Abstract
Complex mechanisms exist between public risk perception, emotions, and coping behaviors during health emergencies. To unravel the relationship between these three phenomena, a meta-analytic approach was employed in this study. Using Comprehensive Meta-Analysis 3.0, 81 papers were analyzed after selection. The results of the meta-analysis showed that (1) risk perception (perceived severity, perceived susceptibility) and negative emotions (especially fear) are both correlated with coping behaviors; (2) risk perception is strongly correlated with fear and moderately correlated with anxiety; and (3) anxiety predicts the adoption of coping behaviors. The existing research provided an empirical basis for implementing effective coping behavior interventions and implied that management decisionmakers need to consider reasonable interventions through multiple channels to maintain the public’s risk perception and emotions within appropriate levels. Finally, future research directions are suggested.
1. Introduction
In December 2019, multiple cases of an unknown form of pneumonia were reported, which were later confirmed to be caused by novel coronavirus (COVID-19) infections. COVID-19 has spread to many countries around the world and has been recognized by the World Health Organization as a global pandemic. In addition to the novel coronavirus outbreak, many other public health events have occurred or are occurring in various countries, such as SARS, Ebola, H1N1, and H7N9 outbreaks. Globally, for the period from January 2020 to December 2021, the World Health Organization estimates that there were 14.83 million excess deaths associated with the COVID-19 pandemic [1]. During the 2009 influenza A (H1N1) pandemic, there were an estimated 201,200 deaths worldwide due to respiratory diseases [2]. Illness and death caused by infectious diseases have exerted a huge burden and negative impact on the world.
Epidemics and pandemics pose a threat to public health, and the uncertainty and hazards associated with such events often cause negative emotions such as public panic, anxiety, and nervousness. Excessive public panic and anxiety can lead to irrational snap behavior [3]. Individuals can even develop mental health problems such as stress disorders, depression, and suicidal behavior [4,5]. Risk perception is considered to be the key factor affecting mood. The higher the risk perception of an individual is, the stronger the impact it has on one’s mental health, leading to the development of negative emotions such as fear and anxiety [6].
In the face of a public health event, before vaccines and preventive medicines are developed and produced, the public adopts a range of nonpharmaceutical interventions, such as washing hands, using masks, and avoiding public transportation. These protective behaviors are simple, inexpensive, and effective in minimizing the spread and impact of diseases. High levels of public support, participation, and cooperation relating to health-protective behaviors are key to overcoming an epidemic or pandemic [7]. Research on health behaviors suggests that risk perception is central to determining individual preventive behaviors. Risk communication forms the basis of risk perception, which facilitates the formation of accurate knowledge and enables the practice of preventive behaviors [8,9]. In addition, studies have shown that emotions are an important factor in decision-making processes among individuals [10,11]. In the context of a public health event, the public may develop negative emotions such as fear and anxiety, and these negative emotions increase the implementation of preventive behaviors [12,13].
As noted above, individuals’ risk perception, emotional states, and coping behaviors are related to their own physical and mental health and then to the normal functioning of society. Coping behavior is directly related to controlling the spread of the outbreak. Individual factors contribute to their correct coping decisions, notably risk perception and emotion [14,15]. Understanding the public’s cognitive and perceptual patterns is important for guiding prevention programs and mental health communications. Media exposure, government intervention, etc., affect the psychology, perceptions, and behavior of individuals [16,17]. It is necessary to examine the current state of public perception and identify the gap between it and the actual situation regarding the development of pandemics. For this purpose, many scholars have applied Protection Motivation Theory (PMT); Knowledge, Attitude, and Practice (KAP); Health Belief Model (HBM); and other health behavior change theories to conduct several studies on public risk perception, emotions, and coping behaviors, which provide a basis for national decisionmakers to adopt precise prevention and control strategies, including health education, for the public [18,19,20,21,22,23]. The research is based on public perceptions of risk, emotions, and coping behaviors. Cross-sectional surveys have been used to understand the performance of the public in terms of risk perception, emotions, and coping behaviors and the relationship between them.
Each survey is independent and decentralized, ranging from targeting a small group of people engaged in a particular career in a city to a nationwide sample of people. Although such studies can provide good guidance in the short term, there are limitations due to their sample size and regional limitations. Inconsistent findings exist in numerous studies. For example, Wang et al. concluded that risk perception inhibits coping behavior [24], whereas Kim et al. found no significant association between the perceived risk of infection and coping behavior in the context of the H1N1 outbreak in 2009 [23]. However, in previous studies, the path of influence between two variables has often been considered or studied for only one variable. Few researchers have explored this issue from the perspective of the internal mechanisms of the three phenomena. However, the existence of linkage effects between these three phenomena may affect the effectiveness of interventions. Therefore, it is necessary to systematically study how they relate to each other. For example, Levkovich et al. examined only the effect of perceived vulnerability on behavior [25]. Shen et al. focused on the role of risk perception in preventive behavior [26]. Yildirim et al. discussed the relationship between risk perception and fear in preventive behavior but lacked consideration of the pathway of risk perception and emotion [12]. Therefore, a systematic study is needed. The strength of the relationship between risk perception, emotion, and behavior also varies considerably across studies. Few studies have been conducted to integrate the results in this area; address the controversies in this area; avoid bias in the results of previous individual studies influenced by sample size, age, and region; and draw more general and accurate conclusions from a macroscopic perspective. The current study aims to integrate and analyze existing research on public health events through meta-analysis and explore future research directions. By estimating the strength of the relationship between public risk perception, negative emotions, and coping behaviors, a critical path is identified. Thus, the current findings will provide a basis for decisionmakers to intervene in risk perception and regulate public emotions and preventive behaviors. By analyzing existing research, we will seek to identify potential research gaps in risk perception, emotions, and behaviors related to public health events and pave the way for future research.
2. Methods
The present study used a meta-analysis technique that describes the outcomes of various empirical studies by using the correlation coefficient as an effect size estimate [27]. Effect size estimates were combined to provide useful insights [19]. A meta-analysis typically involves the identification of studies, the determination of inclusion and exclusion criteria, the coding of studies, statistical analysis, and data analysis. These steps are described below in detail.
2.1. Identification of Studies
Step 1: CNKI (China National Knowledge Internet) is one of the most complete and powerful databases of dissertations and articles in China. It has obvious advantages in terms of the types of journals, the number of citations, and the update cycle. Web of Science is an internationally renowned database with relatively high-quality articles. The CNKI and Web of Science electronic databases were searched using keywords related to public health events, risk perception, emotion, and coping behavior. We identified the keywords to be searched by pre-reading the literature. The search terms used were as follows.
Public health events: “COVID-19”; “SARS-CoV-2”; “novel coronavirus”; “coronavirus disease 2019”; “Ebola”; “H1N1”; “polio”; “poliomyelitis”; “SARS”; “atypical pneumonia”; “Zika”; “H7N9”; “flu”; “influenza”; “grippe”.
Risk perception: “Risk Perception”.
Emotion: “emotion”; “sadness”; “anxious”; “anxiety”; “fear”.
Coping behavior: “practice”; “behavior”; “coping behavior”; “prevention”.
Boolean operators such as “AND” and “OR” were used to combine these search terms. The search was performed from database inception to May 2022. For Chinese studies, the restricted sources were the Peking University Core, Chinese Social Sciences Citation Index (CSSCI), and Chinese Science Citation Database (CSCD). After aggregating the studies and removing duplicates, a total of 8187 publications were found.
Step 2: The inclusion and exclusion criteria (see Section 2.2) were discussed and agreed upon by all authors. These criteria and the relevance of the topic were used as a guide for the initial screening. Two authors individually read the titles, keywords, and abstracts of all 8187 publications to weed out the irrelevant ones. The two authors resolved their differences through discussion. A total of 871 were found to be potentially eligible in this step.
