This paper will look at two aspects of chaplaincy. It draws on the author’s work in a psychiatric hospital system in Missouri and work in a faith-based hospital in Australia as well as drawing on leadership roles in chaplaincy in both Australia and the North America. The first aspect is what importance is placed on chaplaincy by our own faith communities. The second is how chaplaincy is seen by the institutions in which it occurs.
Some years ago, when I worked for Missouri’s Department of Mental Health as Director of Pastoral Resources, it was suggested by a member of the senior management team that I meet with her brother, who was a Diocesan Catholic priest. He offered what can be argued as how institutional chaplaincy, and in particular hospital chaplaincy, functioned. His analysis was simple and yet telling when he said that, “we send our weakest to our most vulnerable.”
At the same time, I often heard chaplains report on conversations with fellow clergy when they would be asked, “when are you coming back to the real ministry?” It was as if what chaplains did was, at best, second rate.
1. The Two Big Changes in Chaplaincy
The first big change draws on the work of both Anton Boison and Granger Westberg. Boison, himself a consumer of mental health services at Worcester State Hospital, recognised the need for both the training and the professionalization of chaplaincy in different ways. Westberg, who in the late 1940s was assigned to what was then Lutheran General Hospital in Chicago, refused his administrator’s requirement that he saw every patient in the hospital every two days. If he were to ‘achieve’ this requirement, it would mean spending roughly five minutes with each person, and that did not allow for interactions with either family or staff. Westberg applied the principle of triage, which was also just emerging in medicine. Boison, who had been an intermittent patient at Worcester (Massachusetts) State (Psychiatric) Hospital, saw the need for training of chaplains.
The second major change in the 20th century was the ordination of women. This occurred first in many of the Protestant faiths and then in other religions. Many of the ordained women were looking for alternatives to standard pulpit appointments, and chaplaincy was a viable option because it allowed some flexibility, including part-time work. At the same time, due to Boison and Westberg, there was training available. In the late 1940s, two professional chaplaincy organisations emerged in the United States that required professional training beyond seminary. These were the College of Chaplains and the Association of Mental Health Clergy, and they merged in 1998 to form the Association of Professional Chaplains.
1 In Australia, chaplaincy associations were seen as primarily Christian and more particularly Protestant, as reflected by the Australian Health and Welfare Chaplains Association. In 2009, it was decided to create Spiritual Care Australia, and for a short while, there was a conscience effort to have a member of the Islamic and Jewish faiths on its Board of Directors.
With the introduction of women, the standard and the quality of chaplaincy improved. There had been good men already functioning as chaplains, but the quality was less than consistent. The women raised the game.
2. How the Institution Sees Chaplaincy
It takes one of two approaches. The first is “what good is the chaplain? They are not reimbursable!”, and the second, as expressed during a survey of Senior Managers (see below), is of “if it’s not a squeaky wheel, then I don’t worry about it!” What both these positions fail to recognise is that agencies that certify institutions are now seeing spiritual services (not necessarily liturgy) as a patient right. In addition, they are seeing documents such as Religious Histories and Spiritual Assessments as just as important as other assessments including Psychological, Nursing, and Social Service Assessments. The (US) Joint Commission’s Comprehensive Accreditation Manual for Hospitals lists standards that surveyors are supposed to verify in an audit for accreditation.
2There has also been a move in ICD-10 and ICF-11 (i.e., the International Coding of Disease or the International Coding of Functioning) (
Carey and Cohen 2015) to assign codes to Spirituality, and this could have an impact on reimbursement.
In many institutions, Spiritual Care is often seen as something that has to be done and as such is given a low priority. The Mayo Clinic (
Mueller et al. 2001) offers another way of seeing this issue: “appropriate spiritual support must be available to all patients who desire it, the same way we provide them with a meal and a warm blanket”.
