To Get Vaccinated, or Not to Get Vaccinated, That Is the Question: Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Predictors of COVID-19 Vaccination Willingness among Young Adults in The Netherlands
Abstract
:1. Introduction
1.1. Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Determinants of the Willingness to Receive the COVID-19 Vaccine
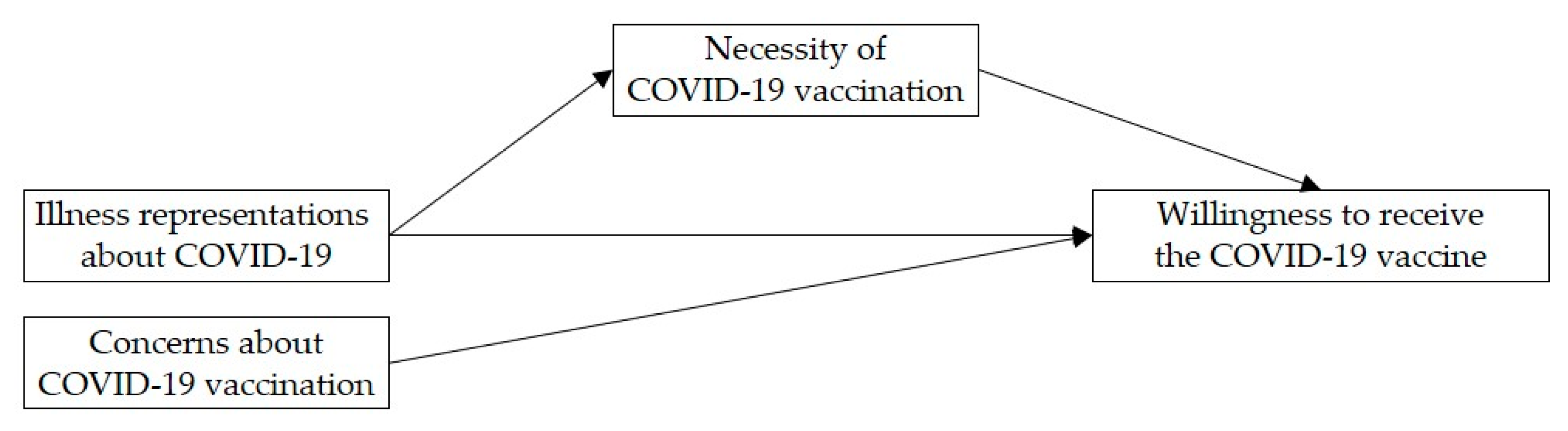
1.2. The Present Study
2. Materials and Methods
2.1. Procedure and Participants
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Associations of Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination with the Willingness to Receive the COVID-19 Vaccine
3.2. Associations of Illness Representations about COVID-19 with Perceptions of Necessity of COVID-19 Vaccination
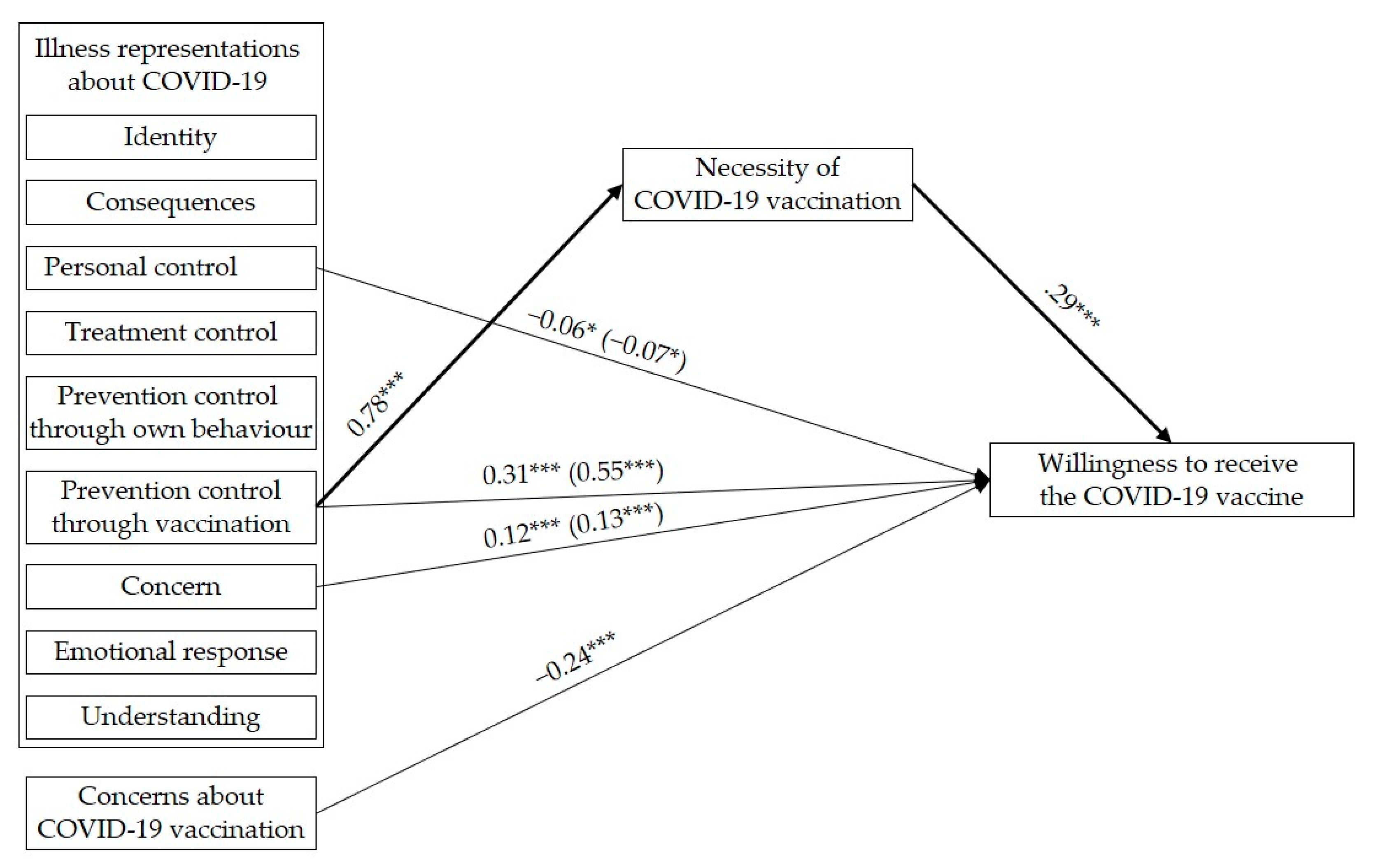
3.3. Direct and Indirect Effects of Illness Representations about COVID-19 via Perceptions of Necessity of COVID-19 Vaccination and Direct Effects of Concerns about COVID-19 Vaccination on the Willingness to Receive the COVID-19 Vaccine
| Predictors | Outcome | |||
|---|---|---|---|---|
| Perceptions of Necessity of the Vaccination | Willingness to Receive the Vaccine (Direct Effect) | Willingness to Receive the Vaccine (Total Effect) | Indirect Effect a via Necessity | |
| ß | ß | ß | ß (BC 95% CI) | |
| Illness representations | ||||
| Identity | −0.01 | 0.02 | 0.01 | −0.00 (−0.02, 0.01) |
| Consequences | −0.02 | 0.05 | 0.04 | −0.01 (−0.02, 0.01) |
| Personal control | −0.03 | −0.06 * | −0.07 * | −0.01 (−0.02, 0.01) |
| Treatment control | 0.01 | 0.04 | 0.05 | 0.00 (−0.01, 0.02) |
| Prevention control through own behavior | 0.03 | 0.04 | 0.04 | 0.01 (−0.01, 0.03) |
| Prevention control through vaccination | 0.79 *** | 0.31 *** | 0.55 *** | 0.23 (0.15, 0.32) |
