Abstract
Spirituality has been widely considered important for patients’ health and for healthcare practice and is related to connectedness, meaning in life, and transcendence. Research concerning spirituality is growing rapidly, and the implementation of spiritual care should be based on evidence. This literature review aims to describe the methods that have been used in nursing research focusing on spirituality. The electronic search on databases through EBSCOhost identified 2091 citations, and a total of 231 studies were included. The methods used in research on spirituality in nursing are mostly quantitative (52.4%), but some are qualitative (42.8%) and mixed (4.8%). Regarding the quantitative research, most studies are observational (90.9%), and these are mainly descriptive (82.7%) and correlational (17.3%). Most studies used a cross-sectional design (98.7%), and few used longitudinal design (1.3%). The qualitative research is descriptive (39.4%), phenomenological (26.3%), and grounded theory (14.1%). Research on spirituality in nursing is based on both main paradigms (quantitative and qualitative), but also on mixed methods. Studies have mainly been conducted using cross-sectional designs when compared to longitudinal designs. The latter seem to constitute a gap in nursing knowledge and evidence regarding the changes of spirituality over time, which is particularly important for nurses’ delivery of spiritual care.
1. Introduction
Spirituality is often defined as a fundamental dimension in people’s lives (), or an integral and universal dimension of the human condition (). Spirituality is based on several foundations from various religious traditions, spiritual movements, belief systems, cultures, and contexts (). The way spirituality is lived and felt depends on each individual, since it is an individual experience, even when beliefs and traditions are shared (). Many authors have defined the concept of spirituality in different ways, so a consensus has been difficult to achieve, as the concept may have several meanings (). Still, the main attribute and characteristic of the concept is the need to find purpose and meaning in life (). Spirituality is also understood as awareness of transcendence, and connection with self, others, or beyond the self with something greater (). When looking at the different definitions of the concept, the common attributes are connectedness, meaning in life, and transcendence ().
Spirituality plays an important role in health, particularly in times of crisis or severe illness, as it is foundational and links the bio-psycho-social dimensions as an integrated whole (). Spirituality has been described as critical for patients’ health and for healthcare practice (), and the benefits of spiritual experiences and beliefs on health have been highlighted (). For example, spirituality plays a critical role in terminally ill patients against end-of-life despair (). Spirituality is a positive dimension of the human being and care and might help patients reframe their experiences and condition of illness as well as find meaning in life and in that circumstance ().
Several barriers to spiritual care have been identified, such as the lack of education and preparedness, and the reductionist understanding of the concept of spirituality, which has led nurses to perceive their competencies as scarce in providing spiritual care. Nurses require competencies in three domains to provide spiritual care: awareness and use of self, spiritual dimension of the nursing process, and assurance and quality of expertise (). These competencies should be adjusted according to the problems, settings, and culture in which nurses are immersed (). Additionally, the nurses’ personal spirituality plays a critical role in the perceptions of spirituality and competencies in providing spiritual care (). Spiritual care is defined as a subjective and dynamic concept, and is considered a unique aspect of care (). It is based on an interdisciplinary approach, in which each professional plays an important role (), and nurses are also responsible for providing individualized spiritual care to patients and families (). Spiritual care is the nurses’ responsibility (; ), and spiritual care integrates the daily practice of nursing ().
Nursing care is expected to be holistic, so the spiritual dimension should be taken into consideration (). In the last couple of decades, the new concept of “spiritual well-being” has emerged, which seeks to bring together the concepts of spirituality and wellness (). This new concept of spiritual well-being is characterized by having a multidimensional background () and is often considered an indicator of the patients’ quality of life and spiritual health status (). Furthermore, spiritual distress is a nursing diagnosis that has been listed in NANDA International (NANDA-I) since 1978 (), and is defined as “a state of suffering associated with the meaning of his/her life, related to a connection to self, others, world, or a Superior” ().
The growing interest in spirituality in nursing, in the understanding of the related concepts, and in exploring spiritual care strategies and procedures has been identified in the scientific literature in this domain in the last three decades (; ). The implementation of spiritual care should be evidence-based, so an overview of research methods seems important in order to raise awareness of what has been done so far and which methods can be used in the future, which will be described in this review. These results may also provide a helpful mapping of common aspects of spirituality that have been most frequently addressed as well as the existing gaps in nursing literature that need further development and research. This study aims to characterize the research methods concerning spirituality in nursing.