Today, what was originally called chaplaincy is known by a number of expressions, beginning with Chaplaincy, but more recently Pastoral Care, and now Spiritual Care. There is a lot of confusion in our society as to what is meant by the terms “faith”, “religion”, and “spirituality”. The contemporary philosopher Jonathan Sacks (
Sacks 2003) observed that “no one creed has a monopoly on spiritual truth; no one civilization encompasses all the spiritual, ethical and artistic expressions of mankind” (p. 62). Lord Sacks, like most others, highlights the ongoing confusion that exists in most people’s minds between faith, religion, and spirituality. He clearly uses them interchangeably in his writings.
Over the years, I have developed my own working statement that has enabled me to see how they are interrelated: while it may seem simplistic, it has enabled me to see how they are interconnected and how their relationship works:
Faith and religion are the cultural and ethnic filters to our spirituality.
The terms “faith” and “religion” are relatively easy to define. Faith is what we believe, while religion tends to be the (public) expression of those beliefs that may (or may not) include ritual. What is less clear in a definition of “spirituality”. Within healthcare the most commonly accepted definition (
Puchalski et al. 2014) was developed in 2009 at a Consensus conference as
Spirituality is a dynamic and intrinsic aspect of humanity through which persons seek ultimate meaning, purpose, and transcendence, and experience relationship to self, family, others, community, society, nature, and the significant or sacred. Spirituality is expressed through beliefs, values, traditions, and practices.
Underlying all this is the question of whether there is any evidence based research on the efficacy of either chaplaincy or spirituality in health care. As
Meador et al. (
2017) have noted that “putting different care approaches ‘to the test’ discourages the persistence of approaches that can be based on a host of questionable foundations, such as tradition, inertia, strong or influential personalities, pet theories”.
The role of the chaplain in the healthcare process is not clear. Some institutions see the chaplain as integral to the function of the team, while others will use a referral system. Also, there has been some work on how chaplains function within the medical setting (
The Joint Commission 2018;
Choi et al. 2015;
Hemming et al. 2016).
Perhaps the largest study conducted was by Press Garney in December 2003. This reviewed the opinions of 1,732,562 patients that demonstrated the following (
