1. Introduction
The concept of Lean Management (LM), derived from the practical sciences of production management, is increasingly used in other areas, including in the area of medicine. The application of the concept of Lean Management in medical facilities is referred to in the literature as Lean Hospitals.
The concept of Lean Hospitals, such as Lean Management, is aimed at avoiding and reducing waste in the processes carried out within the organization [
1]. It focuses on the reduction in operating costs in all aspects of the company’s operations. It helps determine what constitutes an appropriate added value for the client (the patient, in the case of Lean Hospitals) in order to create a culture of high quality and to constantly improve the processes and the organization [
2].
Lean Hospitals is a toolkit, a management system and a philosophy, which will allow a hospital to improve the quality of patient care by reducing errors and medical service waiting times. A lean system is a concept, which can support physicians and other healthcare professionals by eliminating inconveniences and allowing them to focus on those activities, which benefit treatment and care. It enables breaking down the barriers between separate hospital departments, allowing them to better cooperate for the benefit of the patient [
3]. As part of a Lean Hospital system, the following lean tools can be implemented: value stream mapping (VSM), standardized work (SW), 5S best practices (5S), visual management (VM), the Kanban system, employee involvement [
3,
4]. A similar set of tools and practices is presented by T. Zidel, supplementing the above set of tools with the basic assumptions of the Six Sigma methodology [
5].
Value stream mapping [
6] is one of the first steps of implementing the lean philosophy in organizations aspiring to it. It consists of a comprehensive analysis of the processes, looking for muda, which is waste [
7], consisting of [
1,
8,
9]
Overproduction,
Excessive stocks,
Defects,
Waiting,
Excessive motion,
Overprocessing,
Unused human potential.
The next step after verification of the process and identification of waste is to eliminate it using tools from the Lean Management concept. They include, among others, 5S good practices and work standardization [
10], which is the method of a well-organized work place; Kaizen [
3], which is a continuous improvement system used as part of quality improvement projects in accreditation in healthcare, where the actions undertaken have to be based on the Deming cycle [
11]; total productive maintenance (TPM), which ensures the continuity of care for the patient through proper management of the elements of building infrastructure and equipment; Kanban, which is a pull system for control over stock in the medical facility; visual management, an element of which features in all types of descriptions and markings, which accelerate the decision-making and organizational processes.
To identify the research gap, the most important research areas of the Lean Hospitals concept were listed. Publications by Polish and foreign authors in international journals were analyzed. As part of the literature review, the most important research areas of the Lean Hospitals concept were identified. They mainly concern the possibility of improving and perfecting the involvement of managerial staff in the continuous improvement process [
12,
13]; the possibility of assessing the implementation of the lean concept in hospitals [
14]; and the assessment of the degree of readiness of medical facilities to implement the lean concept [
15,
16,
17]. Studies of Lean Hospitals often focused on literature reviews and implementations of case studies [
18,
19,
20,
21,
22,
23,
24,
25,
26]. There is also a dominance of studies reporting successful lean interventions [
21,
27,
28,
29,
30,
31,
32,
33,
34,
35]. The positive aspects of implementation of LM tools refer both to the economic effects (lowering the unit costs, lowering the costs of studies), as well as organizational effects, such as improving the patient flow [
36,
37,
38,
39], shortening the waiting time for procedures [
22], reducing the number of unnecessary examinations or shortening the hospitalization time [
23,
37,
40], and human effects (increasing the engagement of employees, satisfaction from implemented improvements or change of the method of work from individual to team work) [
24,
41,
42,
43]. The latest study provides practical guidance to support the implementation of a cost-effective approach in hospital operations, with the study repeating and testing different processes in different healthcare units [
17,
44]. The others also focus on the impact of lean application on the quality of services provided, as assessed by patients [
42], and on the comparison of the degree of implementation of lean tools and the effects achieved in hospitals in individual countries [
17,
45].
In Poland and around the world, optimization of organizational processes in hospitals is taking place, including with the use of lean tools [
19,
40,
46]. An example of optimization in Polish conditions is the change in the way of working in the emergency departments in Pomeranian hospitals with usage of lean tools initiated by the Marshal’s Office of the Pomeranian region [
47] or a study on changing the patient flow in a hospital in Wroclaw [
36].
Assessing the knowledge and preparation of medical staff is crucial to the success of these projects. Taking into account the above, a preliminary quantitative study was designed to determine the level of practical and theoretical knowledge of defined lean tools based on implementation procedures among the management teams. The level of theoretical and practical knowledge is of key importance in order to correctly establish which elements relating to the implementation procedure (which includes the aforementioned lean tools) must be improved and refined to more effectively implement the lean concept in healthcare. Recognizing the level of theoretical and practical knowledge will allow designing actions in those areas, which are deficient, in order to implement the Lean Hospital concept more effectively.
2. Materials and Methods
In order to determine the knowledge of the management teams about the Lean Hospitals concept in the chosen hospitals in Poland, preliminary quantitative studies were carried out. The level of knowledge of members of the management teams was established through their self-assessment of their knowledge of practical and theoretical individual tools of the Lean Hospitals concept [
2]. The degree of implementation of the Lean Hospitals concept was established by referring to the implementation procedure proposed by the pioneers of the Lean Management concept: J.P. Womack and D.T Jones [
14]. The applied research methodology and the most important results from the research with the discussion are presented in the following parts of the paper. The results of the research are presented graphically and descriptively.
Quantitative empirical research was conducted using the technique of an internet questionnaire. A quantitative method (surveying respondents using the CAWI technique) and selected statistical tools were used to answer the research problem and the formulated research questions. The study was conducted among members of the management teams of the chosen hospitals (a sample of 62 respondents selected using a non-probabilistic targeted choice method in Polish hospitals located in the Pomeranian and Warmia–Masuria region). Hospitals were selected in one region—the northern part of Poland—to minimize the impact of the possible environment on the designed study and to ensure the comparability of the situation in which the surveyed hospitals operate. Inclusion criterion: persons actively performing management roles in the hospital. Exclusion criterion: persons not in management roles, other positions in medical units. The respondents’ position included three types of providers, based on their management roles: doctors, ward nurses and administration. Doctors should be understood as heads of wards. Ward nurses should be understood as ward nurses who manage a group of nurses in a particular ward. Administration should be understood as positions connected with management, not with direct patient care. The research population involved a group of respondents who voluntarily agreed to participate in the study and completed the questionnaire. The study was not conducted among patients; thus, it did not require the approval of the Bioethics Committee.
The survey was conducted in the period from February 2020 to August 2020 using the CAWI technique (Qualtrics Platform), which enables the creation of a research questionnaire, its distribution and data gathering.
The research questionnaire was divided into two subject panels. The first subject panel examined the level of theoretical knowledge with regard to basic tools of the Lean Hospitals concept, such as value stream mapping (hereinafter referred to as VSM), 5S best practices (hereinafter referred to as 5S), inventory management in the Kanban system (hereinafter referred to as Kanban), Kaizen, total productive maintenance (hereinafter referred to as TPM), visual management (hereinafter referred to as VM) and work standardization (hereinafter referred to as SW). The second panel of the questionnaire concerned the respondents’ self-assessment with regard to their level of knowledge of the above-mentioned tools used during the implementation of the Lean Hospitals concept: a practical view. The study used closed questions with a 5-point Likert scale (where 1 means lack of knowledge, 2 means poor knowledge, 3 means average knowledge, 4 means good knowledge, and 5 means very good knowledge) and closed multiple-choice questions. An Excel spreadsheet was used to evaluate and analyze the obtained data. The research questionnaire is attached in
Appendix A. The reliability of the research tool was verified using the Cronbach Alpha test. The result was α = 0.9804, which demonstrates a high degree of reliability of the questionnaire (
Appendix B).
