated that perceived time savings have a positive, statistically significant impact on the intention to use an HIS, indicating that time savings resulting from the usage of the HIS shorten the time for the implementation of other actions [41]. Although concern was expressed in previous research that use of HISs could increase administrative tasks and thus have a negative impact on efficient time usage [30], this was unsubstantiated with our research, leading to the conclusion that the time savings is one of the key factors influencing the intention to use HISs because it ensures the management of the time needed to perform a specific activity and organisation for other business tasks [15]. These results could be useful for the management of the healthcare institution, with the notion that even higher time savings could provide a stronger incentive to employees to use the HIS to an even greater level.
The impact of user privacy protection on the intention to use an HIS, which refers to H2, is rejected, and this relationship is not statistically significant in the model, thus not confirming previous research [13,51]. A possible reason is that the respondents had quite a high and uniform belief that the HIS they use is secure, with a strong data management approach, reflected in low values of variable perceived privacy. Further research should be undertaken in this area with a focus on other aspects of privacy from the perspective of HIS users.
Demographic variables had a mixed effect on the intention to use an HIS. The association between age and intention to use an HIS was not significant. On the other hand, education was positively related to the intention to use an HIS, which builds on the finding that hospital workers with higher education are often associated with a greater intention to use HISs [54]. As well, users with more education may have better digital literacy skills and a greater understanding of the benefits of healthcare technology [55].
The second model shows a greater coverage of variance deviation by 4.4% compared with the first model, resulting in a conclusion that age and education moderate the relationships between perceived time savings, perceived privacy, and intention to use an HIS. In their research, the authors [54] emphasise that it is especially important for public health institutions to have employees who have adequate education to work on information systems, which in some way affects their intention to use the system but also their interest in further training. This is somewhat complementary to our finding that the factor of education is included in the relationship between time savings and intention to use HISs [15,55]. Users have to be included in the development, implementation, and education phases of the HIS software for the system to be upgraded to an ideal level, increase user satisfaction, and improve system acceptance to an ideal level.
The low explainability of the regression models is a limitation of this research, which is, on the other hand, a motivation for future research, indicating that, although perceived time savings and education are plausible drivers, the intention to use an HIS would be additionally better explained with other variables. Also, sample coverage could be expanded in future research, which should focus on examining staff using HISs in public and private healthcare institutions so that a comparative analysis can be carried out. Furthermore, the research should include the highest management part of the health institutions that plans and makes decisions about the implementation of information systems in hospitals.
Author Contributions
Conceptualization, M.P.B. and S.K.; methodology, M.P.B. and F.H.Q.; software, M.S.; validation, I.M., S.K. and F.H.Q.; formal analysis, M.P.B.; investigation, I.M.; data curation, M.P.B.; writing—original draft preparation, M.S.; writing—review and editing, M.P.B. and I.M.; visualization, M.S.; supervision, S.K.; project administration, F.H.Q. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
All datasets generated during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