2. Materials and Methods
The literature review based on electronic searches in March 2017 in the EBSCOhost platform, included the following databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Psychological Information Database (PsycINFO), Medical Literature Analysis and Retrieval System Online (MEDLINE), and Medical Journals in Spanish (MedicLatina). Electronic searches were also conducted in the following databases: Cumulative Index to Nursing and Allied Health Literature (LILACS) and the Scientific Electronic Library Online (SciELO). The search terms were “spiritual care,” “spirituality” and “nursing,” using the search strategy: (“spiritual care” OR “spirituality”) AND “nursing,” in the abstracts (ABSs) (Table 1).

Table 1.
Number of citations on the databases search.
The inclusion criteria previously defined were as follows: search terms in the abstract; primary studies on spirituality in nursing, and articles written in English, French, Spanish, and Portuguese. Two independent reviewers conducted the process of selection and analysis of the articles. The results were imported to EndNote Web®. The initial search found 2091 results of which 749 duplicates were removed. All 1342 titles were read and analyzed according to the inclusion criteria, and 596 articles were selected at this stage. The abstracts were read and, at the end, 231 papers reporting primary studies were included (Figure 1). The critical appraisal of the studies was not performed, since the review aims to identify the research methods and procedures regardless of the quality of the research. Data were extracted to an Excel file comprising the following information: year, country, authors, article title, journal, thematic area, research paradigm, research methods, and data collection methods and procedures.
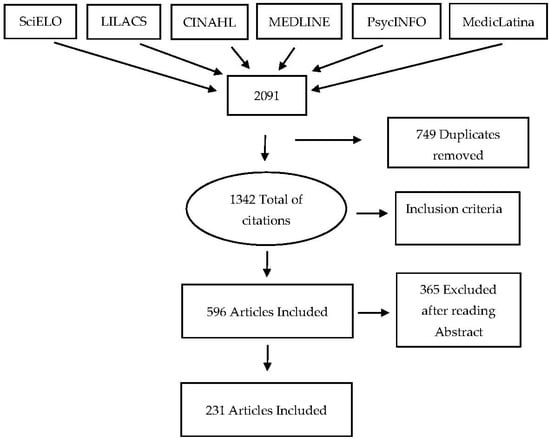
Figure 1.
Study selection process.
3. Results
All 231 studies were published in 102 different international journals. The nursing journals having more publications were: Journal of Clinical Nursing (n = 22), Oncology Nursing Forum (n = 18), Journal of Advanced Nursing (n = 14), Journal of Holistic Nursing (14), Nurse Education Today (n = 10), Holistic Nursing Practice (n = 6), and Journal of Nursing Research (n = 5). Spirituality in nursing is an international research subject, as 34 countries have been identified in the included studies. The USA leads (n = 85), followed by Taiwan (n= 20); Brazil (n = 15), Iran (n = 13), UK (n = 10), Norway and Australia (n = 8), Singapore (n = 7), and Colombia, Netherlands, Jordan, and Sweden (n = 5) (Figure 2).
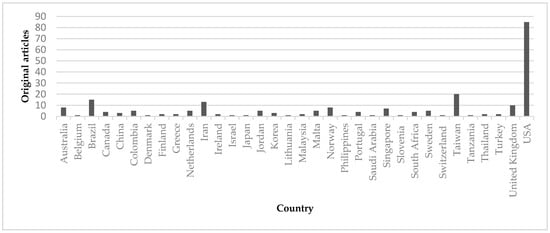
Figure 2.
Distribution of results by country of research.
The first paper included in this review was published in 1986, from the USA, and it concerns spiritual care as a nursing responsibility towards patients’ spiritual needs. Until 2000, few studies had been published, but from that year onwards, an increase in scientific production is clear. The years 2012 and 2016 had the highest number of published studies, with a total of 23 and 25 original studies each. When comparing the years 2010 and 2016, within a timeframe of six years, the number of studies has duplicated (Figure 3).
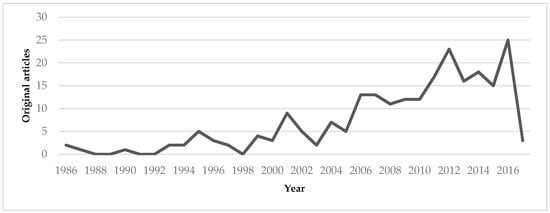
Figure 3.
Distribution of results by year of publication.