The research outcome was determined as a self-assessment of the level of theoretical and practical knowledge regarding single lean tools (value stream mapping (VSM), 5S best practices (5S), inventory management in the Kanban system, Kaizen, total productive maintenance (TPM), visual management (VM) and work standardization (SW)).
The assessment of the level of theoretical and practical knowledge of the Lean Hospitals concept (understood as a set of tools) was made through graphical presentation of the data using spider diagrams and ranking charts created with support of an Excel spreadsheet.
All analyses were performed at the level of respondents’ answers. The study did not analyze data at the level of individual hospitals.
3. Results
The results of the study conducted among a group of management teams of the chosen hospitals are presented below.
First, respondents were asked to undertake a self-assessment concerning their basic knowledge of the Lean Hospitals concept, understood as the theoretical and practical knowledge with regard to different tools, which can be used during the implementation of the Lean Hospitals concept. Their answers (number and statistical values) are presented in
Table 1. More detailed statistics are presented in
Table A1 and
Table A2 in
Appendix C.
This question was asked to illustrate knowledge regarding the basic information of the Lean Hospital concept, which was used as the introduction for further analyses. Afterward, the respondents were asked to undertake a self-assessment of the implementation level of the Lean Hospitals concept in their organization. Additionally, they were asked to assess the benefits it provided to the hospitals’ processes. Most respondents assessed the degree of implementation of the Lean Hospitals concept in their local institution as very poor or poor (42/62 respondents, 66.13%). The average level of implementation was assessed by only 17 respondents, which is 27.42%. No answers indicating a very good implementation of the Lean Hospitals concept were obtained, and only three respondents (4.84%) indicated a good level of implementation of the Lean Hospitals concept. These respondents pointed out several benefits of a good level of implementation of the Lean Hospital concept: shortening the service time, reducing the number of adverse events, reducing the inventory level in pharmacies and increasing patient and employee satisfaction.
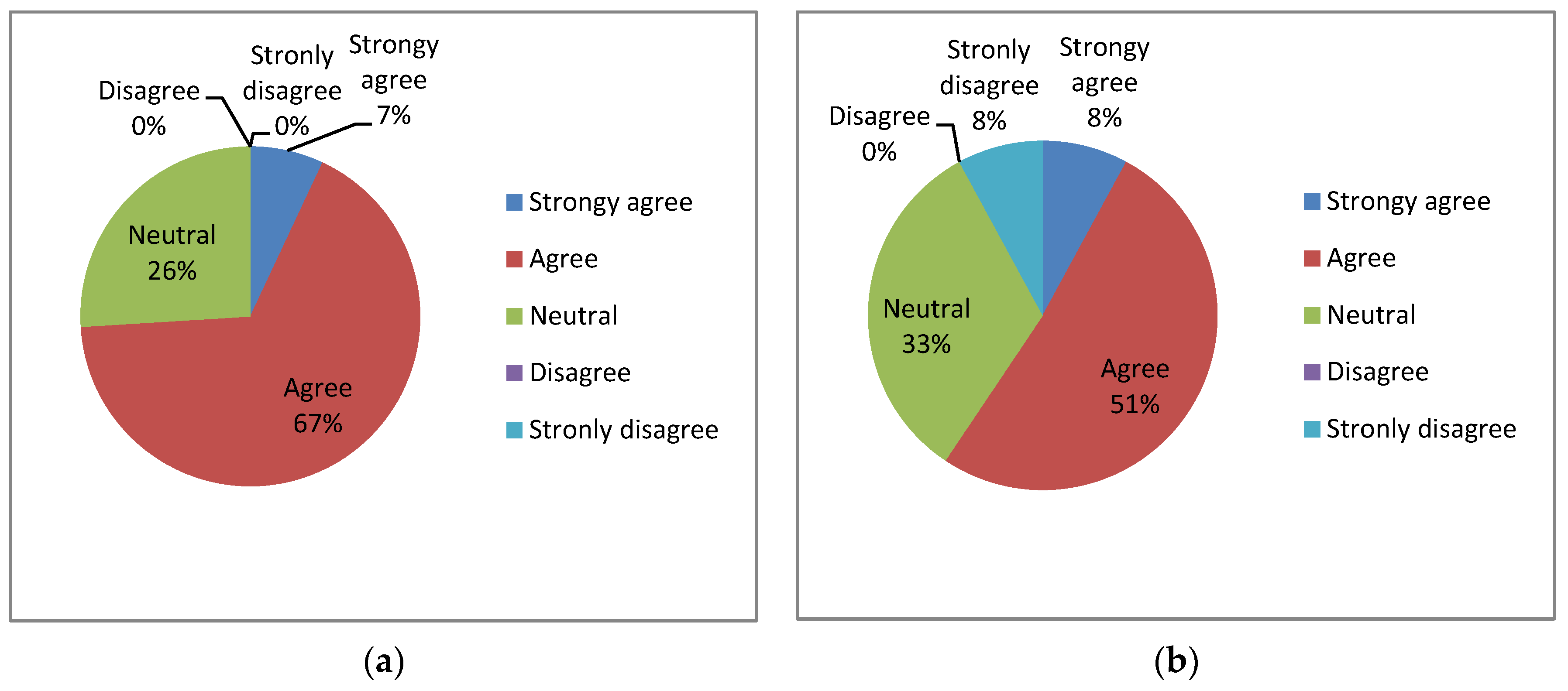
In the next part of the research, the respondents were asked to express their opinion on two statements regarding the Lean Hospitals concept about the possible benefits of its implementation in medical facilities. The following distribution of responses was obtained, in accordance with
Figure 1 and
Figure 2.
Q1: Can the implementation of the Lean Hospitals concept contribute to an improvement in the functioning of a medical facility (from the financial, organizational and technical perspective)? (The results are presented in
Figure 1a)
Q2: Does the area of my responsibility require improvements, which could be obtained through application of selected elements of the Lean Hospitals concept? (The results are presented in
Figure 1b)
The vast majority of respondents strongly agreed or agreed with the second statement (their area of responsibility requires improvements, which can be achieved through the use of elements of the Lean Hospitals concept (8% + 51% of respondents)). In the case of this statement, many neutral answers (33%) were obtained. The responses ranging from “disagree” to “strongly disagree” represented 9% of respondents. The level of responses obtained in the “agree” and “strongly agree” range can be a good starting point for the team to search for knowledge and suggestions for improving and streamlining internal processes.
In the case of the question regarding the possibility of improving the functioning of a hospital (from the financial, technical and organizational perspective) through the use of the Lean Hospitals concept, most respondents strongly agreed or agreed with the above statement (7% + 67% of respondents). The responses in the range of a neutral answer represented 26% of respondents. The responses ranging from “disagree” to “strongly agree” were not noted.