Authors wish to acknowledge the support to of Josipa Osvaldić Galić for her help in data collection.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Poje, I.; Braović, M. Bolnički informacijski sustav—Prednosti i nedostaci u radu. Bilt. Hrvat. Društva Za Med. Inform. 2019, 25, 20–28. [Google Scholar]
- Bach, M.P.; Seljan, S.; Jaković, B.; Buljan, A.; Zoroja, J. Hospital websites: From the information repository to interactive channel. Procedia Comput. Sci. 2019, 164, 64–71. [Google Scholar] [CrossRef]
- Alotaibi, Y.K.; Federico, F. The impact of health information technology on patient safety. Saudi Med. J. 2017, 38, 1173–1180. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.A.; DiazGranados, D.; Dietz, A.S.; Benishek, L.E.; Thompson, D.; Pronovost, P.J.; Weaver, S.J. Teamwork in Healthcare: Key Discoveries Enabling Safer, High-Quality Care. Am. Psychol. 2018, 73, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Isada, F.; Isada, Y. Network Structure of Inter-organizational Alliances in the Health Insurance Industry undergoing Digitalization. Entren. Enterp. Res. Innov. 2023, 9, 281–289. [Google Scholar] [CrossRef]
- Burns, L.R.; Muller, R.W. Hospital-Physician Collaboration: Landscape of Economic Integration and Impact on Clinical Integration. Milbank Q. 2008, 86, 375–434. [Google Scholar] [CrossRef]
- Paul, M.; Maglaras, L.; Ferrag, M.A.; Almomani, I. Digitization of healthcare sector: A study on privacy and security concerns. ICT Express 2023, 9, 571–588. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Rahimi, B.; Nadri, H.; Afshar, H.L.; Timpka, T. A Systematic Review of the Technology Acceptance Model in Health Informatics. Appl. Clin. Inform. 2018, 9, 604–634. [Google Scholar] [CrossRef]
- Rashid, A.H. Technology acceptance models to improve adoption of health information systems. J. Adv. Sci. Eng. Technol. 2018, 1, 17–29. [Google Scholar] [CrossRef]
- Ammenwerth, E. Technology Acceptance Models in Health Informatics: TAM and UTAUT. In Applied Interdisciplinary Theory in Health Informatics; Studies in Health Technology and Informatics; IOS Press: Amsterdam, The Netherlands, 2019; Volume 263, pp. 64–71. [Google Scholar] [CrossRef]
- Dhagarra, D.; Goswami, M.; Kumar, G. Impact of Trust and Privacy Concerns on Technology Acceptance in Healthcare: An Indian Perspective. Int. J. Med. Inform. 2020, 141, 104164. [Google Scholar] [CrossRef] [PubMed]
- Keshta, I.; Odeh, A. Security and privacy of electronic health records: Concerns and challenges. Egypt. Inform. J. 2021, 22, 177–183. [Google Scholar] [CrossRef]
- Birkmeyer, S.; Wirtz, B.W.; Langer, P.F. Determinants of mHealth success: An empirical investigation of the user perspective. Int. J. Inf. Manag. 2021, 59, 102351. [Google Scholar] [CrossRef] [PubMed]
- Wu, J. Healthcare System-Use Behavior: A Systematic Review of ITs Determinants. J. Int. Technol. Inf. Manag. 2016, 25, 5. [Google Scholar] [CrossRef]
- Dünnebeil, S.; Sunyaev, A.; Blohm, I.; Leimeister, J.M.; Krcmar, H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int. J. Med. Inform. 2012, 81, 746–760. [Google Scholar] [CrossRef] [PubMed]
- Bertolazzi, A.; Quaglia, V.; Bongelli, R. Barriers and facilitators to health technology adoption by older adults with chronic diseases: An integrative systematic review. BMC Public Health 2024, 24, 506. [Google Scholar] [CrossRef] [PubMed]
- Tomičić-Pupek, K.; Tomičić Furjan, M.; Pihir, I.; Vrček, N. Disruptive business model innovation and digital transformation. Bus. Syst. Res. Int. J. Soc. Adv. Innov. Res. Econ. 2023, 14, 1–25. [Google Scholar] [CrossRef]
- Li, D.; Hu, Y.; Pfaff, H.; Wang, L.; Deng, L.; Lu, C.; Xia, S.; Cheng, S.; Zhu, X.; Wu, X. Determinants of Patients’ Intention to Use the Online Inquiry Services Provided by Internet Hospitals: Empirical Evidence from China. J. Med. Internet Res. 2020, 22, e22716. [Google Scholar] [CrossRef] [PubMed]
- Medical, R.T. What Are the Differences between PACS, RIS, CIS, LIS and HIS? Available online: https://rtmedical.com.br/what-are-the-differences-between-pacs-ris-cis-lis-and-his/?lang=en (accessed on 2 February 2023).