| Concern | 0.02 | 0.12 *** | 0.13 *** | 0.01 (−0.01, 0.03) |
| Emotional response | 0.02 | −0.00 | 0.00 | 0.01 (−0.01, 0.02) |
| Understanding | 0.03 | −0.03 | −0.02 | 0.01 (−0.01, 0.02) |
| Treatment perceptions | ||||
| Necessity | - | 0.29 *** | - | - |
| Concerns | - | −0.24 *** | - | - |
4. Discussion
4.1. Practical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dagan, N.; Barda, N.; Kepten, E.; Miron, O.; Perchik, S.; Katz, M.A.; Hernán, M.A.; Lipsitch, M.; Reis, B.; Balicer, R.D. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N. Engl. J. Med. 2021, 384, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Zu, J.; Fairley, C.K.; Pagán, J.A.; An, L.; Du, Z.; Guo, Y.; Rong, L.; Xiao, Y.; Zhuang, G.; et al. Projected COVID-19 epidemic in the United States in the context of the effectiveness of a potential vaccine and implications for social distancing and face mask use. Vaccine 2021, 39, 2295–2302. [Google Scholar] [CrossRef]
- Vasileiou, E.; Simpson, C.R.; Shi, T.; Kerr, S.; Agrawal, U.; Akbari, A.; Bedston, S.; Beggs, J.; Bradley, D.; Chuter, A.; et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: A national prospective cohort study. Lancet 2021, 397, 1–7. [Google Scholar] [CrossRef]
- Teslya, A.; Pham, T.M.; Godijk, N.G.; Kretzschmar, M.E.; Bootsma, M.C.; Rozhnova, G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med. 2020, 17, e1003166. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. Situation by WHO Region; Europe. Available online: https://covid19.who.int/ (accessed on 15 May 2021).
- Actuele Informatie over COVID-19. Wekelijkse Update COVID-19: Maart 2021. Available online: https://www.rivm.nl/coronavirus-covid-19/actueel (accessed on 13 April 2021).