The studies have been organized in six categories after independent analysis and discussion, according to the research topics on spirituality: education, management, assessment tools, oncology and palliative care, nursing diagnosis validation, and spiritual care. The topic most often addressed was spiritual care (n = 118), followed by education (n = 52), oncology and palliative care (n = 35), assessment tools (n = 18), nursing diagnosis validation (n = 5), and management (n = 3) (Table 2).

Table 2.
Categories of the results in this review.
When analyzing the methodologies in the studies about spirituality in nursing, the majority are quantitative (52.4%), but some are qualitative (42.8%) and mixed (4.8%). The first studies were mostly based on the qualitative research paradigm, but this trend changed in 2004, when a predominance of quantitative studies started being published (Table 3).

Table 3.
Research paradigm and methods of results in this review.
Regarding the quantitative paradigm, most studies are mainly observational (90.9%), followed by quasi-experimental (5.8%) and experimental (3.3%). The first RCT was published in 2011 and it concerns the effect of nurses’ training on spirituality and nursing care.
Concerning the observational studies, most are descriptive (82.7%) and less are correlational (17.3%). Regarding the time dimension, the research design is mostly cross-sectional (98.7%) and a scarce percentage is longitudinal (1.3%). The first longitudinal study was conducted by () over a period of three years, aiming to analyze nursing students’ perceptions of spirituality and spiritual care using the Spirituality and Spiritual Care Rating Scale.
Studies based on the qualitative paradigm are mostly descriptive (39.4%), phenomenological (26.3%), and grounded theory (14.1%) (Table 3). In relation to data collection, questionnaires have been preferred (39%), followed by interviews (28%) and assessment tools (7.8%).
4. Discussion
Research on spirituality in nursing has existed at least since the 1980s, and this topic continues to be widely studied. Regardless of the evident and recent increase in the number of publications on spirituality, the number of publications is small when compared to other topics, and when considering the overall development and increase of healthcare research and nursing journals. The results of this review concern a period of over 30 years, and 231 articles were included reporting research on spirituality in nursing. Although spirituality has an evident heritage in healthcare, empirical evidence became more often published in nursing literature in the 1980s. Since 2000, a significant increase of primary studies in spirituality has been published and this topic is sometimes considered a new field of research (; ).
When considering the methodological approach, in recent years, the quantitative paradigm has been largely used in nursing studies concerning spirituality. However, there is no superiority of one paradigm over the other, as each paradigm contributes in different ways to the complex study of the health/illness process in nursing (). Therefore, quantitative and qualitative research are complementary methods in the development of nursing science (). There is a small percentage of mixed-method studies (4.7%), but it is becoming increasingly necessary to use both qualitative and quantitative methodologies in the study of spirituality (). Currently, mixed methods is a trend methodology in health research because it facilitates the study of complex human phenomena (). Moreover, research based on the triangulation of methodologies improves the scientific integrity and rigor of knowledge in nursing, and ultimately contributes to the development of nursing as a scientific discipline ().
The existence of more quasi-experimental studies (than experimental studies) on this topic is similar to other research topics in nursing research, and this might be justified by the several barriers that have been described, such as the shortage of potential participants that would lengthen the period required to conduct an experimental study (). The main goal of quasi-experimental and experimental designs are common and both are essential to test the effectiveness of nursing interventions to improve outcomes in nursing practice ().
There is a large percentage of descriptive studies using the qualitative or the quantitative paradigms, and these data meet the results presented in the study by (). Spirituality is an expanding area in terms of knowledge, so it is essential to present a description of all aspects related to this area of research (). Hence, only a clear understanding of what spirituality is may allow a clear and deep assessment and provision of spiritual care (). Spiritual care is based on an interdisciplinary approach, and nurses share the responsibility of assessing, diagnosing, and providing effective interventions, which could be direct (such as listening, presence, or reading) or indirect (such as facilitating chaplain, family, or other visits). The existence of many descriptive studies is not surprising since spirituality is a quite recent concept within nursing literature and descriptive studies are performed when there is little information about a phenomenon ().