- Kwok, D.; Yang, S. Evaluating the intention to use ICT collaborative tools in a social constructivist environment. Int. J. Educ. Technol. High. Educ. 2017, 14, 32. [Google Scholar] [CrossRef]
- Nadri, H.; Rahimi, B.; Lotfnezhad Afshar, H.; Samadbeik, M.; Garavand, A. Factors Affecting Acceptance of Hospital Information Systems Based on Extended Technology Acceptance Model: A Case Study in Three Paraclinical Departments. Appl. Clin. Inform. 2018, 9, 238–247. [Google Scholar] [CrossRef]
- Ribeiro, J.A.; Scapens, R.W. Institutional theories and management accounting change: Contributions, issues and paths for development. Qual. Res. Manag. Account. 2006, 3, 94–111. [Google Scholar] [CrossRef]
- Escobar, B.; Escobar, T.; Monge, P. ERPs in hospitals: A case study. J. Inf. Technol. Res. 2010, 3, 34–50. [Google Scholar] [CrossRef][Green Version]
- Bohr, A.; Memarzadeh, K. The rise of artificial intelligence in healthcare applications. In Artificial Intelligence in Healthcare; Academic Press: Cambridge, MA, USA, 2020; pp. 25–60. [Google Scholar] [CrossRef]
- Thimbleby, H. Technology and the Future of Healthcare. J. Public Health Res. 2013, 2, e28. [Google Scholar] [CrossRef] [PubMed]
- Nutley, T.; Reynolds, H.W. Improving the use of health data for health system strengthening. Glob. Health Action 2013, 6, 20001. [Google Scholar] [CrossRef] [PubMed]
- Menachemi, N.; Collum, T.H. Benefits and drawbacks of electronic health record systems. Risk Manag. Healthc. Policy 2011, 4, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Casalino, N.; Saso, T.; Borin, B.; Massella, E.; Lancioni, F. Digital competences for civil servants and digital ecosystems for more effective working processes in public organizations. In Digital Business Transformation; Lecture Notes in Information Systems and Organisation; Springer International Publishing: Cham, Switzerland, 2020; pp. 315–326. [Google Scholar] [CrossRef]
- Ker, J.I.; Wang, Y.; Hajli, N. Examining the impact of health information systems on healthcare service improvement: The case of reducing in patient-flow delays in a US hospital. Technol. Forecast. Soc. Chang. 2018, 127, 188–198. [Google Scholar] [CrossRef]
- Lee, J.; McCullough, J.S.; Town, R.J. The impact of health information technology on hospital productivity. RAND J. Econ. 2013, 44, 545–568. [Google Scholar] [CrossRef]
- Benbya, H.; Nan, N.; Tanriverdi, H.; Yoo, Y. Complexity and information systems research in the emerging digital world. Manag. Inf. Syst. Q. 2020, 44, 1–17. [Google Scholar] [CrossRef]
- Chen, H.; Hailey, D.; Wang, N.; Yu, P. A Review of Data Quality Assessment Methods for Public Health Information Systems. Int. J. Environ. Res. Public Health 2014, 11, 5170–5207. [Google Scholar] [CrossRef]
- Handayani, P.W.; Sandhyaduhita, P.I.; Hidayanto, A.N.; Pinem, A.A.; Fajrina, H.R.; Junus, K.M.; Budi, I.; Ayuningtyas, D. Integrated hospital information system architecture design in Indonesia. In Hospital Management and Emergency Medicine; IGI Global: Hershey, PA, USA, 2020; pp. 244–273. [Google Scholar] [CrossRef]
- Kovačić, M.; Mutavdžija, M.; Buntak, K. E-Health application, implementation and challenges: A literature review. Bus. Syst. Res. Int. J. Soc. Adv. Innov. Res. Econ. 2022, 13, 1–18. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B. The Technology Acceptance Model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Garavand, A.; Mohseni, M.; Asadi, H.; Etemadi, M.; Moradi-Joo, M.; Moosavi, A. Factors influencing the adoption of health information technologies: A systematic review. Electron. Physician 2016, 8, 2713–2718. [Google Scholar] [CrossRef] [PubMed]
- Beenkens, F.H.; Verburg, R.M. Extending TAM to measure the adoption of E-Collaboration in healthcare arenas. In Encyclopedia of E-Collaboration; IGI Global: Hershey, PA, USA, 2008; pp. 265–271. [Google Scholar] [CrossRef]