- National Institute for Public Health and the Environment. Impact van de Eerste COVID-19 Golf Op de Reguliere Zorg en Gezondheid Inventarisatie van de Omvang van Het Probleem en Eerste Schatting van Gezondheidseffecten; RIVM: Bilthoven, The Netherlands, 2020. [CrossRef]
- Varga, T.V.; Bu, F.; Dissing, A.S.; Elsenburg, L.K.; Bustamante, J.J.H.; Matta, J.; van Zon, S.K.R.; Brouwer, S.; Bültmann, U.; Fancourt, D.; et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health-Eur. 2021, 2, 100020. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, L.S.; Nielsen, J.; Richter, L.; Schmid, D.; Bustos, N.; Braeye, T.; Denissov, G.; Veideman, T.; Luomala, O.; Möttönen, T.; et al. Excess all-cause mortality during the COVID-19 pandemic in Europe–preliminary pooled estimates from the EuroMOMO network, March to April 2020. Eurosurveillance 2020, 25, 2001214. [Google Scholar] [CrossRef] [PubMed]
- Economic Impact of COVID-19. Available online: https://www.cbs.nl/en-gb/dossier/coronavirus-crisis-cbs-figures/economic-impact-of-covid-19 (accessed on 19 April 2021).
- COVID-19 Vaccines: Authorised. Authorised COVID-19 Vaccines. Available online: https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/covid-19-vaccines-authorised#authorised-covid-19-vaccines-section (accessed on 21 April 2021).
- Randolph, H.E.; Barreiro, L.B. Herd immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; Vegvari, C.; Truscott, J.; Collyer, B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet 2020, 396, 1614–1616. [Google Scholar] [CrossRef]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- WHO’s Science in 5 on COVID-19—Herd Immunity. Available online: https://youtu.be/U47SaDAmyrE (accessed on 21 April 2021).
- Coronavirus Disease (COVID-19): Herd Immunity. Lockdowns and COVID-19. Available online: https://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19 (accessed on 21 April 2021).