Concerning the time dimension in research design, only 1.3% of the studies used a longitudinal design. Perhaps one of the reasons for the few longitudinal studies is that they include many limitations, namely, that they require a long time, they are expensive to perform, and there is loss of observations in data collection (; ). Despite the disadvantages mentioned above, longitudinal studies are more powerful than cross-sectional studies and the major advantage concerns the ability of controlling the variation of variables over time and of providing evidence of causal inferences (). Therefore, longitudinal studies are fundamental to evaluate how spirituality (or related phenomena, such as spiritual distress or spiritual well-being) relates to certain variables over time, variables such as stress, life satisfaction, social support satisfaction, depression, and health (). Spirituality, religiosity, and beliefs can change over time, according to life experience, and this is particularly important in the healthcare context. Societies are embedded in a context of globalization, so they are in constant evolution and change over time. The religious environment and religious faith also accompany such change and are influenced by other religions around the world.
Regarding the research topics, few studies have been identified on nursing diagnosis validation concerning spirituality, and those included in this review mainly used Richard Fehring’s models for nursing diagnosis validation. The importance of the validation of nursing diagnoses in spirituality is to assess the needs of patients and to improve clinical practice in nursing (). The validation of nursing diagnoses plays a critical role, such as the nursing diagnosis of spiritual distress, since nurses play a significant role in alleviating the patients´ suffering. In this regard, () conducted a clinical validation of the nursing diagnosis of spiritual distress in cancer patients undergoing chemotherapy, while () validated impaired spirituality in patients with chronic renal disease. However, the greatest obstacle for the validation of nursing diagnoses is the methodology, which can be complex and require broad knowledge in the areas of epidemiology and biostatistics ().
The number of studies about assessment tools has also increased (n = 18). The studies comprise the development of new instruments and the validation of several scales in different populations. It should be noted that () identified only two methodological studies concerning the development of tools for assessing spiritual needs. It is recommended that the development of these assessment tools should involve and promote the participation of patients ().
There has been a growth of studies on educational aspects of spirituality in nursing. For example, () mentioned that only three studies had been published thus far, and () reported that ten studies had been conducted. In this review, a total of 52 studies in education were found; thus, in a time frame of four years, 42 additional studies have been published. In 2006, Ross underlined education in spirituality as an emergent topic and on finding that nurses were receiving little training in this area, and reinforced the growth of this topic in research. Nurses are responsible for assessing the patients’ spiritual needs and for providing spiritual care and so this topic must be included in the nursing curriculum throughout graduation training (). () conducted a grounded theory research on the nursing students’ learning of patient spiritual care and the results suggest that spirituality should be present throughout the nursing program, thereby allowing students to assess and to provide spiritual care, so they can apply theoretical knowledge in their clinical practice. After attending spiritual care training courses, nursing students demonstrate increased self-efficacy in providing spiritual care to patients ().
In relation to topic management, four studies have been conducted, and this can represent a challenge in developing innovative research concerning nursing management and workplace spirituality. Spiritual leadership promotes an environment for learning spiritual care and encourages a holistic approach both to the patient and to teamwork (). However, most of the research topics are in palliative care and oncology and spiritual care.
Future investigation should focus on the production of a higher level of scientific evidence, namely, quasi-experimental, mixed-method, correlational, and longitudinal studies addressing spirituality in nursing.
Nursing research should be simultaneously focused on the patient and on the theoretical framework, aiming to improve the quality of nursing care (). Additionally, nursing research is fundamental to influence evidence-based practice and to guarantee safe patient outcomes, whilst contributing to the growing body of nursing knowledge (). Nursing research is an overwhelming and challenging theme, although in the end it is a rewarding experience ().
5. Conclusions
Spirituality is an important topic in healthcare and in nursing literature, and the interest in this topic has been growing in the last several decades. Nursing is a scientific discipline that is developing rapidly, and nursing practice is expected to be evidence-based. This should also be expected with regard to implementing spirituality in nursing practice or in providing spiritual care. Thus, it is important to find a deeper understanding of the methodological approach previously used in nursing research concerning spirituality towards the continuity of evidence development and the adequacy of research approaches to the study of this human dimension.
This paper aimed to review the research methods used in nursing literature concerning spirituality. The results highlight that both main paradigms (quantitative and qualitative) are predominantly used, while few studies employ mixed methods. Regarding the quantitative paradigm, most studies are observational and with descriptive characteristics. As for qualitative studies, most of them are descriptive, phenomenological, and grounded theory. Considering the timeline, most studies are cross-sectional. Nevertheless, quasi-experimental and experimental studies, mixed methods, and correlational designs appear to be an urgent need for the development and consolidation of knowledge. The findings provided by this review address the existing gap on longitudinal studies on spirituality and related phenomena and their essential role in creating a solid ground for nursing knowledge and for the improvement of effective and adequate spiritual care interventions.