Step 3: For the publications shortlisted in step 2, the two authors further consulted the full text of each study. The studies that could be included in the final meta-analysis were screened according to the criteria in step 2 above. Again, disagreements were resolved by discussions between the two authors. A total of 790 studies were excluded for various reasons, such as unavailability of the original text, irrelevant topics, inconsistent research directions, and nondisclosure of the required data. Ultimately, 81 documents were included in the meta-analysis.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) cross-sectional study—there were no restrictions regarding the method of data collection (paper questionnaire, telephone survey, Google Forms, etc.); (2) the survey used Likert scales for quantitative measures as much as possible and reported Pearson correlation coefficients or Spearman correlation coefficients between at least two variables involved in the study model; (3) the sample size was determined; (4) the publication was a journal paper, conference paper, etc., that had been peer-reviewed; (5) the study population included individuals aged 7 years or older; and (6) the behaviors examined in the study involved nonpharmacological intervention behaviors. Coping behaviors included hygienic behaviors (such as washing one’s hands, coughing or sneezing into one’s hands or a tissue, cleaning surfaces); mask wearing; social distancing (such as avoiding crowds, postponing or canceling large public gatherings, working online); and seeking the advice of a professional or a relative.
The exclusion criteria were as follows (in Figure 1): (1) a systematic review or purely theoretical study; (2) the article only examined the basic performance of the public during the health event; (3) duplicate reports by the same author or based on the same survey; (4) the study examined people under 7 years of age; (5) Pearson correlation coefficients or Spearman correlation coefficients were not reported; (6) the study was too detailed, i.e., classified nonpharmacological interventions for protective behaviors and studied them individually; and (7) the behaviors in the study were presented as pharmacological interventions.
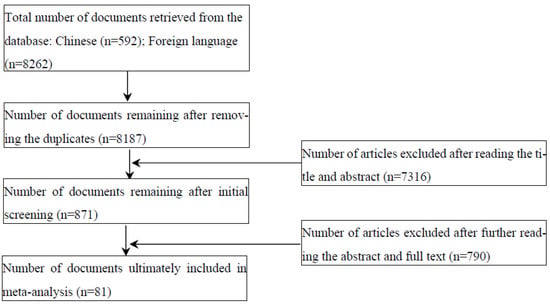
Figure 1.
Flowchart of selected articles included in this systematic review and meta-analysis.
2.3. Literature Coding Procedure
Basic information about the included studies was recorded: title, authors, source, year of publication, sample size, correlation coefficient, events involved, and study population.
To perform Spearman’s correlation analysis, we transformed the statistical derivation of the two sides of the following equation, in accordance with Rupinski and Dunlap [28]:
2.4. Statistical Analysis
The fixed effects model and random effects model are two popular statistical models that have been used for meta-analysis. The fixed effects model assumes that there should be a single effect in the whole population and that the difference between effect sizes is due to variance. The random effects model, on the other hand, assumes that the different effects occur in the aggregate of the extracted sample. This study applied the Q statistic to establish the presence of heterogeneity in the study and used the I2 statistic to estimate the magnitude of heterogeneity [29]. If heterogeneity was significant, the analysis was performed using a random effects model. If there was no significant heterogeneity, a fixed effects model was used.
2.5. Data Analysis Procedures
In this study, Pearson’s correlation coefficient (r) was used as the effect value indicator, where r ≤ 0.10 indicated a low correlation, 0.10 < r < 0.40 indicated a medium correlation, and r ≥ 0.40 indicated a high correlation [30]. The effect size provides an estimate of the degree of existence of the phenomenon of the relationship. The higher the value of the effect size, the greater the existence of the phenomenon. Meta-analysis main effects tests and moderating effects tests were performed using the Comprehensive Meta-Analysis Version 3.3 (CMA 3.3) software. In the process of effect value estimation, to ensure the independence of effect values, if more than 2 effect values appeared for a study factor pair, the effect size of the total sample was included if the overall performance of the sample was disclosed, i.e., the overall effect. If the overall performance of the sample was not disclosed, we decided whether all effect values were included separately depending on the situation.
3. Results
3.1. Basic Characteristics of the Included Literature
The literature was searched using the CNKI and Web of Science databases and screened using strict inclusion and exclusion criteria, and 81 papers were included. In total, 5 papers included studies conducted on multiple occasions at different times and in different groups, and, thus, a total of 86 studies were included. The timespan of the studies ranged from 2005 to 2022, and the public health events included ZIKA, SARS, H1N1, H7N9, MERS, influenza, and the current COVID-19 pandemic. The included studies were all journal papers. A total of 63,358 subjects were identified as the general public, university students, medical-related students, medical workers, service industry workers, firefighters, etc. The basic information of the included studies is shown in Table 1.

Table 1.
Basic information of the included studies.
These studies were conducted in a piecemeal fashion rather than in a systematic way. Of the 86 studies included, 5 studies (5.8%) examined the relationship between emotion and behavior, 10 studies (11.6%) examined the relationship between risk perception and emotion, 59 studies (68.6%) examined the relationship between risk and coping behavior, and 8 studies (9.3%) examined the relationship between risk and behavior as well as emotion and behavior. Only four studies (4.7%) examined the relationship between all three phenomena simultaneously. There is a need to conduct systematic and comprehensive research on this subject.
We reviewed the full text of the 81 included studies. They were relatively uniform in the way they measured variables such as fear, anxiety, risk perception, and coping behavior. All had multiple items set, scored on a scale, and responses were summed to obtain a total score, with the level of the score representing the level of the variable. Fear was measured using the FCV-19S or other self-administered scales. Anxiety was measured using the SAS Anxiety Self-Rating scale, the GAD-7 scale, the POMS scale, the Brunel Mood scale, etc. Risk perception was measured by items such as the PRQ scale, with questions such as “I have a high risk of infection...”, etc. Perceived susceptibility was measured by items such as “I have a high risk of infection with novel coronavirus”. For perceived severity, items such as “I think this novel coronavirus is very serious” were used. Coping behavior was measured using preventive protective behaviors recommended by health agencies. The factors of the included studies are shown in Table 2.

Table 2.
The factors included in the studies.
3.2. Main Effects Test
The corresponding pooled and transformed effect sizes (Pearson’s correlation coefficient r and sample size n) under each of the relationships were imported into CMA 3.3 for heterogeneity test. The results show that the Q statistic was significant for each relationship, indicating the existence of different effects in the population from which the sample was extracted, which does not support the hypothesis of homogeneity. The I2 was greater than 50% for all relationships, indicating a high degree of heterogeneity; therefore, the random effects model was chosen to ensure the stability of effect values.
The results of this study are shown in Table 3. The corresponding forest diagrams are shown in Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7 and Figure 8. The results show that the combined correlation coefficient between risk perception and coping behavior was 0.189 [95% CI (0.121, 0.256)]; the combined correlation coefficient between perceived susceptibility and coping behavior was 0.207 [95% CI (0.133, 0.279)]; the combined correlation coefficient between perceived severity and coping behavior was 0.296 [95% CI (0.237, 0.354)]; the combined correlation coefficient between risk perception and fear level was 0.481 [95% CI (0.327, 0.610)]; the combined correlation coefficient between risk perception and anxiety level was 0.338 [95% CI (0.208, 0.457)]; the combined correlation coefficient between fear and coping behavior was 0.239 [95% CI (0.089, 0.377)]; and the combined correlation coefficient between anxiety and coping behaviors was 0.122 [95% CI (−0.088, 0.321)].

Table 3.
Main effects test results.
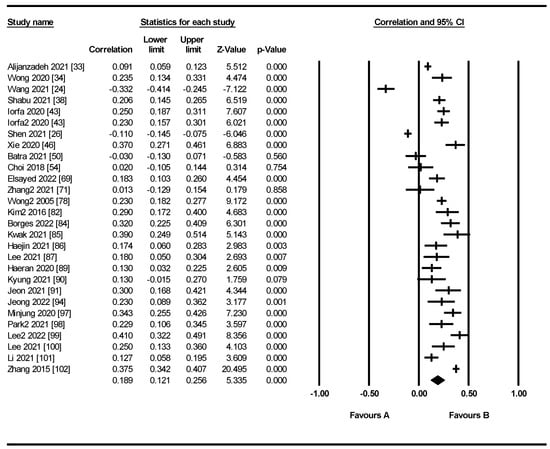
Figure 2.