- IPSOS; NOS. Nederlanders over de Coronavaccinatie; IPSOS: Amsterdam, The Netherlands, 2021; Available online: https://www.ipsos.com/sites/default/files/ct/news/documents/2021-01/ipsos_nos_vaccinatiebereidheid_v3.0.pdf (accessed on 22 April 2021).
- Vaccinatiebereidheid. Verandering in Vaccinatiebereidheid. Available online: https://www.rivm.nl/gedragsonderzoek/maatregelen-welbevinden/vaccinatiebereidheid (accessed on 21 April 2021).
- Aw, J.; Seng, J.J.B.; Seah, S.S.Y.; Low, L.L. COVID-19 vaccine hesitancy—A scoping review of literature in high-income countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Eén op de Tien Test Positief. Positieve Coronatesten. Available online: https://www.rivm.nl/nieuws/een-op-de-tien-test-positief (accessed on 21 April 2021).
- Naleving van en Draagvlak Voor de Basis Gedragsregels. Naleving en Draagvlak van de Gedragsregels per Leeftijdscategorie. Available online: https://www.rivm.nl/gedragsonderzoek/trendonderzoek (accessed on 21 April 2021).
- Tomczyk, S.; Rahn, M.; Schmidt, S. Social distancing and stigma: Association between compliance with behavioral recommendations, risk perception, and stigmatizing attitudes during the COVID-19 outbreak. Front. Psychol. 2020, 11, 1821. [Google Scholar] [CrossRef] [PubMed]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G.; Gottleib, N.H.; Fernández, M.E. Planning Health Promotion Programs: An. Intervention Mapping Approach, 3rd ed.; Wiley Jossey-Bass: San Francisco, CA, USA, 2011. [Google Scholar]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Leventhal, H.; Brissette, I.; Leventhal, E.A. The common-sense model of self-regulation of health and illness. In The Self-Regulation of Health and Illness Behaviour; Cameron, L.D., Leventhal, H., Eds.; Routledge: New York, NY, USA, 2003; pp. 42–65. [Google Scholar] [CrossRef]
- Horne, R. Treatment perceptions and self-regulation In The Self-Regulation of Health and Illness Behaviour; Cameron, L.D., Leventhal, H., Eds.; Routledge: New York, NY, USA, 2003; pp. 138–153. [Google Scholar] [CrossRef]
- Leventhal, H.; Leventhal, E.A.; Contrada, R.J. Self-regulation, health, and behaviour: A perceptual-cognitive approach. Psychol. Health 1998, 13, 717–733. [Google Scholar] [CrossRef]
- Leventhal, H.; Phillips, L.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Moss-Morris, R.; Weinman, J.; Petrie, K.J.; Horne, R.; Cameron, L.D.; Buick, D. The revised Illness Perception Questionnaire (IPQ-R). Psychol. Health 2002, 17, 1–16. [Google Scholar] [CrossRef]
- Bish, A.; Michie, S. Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. Br. J. Health Psychol. 2010, 15, 797–824. [Google Scholar] [CrossRef] [Green Version]
- Cameron, L.D. Illness risk representations and motivations to engage in protective behavior: The case of skin cancer risk. Psychol. Health 2008, 23, 91–112. [Google Scholar] [CrossRef]
- Figueiras, M.J.; Alves, N.C. Lay perceptions of serious illnesses: An adapted version of the Revised Illness Perception Questionnaire (IPQ-R) for healthy people. Psychol. Health 2007, 22, 143–158. [Google Scholar] [CrossRef]
- Garg, R.; Meraya, A.; Murray, P.J.; Kelly, K. Illness representations of pertussis and predictors of child vaccination among mothers in a strict vaccination exemption state. Matern. Child Health J. 2018, 22, 137–146. [Google Scholar] [CrossRef]