Author Contributions
H.M. and S.C. conceived and designed the study and analyzed the data; H.M., J.R., and S.C. wrote and reviewed the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aalen, Odd O., and Nina Gunnes. 2010. A Dynamic Approach for Reconstructing Missing Longitudinal Data Using the Linear Increments Model. Biostatistics (Oxford, England) 11: 453–72. [Google Scholar] [CrossRef] [PubMed]
- Balboni, Tracy, Michael Balboni, Elizabeth M. Paulk, Andrea Phelps, Alexi Wright, John Peteet, Susan Block, Chris Lathan, Tyler VanderWeele, and Holly Prigerson. 2011. Support of Cancer Patients’ Spiritual Needs and Associations with Medical Care Costs at the End of Life. Cancer 117: 5383–91. [Google Scholar] [CrossRef] [PubMed]
- Baldacchino, Donia R. 2006. Nursing Competencies for Spiritual Care. Journal of Clinical Nursing 15: 885–96. [Google Scholar] [CrossRef] [PubMed]
- Baldacchino, Donia. 2015. Spiritual Care Education of Health Care Professionals. Religions 6: 594–613. [Google Scholar] [CrossRef]
- Caldeira, Sílvia Maria Alves, Erika da Cássia Lopes Chaves, Emília Campos de Carvalho, and Margarida Maria da Silva Vieira. 2012. Nursing Diagnoses Validation—The Differential Diagnostic Validation Model as a Strategy. Journal of Nursing UFPE 6: 1441–45. [Google Scholar]
- Caldeira, Sílvia, Emília Campos Carvalho, and Margarida Vieira. 2013. Spiritual Distress-Proposing a New Definition and Defining Characteristics. International Journal of Nursing Knowledge 24: 77–84. [Google Scholar] [CrossRef] [PubMed]
- Caldeira, Sílvia, Amélia Simões Figueiredo, Ana Paula da Conceição, Célia Ermel, João Mendes, Erika Chaves, Emília Campos de Carvalho, and Margarida Vieira. 2016. Spirituality in the Undergraduate Curricula of Nursing Schools in Portugal and São Paulo-Brazil. Religions 7: 134. [Google Scholar] [CrossRef]
- Caldeira, Sílvia, Fiona Timmins, Emília Campos de Carvalho, and Margarida Vieira. 2017. Clinical Validation of the Nursing Diagnosis Spiritual Distress in Cancer Patients Undergoing Chemotherapy. International Journal of Nursing Knowledge 28: 44–52. [Google Scholar] [CrossRef] [PubMed]
- Chaves, Erika de Cássia Lopes, Emília Campos de Carvalho, Fábio de Souza Terra, and Luiz de Souza. 2010. Clinical Validation of Impaired Spirituality in Patients With Chronic Renal Disease. Revista Latino-Americana de Enfermagem 18: 309–16. [Google Scholar] [CrossRef]
- Clarke, Janice. 2009. A Critical View of How Nursing Has Defined Spirituality. Journal of Clinical Nursing 18: 1666–73. [Google Scholar] [CrossRef] [PubMed]
- Cleary, Michelle. 2016. Essentials of Building a Career in Nursing Research. Nurse Researcher 23: 8–12. [Google Scholar] [CrossRef] [PubMed]
- Cockell, Nell, and Wilfred McSherry. 2012. Spiritual Care in Nursing: an Overview of Published International Research. Journal of Nursing Management 20: 958–69. [Google Scholar] [CrossRef] [PubMed]
- Doyle, Louise, Anne-Marie Brady, and Gobnait Byrne. 2016. An Overview of Mixed Methods Research—Revisited. Journal of Research in Nursing 21: 623–35. [Google Scholar] [CrossRef]
- Evangelista, Carla Braz, Maria Emilia Limeira Lopes, Solange Fatima Geraldo Costa, Patricia Serpa de Souza Batista, Jaqueline Brito Vidal Batista, and Amanda Maritsa de Magalhães Oliveira. 2016. Palliative Care and Spirituality: An Integrative Literature Review. Revista Brasileira de Enfermagem 69: 591–601. [Google Scholar] [CrossRef] [PubMed]
- Fehring, Richard J., Judith Fitzgerald Miller, and Christine Shaw. 1997. Spiritual Well-Being, Religiosity, Hope, Depression, and Other Mood States in Elderly People Coping with Cancer. Oncology Nursing Forum 24: 663–71. [Google Scholar] [PubMed]