The correlation between risk perception and coping behavior. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
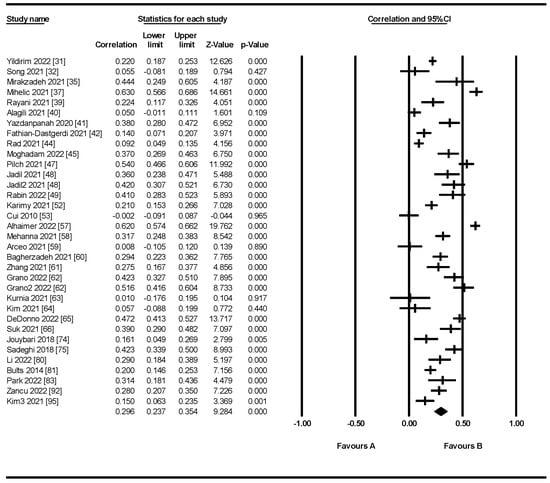
Figure 3.
The correlation between perceived severity and coping behavior. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
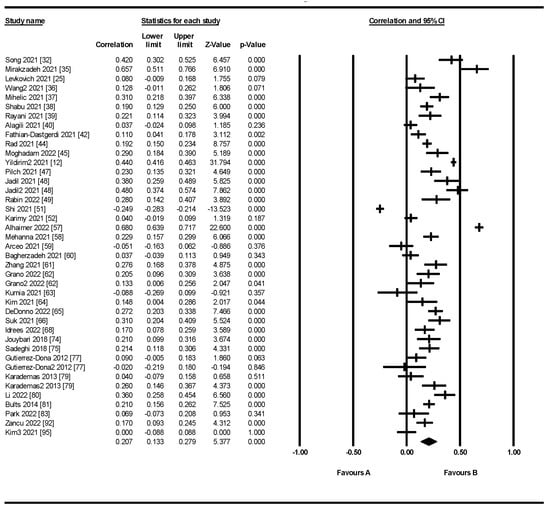
Figure 4.
The correlation between perceived susceptibility and coping behavior. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
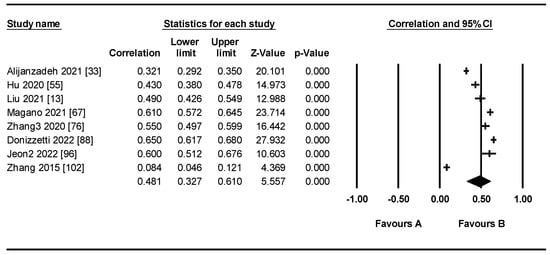
Figure 5.
The correlation between risk perception and fear. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
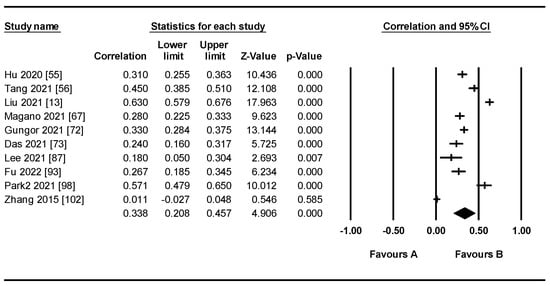
Figure 6.
The correlation between risk perception and anxiety. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
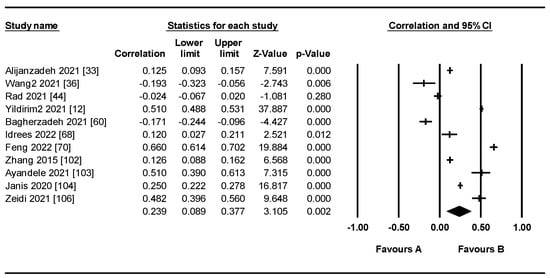
Figure 7.
The correlation between fear and coping behavior. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
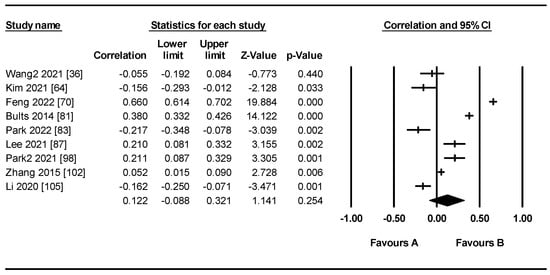
Figure 8.
The correlation between anxiety and coping behavior. The columns of the figure as labeled above in the figure represent the following: study, correlation, upper limit, lower limit, Z-value, p-value, correlation, and 95% CI. Favors A indicates the degree of negative correlation between the two factors. Favors B indicates the degree of positive correlation.
The results indicate that risk perception, perceived susceptibility, perceived severity, and fear were significant predictors of coping behavior. The effect sizes of anxiety and coping behavior were not statistically significant. Perceived severity had the strongest relationship with coping behavior, followed by perceived susceptibility and risk perception. For emotion, risk perception was significantly and positively associated with fear and anxiety. Risk perception had the strongest relationship with fear, followed by anxiety.
3.3. Publication Bias Test
Review studies based on empirical results are often prone to publication bias because the effect values of meta-analyses are determined and influenced by the data included in the study. For publication, authors and journal editors may prefer studies that are statistically significant, resulting in the omission of studies that have smaller effect sizes, which is why publication bias exists. In this study, quantitative tests for publication bias were conducted using the fail-safe number, Begg’s test, and Egger’s test.
For a meta-analysis process under a certain relationship, if the meta-analysis process includes the study data of X, the number of fail-safes must be much greater than 5X to indicate that there is no publication bias [107]. Egger’s test is the most commonly used test for publication bias. When the intercept term of Egger’s regression is not significant, it indicates that there is no publication bias [108]. Begg’s test determines the existence of publication bias by testing the correlation between the effect and sample size [109].
The number of insecurities under the meta-analysis process for each relationship in this study is shown in the table below, all of which satisfy this condition, indicating that there is no publication bias. The results of Begg’s test were not significant, with p-values greater than 0.05, indicating that the results show no publication bias; the intercept terms of the Egger regressions under all relationships except for risk perception–anxiety and negative emotion–behavior were not significant, and the intercepts and 95% confidence intervals are shown in Table 4, further supporting the absence of publication bias in these studies. Due to the small number of included studies, the results of the meta-analysis studies of the risk perception–anxiety relationship under Egger regression were significant with a p-value of less than 0.05; publication bias was present, but the results did not change significantly in the follow-up sensitivity test, indicating that publication bias did not have a significant effect on the results.

Table 4.
Publication bias test.
3.4. Sensitivity Analyses
The samples used in the meta-analysis were individual studies, and outliers may occur. Sensitivity analysis was performed using the leave-one-out method [110] to observe changes in effect sizes and 95% confidence intervals. One study was removed at a time, and a meta-analysis of the remaining studies yielded multiple combined effect sizes with the intervals shown in Table 5. None of the total effect estimates after removing a study exceeded the upper and lower 95% confidence interval limits of all study estimates, indicating that the results were robust.

Table 5.
Sensitivity analysis.
4. Discussion
To examine the relationship between risk perception, emotion, and behavior in the context of public health events, this meta-analysis quantitatively synthesized the results of 86 relevant studies. The results of the random effects model showed positive correlations between risk perception, perceived severity, perceived susceptibility, fear, and coping behavior. These results were highly statistically significant. Only the combined correlation coefficient between anxiety and coping behavior was statistically insignificant. The following findings can be confirmed. The higher the individual’s risk perception of a public health event, the more actively the individual takes precautions with non-pharmacological interventions. Risk perception, as the primary evaluation of a public health emergency, is a key factor in the emotional response and determines the individual’s emotional feelings. Fear can increase alertness and trigger coping behaviors. We performed a quantitative test for publication bias and found no significant publication bias. Sensitivity analysis was used to test the robustness of the results. This study also provides various theoretical and practical implications that can provide suggestions for future research and government interventions.