- Karademas, E.C.; Bati, A.; Karkania, V.; Georgiou, V.; Sofokleous, S. The association between pandemic influenza A (H1N1) public perceptions and reactions: A prospective study. J. Health Psychol. 2013, 18, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.; Griffiths, S.; Choi, K.C.; Lin, C. Prevalence of preventive behaviors and associated factors during early phase of the H1N1 influenza epidemic. Am. J. Infect. Control. 2010, 38, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.T.; Yang, X.; Tsui, H.Y.; Kim, J.H. Prevalence of influenza vaccination and associated factors among community-dwelling Hong Kong residents of age 65 or above. Vaccine 2006, 24, 5526–5534. [Google Scholar] [CrossRef] [PubMed]
- Marmarà, D.; Marmarà, V.; Hubbard, G. Health beliefs, illness perceptions and determinants of breast screening uptake in Malta: A cross-sectional survey. BMC Public Health 2017, 17, 416. [Google Scholar] [CrossRef]
- Renner, B.; Reuter, T. Predicting vaccination using numerical and affective risk perceptions: The case of A/H1N1 influenza. Vaccine 2012, 30, 7019–7026. [Google Scholar] [CrossRef]
- Salewski, C.; Trusch, B.; Vollmann, M. How effective is a short CSM-based online intervention on intended flu prevention behaviour? In Proceedings of the 31st Conference of the European Health Psychology Society (EHPS), Padua, Italy, 29 August–2 September 2017. [Google Scholar] [CrossRef]
- Setbon, M.; Raude, J. Factors in vaccination intention against the pandemic influenza A/H1N1. Eur. J. Public Health 2010, 20, 490–494. [Google Scholar] [CrossRef] [Green Version]
- Vollmann, M.; Engelhardt, G.; Salewski, C. Effects of a brief multimodal online intervention on the intention to conduct sun protective behaviours through targeting illness representations about skin cancer: A randomized controlled trial. Psychol. Health 2021, 36, 253–270. [Google Scholar] [CrossRef]
- Wang, Z.; Fang, Y.; Dong, W.; Lau, M.; Mo, P.K. Illness representations on pneumonia and pneumococcal vaccination uptake among community-living Chinese people with high-risk conditions aged ≥65 years—A population-based study. Hum. Vaccines Immunother. 2021, 17, 1455–1462. [Google Scholar] [CrossRef]
- Neto, D.D.; da Silva, A.N.; Roberto, M.S.; Lubenko, J.; Constantinou, M.; Nicolaou, C.; Lamnisos, D.; Papacostas, S.; Höfer, S.; Presti, G.; et al. Illness Perceptions of COVID-19 in Europe: Predictors, Impacts and Temporal Evolution. Front. Psychol. 2021, 12, 640955. [Google Scholar] [CrossRef]
- Horne, R.; Clatworthy, J. Adherence to advice and treatment. In Health Psychology, 2nd ed.; French, D., Vedhara, K., Kaptein, A.A., Weinman, J., Eds.; Blackwell Publishing Ltd.: Oxford, UK, 2010; pp. 175–188. [Google Scholar]
- Foot, H.; La Caze, A.; Gujral, G.; Cottrell, N. The necessity–concerns framework predicts adherence to medication in multiple illness conditions: A meta-analysis. Patient Educ. Couns. 2016, 99, 706–717. [Google Scholar] [CrossRef] [Green Version]
- Horne, R.; Weinman, J. Self-regulation and self-management in asthma: Exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychol. Health 2002, 17, 17–32. [Google Scholar] [CrossRef]
- Horne, R.; Chapman, S.C.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE 2013, 8, e80633. [Google Scholar] [CrossRef]
- Myers, L.B.; Goodwin, R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health 2011, 11, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef]
- Vasilevska, M.; Ku, J.; Fisman, D.N. Factors associated with healthcare worker acceptance of vaccination: A systematic review and meta-analysis. Infect. Control. Hosp. Epidemiol. 2014, 35, 699–708. [Google Scholar] [CrossRef]