- Fisher, John W. 2016. Assessing Adolescent Spiritual Health and Well-Being. Social Science and Medicine—Population Health 2: 304–5. [Google Scholar]
- Frouzandeh, Nasrin, Fereshteh Aein, and Cobra Noorian. 2015. Introducing a Spiritual Care Training Course and Determining its Effectiveness on Nursing Students’ Self-Efficacy in Providing Spiritual Care for the Patients. Journal of Education and Health Promotion 4: 34. [Google Scholar] [CrossRef] [PubMed]
- Giske, Tove, and Pamela H. Cone. 2012. Opening up to Learning Spiritual care of Patients: A Grounded Theory Study of Nursing Students. Journal of Clinical Nursing 21: 2006–15. [Google Scholar] [CrossRef] [PubMed]
- Gommez, Rapson, and John W. Fisher. 2003. Domains of Spiritual Well-Being and Development and Validation of the Spiritual Well-Being Questionnaire. Personality and Individual Differences 35: 1975–91. [Google Scholar] [CrossRef]
- Gouveia, Maria João, Marta Marques, and José Luís Pais Ribeiro. 2009. Versão Portuguesa do Questionário de Bem-estar Espiritual (SWBQ): Análise Confirmatória da sua Estrutura Factorial. Psiologia, Saúde & Doenças 10: 285–93. [Google Scholar]
- Gray, Jennifer R., Susan K. Grove, and Suzanne Sutherland. 2017. Burns and Grove’s the Practice of Nursing Research: Appraisal, Synthesis, and Generation of Evidence, 8th ed. Grand Rapids: Elsevier, 738 p. First published 1987. [Google Scholar]
- Haase, Joan E., Nancy Kline Leidy, Doris D. Coward, Teresa Britt, and Patricia E. Penn. 2000. Simultaneous Concept Analysis: A Strategy for Developing Multiple Interrelated Concepts. In Concept Develpment in Nursing: Foundations, Techiniques and Applications. Edited by Beth L. Rodgers and Kathleen A. Knafl. Philadelphia: Saunders, pp. 209–29. First published 1993. [Google Scholar]
- Herdman, Heather T., and Shigemi Kamitsuru, eds. 2014. NANDA: NANDA International Nursing Diagnoses: Definitions and Classification 2015–2017, 10th ed. Chichester and Ames: Wiley-Blackwell, 468 p. First published 1994. [Google Scholar]
- Jahnukainen, Markku. 2011. Longitudinal Research on Emotional and Behavioural Difficulties. Emotional & Behavioural Difficulties 16: 337–38. [Google Scholar]
- Kaye, Judy, and Senthil Kumar Raghavan. 2002. Spirituality in Disability and Illness. Journal of Religion and Health 41: 231–42. [Google Scholar] [CrossRef]
- Lepherd, Laurence. 2015. Spirituality: Everyone Has It, but What Is It? International Journal of Nursing Practice 21: 566–74. [Google Scholar] [CrossRef] [PubMed]
- Liu, Shan, Jane Dixon, Guang Qiu, Yu Tian, and Ruth McCorkle. 2009. Using Generalized Estimating Equations to Analyze Longitudinal Data in Nursing Research. Western Journal of Nursing Research 31: 948–64. [Google Scholar] [CrossRef] [PubMed]
- Lopes, Marcos Venícios de Oliveira, Viviane Martins da Silva, and Thelma Leite de Araujo. 2013. Validação de Diagnósticos de Enfermagem: Desafios e Alternativas. Revista Brasileira de Enfermagem 66: 649–55. [Google Scholar] [CrossRef] [PubMed]
- McClain, Collen S., Barry Rosenfeld, and William Breitbart. 2003. Effect of Spiritual Well-Being on End-of-Life Despair in Terminally-Ill Cancer Patients. Lancet 361: 1603–7. [Google Scholar] [CrossRef]
- McSherry, Wilfred, Mark Gretton, Peter Draper, and Roger Watson. 2008. The Ethical Basis of Teaching Spirituality and Spiritual Care: A Survey of Student Nurses Perceptions. Nurse Education Today 28: 1002–8. [Google Scholar] [CrossRef] [PubMed]