4.1. Theoretical and Practical Implications
This study offers multiple theoretical implications. First, it synthesizes the results of 86 studies to reveal the link between risk perception, emotions, and behaviors in the context of public health events. These included cross-sectional studies that looked at people’s performance across dimensions and the relationships that existed between them. The relationship between the two or the three phenomena is explored in depth. However, research into combining them to gain in-depth knowledge is limited. These studies were conducted in a piecemeal fashion rather than in a systematic way. This meta-analysis provides strong support for the relationship between risk perception, emotion, and behavior. This meta-analysis provides strong support for the relationship between risk perception, emotion, and behavior, and provides a theoretical tool for studying individuals’ coping behaviors in the face of a pandemic. Second, by combing and analyzing previous studies, we have identified some research gaps, which will help provide scholars with ideas for conducting subsequent studies. In the studies we have included, the regions covered are biased toward Asia, followed by European countries, with relatively few studies in Africa, the Americas, etc. This may be due to the different research hotspots preferred by scholars in different countries because of their different cultural backgrounds. Different cultural backgrounds do have an impact on the associations between risk perception, emotions, and coping behaviors [111,112]. The moderating role of cultural elements such as individualism and collectivism could be studied in the future. Third, religious beliefs deserve to be taken into account in future research. Different countries have different dominant religious beliefs. Religious beliefs have been associated with emotional well-being and healthy behaviors [113]. Religious beliefs can also be added as a moderating factor. Fourth, we are in the post-pandemic era as the pandemic progresses and policies change. Psychological mechanisms may change across different time periods. Anderson et al. found that fear of COVID-19 did not appear to predict COVID-19 prevention behavior 6 months after initial measurement [114]. Future studies should rigorously test these associations longitudinally and should consider alternative approaches to long-term public health prevention campaigns.
This study also provides key insights from a practical perspective that will help in the development of practical applications. Increased risk perception will motivate people to adopt coping behaviors. The government needs to adjust the public’s risk perception in comparison to the actual disease risk. However, it is worth noting that risk perception is related to populations, individuals, geography, and time [115]. In China, people tend to trust the government’s advice more and obey the government’s guidance. In contrast, in countries where government trust is low, the public tends to be less motivated to adopt coping behaviors because of other factors. In our study, perceived severity plays a greater role in promoting the adoption of health behaviors. However, this can lead to negative emotions such as fear and anxiety. Negative emotions such as fear will motivate people to take precautionary measures, but excessive negative emotions will lead to irrational behavior [3]. Thus, the intervention has to be adapted to the local context and also consider the gap between perceptions and the actual situation. Different governments should assess the gap between individual perception and actual disease severity, as well as the current emotional state. By considering different focuses for risk communication, governments can reasonably intervene in the public’s perception of disease severity to promote the adoption of self-protective behaviors.
For intervention, the direction of entry is the monitoring and adjustment of information sources. The public’s risk perception and emotions are greatly influenced by the sources of information to which individuals are exposed [116,117]. The media is the main channel of information dissemination and should report the development of events objectively and positively so that the public can form reasonable risk judgments and thus establish a correct risk perception. The use of social media influences users’ risk perception through negative sentiment mediation [118]. At high risk perception levels, the public will seek more emotional support from social support systems and vent their emotions in multiple ways [119]. Currently, technologies such as artificial intelligence and big data have become important forces in the field of public management. In response to the public’s emotional expression through social media such as Twitter and Facebook, natural language processing tools for artificial intelligence and text mining technology can be used to build a monitoring system to understand the public’s current situation and response to intervention strategies. Management can develop better public policy strategies based on the public’s identified level of risk perception and changes in sentiment. Inefficient prevention behaviors should be avoided to prevent too low negative emotions and risk perception as well as too high negative sentiment, which can influence larger public opinion. In addition, rumors on social media influence public sentiment through emotional infection, leading to irrational behavior. Managers can use big data technology and specific artificial intelligence algorithms to establish a rumor assessment and graded warning system [120]. By performing rapid response actions to address rumors, their spread can be curbed. Effective risk information communication is essential for establishing correct risk perception and reducing the generation and spread of panic and anxiety. Timely and accurate information disclosure is particularly important for effective risk communication [121]. Managers can use blockchain technology and big data technology for information disclosure platform development to accurately, openly, and transparently release epidemic/pandemic information and respond to public concerns.
4.2. Strengths
To the best of our knowledge, this is the first study to conduct a quantitative meta-analysis of the relationship between risk perception, negative emotions, and coping behaviors based on the context of a public health event. Wang et al. and Teasdale et al. conducted a qualitative systematic evaluation [15,122], but they lacked comprehensive data results to support their findings. Brewer et al. conducted a meta-analysis of the relationship between risk perception and health behavior in the context of vaccination, a pharmacological intervention [123]. This was not conducted for non-pharmacological preventive behaviors. Our study is novel and complements quantitative meta-analyses of the relationship between risk, emotion, and coping behavior in the context of public health events.
In addition, this study proposed future research directions from the perspectives of culture, religion, and time. Further research could focus on a meta-analysis of these possible behavioral determinants or moderators for a more comprehensive understanding of public health protective behaviors during a pandemic. We also suggest practical applications based on our findings, including risk communication and emotion monitoring through big data algorithms or artificial intelligence.
4.3. Limitations
In this study, when searching for studies in major popular electronic databases, the keywords used may not reach all of the relevant literature, and some relevant studies may be missed as a result. In addition, studies in other electronic databases may have been overlooked. Since journals tend to publish studies with significant findings, some studies with insignificant results may be omitted. Thus, we tried to discover whether there was any publication bias in our study. No significant publication bias was found to exist among the included studies.
Pre-published papers were not taken into account considering the quality of the study. Additionally, some relevant studies may have been missed due to limited key search terms. These factors resulted in the relatively low number of studies we included. As such relevant studies accumulate, future reviews should include more research to further validate the results. The advent of the post-pandemic era and changes in policy may lead to changes in the strength of these linkage effects. More comprehensive studies are needed.
5. Conclusions
This study used meta-analysis to evaluate the correlation between risk perception, negative emotions, and coping behaviors in the context of the current COVID-19 pandemic and other public health events. Individual risk perception, especially perceived severity, can prompt people to perform coping actions. High risk perception will lead to negative emotions such as fear and anxiety. Fear predicts the adoption of coping behaviors. This provides a theoretical reference for practical health behavior interventions. The magnitude and direction of effects between relationships may vary across cultures, religions, and time periods. For future research, the moderating role of these factors should be considered.
Author Contributions
Study conception and design: W.Z. and Y.Z. (Yanchun Zhu ); data acquisition: Y.Z. (Yuxia Zhao) and Y.J.; data analysis and/or interpretation: Y.Z. (Yuxia Zhao), manuscript drafting: Y.Z. (Yuxia Zhao), W.Z. and Y.Z. (Yanchun Zhu); critical manuscript revision for important intellectual content: W.Z., Y.Z. (Yuxia Zhao), Y.Z. (Yanchun Zhu) and Y.J. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the National Natural Science Foundation of China (Grant number: 72061147005, 71874215, 72004244, 71571191), the National Social Science Foundation of China (Grant number: 21BZZ108), the Beijing Natural Science Foundation (Grant number: 9182016, 9194031), the MOE (Ministry of Education in China) Project of Humanities and Social Sciences (Grant number: 17YJAZH120, 19YJCZH253), the Fundamental Research Funds for the Central Universities (SKZZY2015021), and Political Education Special Fund in Central University of Finance and Economics (“Diffusion mechanism and synergistic analysis of epidemic prevention policies during COVID-19 epidemics”, SZJ2208).