Clark et al. 2003, p. 662):
Patients place a high value on their emotional and spiritual needs while in the hospital;
A strong relationship exists between the hospitals’ care of patients’ emotional and spiritual needs and overall patient satisfaction;
Care for patients’ emotional and spiritual needs constitutes a significant opportunity for improvement for most hospitals.
Perhaps the biggest problem is that nobody in the health care system is quite sure what chaplains actually do. As
Nieuwsma et al. (
2017) noted, “many chaplains perceived that they were vaguely appreciated by mental health, even when mental health had little clue as to what they did.” When I functioned in the institution, I often felt that I would be brought in as the response of “last resort”. Psychiatry had not worked, neither had psychology, and social work and nursing were at a loss, so why not bring in the chaplain, for it really could not do any harm.
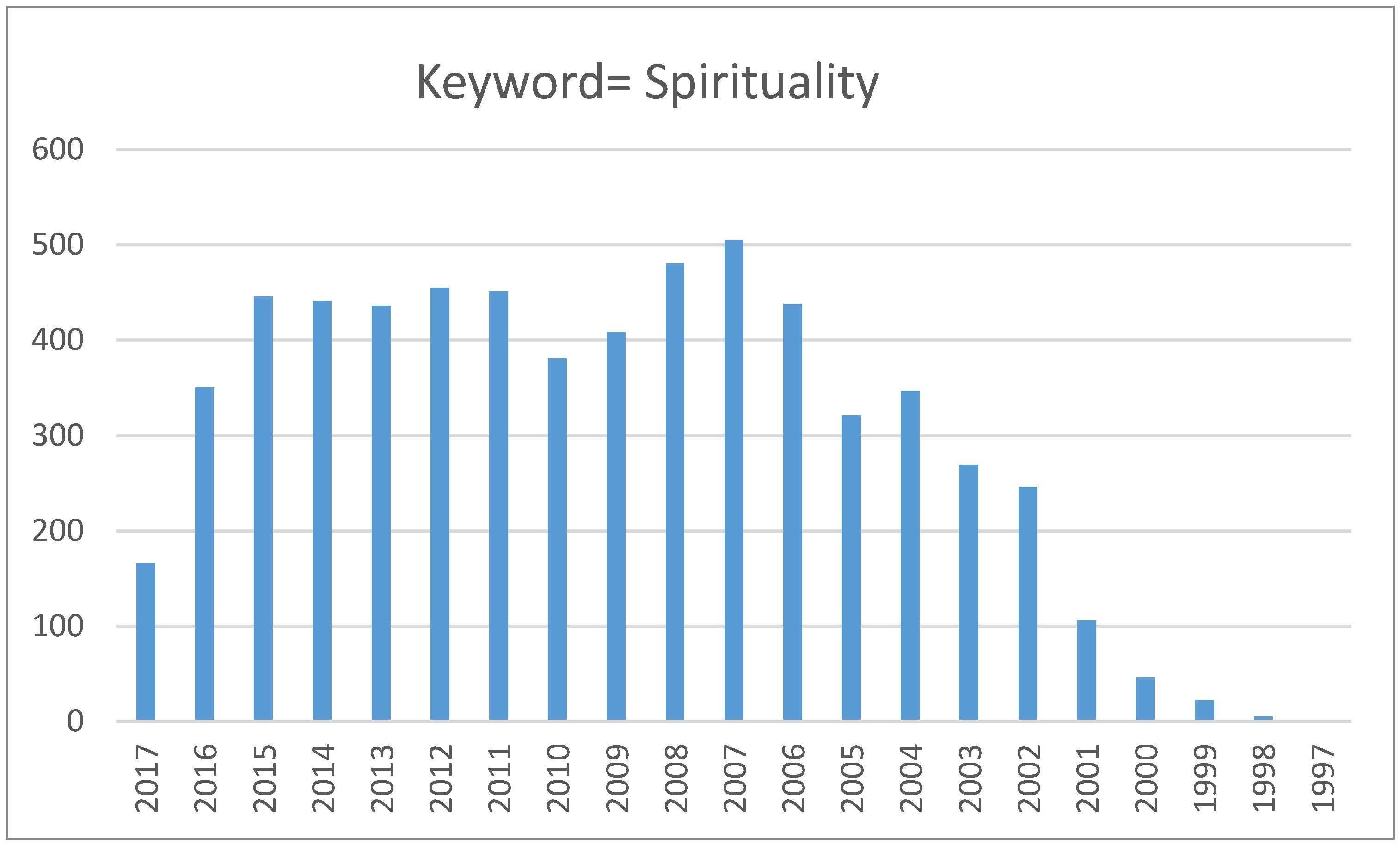
What we have seen is a mushrooming of articles on spirituality in the health care literature over the past 20 years (see
Figure 1). More and more researchers are seeking to find whether there is an evidence base for spirituality within health.
3. Looking to the Evidence
Over the past five years, there have been two studies conducted in the School of Public Health and Community Medicine at UNSW Australia focusing on the question of chaplaincy or spirituality in health. The first was conducted by a Year 4 Medical Student and focuses on how palliative care patients perceive chaplaincy. This was an attempt to fill the knowledge gap between what professionals perceive as patients’ religious/spiritual needs and the perceptions of family members and friends as to the patient experience from chaplains.
The second is a Masters in Public Health (Research) thesis on how senior managers see the place of spirituality in the health care system.
The first study aimed to investigate any factors that were associated with effective spiritual care delivery, with particular focus on encounters with pastoral care staff. To achieve this, it used a two-step process. The first focused on exploring the patients’ spiritual needs as they presented them. The second stage of the study explored how the patients experienced, in their own words, the pastoral care encounter.
The hypothesis upon which all this was based was that pastoral encounters that addressed spiritual needs would be more helpful to patients than those which did not address spiritual needs.