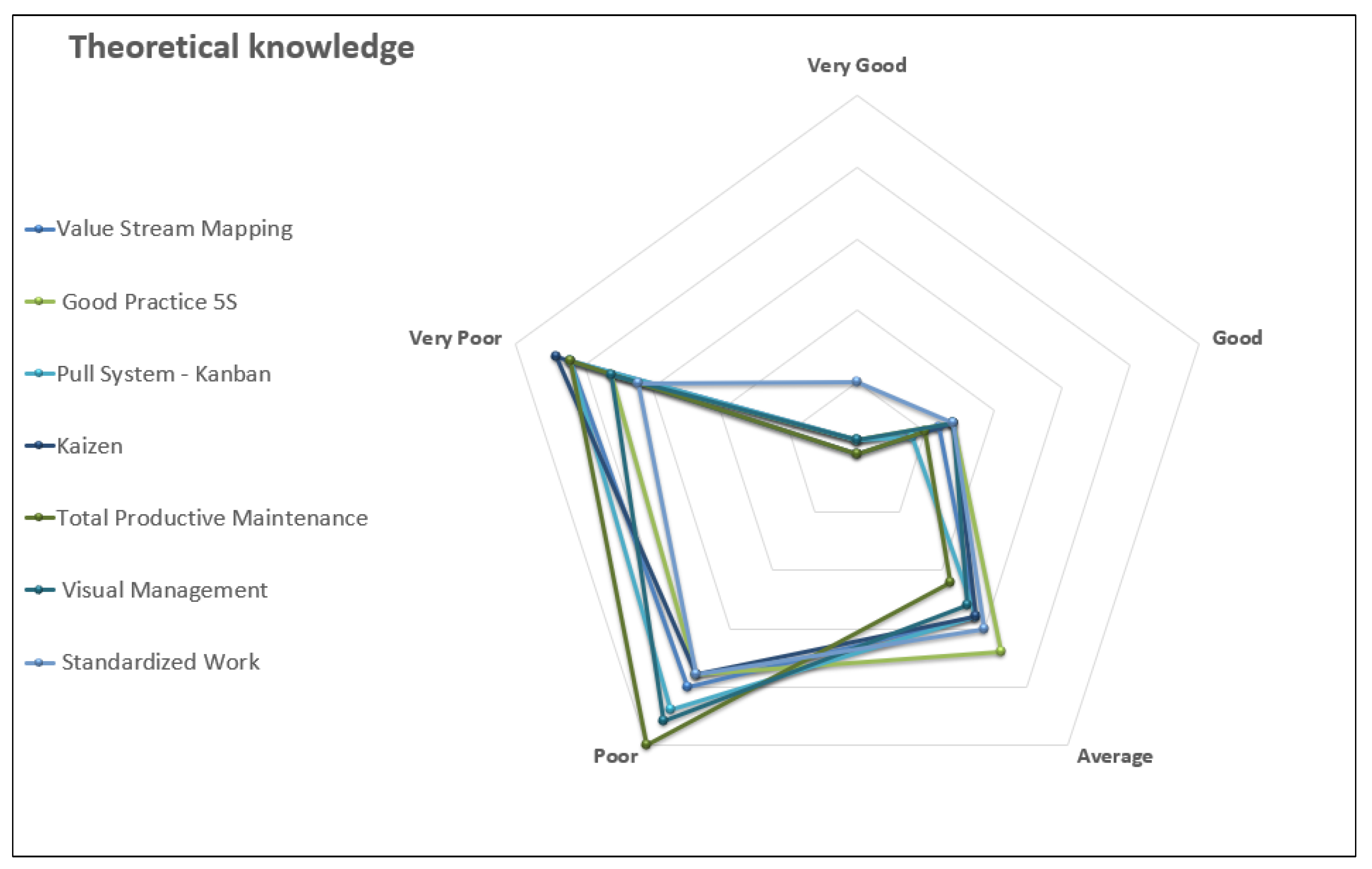
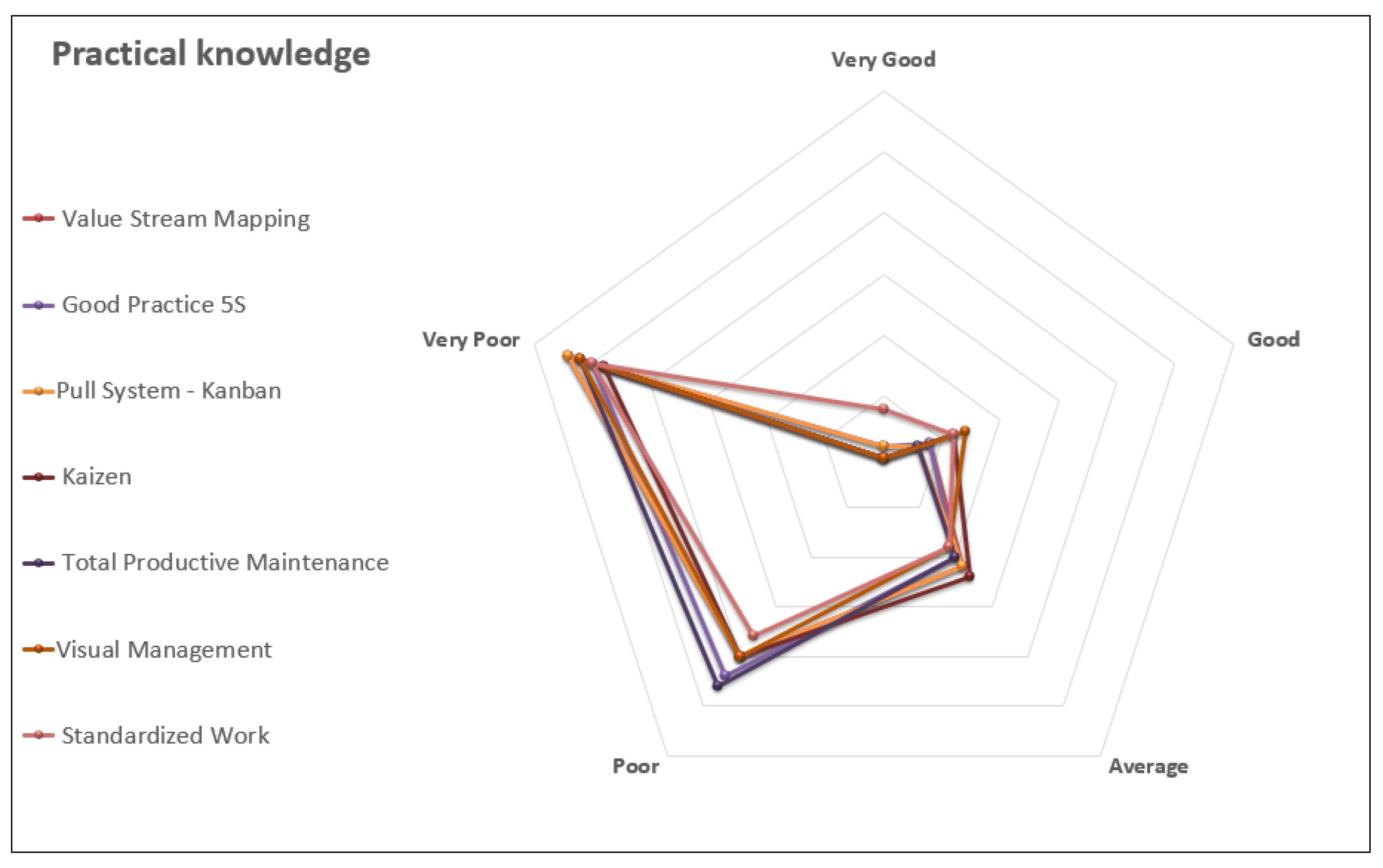
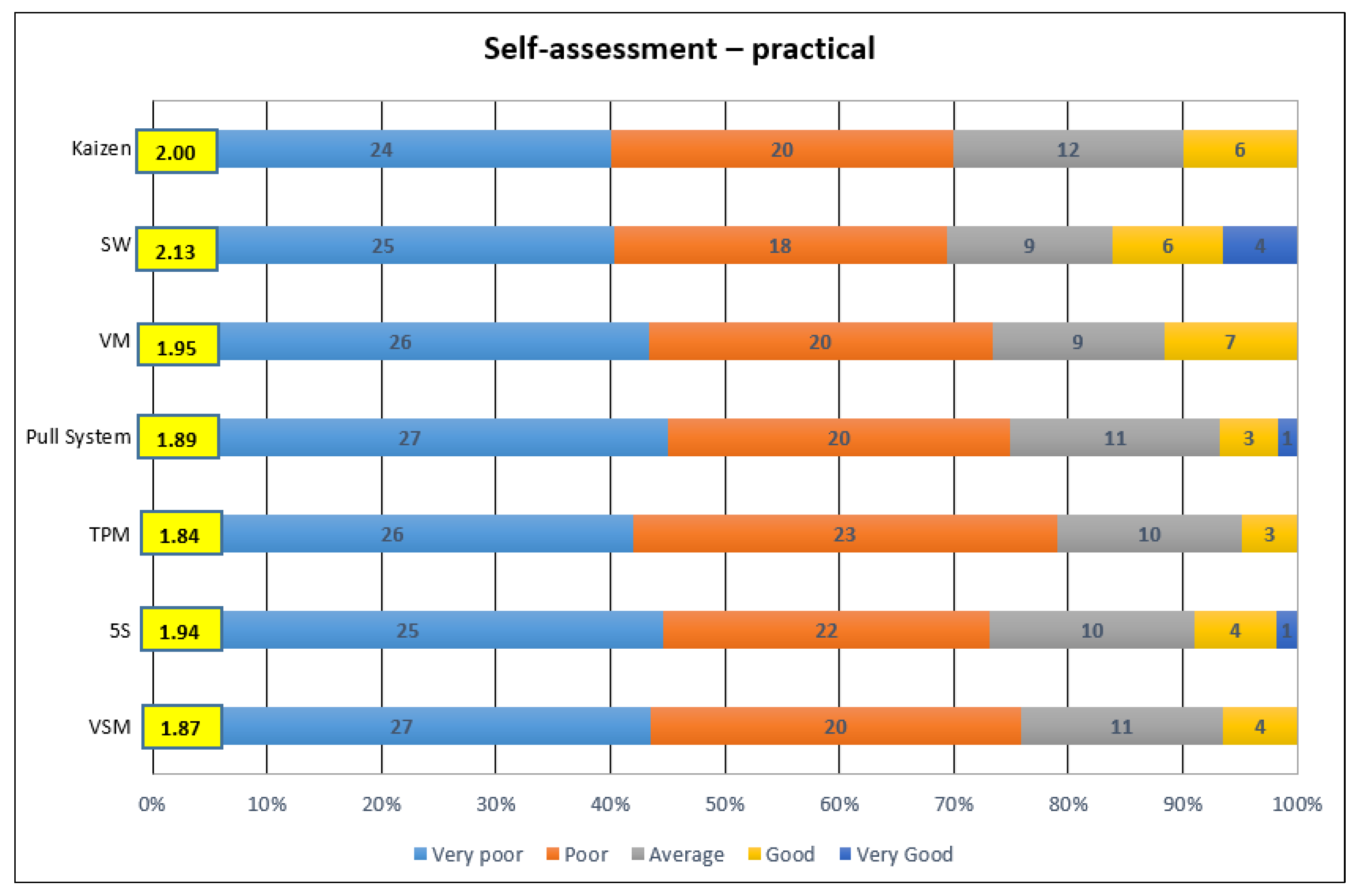
Afterward, a ranking of individual tools of the lean concept for self-assessment of the theoretical and practical knowledge was made, which is presented in
Figure 2 and
Figure 3. Detailed data, pursuant to which the scopes were prepared, are included in
Table A2 in
Appendix C.
Based on the results of ranking in the area of theory, it can be concluded that the level of knowledge is low for each tool. The weighted average does not exceed 2.5 for any of the tools. Based on the results, it is possible to rank the individual tools in terms of the level of theoretical knowledge, starting with those where knowledge is highest, as follows: standardized work (2.45), 5S (2.26), visual management (2.19), value stream mapping (2.13), Kaizen (2.10), pull system (2.06), TPM (2.00).
Based on the results of the ranking, it can be concluded that the level of practical knowledge is also low for each tool. The weighted average does not exceed 2.5 for any of the tools—the same as in the field of theoretical self-assessment. Based on the results, it is possible to rank the individual tools in terms of the level of practical knowledge, starting with those where knowledge is highest, as follows: standardized work (2.13), Kaizen (2.00), visual management (1.95), 5S (1.94), pull system (1.89), value stream mapping (1.87), TPM (1.84).