Informed Consent Statement
Not applicable.
Data Availability Statement
The extracted data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO Estimates of Excess Mortality Associated with the COVID-19 Pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Dawood, F.S.; Iuliano, A.D.; Reed, C.; Meltzer, M.I.; Shay, D.K.; Cheng, P.-Y.; Bandaranayake, D.; Breiman, R.F.; Brooks, W.A.; Buchy, P.; et al. Estimated Global Mortality Associated with the First 12 Months of 2009 Pandemic Influenza A H1N1 Virus Circulation: A Modelling Study. Lancet Infect. Dis. 2012, 12, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Wang, M. Evolution of management of emergency protective materials for mass panic in the context of public health emergencie. Oper. Res. Trans. 2023, 27, 30–42. [Google Scholar]
- Xi, J.; Wang, Y.; Ju, K. Psychological intervention in major public health emergencies from the perspective of positive psychology. J. Cap. Norm. Univ. 2022, 50, 181–187. [Google Scholar]
- Zhao, G.; Wang, Y.G.; Wang, Y.Q.; Cao, R.F.; Fu, S.F. Psychological Crisis Intervention in Disasters: Comment on Psychiatric View. Adv. Psychol. Sci. 2009, 17, 489–494. [Google Scholar]
- Shi, K. Research and Thinking on Socio-psychological Early Warning System of Disaster and Major Events in China. Manag. Rev. 2003, 15, 18–22. [Google Scholar]
- Zhang, N.; Zhang, S.W. Emergent Management Strategies during Public Health Emergency: Perspectives from Behavioral Sciences. J. Comp. Econ. Soc. Syst. 2020, 36, 25–34. [Google Scholar]
- Brug, J.; Oenema, A.; Ferreira, I. Theory, evidence and Intervention Mapping to improve behavior nutrition and physical activity interventions. Int. J. Behav. Nutr. Phy. 2005, 2, 2. [Google Scholar] [CrossRef]
- Brug, J.; Aro, A.R.; Richardus, J.H. Risk Perceptions and Behaviour: Towards Pandemic Control of Emerging Infectious Diseases: International Research on Risk Perception in the Control of Emerging Infectious Diseases. Int. J. Behav. Med. 2009, 16, 3–6. [Google Scholar] [CrossRef]
- Dolan, R.J. Emotion, Cognition, and Behavior. Science 2002, 298, 1191–1194. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- Yıldırım, M.; Geçer, E.; Akgü, Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2021, 26, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Duong, H.T.; Nguyen, H.T. Media exposure and intentions to wear face masks in the early stages of the COVID-19 outbreak: The mediating role of negative emotions and risk perception. Atl. J. Commun. 2021, 30, 467–480. [Google Scholar] [CrossRef]
- Zhang, W.; Li, L.; Mou, J.; Zhang, M.; Cheng, X.; Xia, H. Mediating Effects of Attitudes, Risk Perceptions, and Negative Emotions on Coping Behaviors: Evidence From a Survey of Older Chinese Adults. J. Organ. End User Com. 2022, 34, 1–22. [Google Scholar] [CrossRef]
- Teasdale, E.; Santer, M.; Geraghty, A.W.A.; Little, P.; Yardley, L. Public Perceptions of Non-Pharmaceutical Interventions for Reducing Transmission of Respiratory Infection: Systematic Review and Synthesis of Qualitative Studies. BMC Public Health 2014, 14, 589. [Google Scholar] [CrossRef]
- Parsons, J.E.; Newby, K.V.; French, D.P. Do Interventions Containing Risk Messages Increase Risk Appraisal and the Subsequent Vaccination Intentions and Uptake?—A Systematic Review and Meta-Analysis. Br. J. Health Psychol. 2018, 23, 1084–1110. [Google Scholar] [CrossRef]
- Liu, M.; Zhang, H.; Huang, H. Media Exposure to COVID-19 Information, Risk Perception, Social and Geographical Proximity, and Self-Rated Anxiety in China. BMC Public Health 2020, 20, 1649. [Google Scholar] [CrossRef]
- Mahmood, S.; Hussain, T.; Mahmood, F.; Ahmad, M.; Majeed, A.; Beg, B.M.; Areej, S. Attitude, Perception, and Knowledge of COVID-19 Among General Public in Pakistan. Front. Public Health 2020, 8, 602434. [Google Scholar] [CrossRef]
- Li, J.B.; Yang, A.; Dou, K.; Wang, L.X.; Zhang, M.C.; Lin, X.Q. Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: A national survey. BMC Public Health 2020, 20, 1589. [Google Scholar] [CrossRef]
- Cheng, C.; Espanha, R. Association of Sina-microblog Use with Knowledge, Attitude and Practices Towards COVID-19 Control in China. Open Access J. Public Health 2021, 4, 7. [Google Scholar]
- Lyu, X.; Hu, J.; Xu, X.; Xianyu, Y.; Dong, W. Factors influencing risk perception and nosocomial infection prevention practices of frontline nurses during the COVID-19 pandemic. BMC Nurs. 2021, 20, 78. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.P.; Shi, K. Comparative Study on Risk Perception and Coping Behavior of Beijing Residents During SARS Period. Chin. J. Clin. Psychol. 2004, 12, 293–295+298. [Google Scholar]
- Kim, Y.; Zhong, W.; Jehn, M.; Walsh, L. Public Risk Perceptions and Preventive Behaviors During the 2009 H1N1 Influenza Pandemic. Disaster Med. Public 2015, 9, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.N.; Zhang, Y.C.; Wu, R.K.; Li, B.; Li, C.W.; Yu, B.T.; Zhang, Y.L. A study of self-precaution against the background of the COVID-19 pandemic from the perspective of risk perception attitude theory and social support. BMC Public Health 2021, 21, 1527. [Google Scholar] [CrossRef]
- Levkovich, I.; Shinan-Altman, S. The Impact of Gender on Emotional Reactions, Perceived Susceptibility and Perceived Knowledge about COVID-19 among the Israeli Public. Int. Health 2021, 13, 555–561. [Google Scholar] [CrossRef]
- Shen, F.; Min, C.; Lu, Y.; Chu, Y. The Effect of Cognition and Affect on Preventive Behaviors during the COVID-19 Pandemic: A Cross-Sectional Study in China. BMC Public Health 2021, 21, 722. [Google Scholar] [CrossRef]
- Hedges, L.V.; Vevea, J.L. Fixed- and Random-Effects Models in Meta-Analysis. Psychol. Methods 1998, 3, 486–504. [Google Scholar] [CrossRef]
- Rupinski, M.T.; Dunlap, W.P. Approximating Pearson product-moment correlations from Kendall’s tau and Spearman’s rho. Educ. Psychol. Meas. 1996, 56, 419–429. [Google Scholar] [CrossRef]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index. Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef]
- Lipsey, M.W.; Wilson, D.B. The way in which intervention studies have “personality” and why it is important to meta-analysis. Eval. Health Prof. 2001, 24, 236–254. [Google Scholar]
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2022, 46, 979–986. [Google Scholar] [CrossRef]
- Song, E.; Lee, J.E.; Kwon, S. Effect of Public Empathy with Infection-Control Guidelines on Infection-Prevention Attitudes and Behaviors: Based on the Case of COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 13408. [Google Scholar] [CrossRef] [PubMed]
