Protection Elicited by Attenuated Live Yersinia pestis Vaccine Strains against Lethal Infection with Virulent Y. pestis
Abstract
1. Introduction
2. Materials and Methods
2.1. Media and Chemicals
2.2. Mutant Construction
2.3. LD50 Determinations
2.4. Bacterial Strains
2.5. Animals and Vaccination Studies
2.6. Preparation of Vaccine Strains for Immunizations
2.7. Exposure of Immunized Mice to Virulent Y. pestis Challenge
2.8. Immune Response Assays
2.8.1. ELISAs
2.8.2. Cellular Responses: Analysis of Stimulated Splenocytes
2.9. Statistics
3. Results
3.1. Characterization of Virulent and Live Attenuated Y. pestis Strains
3.2. Safety and Efficacy of Live Vaccine Strain Candidates
3.3. Characterization of the Outbred CD-1 Mouse Strain: Susceptibility and Vaccine Responses
3.4. Humoral Immune Responses Elicited by Vaccines
3.5. Vaccine Optimization: Comparison of Vaccine Composition and Number of Doses
3.5.1. Protective Efficacy
3.5.2. Humoral Immune Responses
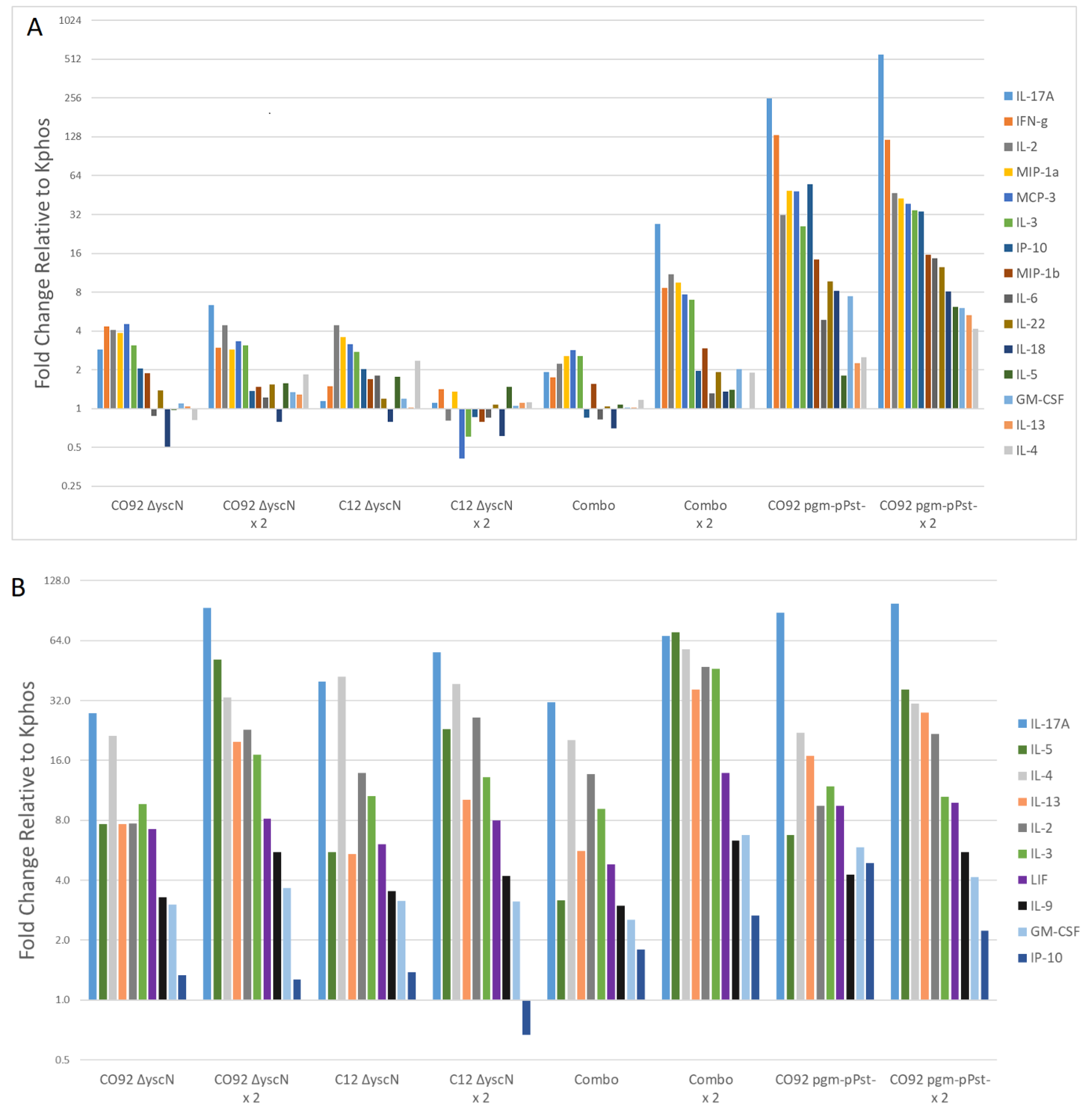
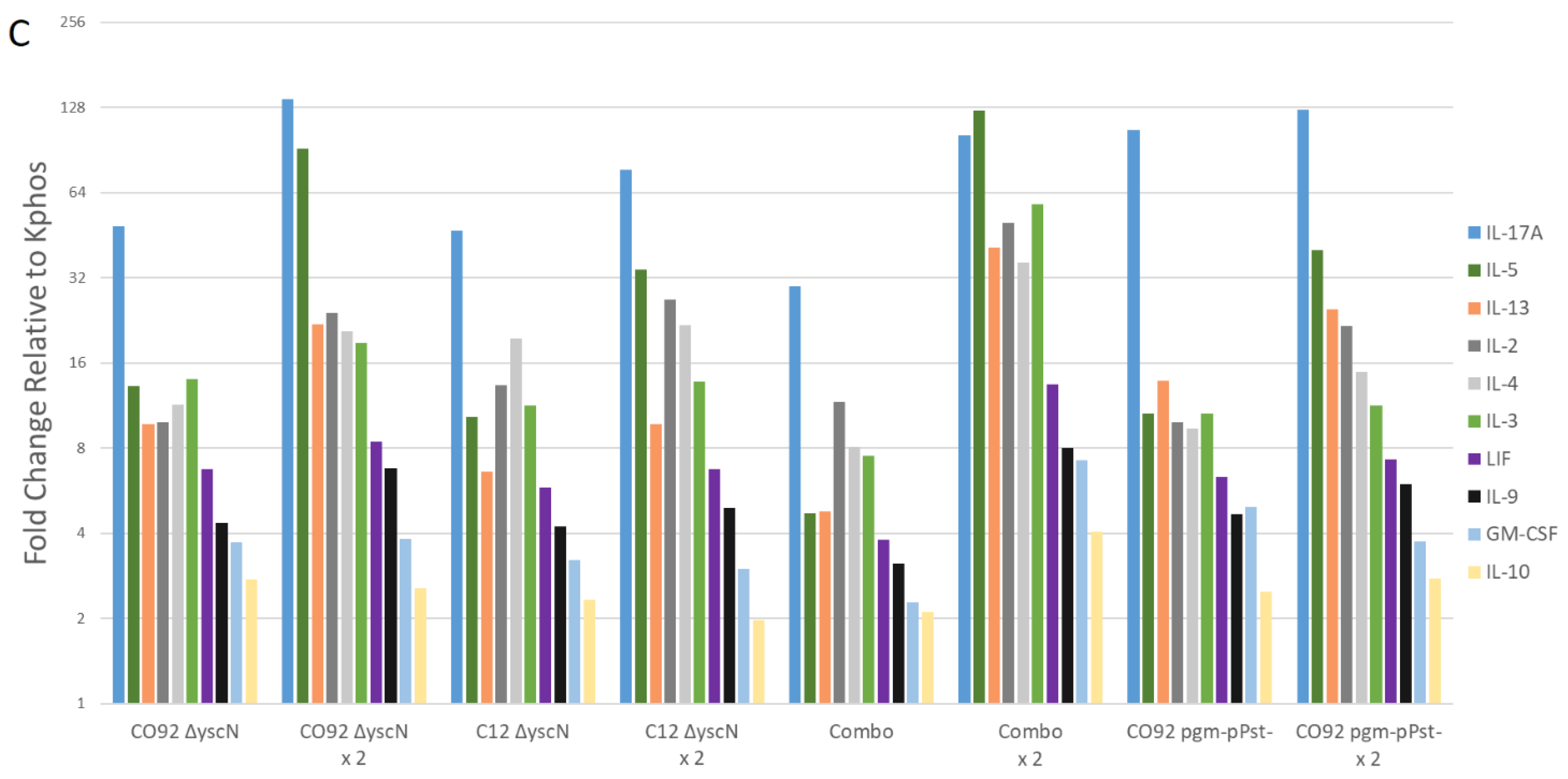
3.5.3. Cell-Mediated Immune Responses to the Live Vaccines
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Financial Disclosure
Conflicts of Interest
References
- Wang, X.; Zhang, X.; Zhou, D.; Yang, R. Live-attenuated Yersinia pestis vaccines. Expert Rev. Vaccines 2013, 12, 677–686. [Google Scholar] [CrossRef]
- Meyer, K.F. Effectiveness of live or killed plague vaccines in man. Bull. World Health Organ. 1970, 42, 653–666. [Google Scholar]
- Sun, W. Plague vaccines: Status and future. Adv. Exp. Med. Biol. 2016, 918, 313–360. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Tuteja, U. Plague vaccine development: Current research and future trends. Front. Immunol. 2016, 7, 602. [Google Scholar] [CrossRef] [PubMed]
- Andrews, G.P.; Strachan, S.T.; Benner, G.E.; Sample, A.K.; Anderson, G.W., Jr.; Adamovicz, J.J.; Welkos, S.L.; Pullen, J.K.; Friedlander, A.M. Protective efficacy of recombinant yersinia outer proteins against bubonic plague caused by encapsulated and nonencapsulated Yersinia pestis. Infect. Immun. 1999, 67, 1533–1537. [Google Scholar] [CrossRef]
- Welkos, S.L.; Davis, K.M.; Pitt, L.M.; Worsham, P.L.; Friedlander, A.M. Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib. Microbiol. Immunol. 1995, 13, 299–305. [Google Scholar]