- Andela, C.D.; Biermasz, N.R.; Kaptein, A.A.; Pereira, A.M.; Tiemensma, J. More concerns and stronger beliefs about the necessity of medication in patients with acromegaly are associated with negative illness perceptions and impairment in quality of life. Growth Horm. IGF Res. 2015, 25, 219–226. [Google Scholar] [CrossRef]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The Brief Illness Perception Questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Moon, Z.; Moss-Morris, R.; Hunter, M.S.; Hughes, L.D. Measuring illness representations in breast cancer survivors (BCS) prescribed tamoxifen: Modification and validation of the Revised Illness Perceptions Questionnaire (IPQ-BCS). Psychol. Health 2017, 32, 439–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, E.C.; O’Neill, M.; Hughes, L.D.; Moss-Morris, R. An illness-specific version of the Revised Illness Perception Questionnaire in patients with atrial fibrillation (AF IPQ-R): Unpacking beliefs about treatment control, personal control and symptom triggers. Psychol. Health 2018, 33, 499–517. [Google Scholar] [CrossRef] [Green Version]
- Tiemensma, J.; Andela, C.D.; Pereira, A.M.; Romijn, J.A.; Biermasz, N.R.; Kaptein, A.A. Patients with adrenal insufficiency hate their medication: Concerns and stronger beliefs about the necessity of hydrocortisone intake are associated with more negative illness perceptions. J. Clin. Endocrinol. Metab. 2014, 99, 3668–3676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilhelm, M.; Rief, W.; Doering, B.K. It’s all a matter of necessity and concern: A structural equation model of adherence to antihypertensive medication. Patient Educ. Couns. 2018, 101, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Berglund, E.; Lytsy, P.; Westerling, R. Adherence to and beliefs in lipid-lowering medical treatments: A structural equation modeling approach including the necessity-concern framework. Patient Educ. Couns. 2013, 9, 105–112. [Google Scholar] [CrossRef] [PubMed]
- De Raaij, E.J.; Schröder, C.; Maissan, F.J.; Pool, J.J.; Wittink, H. Cross-cultural adaptation and measurement properties of the Brief Illness Perception Questionnaire-Dutch language version. Man. Ther. 2012, 17, 330–335. [Google Scholar] [CrossRef]
- Martin, L.R.; Petrie, K.J. Understanding the dimensions of anti-vaccination attitudes: The vaccination attitudes examination (VAX) scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis, 2nd ed.; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Clatworthy, J.; Bowskill, R.; Parham, R.; Rank, T.; Scott, J.; Horne, R. Understanding medication non-adherence in bipolar disorders using a Necessity-Concerns Framework. J. Affect. Disord. 2009, 116, 51–55. [Google Scholar] [CrossRef]
- Horne, R.; Cooper, V.; Gellaitry, G.; Date, H.L.; Fisher, M. Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence: The utility of the necessity-concerns framework. J. Acquir. Immune Defic. Syndr. 2007, 45, 334–341. [Google Scholar] [CrossRef]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2021, 1–25. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef]
- Bish, A.; Yardley, L.; Nicoll, A.; Michie, S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine 2011, 29, 6472–6484. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Chilcot, J.; Moss-Morris, R. Changes in illness-related cognitions rather than distress mediate improvements in irritable bowel syndrome (IBS) symptoms and disability following a brief cognitive behavioural therapy intervention. Behav. Res. Ther. 2013, 51, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Granger, B.B.; Ekman, I.; Hernandez, A.F.; Sawyer, T.; Bowers, M.T.; DeWald, T.A.; Zhao, Y.; Levy, J.; Bosworth, H.B. Results of the Chronic Heart Failure Intervention to Improve MEdication Adherence study: A randomized intervention in high-risk patients. Am. Heart J. 2015, 169, 539–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karamanidou, C.; Weinman, J.; Horne, R. Improving haemodialysis patients’ understanding of phosphate-binding medication: A pilot study of a psycho-educational intervention designed to change patients’ perceptions of the problem and treatment. Br. J. Health Psychol. 