- Alijanzadeh, M.; Ahorsu, D.K.; Alimoradi, Z.; Mahmoudi, N.; Griffiths, M.D.; Lin, C.Y.; Liu, H.K.; Pakpour, A.H. Fear of COVID-19 and Trust in the Healthcare System Mediates the Association between Individual’s Risk Perception and Preventive COVID-19 Behaviours among Iranians. Int. J. Environ. Res. Public Health 2021, 18, 12146. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.; Chen, J.; Chow, K.M.; Law, B.M.H.; Chan, D.N.S.; So, W.K.W.; Leung, A.W.Y.; Chan, C.W.H. Knowledge, Attitudes and Practices Towards COVID-19 Amongst Ethnic Minorities in Hong Kong. Int. J. Environ. Res. Public Health 2020, 17, 7878. [Google Scholar] [CrossRef] [PubMed]
- Mirakzadeh, A.A.; Karamian, F.; Khosravi, E.; Parvin, F. Analysis of Preventive Behaviors of Rural Tourism Hosts in the Face of COVID-19 Pandemic: Application of Health Belief Model. Front. Public Health 2021, 9, 793173. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Rao, N.; Han, B. Pathways Improving Compliance with Preventive Behaviors during the Remission Period of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3512. [Google Scholar] [CrossRef] [PubMed]
- Mihelič, A.; Jelovčan, L.; Prislan, K. Internal and external drivers for compliance with the COVID-19 preventive measures in Slovenia: The view from general deterrence and protection motivation. PLoS ONE 2021, 16, e0259675. [Google Scholar] [CrossRef] [PubMed]
- Shabu, S.A.; M-Amin, K.; Mahmood, K.I.; Shabila, N.P. Risk Perception and Behavioral Response to COVID-19: A Survey of University Students and Staff in the Iraqi Kurdistan Region. Soc. Work Public Health 2021, 36, 474–485. [Google Scholar] [CrossRef]
- Rayani, M.; Rayani, S.; Najafi-Sharjabad, F. COVID-19-related knowledge, risk perception, information seeking, and adherence to preventive behaviors among undergraduate students, southern Iran. Environ. Sci. Pollut. Res. 2021, 28, 59953–59962. [Google Scholar] [CrossRef]
- Alagili, D.E.; Bamashmous, M. The Health Belief Model as an explanatory framework for COVID-19 prevention practices. J. Infect. Public Health 2021, 14, 1398–1403. [Google Scholar] [CrossRef]
- Yazdanpanah, M.; Abadi, B.; Komendantova, N.; Zobeidi, T.; Sieber, S. Some at Risk for COVID-19 Are Reluctant to Take Precautions, but Others Are Not: A Case From Rural in Southern Iran. Front. Public Health 2020, 8, 562300. [Google Scholar] [CrossRef] [PubMed]
- Fathian-Dastgerdi, Z.; Khoshgoftar, M.; Tavakoli, B.; Jaleh, M. Factors associated with preventive behaviors of COVID-19 among adolescents: Applying the health belief model. Res. Soc. Admin. Pharm. 2021, 17, 1786–1790. [Google Scholar] [CrossRef] [PubMed]
- Iorfa, S.K.; Ottu, I.F.A.; Oguntayo, R.; Ayandele, O.; Kolawole, S.O.; Gandi, J.C.; Dangiwa, A.L.; Olapegba, P.O. COVID-19 Knowledge, Risk Perception, and Precautionary Behavior Among Nigerians: A Moderated Mediation Approach. Front. Psychol. 2020, 11, 566773. [Google Scholar] [CrossRef] [PubMed]
- Ezati Rad, R.; Mohseni, S.; Kamalzadeh Takhti, H.; Hassani Azad, M.; Shahabi, N.; Aghamolaei, T.; Norozian, F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: A cross-sectional study. BMC Public Health 2021, 21, 466. [Google Scholar] [CrossRef] [PubMed]
- Tajeri Moghadam, M.; Zobeidi, T.; Sieber, S.; Löhr, K. Investigating the Adoption of Precautionary Behaviors Among Young Rural Adults in South Iran During COVID-19. Front. Public Health 2022, 10, 787929. [Google Scholar] [CrossRef]
- Xie, K.; Liang, B.; Dulebenets, M.A.; Mei, Y. The Impact of Risk Perception on Social Distancing during the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 6256. [Google Scholar] [CrossRef]
- Pilch, I.; Wardawy, P.; Probierz, E. The predictors of adaptive and maladaptive coping behavior during the COVID-19 pandemic: The Protection Motivation Theory and the Big Five personality traits. PLoS ONE 2021, 16, e0258606. [Google Scholar] [CrossRef]
- Jadil, Y.; Ouzir, M. Exploring the predictors of health-protective behavior during the COVID-19 pandemic: A multi-country comparison. Environ. Res. 2021, 199, 111376. [Google Scholar] [CrossRef]
- Rabin, C.; Dutra, S. Predicting engagement in behaviors to reduce the spread of COVID-19: The roles of the health belief model and political party affiliation. Psychol. Health Med. 2022, 27, 379–388. [Google Scholar] [CrossRef]
- Batra, K.; Urankar, Y.; Batra, R.; Gomes, A.F.; Kaurani, P. Knowledge, Protective Behaviors and Risk Perception of COVID-19 among Dental Students in India: A Cross-Sectional Analysis. Healthcare 2021, 9, 574. [Google Scholar] [CrossRef]
- Shi, G.; Zhong, X.; He, W.; Liu, H.; Liu, X.; Ma, M. Factors influencing protective behavior in the post-COVID-19 period in China: A cross-sectional study. Environ. Health Prev. Med. 2021, 26, 95. [Google Scholar] [CrossRef] [PubMed]
- Karimy, M.; Bastami, F.; Sharifat, R.; Heydarabadi, A.B.; Hatamzadeh, N.; Pakpour, A.H.; Cheraghian, B.; Zamani-Alavijeh, F.; Jasemzadeh, M.; Araban, M. Factors related to preventive COVID-19 behaviors using health belief model among general population: A cross-sectional study in Iran. BMC Public Health 2021, 21, 1934. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Jeon, M.J.; Lim, M.H. A study on knowledge of influenza A(H1N1) and preventive behavior in the midst of the spread of the flu. J. Korean Soc. Dent. Hyg. 2010, 10, 567–576. [Google Scholar]
- Choi, J.S.; Kim, K.M. Infection-control knowledge, attitude, practice, and risk perception of occupational exposure to Zika virus among nursing students in Korea: A cross-sectional survey. J. Infect. Public Health 2018, 11, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Wang, Q.; Chen, H.L.; Jiang, Y.H. Relationship between Risk Perception and Unintentional/Intentional Rumor Spread Behavior during The COVID-19 Pneumonia Outbreak in China: The Mediating Role of Negative Emotion. Chin. J. Clin. Psychol. 2020, 28, 734–738. [Google Scholar]
- Tang, X.M.; Lai, S.Q. Research on the Online Health Rumor Forwarding in Public Health and Safety Incidents—The Interaction of Perceived Risk and Information Credibility. J. Intell. 2021, 40, 101–107. [Google Scholar]
- Alhaimer, R. The health belief model: Evaluating governmental public health messages on social media aimed at preventing a COVID-19 epidemic in Kuwait. Cogent. Bus. Manag. 2022, 9, 2031682. [Google Scholar] [CrossRef]
- Mehanna, A.; Elhadi, Y.A.M.; Lucero-Prisno Iii, D.E. Public willingness to adhere to COVID-19 precautionary measures in Sudan: An application of the Health Belief Model. Pan Afr. Med. J. 2021, 39, 135. [Google Scholar] [CrossRef]
- Arceo, E.; Jurado, J.E.; Cortez, L.A.; Sibug, N.; Sarmiento, G.L.; Lawingco, A.C.; Carbungco, C.; Tiongco, R.E. Understanding COVID-19 preventive behavior: An application of the health belief model in the Philippine setting. J. Educ. Health Promot. 2021, 10, 228. [Google Scholar]
- Bagherzadeh, M.; Salehi, L.; Mahmoodi, Z. Investigating preventive health behaviors against COVID-19 in elementary school students’ parents: A cross-sectional study from Tehran—Capital of Iran. J. Educ. Health Promot. 2021, 10, 435. [Google Scholar]
