Dyadic Adjustment and Spiritual Activities in Parents of Children with Cystic Fibrosis
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Marital Adjustment
2.3.2. Spiritual Activities
2.3.3. Disease Severity
2.4. Statistical Analyses
2.4.1. Exploratory Data Analysis
2.4.2. Inferential Analysis
3. Results
| Characteristic | |
|---|---|
| Parent gender, N (%) Female | 86 (68%) |
| Parent age (years), N (%) | |
| 18–25 | 8 (6%) |
| 26–30 | 21 (17%) |
| 31–35 | 44 (35%) |
| 36–40 | 28 (22%) |
| 41–45 | 16 (13%) |
| >45 | 9 (7%) |
| Religious affiliation, N (%) | |
| Protestant | 21 (17%) |
| Roman Catholic | 23 (18%) |
| Non-denominational Christian | 42 (33%) |
| Other | 18 (14%) |
| None | 22 (17%) |
| Child gender, N (%) Female | 62 (50%) |
| Child age, mean (SD) | 5.6 (4.1) |
| Pulmonary exacerbations in prior 12 mos, mean (SD) | 0.92 (1.4) |
| DAS, mean (SD) | |
| Total | 106 (18.7) |
| Dyadic cohesion | 16.5 (4.6) |
| Dyadic affection | 48.8 (8.9) |
| Dyadic consensus | 8.6 (2.7) |
| Dyadic satisfaction | 32.5 (5.0) |
| Religious spiritual activity duration in minutes, mean (SD) | |
| Private | |
| Individual (198 activities) | 14.8 (16.4) |
| Conjugal (9 activities) | 12.8 (13.3) |
| Familial (233 activities) | 7.4 (9.8) |
| Public | |
| Individual (21 activities) | 109.3 (188.4) |
| Conjugal (1 activity) | 10.0 (0) |
| Familial (57 activities) | 69.6 (57.4) |
| Distressed (DAS < 100) Mean (SD) N | Non-distressed (DAS ≥ 100) Mean (SD) N | P-value | |
|---|---|---|---|
| Spiritual activity | |||
| Individual | |||
| Frequencies | |||
| Total | 0.4 (0.6)
30 | 0.8 (1.2)
96 | 0.044 |
| Private | 0.4 (0.6)
30 | 0.7 (1.0)
96 | 0.043 |
| Duration | |||
| Total | 5.4 (13.8)
30 | 14.2 (29.8)
96 | 0.023 |
| Private | 2.7 (5.0)
30 | 11.6 (26)
96 | 0.011 |
| Private | |||
| Frequency | 6.1 (8.3)
30 | 18.6 (29.7)
96 | 0.018 |
| Duration | 0.9 (1.0)
30 | 1.6 (1.6)
96 | 0.010 |
| Total Duration | 16.6 (33.9)
30 | 36.9 (53.9)
95 | 0.042 |
| Child gender, N (%) | 0.038 | ||
| Female
Male | 21 (70%)
9 (30%) | 46 (48%)
50 (52%) | |
| Parent age (years), N (%) | 0.001 | ||
| 18–25 | 2 (6.7%) | 6 (6.3%) | |
| 26–30 | 1 (3.3%) | 20 (20.8%) | |
| 31–35 | 6 (20%) | 38 (39.7%) | |
| 36–40 | 9 (30%) | 19 (19.9%) | |
| 41–45 | 10 (33.3%) | 6 (6.3%) | |
| >45 | 2 (6.7%) | 7 (7.3%) |
4. Conclusions
Author Contributions
Appendix
| 1 0 0 Spiritual Activities |
| 1 1 0 Individual spiritual activities |