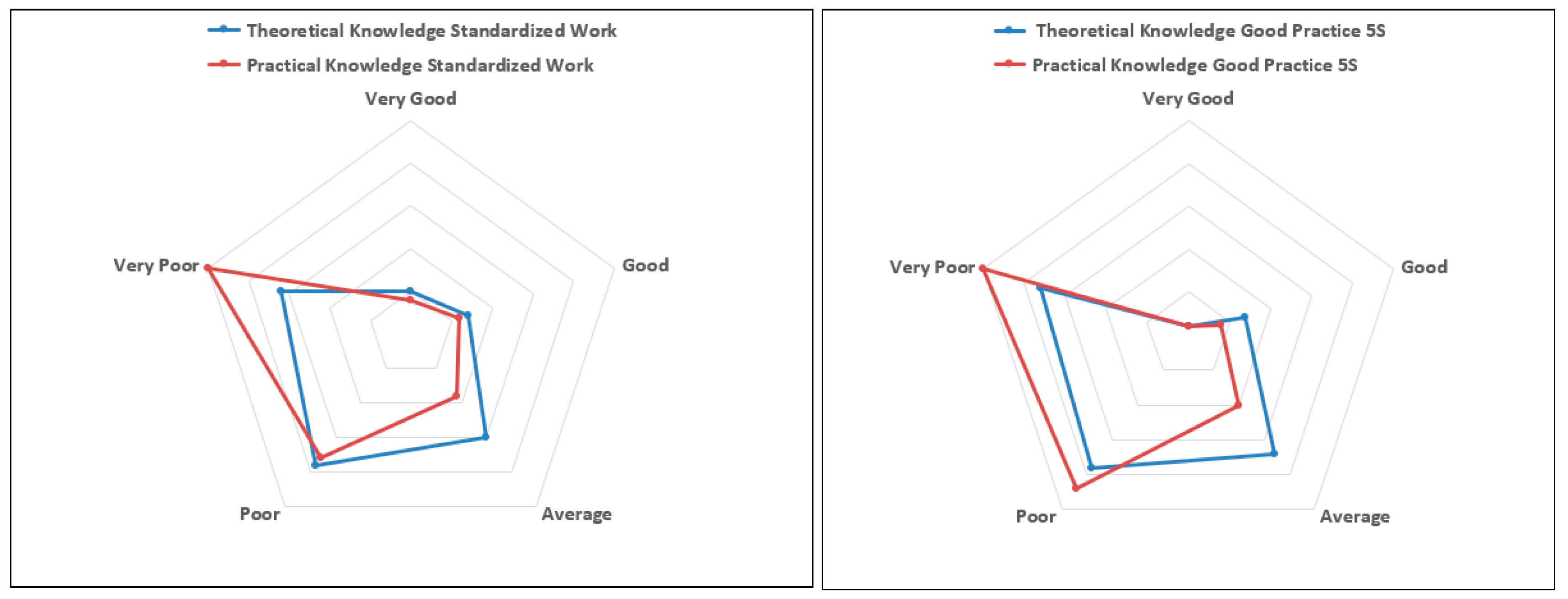
Afterward, a comparison was made of the respondents’ answers regarding the level of theoretical and practical knowledge for each lean tool. An in-depth analysis is presented in the radar plots forming
Appendix C and
Appendix D. A graphical diagram is presented below for the tools for which the largest differences were found between the theoretical and practical knowledge for the scope of their application.
Practical knowledge concerning the standard work tool was assessed at a lower level compared to theoretical knowledge. This is demonstrated by the location of the apex of the red diagram line in the “Very Poor” response over the blue diagram line presented in
Figure 4a. In the case of this tool, a higher number of answers from respondents, who self-assessed their theoretical knowledge as higher than their practical knowledge, was noted, with self-assessment of the theoretical and practical knowledge of the SW tool at the “Very Good” and “Good” level representing a small percentage of all answers, and in both of those cases, at a similar level (as demonstrated by the position of the apices of the diagrams of the blue and red lines assigned to the “Very Good” and “Good” answers).