- Worsham, P.L.; Stein, M.P.; Welkos, S.L. Construction of defined F1 negative mutants of virulent Yersinia pestis. Contrib. Microbiol. Immunol. 1995, 13, 325–328. [Google Scholar]
- Heath, D.G.; Anderson, G.W., Jr.; Mauro, J.M.; Welkos, S.L.; Andrews, G.P.; Adamovicz, J.; Friedlander, A.M. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine 1998, 16, 1131–1137. [Google Scholar] [CrossRef]
- Powell, B.S.; Andrews, G.P.; Enama, J.T.; Jendrek, S.; Bolt, C.; Worsham, P.; Pullen, J.K.; Ribot, W.; Hines, H.; Smith, L.; et al. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol. Prog. 2005, 21, 1490–1510. [Google Scholar] [CrossRef]
- Williamson, E.D.; Oyston, P.C. Protecting against plague: Towards a next-generation vaccine. Clin. Exp. Immunol. 2013, 172, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pitt, L.M. Non-human primates as a model for pneumonic plague: Animal models and correlates of protection for plague. In Proceedings of the Plague Vaccines Workshop, Gaithersburg, MD, USA, 13 October 2004. [Google Scholar]
- Adamovicz, J.J.; Worsham, P.L. Laboratory Animal Models of Plague; CRC Press: Boca Raton, FL, USA, 2012; pp. 113–145. [Google Scholar]
- Mizel, S.B.; Graff, A.H.; Sriranganathan, N.; Ervin, S.; Lees, C.J.; Lively, M.O.; Hantgan, R.R.; Thomas, M.J.; Wood, J.; Bell, B. Flagellin-F1-V fusion protein is an effective plague vaccine in mice and two species of nonhuman primates. Clin. Vaccine Immunol. 2009, 16, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Quenee, L.E.; Ciletti, N.A.; Elli, D.; Hermanas, T.M.; Schneewind, O. Prevention of pneumonic plague in mice, rats, guinea pigs and non-human primates with clinical grade rV10, rV10-2 or F1-V vaccines. Vaccine 2011, 29, 6572–6583. [Google Scholar] [CrossRef] [PubMed]
- Anisimov, A.P.; Dentovskaya, S.V.; Panfertsev, E.A.; Svetoch, T.E.; Kopylov, P.; Segelke, B.W.; Zemla, A.; Telepnev, M.V.; Motin, V.L. Amino acid and structural variability of Yersinia pestis LcrV protein. Infect. Genet. Evol. 2010, 10, 137–145. [Google Scholar] [CrossRef]