| 1 1 1 praying |
| 1 1 2 reading devotional material |
| 1 1 3 watching religious programming on tv or internet |
| 1 1 4 sacrament/other ritual (confession, healing) |
| 1 1 5 visit cemetery by one’s self |
| 1 1 6 talk with religious leader about spiritual issue(s) |
| 1 1 7 talk with lay person about spiritual issue(s) |
| 1 1 8 drive to/from spiritual activity |
| 1 1 9 other individual spiritual activity |
| 1 2 0 Group spiritual activities |
| 1 2 1 family prayer (incl. grace at meals) |
| 1 2 2 attend public worship |
| 1 2 3 drive to/from or drop off youth group for child |
| 1 2 4 drive to/from or drop off group spiritual activity (for self or family) |
| 1 2 5 attend bible study |
| 1 2 6 attend Sunday school/church school/Hebrew school/religious school |
| 1 2 7 attend wedding, baptism, funeral, bat mitzvah, festival, etc. |
| 1 2 8 watching religious programming on tv or internet |
| 1 2 9 participate in 1 2 -step recovery program (meeting or call sponsor) |
| 1 2 10 attend social hour related to worship (coffee hour, breakfast) |
| 1 2 11 visit cemetery with others |
| 1 2 12 attend small group activity at place of worship |
| 1 2 13 other group spiritual activity |
| 1 2 14 reading religious/spiritual literature |
| 1 3 0 Mind body spirit modalities |
| 1 3 1 drive to/from mind body spirit modality |
| 1 3 2 yoga |
| 1 3 3 massage |
| 1 3 4 chiropractic |
| 1 3 5 art therapy |
| 1 3 6 music therapy |
| 1 3 7 aroma therapy (incl. candles) |
| 1 3 8 acupuncture/acupressure |
| 1 3 9 healing touch/reiki |
| 1 3 10 other mind body spirit modality |
| 1 3 11 writing (journal, diary, creative, poetry, etc.) |
| 1 3 12 meditating |
Acknowledgements
Conflicts of Interest
Abbreviations
| CF | cystic fibrosis |
| DAS | Dyadic Adjustment Scale |
| DPD | Daily Phone Diary |
References and Notes
- Ety Berant, Mario Mikulincer, and Victor Florian. “Marital satisfaction among mothers of infants with congenital heart disease: the contribution of illness severity, attachment style, and the coping process.” Anxiety, Stress & Coping no. 4. 16 (2003): 397–415. [Google Scholar]
- Anne Marie Meijer, and Godfried L.H. van den Wittenboer. “Contribution of infants’ sleeep and crying to marital relationship of first-time parent couples in the 1st year after childbirth.” Journal of Family Psychology no. 1. 21 (2007): 49–57. [Google Scholar] [CrossRef]