- Ketikidis, P.; Dimitrovski, T.; Lazuras, L.; Bath, P.A. Acceptance of health information technology in health professionals: An application of the revised technology acceptance model. Health Inform. J. 2021, 18, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Hajek, A.; Kretzler, B.; König, H.H. Determinants of healthcare use based on the Andersen model: A study protocol for a systematic review of longitudinal studies. BMJ Open 2021, 11, e044435. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Lu, J. An empirical study on user acceptance of healthcare website. Int. J. Netw. Virtual Organ. 2014, 14, 57–73. [Google Scholar] [CrossRef]
- Bansal, G.; Zahedi, F.; Gefen, D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decis. Support Syst. 2010, 49, 138–150. [Google Scholar] [CrossRef]
- Angst, N.; Agarwal, N. Adoption of electronic health records in the presence of privacy concerns: The elaboration likelihood model and individual persuasion. Manag. Inf. Syst. Q. 2009, 33, 339. [Google Scholar] [CrossRef]
- Caine, K.; Hanania, R. Patients want granular privacy control over health information in electronic medical records. J. Am. Med. Inform. Assoc. 2013, 20, 7–15. [Google Scholar] [CrossRef]
- Sætra, H.S.; Fosch-Villaronga, E. Healthcare Digitalisation and the Changing Nature of Work and Society. Healthcare 2021, 9, 1007. [Google Scholar] [CrossRef]
- Mosadeghrad, A.M. Factors influencing healthcare service quality. Int. J. Health Policy Manag. 2014, 3, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Ljubicic, V.; Ketikidis, P.H.; Lazuras, L. Drivers of intentions to use healthcare information systems among health and care professionals. Health Inform. J. 2020, 26, 56–71. [Google Scholar] [CrossRef]
- Beard, J.W.; Sethi, A.; Jiao, W.; Hyatt, H.W.; Yapici, H.O.; Erslon, M.; Overdyk, F.J. Cost savings through continuous vital sign monitoring in the medical-surgical unit. J. Med. Econ. 2023, 26, 760–768. [Google Scholar] [CrossRef]
- El-Haddad, C.; Hegazi, I.; Hu, W. Understanding Patient Expectations of Health Care: A Qualitative Study. J. Patient Exp. 2020, 7, 1724–1731. [Google Scholar] [CrossRef] [PubMed]
- Clayton, E.W.; Embí, P.J.; Malin, B.A. Dobbs and the future of health data privacy for patients and healthcare organizations. J. Am. Med. Inform. Assoc. JAMIA 2022, 30, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Tariq, R.A.; Hackert, P.B. Patient Confidentiality. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519540/ (accessed on 27 May 2024).
- Lupton, D. Young People’s Use of Digital Health Technologies in the Global North: Narrative Review. J. Med. Internet Res. 2021, 23, e18286. [Google Scholar] [CrossRef] [PubMed]
- Alipour, J.; Mehdipour, Y.; Karimi, A. Factors Affecting Acceptance of Hospital Information Systems in Public Hospitals of Zahedan University of Medical Sciences: A Cross-Sectional Study. J. Med. Life 2019, 12, 403–410. [Google Scholar] [CrossRef]
- Tegegne, M.D.; Tilahun, B.; Mamuye, A.; Kerie, H.; Nurhussien, F.; Zemen, E.; Mebratu, A.; Sisay, G.; Getachew, R.; Gebeyehu, H.; et al. Digital literacy level and associated factors among health professionals in a referral and teaching hospital: An implication for future digital health systems implementation. Front. Public Health 2023, 11, 1130894. [Google Scholar] [CrossRef]
- De Vito Dabbs, A.; Myers, B.A.; Mc Curry, K.R.; Dunbar-Jacob, J.; Hawkins, R.P.; Begey, A.; Dew, M.A. User-Centered Design and Interactive Health Technologies for Patients. Comput. Inform. Nursing CIN 2009, 27, 175. [Google Scholar] [CrossRef]
- Cooksey, R.W.; Cooksey, R.W. Descriptive statistics for summarising data. Illus. Stat. Proced. Find. Mean. Quant. Data 2020, 15, 61–139. [Google Scholar]
- Bujang, M.A.; Omar, E.D.; Baharum, N.A. A Review on Sample Size Determination for Cronbach’s Alpha Test: A Simple Guide for Researchers. Malays. J. Med. Sci. MJMS 2018, 25, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods 1999, 4, 272–299. [Google Scholar] [CrossRef]
- Costello, A.B.; Osborne, J. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2019, 10, 7. [Google Scholar] [CrossRef]
- Thompson, B. Exploratory and Confirmatory Factor Analysis: Understanding Concepts and Applications; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).