- Miller, N.C.; Quenee, L.E.; Elli, D.; Ciletti, N.A.; Schneewind, O. Polymorphisms in the lcrv gene of Yersinia enterocolitica and their effect on plague protective immunity. Infect. Immun. 2012, 80, 1572–1582. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roggenkamp, A.; Geiger, A.M.; Leitritz, L.; Kessler, A.; Heesemann, J. Passive immunity to infection with Yersinia spp. mediated by anti-recombinant V antigen is dependent on polymorphism of V antigen. Infect. Immun. 1997, 65, 446–451. [Google Scholar] [CrossRef]
- Daniel, C.; Dewitte, A.; Poiret, S.; Marceau, M.; Simonet, M.; Marceau, L.; Descombes, G.; Boutillier, D.; Bennaceur, N.; Bontemps-Gallo, S.; et al. Polymorphism in the Yersinia LcrV antigen enables immune escape from the protection conferred by an LcrV-secreting Lactococcus lactis in a pseudotuberculosis mouse model. Front. Immunol. 2019, 10, 1830. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Motin, V.L. Plague vaccines: Current developments and future perspectives. Emerg. Microbes Infect. 2012, 1, e36. [Google Scholar] [CrossRef]
- Stepanov, A.V.; Marinin, L.I.; Vorob’ev, A.A. Aerosol vaccination against dangerous infectious diseases. Vestn. Ross. Akad. Med. Nauk 1999, 8, 47–54. [Google Scholar]
- Smiley, S.T. Current challenges in the development of vaccines for pneumonic plague. Expert Rev. Vaccines 2008, 7, 209–221. [Google Scholar] [CrossRef]
- Elvin, S.J.; Williamson, E.D. Stat 4 but not stat 6 mediated immune mechanisms are essential in protection against plague. Microb. Pathog. 2004, 37, 177–184. [Google Scholar] [CrossRef]
- Kummer, L.W.; Szaba, F.M.; Parent, M.A.; Adamovicz, J.J.; Hill, J.; Johnson, L.L.; Smiley, S.T. Antibodies and cytokines independently protect against pneumonic plague. Vaccine 2008, 26, 6901–6907. [Google Scholar] [CrossRef]
- Achtman, M.; Morelli, G.; Zhu, P.; Wirth, T.; Diehl, I.; Kusecek, B.; Vogler, A.J.; Wagner, D.M.; Allender, C.J.; Easterday, W.R.; et al. Microevolution and history of the plague bacillus, Yersinia pestis. Proc. Natl. Acad. Sci. USA 2004, 101, 17837–17842. [Google Scholar] [CrossRef]
- Lin, J.S.; Kummer, L.W.; Szaba, F.M.; Smiley, S.T. IL-17 contributes to cell-mediated defense against pulmonary Yersinia pestis infection. J. Immunol. 2011, 186, 1675–1684. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.S.; Park, S.; Adamovicz, J.J.; Hill, J.; Bliska, J.B.; Cote, C.K.; Perlin, D.S.; Amemiya, K.; Smiley, S.T. TNFα and IFNγ contribute to F1/LcrV-targeted immune defense in mouse models of fully virulent pneumonic plague. Vaccine 2010, 29, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Bozue, J.; Cote, C.K.; Webster, W.; Bassett, A.; Tobery, S.; Little, S.; Swietnicki, W. A Yersinia pestis YscN atpase mutant functions as a live attenuated vaccine against bubonic plague in mice. FEMS Microbiol. Lett. 2012, 332, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.F.; Smith, G.; Foster, L.; Brookman, M.; Sung, M. Live, attenuated Yersinia pestis vaccine: Virulent in nonhuman primates, harmless to guinea pigs. J. Infect. Dis. 1974, 129, S85–S120. [Google Scholar] [CrossRef]
- Welkos, S.; Pitt, M.L.; Martinez, M.; Friedlander, A.; Vogel, P.; Tammariello, R. Determination of the virulence of the pigmentation-deficient and pigmentation-/plasminogen activator-deficient strains of Yersinia pestis in non-human primate and mouse models of pneumonic plague. Vaccine 2002, 20, 2206–2214. [Google Scholar] [CrossRef]
- Jia, Q.; Bowen, R.; Dillon, B.J.; Maslesa-Galic, S.; Chang, B.T.; Kaidi, A.C.; Horwitz, M.A. Single vector platform vaccine protects against lethal respiratory challenge with tier 1 select agents of anthrax, plague, and tularemia. Sci. Rep. 2018, 8, 7009. [Google Scholar] [CrossRef]
- Derbise, A.; Guillas, C.; Gerke, C.; Carniel, E.; Pizarro-Cerda, J.; Demeure, C.E. Subcutaneous vaccination with a live attenuated Yersinia pseudotuberculosis plague vaccine. Vaccine 2020, 38, 1888–1892. [Google Scholar] [CrossRef]
- Demeure, C.E.; Derbise, A.; Guillas, C.; Gerke, C.; Cauchemez, S.; Carniel, E.; Pizarro-Cerda, J. Humoral and cellular immune correlates of protection against bubonic plague by a live Yersinia pseudotuberculosis vaccine. Vaccine 2019, 37, 123–129. [Google Scholar] [CrossRef]
- Derbise, A.; Hanada, Y.; Khalife, M.; Carniel, E.; Demeure, C.E. Complete protection against pneumonic and bubonic plague after a single oral vaccination. PLoS Negl. Trop. Dis. 2015, 9, e0004162. [Google Scholar] [CrossRef] [PubMed]
- Hinnebusch, B.J.; Chouikha, I.; Sun, Y.C. Ecological opportunity, evolution, and the emergence of flea-borne plague. Infect. Immun. 2016, 84, 1932–1940. [Google Scholar] [CrossRef] [PubMed]
- Bliska, J.B.; Ryndak, M.B.; Grabenstein, J.P. Type III secretion system in Yersinia pestis and Yersinia pseudotuberculosis. In Bacterial genomes and Infectious Diseases; Chan, V.L., Sherman, P.M., Bourke, B., Eds.; Humana Press: Totowa, NJ, USA, 2006. [Google Scholar]