- Moberg, David O. 2002. Assessing and Measuring Spirituality: Confronting Dilemmas of Universal and Particular Evaluative Criteria. Journal of Adult Development 9: 47–60. [Google Scholar] [CrossRef]
- Narayanasamy, Aru. 2004. Spiritual care. The Puzzle of Spirituality for Nursing: A Guide to Practical Assessment. British Journal of Nursing 13: 1140–44. [Google Scholar] [CrossRef] [PubMed]
- Pesut, Barbara, Marsha Fowler, Elizabeth J. Taylor, Sheryl Reimer-Kirkham, and Richard Sawatzky. 2008. Conceptualising Spirituality and Religion for Healthcare. Journal of Clinical Nursing 17: 2803–10. [Google Scholar] [CrossRef] [PubMed]
- Puchalski, Christina M. 2006. Spirituality and Medicine: Curricula in Medical Education. Journal of Cancer Education: The Official Journal of The American Association For Cancer Education 21: 14–18. [Google Scholar] [CrossRef] [PubMed]
- Puchalski, Christina M. 2012. Spirituality in the Cancer Trajectory. Annals Oncology 23 S3: 49–55. [Google Scholar] [CrossRef]
- Ramezani, Monir, Fazlollah Ahmadi, Eesa Mohammadi, and Anoshirvan Kazemnejad. 2014. Spiritual Care in Nursing: a Concept Analysis. International Nursing Review 61: 211–19. [Google Scholar] [CrossRef] [PubMed]
- Ross, Linda. 2006. Spiritual Care in Nursing: An Overview of the Research to Date. Journal of Clinical Nursing 15: 852–62. [Google Scholar] [CrossRef] [PubMed]
- Rothman, Juliet. 2009. Spirituality: What We Can Teach and How We Can Teach It. Journal of Religion & Spirituality in Social Work 28: 161–84. [Google Scholar]
- Severinsson, Elisabeth. 2012. Nursing Research in Theory and Practice—Is Implementation the Missing Link? Journal of Nursing Management 20: 141–43. [Google Scholar] [CrossRef] [PubMed]
- Swinton, John, and Stephen Pattison. 2010. Moving Beyond Clarity: Towards a Thin, Vague, and Useful Understanding of Spirituality in Nursing Care. Nursing Philosophy: An International Journal for Healthcare Professionals 11: 226–37. [Google Scholar] [CrossRef] [PubMed]
- Timmins, Fiona, and Sílvia Caldeira. 2017a. Assessing the Spiritual Needs of Patients. Nursing Standard 31: 47–53. [Google Scholar] [CrossRef] [PubMed]
- Timmins, Fiona, and Sílvia Caldeira. 2017b. Understanding Spirituality and Spiritual Care in Nursing. Nursing Standard 31: 50–57. [Google Scholar] [CrossRef] [PubMed]
- Timmins, Fiona, and Wilf McSherry. 2012. Spirituality: The Holy Grail of Contemporary Nursing Practice. Journal of Nursing Management 20: 951–57. [Google Scholar] [CrossRef] [PubMed]
- Van Cott, Alicia, and Mary C. Smith. 2009. Nursing Research: Tips and Tools to Simplify the Process. Dermatology Nursing 21: 138–40. [Google Scholar] [PubMed]
- Van Leeuwen, René, and Bart Cusveller. 2004. Nursing Competencies for Spiritual Care. Journal of Advanced Nursing 48: 234–46. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, René, and Annemiek Schep-Akkerman. 2015. Nurses’ Perceptions of Spirituality and Spiritual Care in Different Health Care Settings in the Netherlands. Religions 6: 1346–57. [Google Scholar] [CrossRef]
- Weathers, Elizabeth, Geraldine McCarthy, and Alice Coffey. 2016. Concept Analysis of Spirituality: An Evolutionary Approach. Nursing Forum 51: 79–96. [Google Scholar] [CrossRef] [PubMed]
- Weaver, Kathryn, and Joanne K. Olson. 2006. Understanding Paradigms Used for Nursing Research. Journal of Advanced Nursing 53: 459–69. [Google Scholar] [CrossRef] [PubMed]
- Woll, Monica L., Daniel B. Hinshaw, and Timothy M. Pawlik. 2008. Spirituality and Religion in the Care of Surgical Oncology Patients with Life-Threatening or Advanced Illnesses. Annals of Surgical Oncology 15: 3048–57. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).