The self-assessment of the 5S good practices tool was similar to the self-assessment of the practical and theoretical knowledge of standardized work. Practical knowledge was assessed as worse than theoretical knowledge by respondents (as demonstrated by the position of the apex of the line of the red diagram over the line of the blue diagram in the “Very Poor” and “Poor” categories in
Figure 4b). Moreover, a higher number of answers from respondents assessing, on an average level, their theoretical knowledge rather than practical knowledge of 5S good practices was noted (location of the apex of the blue line over the red line in the “Average” and “Good” categories). Assessment of the theoretical and practical knowledge as “Very Good” remained at the same level, as demonstrated by the ideal coverage of the apices of the blue and red lines assigned to the “Very Good” category.
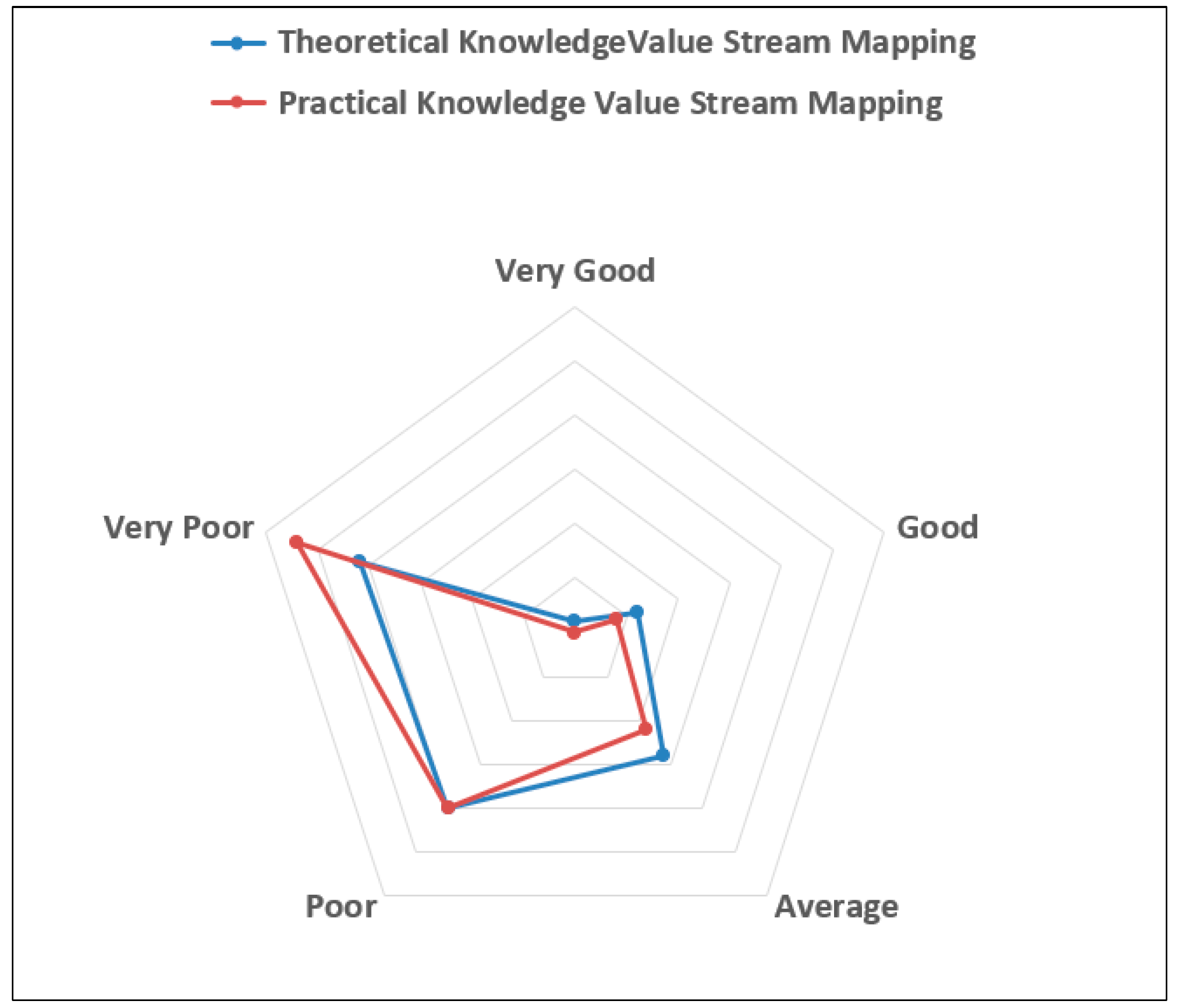
In examining the theoretical knowledge of the value stream mapping tool, the answers “Very Poor”, “Poor” and “Average” are dominating, which overlaps with the self-assessment of practical knowledge, whereby the theoretical knowledge is slightly higher than practical, as demonstrated by the shift of the apex of the radar plot presented in
Figure A1 in
Appendix D toward the center.
Concerning knowledge of the Kaizen tool, the respondents self-assessed their knowledge, both theoretical and practical, on a “Good” level, which is visible in the same position of the apices of the red and blue lines of the diagram in all answers in
Figure A2 in
Appendix D. Small differences were noted in the scope of the “Very Poor” and “Poor” categories, where theoretical knowledge was self-assessed as slightly worse, as demonstrated by the position of the apices of the blue diagram under the apex of the red diagram in the indicated answers. Both for the self-assessment of theoretical and practical knowledge, no “Very Good” answer was obtained, as demonstrated by the ideal coverage of the apices of the blue and red lines in the central point of the radar plot for the “Very Good” answer.