- Zhang, Y.; Young, L.S. A Study on the Factors Influencing the Intention to Continue COVID-19 Preventive Behavior: Focusing on the Health Belief Model (HBM), Media/interpersonal Information Exposure, Negative Emotions, and Interdependent Self-construal. J. Speech Media Commun. Res. 2021, 20, 315–348. [Google Scholar] [CrossRef]
- Grano, C.; Singh, S.C.; Di, P.A. Predictors of protective behaviours during the Italian COVID-19 pandemic: An application of protection motivation theory. Psychol. Health 2022, 37, 1584–1604. [Google Scholar] [CrossRef] [PubMed]
- Kurnia, A.D.; Masruroh, N.L.; Melizza, N.; Rofi’i, A.Y. Factors associated with preventive behaviors of COVID-19 among Indonesian nursing students: Application of Health Belief Model. Russ. Open Med. J. 2021, 10, e0201. [Google Scholar] [CrossRef]
- Kim, S.J.; Kim, E.Y.; Yang, H.R.; Chae, Y.J. Gyeongnam Inhabitants’ Effects of COVID-19 Infection Prevention Behavior: Focus on Anxiety and Health Belief. J. Korean Public Health Nurs. 2021, 35, 19–32. [Google Scholar]
- DeDonno, M.A.; Longo, J.; Levy, X.; Morris, J.D. Perceived Susceptibility and Severity of COVID-19 on Prevention Practices, Early in the Pandemic in the State of Florida. J. Community Health 2022, 47, 627–634. [Google Scholar] [CrossRef]
- Song, H.S.; Bang, S.H.; Shim, G.S.; Kim, E.M. An Analysis of COVID-19 Prevention Behaviors between Firefighters and Maritime Police Officers. J. Korea Soc. Comput. Inf. 2021, 26, 213–220. [Google Scholar]
- Magano, J.; Vidal, D.G.; Sousa, H.F.P.e.; Dinis, M.A.P.; Leite, Â. Psychological Factors Explaining Perceived Impact of COVID-19 on Travel. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 1120–1133. [Google Scholar] [CrossRef]
- Idrees, M.; Asif, M.; Ghazal, S. Effect of Risk Perceptions, Fear and myths about COVID-19 infection susceptibility on Protective behaviors in Pakistan. Asean J. Psychiatr. 2022, 23, 1–8. [Google Scholar]
- Elsayed, E.A. Impact of COVID-19 risk perception on compliance with preventive measures among adult Egyptians. Med. Sci. 2022, 26, ms65e1826. [Google Scholar] [CrossRef]
- Feng, Y.; Tong, Q. Exploring the Mediating Role of Situation Awareness and Crisis Emotions Between Social Media Use and COVID-19 Protective Behaviors: Cross-Sectional Study. Front. Public Health. 2022, 10, 793033. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, R. Promoting social distancing and preventing panic buying during the epidemic of COVID-19: The contributions of people’s psychological and behavioural factors. J. Public Health 2023, 31, 187–201. [Google Scholar] [CrossRef] [PubMed]
- Güngör, A.; Brahim Sarı, H.; Asıcı, E. Health Anxiety in the Early Phase of COVID-19 Outbreak in Turkey: Investigation of Predictive Variables. Ansiedad Estrés 2021, 27, 74–80. [Google Scholar] [CrossRef]
- Das, D.; Pal, S. Do Socio-Demographic and Corona Reassurance-Seeking Behaviour Predict Corona Anxiety?—A study among Indian population. Asia-Pac. J. Health Manag. 2021, 16, 86–93. [Google Scholar] [CrossRef]
- Jouybari, T.A.; Hatamzadeh, N.; Fattahi, M.; Gharibnavaz, H.; Khashij, S.; Mahboubi, M. Cognitive Determinants of Influenza Preventive Behaviors among Students: An Application of the Health Belief Model (HBM). Int. J. Pediatr. 2018, 6, 7833–7841. [Google Scholar]
- Sadeghi, R.; Khanjani, N.; Naghibzadeh-Tahami, A.; Kakolaki, Z.K. Education of Iranian Pregnant Women About Prevention of Influenza A. Int. J. Women’s Health Reprod. Sci. 2017, 6, 321–327. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, H.; Cheng, P.; Luqman, A. Predicting consumers’ intention to consume poultry during an H7N9 emergency: An extension of the theory of planned behavior model. Hum. Ecol. Risk Assess. 2020, 26, 190–211. [Google Scholar] [CrossRef]
- Gutiérrez-Doña, B.; Renner, B.; Reuter, T.; Giese, H.; Schubring, D. Health Behavior Education, e-research and a (H1N1) Influenza (Swine Flu): Bridging the Gap between Intentions and Health Behavior Change. Procedia-Soc. Behav. Sci. 2012, 46, 2782–2795. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.Y.; Tang, C.S.K. Practice of habitual and volitional health behaviors to prevent severe acute respiratory syndrome among Chinese adolescents in Hong Kong. J. Adolesc. Health 2005, 36, 193–200. [Google Scholar] [CrossRef]
- Karademas, E.C.; Bati, A.; Karkania, V.; Georgiou, V.; Sofokleous, S. The association between Pandemic Influenza A (H1N1) public perceptions and reactions: A prospective study. J. Health Psychol. 2013, 18, 419–428. [Google Scholar] [CrossRef]
- Li, P.P.; Zhong, F. A Study on the Correlation Between Media Usage Frequency and Audiences’ Risk Perception, Emotion and Behavior. Front. Psychol. 2022, 12, 822300. [Google Scholar] [CrossRef]
- Bults, M.; Beaujean, D.; Wijkmans, C.; Richardus, J.H.; Voeten, H. Q fever in the Netherlands: Public perceptions and behavioral responses in three different epidemiological regions: A follow-up study. BMC Public Health 2014, 14, 263. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Choi, J.S. Middle East respiratory syndrome-related knowledge, preventive behaviours and risk perception among nursing students during outbreak. J. Clin. Nurs. 2016, 25, 2542–2549. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.M.; Kim, J.Y. Predictors of Respiratory Infection Prevention Behavoirs of Nursing College Students. J. Korea Acad.-Ind. Cooper. Soc. 2022, 23, 134–145. [Google Scholar]
- Borges, J.; Byrne, M. Investigating COVID-19 risk perception and preventive behaviours in third-level students in Ireland. Acta Psychol. 2022, 224, 103535. [Google Scholar] [CrossRef] [PubMed]
- Kwak, S.J.; Kim, N.Y. Media Dependence of Nursing Students on COVID-19-Related Infection Prevention Behavior: Mediating Effect of Risk Perception. Korean J. Adul. Nurs. 2021, 33, 630–638. [Google Scholar] [CrossRef]
- Kim, H.; Cheon, E.Y.; Yoo, J.H. A Study on the Relationship between Knowledge, Risk Perception, Preventive Health Behavior from Coronavirus disease-2019 in Nursing Students. J. Korea Acad.-Ind. Cooper. Soc. 2021, 22, 246–254. [Google Scholar]
- Lee, S.J.; Jin, X.; Lee, S. Factors Influencing COVID-19 Preventive Behaviors in Nursing Students: Knowledge, Risk Perception, Anxiety, and Depression. J. Korean Biol. Nurs. Sci. 2021, 23, 110–118. [Google Scholar] [CrossRef]
- Donizzetti, A.R.; Lagacé, M. COVID-19 and the Elderly’s Mental Illness: The Role of Risk Perception, Social Isolation, Loneliness and Ageism. Int. J. Environ. Res. Public Health 2022, 19, 4513. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.R.; Choi, E.Y.; Park, S.Y.; Kim, E.A. Factors Influencing Preventive Behavior against Coronavirus Disease 2019 (COVID-19) among Medically Inclined College Students. J. Korean Acad. Fund Nurs. 2020, 27, 428–437. [Google Scholar] [CrossRef]