- Cystic Fibrosis Foundation. “About Cystic Fibrosis.” Available online: http://www.cff.org/AboutCF/ (accessed on 12 November 2013).
- Cecile Loetz, Jakob Muller, Eckhard Frick, Yvonne Petersen, Niels Christian Hvidt, and Christine Mauer. “Attachment theory and spirituality: Two threads converging in palliative care? ” Evidence-Based Complementary and Alternative Medicine 2013 (2013): 1–14. [Google Scholar]
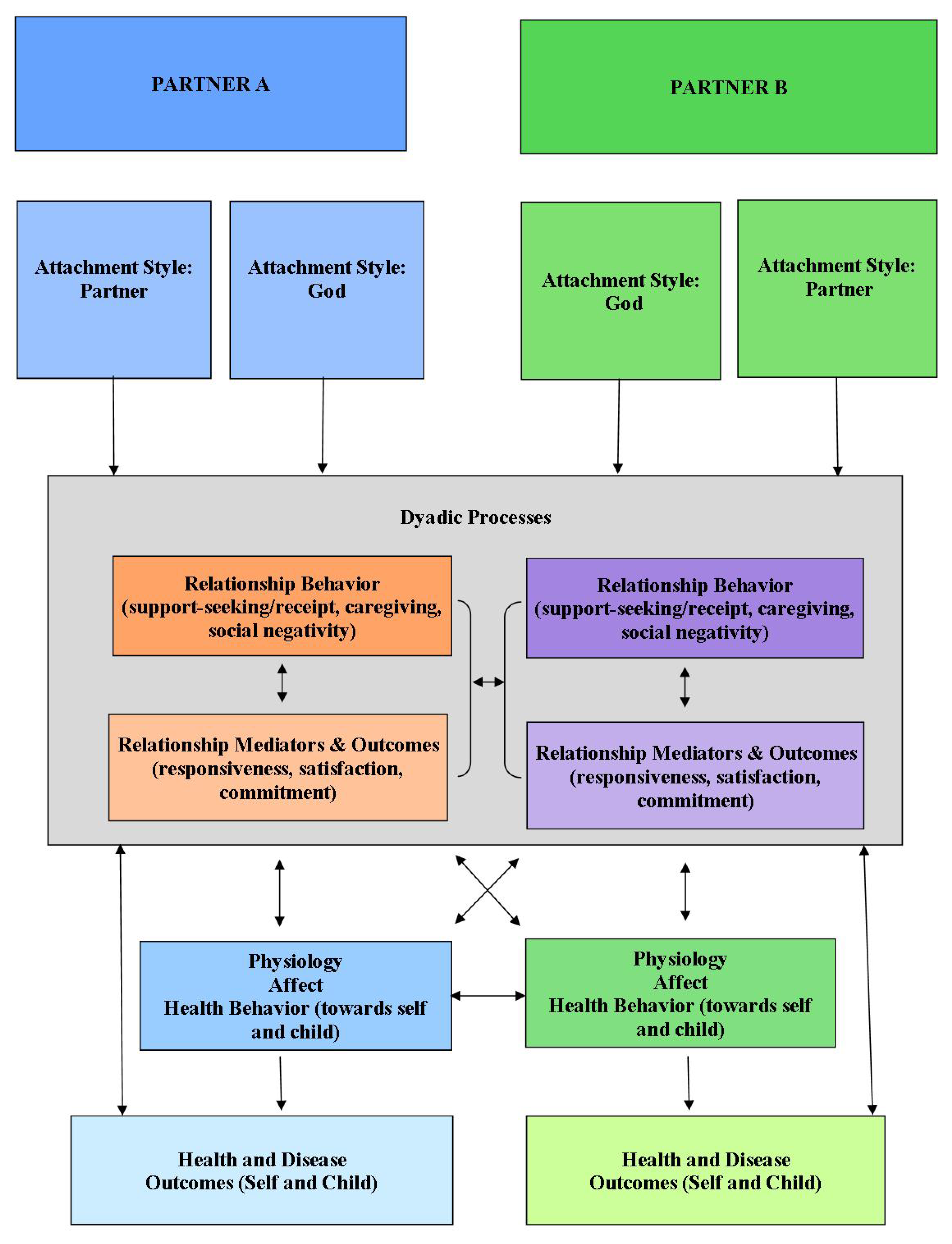
- Paula R. Pietromonaco, Bert Uchino, and Christine Dunkel Schetter. “Close relationship processes and health: Implications of attachment theory for health and disease.” Health Psychology no. 5. 32 (2013): 499–513. [Google Scholar] [CrossRef]
- Kevin J. Flannelly, and Kathleen Galek. “Religion, evolution and mental health: Attachment theory and ETAS theory.” Journal of Religion and Health no. 3. 49 (2010): 337–350. [Google Scholar] [CrossRef]
- Frank Newport. “More Than 9 in 10 Americans Continue to Believe in God.” Gallup. 3 June 2011. Available online: http://www.gallup.com/poll/147887/Americans-Continue-Believe-God.aspx.
- Frank Newport. “Seven in 10 Americans are very or moderately religious.” Gallup Politics. 15 April 2013. Available online: http://www.gallup.com/poll/159050/seven-americans-moderately-religious.aspx?ref=more.
- Kenneth I. Pargament, Harold G. Koenig, and Lisa M. Perez. “The many methods of religious coping: Development and initial validation of the RCOPE.” Journal of Clinical Psychology no. 4. 56 (2000): 519–543. [Google Scholar] [CrossRef]
- Daniel H. Grossoehme, Judy R. Ragsdale, Jamie L. Wooldridge, Sian Cotton, and Michael Seid. “We can handle this’: Parents’ use of religion in the first year following their child’s diagnosis with cystic fibrosis.” Journal of Health Care Chaplaincy no. 3. 16 (2010): 95–108. [Google Scholar]
- Daniel H. Grossoehme, and Sian Cotton. “Religious/Spiritual Coping by Parents of Adolescents with Sickle Cell Disease: A Pilot Study.” In Paper read at 1st Annual Meeting, Society for Spirituality, Theology and Health, Durham, North Carolina, 26 June 2008.
- Nalini Tarakeshwar, and Kenneth I. Pargament. “Religious coping in families of children with autism.” Focus on Autism and other Developmental Disabilities no. 4. 16 (2001): 247–260. [Google Scholar] [CrossRef]
- Harold G. Koenig, Dana King, and Verna B. Carson, eds. Handbook of Religion and Health. New York, NY: Oxford University Press, 2012.