Patients were recruited at two faith-based palliative care units over a period of five weeks. Twenty patients out of 36 approached accepted participation in the study. Patients were recruited at arm’s length by staff at each site and excluded if they were under 18, insufficiently fluent in English, or overly sick/tired/distressed/cognitively impaired. In addition, the demographics of the patient sample were relatively homogenous. The majority of participants were of an Anglo-Saxon background, which does not represent the multi-cultural nature of Australian society. Indigenous spirituality was not represented.
A structured, mixed method interview approach was used. It had its strengths and weaknesses:
Strength: The open-ended questions enabled us to elicit patients’ perceptions of spiritual needs, while the closed ended questions allowed for greater comparison between different patients.
Weaknesses: The structured format of the interview did not provide much scope to explore each patient’s spirituality in further depth.
The survey was divided into two broad sections:
The second section of the survey (details of pastoral encounter) was not as effective as had been expected. It was adapted from the “Clinical Chaplaincy Data Card” by
Rodrigues et al. (
2000). Most of the options listed in the Data Card did not adequately describe the patients’ encounters with pastoral carers. This was possibly because the Clinical Chaplaincy Data Card was designed with American patients in mind. Fortunately, most patients’ experiences were still able to record under the ‘other’ option, which requires patients to further describe their encounter.
The question about how spiritual care can be delivered produced different results from other surveys (
Balboni et al. 2011;
Hart et al. 2003;
Tan et al. 2005), which all indicated that patients were favourably predisposed to hospice staff (not just chaplains) asking about spirituality. In this study, the majority of patients were unfavourable/ambivalent to doctors or nurses asking about spirituality. In narrowing to whether they would find it acceptable for doctors or nurses ask about their beliefs, the responses were that only four out of 20 thought it acceptable, while seven were unsure/did not know, and nine were negative.
Most (18 out of 20) believed that hospitals had a responsibility to provide pastoral care services, and 11 patients believed that pastoral carers can provide for patients’ spiritual needs, regardless of the faith of the chaplain.
The second study looked at how senior managers (Executive Directors, Directors of Nursing, Quality Assurance) perceive the place of both chaplains and spirituality in caring for patients. It was based in one Health Services Area in Sydney, Australia, which is a 5000+ bed system. The initial interviews were conducted in 2002. Potentially, there were 24 individuals, and 16 were actually interviewed. In 2012, it was decided to revisit those who had been interviewed 10 years before. Only six individuals were still in the system, and three agreed to be interviewed. Perceptions over the decade had not changed substantially. All interviewees knew that Pastoral/Spiritual Care existed in their institution. There was neither consistency about any lines of reporting nor even how appointments were made- some had full time chaplains while others relied on local (volunteer) chaplains.
Most respondents felt that spirituality was important and that it was poorly acknowledged in the public health system. No one interviewed had serious concerns about chaplaincy. There was an awareness that chaplaincy happened in their facility. Besides the offering of liturgy, there was little grasp about what chaplains do—except for the faith-based facilities.
There was no sense of “patient load” (i.e., how many patients of a particular faith was each chaplain expected to visit in any period of time). There was no sense of an ideal patient–chaplain ratio as there was in other disciplines such as nursing, social services, etc. The model that they accepted was faith-based. In the past 20 years, there has been a shift toward clinical-service/disease-focused chaplaincy (
Lucas 2001).
There was also no sense of how chaplains could be more efficient, and by inference, could be more involved in helping the institution achieve its mission and objectives. Except in the case of faith-based institutions, the chaplains are externally funded, and hence there is no sense of ownership of the institution of chaplaincy.
While each senior manager saw the need to develop awareness of spirituality in health, there was no consistency in how this could be achieved nor who would deliver such training. Some thought it should be through a university as part of the degree process, while others thought it should be either the Department of Health or by the professional organisations such as the Medical Association or the College of Nursing. The only consistency was that they did not see it as their responsibility.
4. Conclusions
At the end of the day, the issues that will need to be addressed in the near future include (as suggested by Meador et al.)
What are the evidence-based expectations for chaplaincy for it to flourish as a discipline in contemporary health care?
How might chaplaincy engage evidence-based practices while retaining its soul—daresay even more fully embrace its faithfulness to patient-centered spiritual care?