- Kyung, L.H.; Kang, N.G.; Kim, S.H.; Kim, M.S.; Nam, Y.N.; Noh, S.H.; Lee, H.D.; Jung, D.U.; Joo, S.H.; Choi, S.R. Effect of nursing students’ knowledge of COVID-19 and risk perception on COVID-19 prevention behavior. J. Ind. Converg. 2021, 19, 29–137. [Google Scholar]
- Jeon, S.W.; Han, S.J. Factors Influencing Hospital Nurses’ COVID-19 Prevention Behaviors. J. Korea Converg. Soc. 2021, 12, 583–594. [Google Scholar]
- Zancu, S.A.; Măirean, C.; Diaconu-Gherasim, L.R. The longitudinal relation between time perspective and preventive behaviors during the COVID-19 pandemic: The mediating role of risk perception. Curr. Psychol. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fu, H.; Wang, B. The Effect of Risk Perception on Anxiety in Emerging Adulthood Under the Local Outbreak of COVID-19: A Conditional Process Analysis. Front. Psychol. 2022, 13, 759510. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.J.; Park, J.H.; Kim, H.S. Effects of Information Literacy, Risk Perception and Crisis Communication Related to COVID-19 on Preventive Behaviors of Nursing Students in Clinical Practice. J. Converge. Inf. Technol. 2022, 12, 66–74. [Google Scholar]
- Kim, Y.; Yoon, T.; Sohn, A. Effects of COVID-19 knowledge, risk perception, subjective norms, and perceived behavioral control on preventive action intentions and preventive action practices in college students. Korean J. Educ. Health Promot. 2021, 38, 25–36. [Google Scholar] [CrossRef]
- Jeon, E.B.; Baek, E.M.; Cho, S.I.; Jeong, Y. The Impact of Fear and Perception of Infection Risk on Depression among Service Workers during COVID-19. Korean J. Occup. Health Nurs. 2022, 31, 1–10. [Google Scholar]
- Park, M.; Chai, S. The Effects of COVID-19 Risk Information Seeking and Processing on its Preventive Behaviors and Information Sharing. J. Inf. Technol. Serv. 2020, 19, 65–81. [Google Scholar]
- Park, J.H.; Kim, J.H.; Lee, H.J.; Kang, P. The Relationship of Anxiety, Risk Perception, Literacy, and Compliance of Preventive Behaviors during COVID-19 Pandemic in Nursing Students. J. Korean Appl. Sci. Technol. 2021, 38, 48–59. [Google Scholar]
- Lee, C.K.; Jung, E.K.; Kang, S.E.; Petrick, J.F.; Park, Y.N. Impact of perception of COVID-19 on NPI, job satisfaction, and customer orientation: Highlighting three types of NPIs for the airline industry. J. Air Transp. Manag. 2022, 100, 102191. [Google Scholar] [CrossRef]
- Lee, H.; Park, J.; Kim, J.; Kang, P. Factors Influencing University Students’ Infection Prevention Behaviors Compliance in the Early Stage of COVID-19. J. Korean Soc. Sch. Health 2021, 34, 190–199. [Google Scholar]
- Li, X.J.; Liu, Q.L. An Extended Model of Risk Transmission from the Perspective of Media Credibility—Based on the National Survey of COVID-19. Mod. Commun. 2021, 43, 33–40. [Google Scholar]
- Zhang, R.J.; Jiang, T.T.; Li, N. The negative psychology for the public in Zhejiang province during the epidemic of human H7N9 avian influenza. Chin. J. Prev. Med. 2015, 49, 1073–1079. [Google Scholar]
- Ayandele, O.; Ramos-Vera, C.A.; Iorfa, S.K.; Chovwen, C.O.; Olapegba, P.O. Exploring the Complex Pathways between the Fear of COVID-19 and Preventive Health Behavior among Nigerians: Mediation and Moderation Analyses. Am. J. Trop. Med. Hyg. 2021, 105, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Zickfeld, J.H.; Schubert, T.W.; Herting, A.K.; Grahe, J.; Faasse, K. Correlates of Health-Protective Behavior During the Initial Days of the COVID-19 Outbreak in Norway. Front. Psychol. 2020, 11, 564083. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, S.H.; Yu, R.H. Compliance of home quarantine protection and its effect on anxiety degree during the epidemic outbreak period of COVID-19. Chin. J. Control 2020, 19, 404–410. [Google Scholar]
- Zeidi, I.M.; Zeidi, B.M. Knowledge, Attitude, Fear, and Practice towards Coronavirus Disease-2019 Preventive Measures among Iranian Dentists. Iran. Red. Crescent. Me. 2021, 23, e778. [Google Scholar]
- Rosenthal, R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979, 86, 638–641. [Google Scholar] [CrossRef]
- Egger, M.; Davey, S.G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ-Clin. Res. Ed. 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Patsopoulos, N.A.; Evangelou, E.; Ioannidis, J.P.A. Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. Int. J. Epidemiol. 2008, 37, 1148–1157. [Google Scholar] [CrossRef]
- Shekriladze, I.; Javakhishvili, N.; Chkhaidze, N. Culture Related Factors May Shape Coping During Pandemics. Front. Psychol. 2021, 12, 634078. [Google Scholar] [CrossRef]
- Cho, H.; Lee, J.-S. The Influence of Self-Efficacy, Subjective Norms, and Risk Perception on Behavioral Intentions Related to the H1N1 Flu Pandemic: A Comparison between Korea and the US. Asian J. Soc. Psychol. 2015, 18, 311–324. [Google Scholar] [CrossRef]
- Kowalczyk, O.; Roszkowski, K.; Montane, X.; Pawliszak, W.; Tylkowski, B.; Bajek, A. Religion and Faith Perception in a Pandemic of COVID-19. J. Relig. Health 2020, 59, 2671–2677. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.M.; Stockman, J.K. Fear of COVID-19 and Prevention Behaviors: Cross-Lagged Panel Analysis. JMIR Form. Res. 2022, 6, e35730. [Google Scholar] [CrossRef] [PubMed]
- Cipolletta, S.; Andreghetti, G.R.; Mioni, G. Risk Perception towards COVID-19: A Systematic Review and Qualitative Synthesis. Int. J. Environ. Res. Public Health 2022, 19, 4649. [Google Scholar] [CrossRef]
- Fuentes, A.; Peterson, J.V. Social Media and Public Perception as Core Aspect of Public Health: The Cautionary Case of @realdonaldtrump and COVID-19. PLoS ONE 2021, 16, e0251179. [Google Scholar] [CrossRef]
- Abbas, J.; Wang, D.; Su, Z.; Ziapour, A. The Role of Social Media in the Advent of COVID-19 Pandemic: Crisis Management, Mental Health Challenges and Implications. Risk Manag. Healthc. Policy 2021, 14, 1917–1932. [Google Scholar] [CrossRef]
- Liu, Y.; Luo, D. The use of social media in public health emergencies and its impact on college students’ health behavior. New Media Res. 2021, 7, 19–24. [Google Scholar]
- Liu, F.; Chen, X.; Yuan, L. The relationship between risk perception and negative coping behaviors in public crisis events: Analysis of a moderated mediation model. Psychol. Mon. 2021, 16, 7–9+70. [Google Scholar]
- Mesquita, C.T.; Oliveira, A.; Seixas, F.L.; Paes, A. Infodemia, Fake News and Medicine: Science and The Quest for Truth. Int. J. Cardiovasc. Sci. 2020, 33, 203–205. [Google Scholar] [CrossRef]
- Zhang, L.; Li, H.; Chen, K. Effective Risk Communication for Public Health Emergency: Reflection on the COVID-19 (2019-NCoV) Outbreak in Wuhan, China. Healthcare 2020, 8, 64. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Zhang, A.H.; Feng, X.Q. Research progress on risk perception, emotion and behavior of the public under major emergencies. Chin. Nurs. Res. 2022, 36, 1803–1809. [Google Scholar]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).