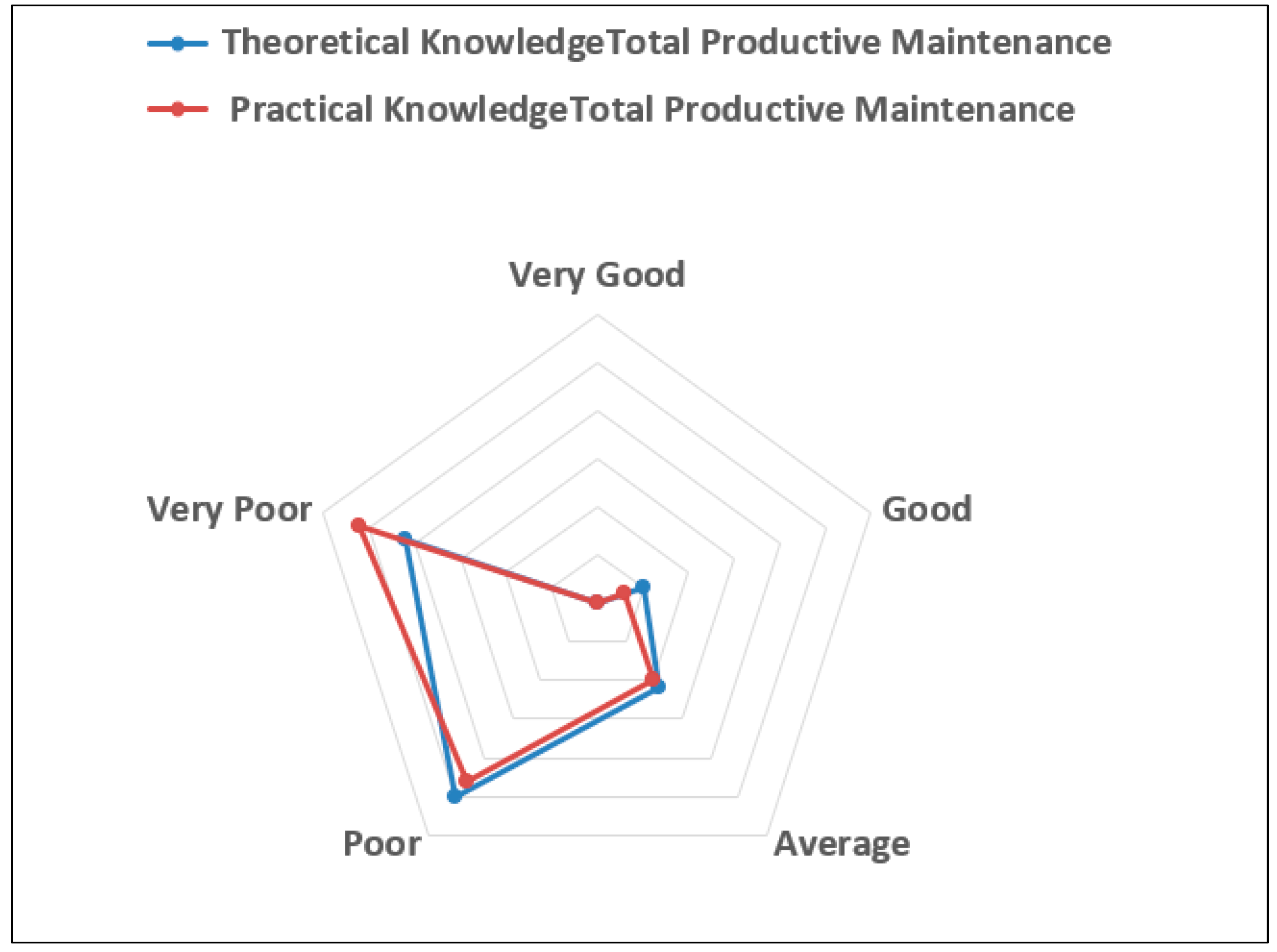
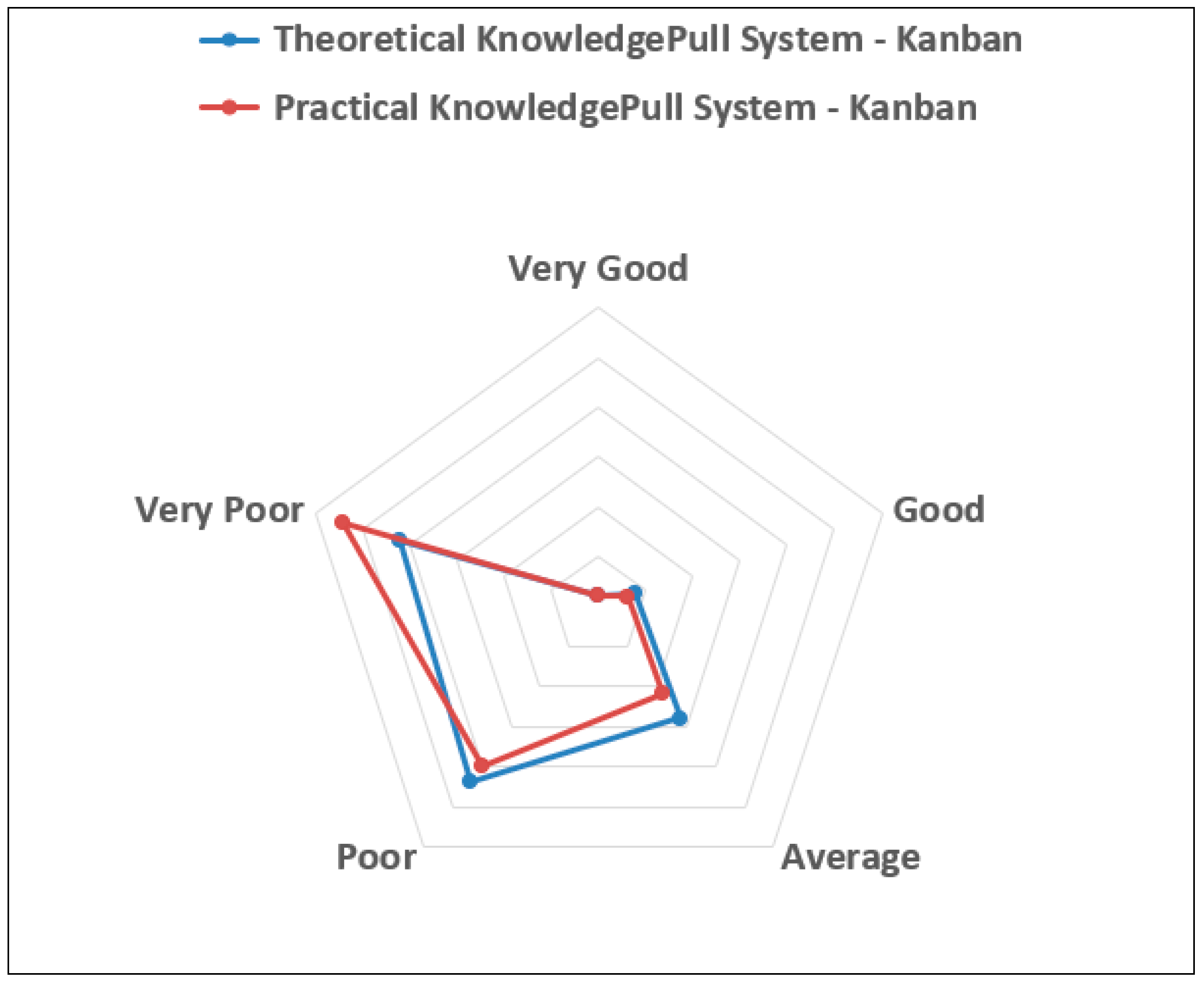
In the case of remaining tools, TPM and Kanban, at the “Poor” level of self-assessment, the theoretical knowledge was self-assessed to be similar to practical knowledge. In the scope of the answer of respondents who self-assessed their level of knowledge as “Good”, the theoretical knowledge was assessed higher than practical. Meanwhile, when assessing the knowledge of both tools, both for self-assessment of theoretical and of practical knowledge, no “Very Good” answer was obtained, as demonstrated by the ideal coverage of the apices of the blue and red lines in the central point of the radar plot for the “Very Good” answer in
Figure A3 and
Figure A4 in
Appendix D.