2008, 13, 205–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kok, G.; Peters, G.-J.Y.; Kessels, L.T.E.; ten Hoor, G.A.; Ruiter, R.A.C. Ignoring theory and misinterpreting evidence: The false belief in fear appeals. Health Psychol. Rev. 2018, 12, 111–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheeran, P.; Webb, T.L. The intention–behavior gap. Soc. Pers. Psychol. Compass 2016, 10, 503–518. [Google Scholar] [CrossRef]
- Lehmann, B.A.; Ruiter, R.A.; Chapman, G.; Kok, G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine 2014, 32, 6986–6991. [Google Scholar] [CrossRef] [Green Version]
- Pot, M.; van Keulen, H.M.; Ruiter, R.A.; Eekhout, I.; Mollema, L.; Paulussen, T.W. Motivational and contextual determinants of HPV-vaccination uptake: A longitudinal study among mothers of girls invited for the HPV-vaccination. Prev. Med. 2017, 100, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Winer, E.S.; Cervone, D.; Bryant, J.; McKinney, C.; Liu, R.T.; Nadorff, M.R. Distinguishing mediational models and analyses in clinical psychology: Atemporal associations do not imply causation. J. Clin. Psychol. 2016, 72, 947–955. [Google Scholar] [CrossRef] [PubMed]
- McGrath, A. Dealing with dissonance: A review of cognitive dissonance reduction. Soc. Pers. Psychol. Compass 2017, 11, 1–17. [Google Scholar] [CrossRef]
- Rademakers, J.; Waverijn, G.; Rijken, M.; Osborne, R.; Heijmans, M. Towards a comprehensive, person-centred assessment of health literacy: Translation, cultural adaptation and psychometric test of the Dutch Health Literacy Questionnaire. BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Rowlands, G. Health literacy: Ways to maximise the impact and effectiveness of vaccination information. Hum. Vaccines Immunother. 2014, 10, 2130–2135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fishbein, M. A reasoned action approach to health promotion. Med. Decis. Mak. 2008, 28, 834–844. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R. Health Action Process Approach (HAPA) as a theoretical framework to understand behavior change. Actual. Psicol. 2016, 30, 119–130. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Reno, C.; Maietti, E.; Fantini, M.P.; Savoia, E.; Manzoli, L.; Montalti, M.; Gori, D. Enhancing COVID-19 vaccines acceptance: Results from a survey on vaccine hesitancy in Northern Italy. Vaccines 2021, 9, 378. [Google Scholar] [CrossRef] [PubMed]
| Gender | Occupation | ||
|---|---|---|---|
| female | 408 (69.9%) | working | 285 (48.9%) |
| male | 167 (28.6%) | student/in training | 285 (48.9%) |
| other | 8 (1.4%) | homemaker | 1 (0.2%) |
| no information | 1 (0.2%) | unemployed | 12 (2.1%) |
| Highest education (ongoing or completed) | Higher risk of severe COVID-19 due to an underlying heath condition | ||
| secondary or vocational education | 32 (5.5%) | yes | 553 (94.7%) |
| tertiary education | 552 (94.5%) | no | 31 (5.5%) |
| Previous COVID-19 infection (self) | Previous COVID-19 infection (others) | ||
| no | 450 (77.1%) | no | 89 (15.2%) |
| yes, but not tested | 58 (9.9%) | yes | 478 (81.8%) |