- Annette Mahoney. “Religion in families 1999 to 2009: A relational spirituality framework.” Journal of Marriage and Family no. 4. 72 (2010): 805–827. [Google Scholar] [CrossRef]
- Marianne Dainton, Laura Stafford, and Daniel H. Canary. “Maintenance strategies and physical affection as predictors of love, liking, and satisfacation in marriage.” Communication Reports no. 2. 7 (1994): 88–98. [Google Scholar] [CrossRef]
- Mary W. Hicks, Lenore M. McWey, Kristen E. Benson, and Stacy Hernandez West. “Using what premarital couples already know to inform marriage education: Integration of a Gottman model perspective.” Contemporary Family Therapy no. 1. 26 (2004): 97–113. [Google Scholar] [CrossRef]
- Harold G. Koenig, Michael E. McCullough, and David B. Larson. Handbook of Religion and Health. New York, NY: Oxford University Press, 2001. [Google Scholar]
- Loren Marks. “Religion and family relational health: An overview and conceptual model.” Journal of Religion and Health no. 4. 45 (2006): 603–618. [Google Scholar] [CrossRef]
- Dennis Drotar, and Carolyn E. Ievers. “Age differences in parent and child responsibilities for management of cystic fibrosis and insulin-dependent diabetes mellitus.” Journal of Developmental and Behavioral Pediatrics no. 4. 15 (1994): 265–272. [Google Scholar]
- Paul A. Harris, Robert Taylor, Robert Thielke, Jonathon Payne, Nathaniel Gonzalez, and Jose G. Conde. “Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support.” Journal of Biomedical Informatics no. 2. 42 (2009): 377–381. [Google Scholar] [CrossRef]
- Graham B. Spanier. “Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads.” Journal of Marriage and Family no. 1. 38 (1976): 15–28. [Google Scholar] [CrossRef]
- Martin Fishbein, and Icek Ajzen. Predicting and Changing Behavior. New York, NY: Taylor & Francis, 2010. [Google Scholar]
- Stephane Sabourin, Pierre Valois, and Yvan Lussier. “Development and validation of a brief version of the Dyadic Adjustment Scale with a nonparametric item analysis model.” Psychological Assessment no. 1. 17 (2005): 15–27. [Google Scholar] [CrossRef]
- Alan Booth, David R. Johnson, Ann Branaman, and Alan Sica. “Belief and behavior: Does religion matter in today’s marriage? ” Journal of Marriage and Family no. 3. 57 (1995): 661–671. [Google Scholar] [CrossRef]
- Alexandra L. Quittner, Dorothy L. Espelage, Lisa C. Opipari, Bryan D. Carter, and Howard Eigen. “Role strain in couples with and without a chronically ill child: Associations with marital satisfaction, intimacy and daily mood.” Health Psychology no. 2. 17 (1998): 112–124. [Google Scholar] [CrossRef]
- Alexandra L. Quittner, and Lisa C. Opipari. “Differential treatment of siblings: interview and diary analyses comparing two family contexts.” Child Development no. 3. 65 (1994): 800–814. [Google Scholar] [CrossRef]
- Alexandra L. Quittner, Avani C. Modi, Kathleen L. Lemanek, Carolyn E. Ievers-Landis, and Michael A. Rapoff. “Evidence-based assessment of adherence to medical treatments in pediatric psychology.” Journal of Pediatric Psychology no. 9. 33 (2007): 916–936. [Google Scholar]
- Mark R. Elkins, Michael Robinson, Barbara R. Rose, Colin Harbour, Carmel P. Moriarty, Guy B. Marks, Elena G. Belousova, Wei Xuan, and Peter T.P. Bye. “A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis.” New England Journal of Medicine no. 3. 354 (2006): 229–240. [Google Scholar] [CrossRef]
- Bonnie W. Ramsey, Margaret S. Pepe, Joanne M. Quan, Lelly L. Otto, A. Bruce Montgomery, Judy Williams-Warren, Michael Vasijev-K, Drucy Borowitz, C. Michael Bowman, Bruce C. Marshall, and et al. “Intermittent administration of inhaled tobramycin in patients with cystic fibrosis.” New England Journal of Medicine no. 1. 340 (1999): 23–30. [Google Scholar] [CrossRef]
- Philip L. Roth. “Missing data: A conceptual review for applied psychologists.” Personnel Psychology no. 3. 47 (1994): 537–560. [Google Scholar] [CrossRef]
- Fang Wang, Steven Pedlow, and Yongyi Wang. “NORCSuite_Impute: Two-way search hot-deck imputation macro using a flexible number of donors and donr use limit with SAS IML.” In Paper presented at Joint Statistical Meeting, SanDiego, CA, 28 July to 2 Auguest 2012.