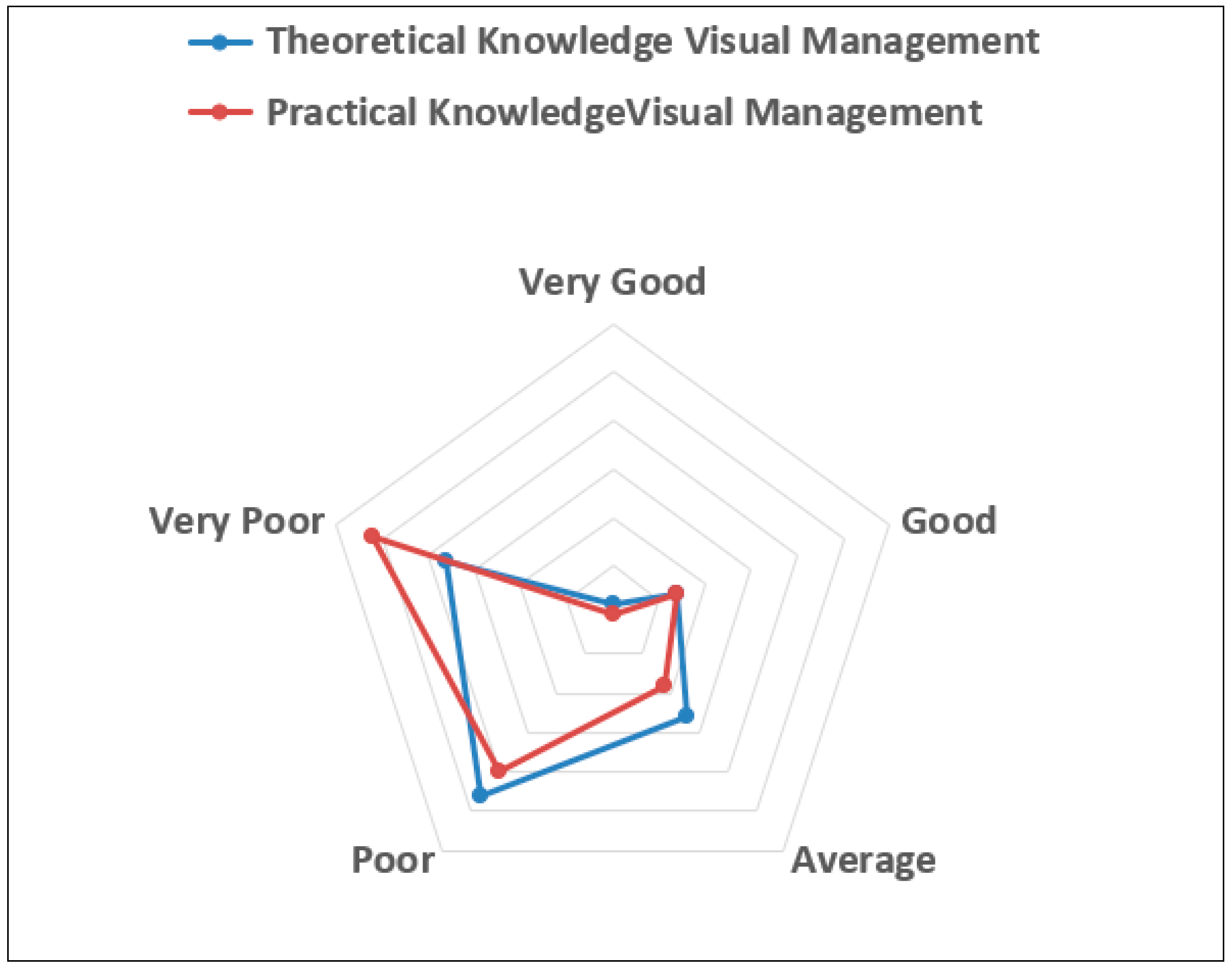
Practical knowledge concerning the visual management tool was self-assessed as worse compared to theoretical knowledge by respondents, as demonstrated by the position of the apex of the red diagram over the blue diagram line in the “Very Poor” category, which is presented in
Figure A5 in
Appendix D. Similar coverage of the line of the diagram of self-assessment of theoretical and practical knowledge for the visual management tool was obtained for the “Good” and “Very Good” answers, which was demonstrated by the position of the apices of the red and blue diagrams for the “Good” and “Very Good” answers. The position of the apex of the blue line in the “Average” answer indicates a higher share of respondents, who assessed their theoretical knowledge rather than their practical knowledge at the “Average” level.
The largest number of answers for the self-assessment of theoretical knowledge at the “Very Good” level was obtained for the standardized work tool, as demonstrated by the projection of the diagram line for the indicated tool (light blue), which is presented in
Figure A6 in
Appendix E. Similarly, for the “Good” category, the standardized work also obtained the largest number of indications from respondents. The worst self-assessments for theoretical knowledge were given for Kaizen and TPM, as indicated by the apices of the diagrams for these tools located farthest away from the central part of the radar plot for the “Very Poor” and “Poor” answers.
The largest number of answers for the self-assessment of practical knowledge at the “Very Good” level was obtained for the standardized work tool, as demonstrated by the projection of the diagram line for the indicated tool (light orange), which is presented in
Figure A7 in
Appendix E.
The worst self-assessments for practical knowledge were given for Kaizen and TPM, as indicated by the apices of the diagrams for these tools located farthest away from the central part of the radar plot for the “Very Poor” and “Poor” answers.
4. Discussion
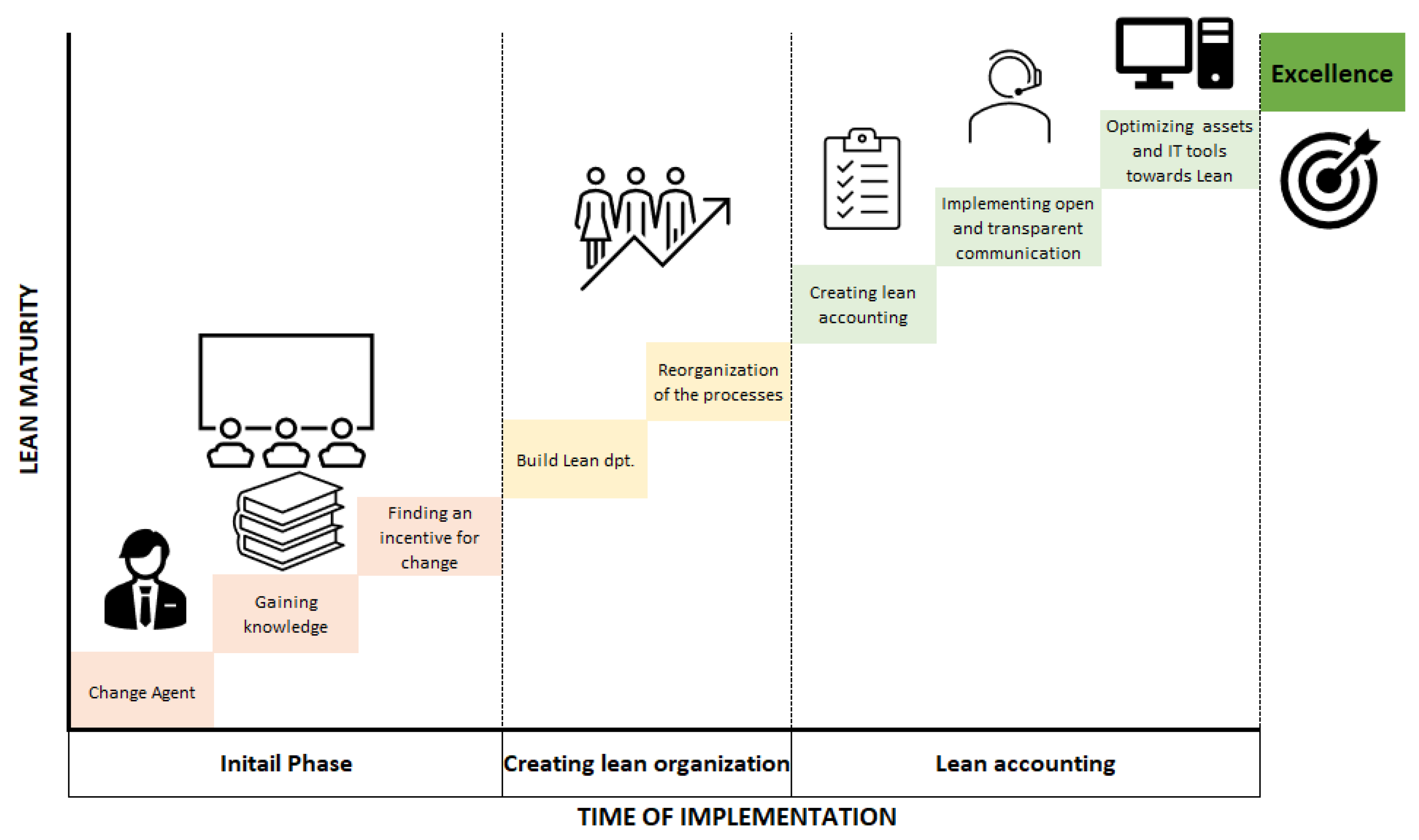
The results of a questionnaire conducted among members of management teams at selected hospitals in Poland presented in the article indicated a limited knowledge of the Lean Hospitals concept among the management teams. The implementation procedure presented by. J.P. Womack and D.T Jones consists of the following phases (
Figure 5):
- -
the initial phase (finding a change agent, gaining relevant knowledge, finding an incentive for change);
- -
the phase of creating a lean organization in the entire production system (including the creation of a lean promotion department, reorganization of processes);
- -
the phase of creating lean accounting, implementing open and transparent communication, optimizing the organization’s assets and IT tools toward lean management;
- -
the phase of completing the transformation process;
- -
the phase of continuous development of the organization and striving for excellence [
48].