| yes, confirmed by a test | 76 (13.0%) | not sure | 17 (2.9%) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | M (SD) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Vaccination willingness a | 8.10 (2.96) | ||||||||||||
| Illness representations a | |||||||||||||
| 2 Identity | 0.19 *** | 4.49 (1.56) | |||||||||||
| 3 Timeline | 0.01 | 0.43 *** | 3.47 (1.67) | ||||||||||
| 4 Consequences | 0.19 *** | 0.30 *** | 0.20 *** | 6.30 (2.28) | |||||||||
| 5 Personal control | −0.15 *** | 0.04 | 0.06 | −0.01 | 4.10 (2.59) | ||||||||
| 6 Treatment control | 0.27 *** | 0.17 *** | 0.07 | 0.16 *** | 0.11 ** | 6.41 (2.18) | |||||||
| 7 Prevention control through own behavior | 0.30 *** | 0.15 *** | 0.05 | 0.14 ** | 0.06 | 0.23 *** | 6.89 (1.86) | ||||||
| 8 Prevention control through vaccination | 0.76 *** | 0.17 *** | 0.05 | 0.15 *** | −0.10 * | 0.32 *** | 0.31 *** | 7.65 (2.22) | |||||
| 9 Concern | 0.42 *** | 0.43 *** | 0.30 *** | 0.35 *** | −0.05 | 0.13 ** | 0.24 *** | 0.38 *** | 5.21 (2.39) | ||||
| 10 Emotional response | 0.19 *** | 0.18 *** | 0.16 *** | 0.17 *** | 0.01 | 0.04 | 0.05 | 0.20 *** | 0.40 *** | 5.79 (2.31) | |||
| 11 Understanding | 0.08 * | 0.03 | −0.06 | 0.09 * | 0.04 | 0.09 * | 0.20 *** | 0.12 ** | 0.03 | −0.01 | 7.14 (1.70) | ||
| Treatment perceptions b | |||||||||||||
| 12 Necessity | 0.76 *** | 0.14 ** | 0.02 | 0.12 ** | −0.11 ** | 0.27 *** | 0.28 *** | 0.82 *** | 0.33 *** | 0.18 *** | 0.12 ** | 3.50 (1.19) | |
| 13 Concerns | −0.61 *** | −0.04 | 0.03 | −0.03 | 0.10 * | −0.12 ** | −0.19 *** | −0.53 *** | −0.16 *** | −0.07 | −0.10 * | −0.57 *** | 2.87 (1.29) |
| Predictors | Outcome | |
|---|---|---|
| Willingness to Receive the Vaccine | Perceptions of Necessity of the Vaccination | |
| ß | ß | |
| Illness representations | ||
| Identity | 0.02 | −0.01 |
| Consequences | 0.05 | −0.02 |
| Personal control | −0.06 * | −0.03 |
| Treatment control | 0.04 | 0.01 |
| Prevention control through own behavior | 0.04 | 0.03 |
| Prevention control through vaccination | 0.31 *** | 0.79 *** |
| Concern | 0.12 *** | 0.02 |
| Emotional response | −0.00 | 0.02 |
| Understanding | −0.03 | 0.03 |
| Treatment perceptions | ||
| Necessity | 0.29 *** | - |
| Concerns | −0.24 *** | - |
| adj. R2 = 0.69 F(11,572) = 119.89 *** | adj. R2 = 0.66 F(9574) = 128.31 *** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vollmann, M.; Salewski, C. To Get Vaccinated, or Not to Get Vaccinated, That Is the Question: Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Predictors of COVID-19 Vaccination Willingness among Young Adults in The Netherlands. Vaccines 2021, 9, 941. https://doi.org/10.3390/vaccines9090941
Vollmann M, Salewski C. To Get Vaccinated, or Not to Get Vaccinated, That Is the Question: Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Predictors of COVID-19 Vaccination Willingness among Young Adults in The Netherlands. Vaccines. 2021; 9(9):941. https://doi.org/10.3390/vaccines9090941
Chicago/Turabian StyleVollmann, Manja, and Christel Salewski. 2021. "To Get Vaccinated, or Not to Get Vaccinated, That Is the Question: Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Predictors of COVID-19 Vaccination Willingness among Young Adults in The Netherlands" Vaccines 9, no. 9: 941. https://doi.org/10.3390/vaccines9090941
APA StyleVollmann, M., & Salewski, C. (2021). To Get Vaccinated, or Not to Get Vaccinated, That Is the Question: Illness Representations about COVID-19 and Perceptions about COVID-19 Vaccination as Predictors of COVID-19 Vaccination Willingness among Young Adults in The Netherlands. Vaccines, 9(9), 941. https://doi.org/10.3390/vaccines9090941