- Alan Agresti. Categorical Data Analysis, 3rd ed. Hoboken, NY: Wiley, 2013. [Google Scholar]
- William J. Youden. “An index for rating diagnostic tests.” Cancer no. 1. 3 (1950): 32–35. [Google Scholar] [CrossRef]
- Jessica A. Parker, Barbara Mandleco, Susanne Olsen Roper, Donna Freeborn, and Tina Taylor Dyches. “Religiosity, spirituality, and martial relationships of parents raising a typically developing child or a child with a disabilty.” Journal of Family Nursing no. 1. 14 (2011): 82–104. [Google Scholar]
- Caprice Knapp, Vanessa Madden, Hua Wang, Charlotte Curtis, Phyllis Sloyer, and Elizabeth Shenkman. “Spirituality of parents of children in palliative care.” Journal of Palliative Medicine no. 4. 14 (2011): 437–443. [Google Scholar] [CrossRef]
- Daniel H. Grossoehme, Judith R. Ragsdale, Amy Snow, and Michael Seid. “We were chosen as a family: Parents’ evolving use of religion when their child has cystic fibrosis.” Journal of Religion and Health no. 4. 51 (2012): 1347–1358. [Google Scholar] [CrossRef]
- David C. Dollahite, Loren D. Marks, and Michael M. Olson. “Faithful fathering in trying times: Religious beliefs and practices of latter-day saint fathers of children with special needs.” The Journal of Men’s Studies no. 1. 7 (1997): 71–93. [Google Scholar]
- Matthijs Kalmijn, and Wim Bernasco. “Joint and separated lifestyles in couple relationships.” Journal of Marriage and Family no. 3. 63 (2011): 639–654. [Google Scholar]
- Robyn Parker. “Why marriages last: a discussion of the literature.” Research Paper No. 28; Melbourne, Australia: Australian Institute of Family Studies, 2002. [Google Scholar]
- Anne E. Kazak, Alice Prusak, Mary McSherry, Steven Simms, David Beele, Mary Rourke, Melissa Alderfer, and Beverly Lange. “The Psychosocial Assessment Tool (PAT)©: Pilot data on a brief screening instrument for identifying high risk families in pediatric oncology.” Families, Systems & Health no. 3. 19 (2001): 303–317. [Google Scholar]
- Jan Gordon Walker. “A marital intervention program for couples with chronically ill children.” Ph.D. Dissertation, Univeristy of Ottawa, 1994. [Google Scholar]
- Joanne E. Kersh, Tara T. Hedvat, Penny Hauser-Cram, and Marji Erickson Warfield. “The contribution of marital quality to the well-being of parents of children with developmental disabilities.” Journal of Intellectual & Developmental Disability no. 12. 50 (2006): 883–893. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Grossoehme, D.H.; Szczesniak, R.; Dodd, C.; Opipari-Arrigan, L. Dyadic Adjustment and Spiritual Activities in Parents of Children with Cystic Fibrosis. Religions 2014, 5, 385-401. https://doi.org/10.3390/rel5020385
Grossoehme DH, Szczesniak R, Dodd C, Opipari-Arrigan L. Dyadic Adjustment and Spiritual Activities in Parents of Children with Cystic Fibrosis. Religions. 2014; 5(2):385-401. https://doi.org/10.3390/rel5020385
Chicago/Turabian StyleGrossoehme, Daniel H., Rhonda Szczesniak, Caitlin Dodd, and Lisa Opipari-Arrigan. 2014. "Dyadic Adjustment and Spiritual Activities in Parents of Children with Cystic Fibrosis" Religions 5, no. 2: 385-401. https://doi.org/10.3390/rel5020385
APA StyleGrossoehme, D. H., Szczesniak, R., Dodd, C., & Opipari-Arrigan, L. (2014). Dyadic Adjustment and Spiritual Activities in Parents of Children with Cystic Fibrosis. Religions, 5(2), 385-401. https://doi.org/10.3390/rel5020385