It can be concluded that gaining relevant practical and theoretical knowledge is crucial for the first step of lean implementation and contributes to the success of the whole project. Hence, recognizing the level of knowledge is crucial for the preparation for implementation, which is reflected in the implementation approach focusing on the introduction of principles of continuous flow and standardization of operations and processes [
49] and being based on two phases: preparation for implementation and implementation [
50].
Turning to a layer of recognition of the level of knowledge of various tools, the results of the study presented in the article demonstrated the lowest level of knowledge in the area of use of Kanban and TPM, whereas knowledge of the problems related to the standardization of work was assessed at the highest level. This may be related to the quality systems, which have been implemented in hospitals for many years already, an element of which is the preparation and application of procedures and standards [
51]. Moreover, the organization of the healthcare sector units itself, the division of work and the clinical paths induce the need to order and retain the sequence of performance of tasks [
52,
53,
54].
Despite the low level of knowledge of management staff about the Lean Hospitals concept, respondents expressed positive opinions on the possibility of the use of elements of this concept in the improvement of hospital processes. The above view is confirmed by the literature and leads to a conclusion that the implementation of the Lean Hospitals concept should be preceded by training of medical personnel (first of all, those at the management level), which will enable not only effectively conducting the Lean Hospitals implementation process but will also decrease the fear of change [
31,
55]. The lack of knowledge and preparation of persons participating in the implementation of new solutions and the organization’s structure itself are some of the primary barriers in the implementation of Lean Management presented in the literature [
25,
32,
56]. One opinion—which is frequently raised in academic studies, in addition to the resistance to change among the personnel—mainly presented by clinicians is that lean puts an additional burden on their daily duties and that it is a method for a reduction in costs and not for improving their work [
24,
57]. Moreover, the literature also describes problems related to the lack of adaptation of the assumptions of the LM concept to the specifics of a given unit [
22,
32,
33,
34,
35].
One important element in the obtained result is the openness of management staff to the possibility of the use of LM tools in their facilities. A significant majority of those surveyed confirmed that their area of responsibility requires improvements, which may be achieved through the use of elements of the Lean Hospitals concept (
Figure 1). However, they demonstrated limited basic knowledge of the Lean Hospitals concept, with the largest deficiencies in knowledge established for the practical (implementation area) knowledge of the tools. This result may mean that mid-level managers in healthcare units are constantly looking for new solutions enabling the improvement of their daily work; however, they do not have sufficient knowledge concerning such solutions, and in particular, their practical use. The results presented are also reflected in the literature. Jeffrey Pfeffer and Robert Stutton have defined the condition in which people have demonstrated the willingness to change or have basic knowledge in this subject but are lacking sufficient abilities and skills to implement an action as the “knowing-doing gap” [
58]. In the healthcare sector, the occurrence of such gap may result both from the lack of sufficient knowledge, lack of cooperation (significant hierarchies, organizational siloing of hospitals) and from geographical (location of the hospital) or demographical (generation gap) conditions [
51].
The research presented in this article concentrates on identifying the practical and theoretical knowledge of the Lean Hospital concept among managers. Respondents were asked not only to self-assess their level of general knowledge of the Lean Hospital concept but to also refer to a more detailed self-assessment, which focused on specific lean tools. As the literature indicates, most research works concentrate on the impact of implementing Lean Management on the patient flow process, including the reduction in service time, length of stay, waiting time and rotation. Nevertheless, few studies refer to analyses of the level of personnel knowledge, which would enable a smooth implementation of the new concept [
59]. Some of these provide opportunities to involve medical personnel in the preparation of a simulation of lean implementation in a hospital, both on the training side (familiarizing the personnel with the principles and theoretical foundations of Lean Management application [
60]) and on the practical side (applying the tools in the improvement of simulated hospital processes) [
61].
However, these studies do not refer to a self-assessment of the level of knowledge of the concept or to the potential benefits and barriers present in the implementation of lean tools. A common view presented in the literature is that the involvement of medical personnel is a precondition for the successful implementation of the Lean Hospitals concept [
60,
62]. Hence, the research conducted is a key element for the next stage, which is to supplement the practical and theoretical knowledge, find the change agents and model the process of implementing Lean Hospital tools in selected healthcare units.
5. Conclusions
The results of the studies conducted indicate a low level of knowledge and advancement in the implementation of the Lean Hospitals concept in the selected Polish hospitals. Limited knowledge of the Lean Hospital concept was established for entire management teams. This confirms the passing acquaintance with this concept in the Polish healthcare sector. However, the key fact is that despite the low level of knowledge of management staff about the Lean Hospitals concept (see
Table 1), respondents expressed positive opinions on the possibility of the use of elements of this concept in the improvement of hospital processes.
Moreover, the study indicated tools, which can be implemented faster in hospitals due to the manner of the performance of tasks and the division of labor in these tasks and the currently used qualitative solutions (e.g., standardization).
The results of the study, which assessed the level of knowledge of the Lean Hospital concept in the healthcare sector, are an important initial point for preparing the hospitals for the implementation of lean. Successful implementation of the lean philosophy depends on having the theoretical and practical knowledge. Supplementing knowledge only at the theoretical level, without taking care of the practical knowledge aspect, may prolong the implementation procedure or stop it completely. The first stage should focus on supplementing the knowledge and preparing the employees for work in a lean culture, diverting particular attention to the practical part of the training [
63]. Only a positive outcome of this stage may provide positive effects concerning the improvement of processes and improvement of the quality of services provided [
55].
The authors recommend that the next step of this research focuses on the search for correlations between the level of theoretical and practical knowledge and demographics, professional group, work experience, as a starting point to identify the leaders for improving the processes by implementing lean tools.
5.1. Implications of the Research
The Lean Hospital concept has already been proven to streamline processes, improve quality and reduce the time it takes to deliver healthcare services [
2]. However, studies show that there is still limited theoretical and practical knowledge of the Lean Hospital concept among those actively performing management roles in the hospital.
Therefore, a short-term recommendation is to supplement the theoretical and practical knowledge, which should be achieved by special training and implementation workshops held among hospital personnel.
However, a long-term recommendation should focus on further research to define the cause of the low level of knowledge among management staff. It would certainly be appropriate to analyze the education system for healthcare managers in Polish hospitals in order to propose changes to the education system program.
5.2. Limitations
The results obtained should be treated as an initial/pilot study of issues related to the use of the Lean Hospitals concept in medical facilities, which requires further, more detailed studies. The study has multiple limitations. First, our results are derived from an initial study, and their general interpretation should be conducted with care. Second, our sample is relatively small, which is related to the character of the study (an initial study) and the low knowledge of the Lean Hospitals concept in Poland. Third, the low level of knowledge of management staff in Polish hospitals may be related to both the low number of implementations and the low scope of training programs for medical personnel and healthcare facility management personnel, which take into account the use of Lean Management tools.