- Donnenberg, M.S.; Kaper, J.B. Construction of an eae deletion mutant of enteropathogenic Escherichia coli by using a positive-selection suicide vector. Infect. Immun. 1991, 59, 4310–4317. [Google Scholar] [CrossRef] [PubMed]
- Bozue, J.; Mou, S.; Moody, K.L.; Cote, C.K.; Trevino, S.; Fritz, D.; Worsham, P. The role of the phoPQ operon in the pathogenesis of the fully virulent CO92 strain of Yersinia pestis and the IP32953 strain of Yersinia pseudotuberculosis. Microb. Pathog. 2011, 50, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Bozue, J.; Cote, C.K.; Chance, T.; Kugelman, J.; Kern, S.J.; Kijek, T.K.; Jenkins, A.; Mou, S.; Moody, K.; Fritz, D.; et al. A Yersinia pestis tat mutant is attenuated in bubonic and small-aerosol pneumonic challenge models of infection but not as attenuated by intranasal challenge. PLoS ONE 2014, 9, e104524. [Google Scholar] [CrossRef]
- Anderson, G.W., Jr.; Leary, S.E.; Williamson, E.D.; Titball, R.W.; Welkos, S.L.; Worsham, P.L.; Friedlander, A.M. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect. Immun. 1996, 64, 4580–4585. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.E.; Cavanaugh, D.C. Measuring the efficacy of vaccination in affording protection against plague. Bull. World Health Organ. 1979, 57, 309–313. [Google Scholar]
- Doll, J.M.; Zeitz, P.S.; Ettestad, P.; Bucholtz, A.L.; Davis, T.; Gage, K. Cat-transmitted fatal pneumonic plague in a person who traveled from colorado to arizona. Am. J. Trop. Med. Hyg. 1994, 51, 109–114. [Google Scholar] [CrossRef]
- Andrews, G.P.; Heath, D.G.; Anderson, G.W., Jr.; Welkos, S.L.; Friedlander, A.M. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect. Immun. 1996, 64, 2180–2187. [Google Scholar] [CrossRef]
- Swietnicki, W.; Carmany, D.; Retford, M.; Guelta, M.; Dorsey, R.; Bozue, J.; Lee, M.S.; Olson, M.A. Identification of small-molecule inhibitors of Yersinia pestis type III secretion system YscN atpase. PLoS ONE 2011, 6, e19716. [Google Scholar] [CrossRef]
- Welkos, S.L.; Friedlander, A.M.; Davis, K.J. Studies on the role of plasminogen activator in systemic infection by virulent Yersinia pestis strain CO92. Microb. Pathog. 1997, 23, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Sikkema, D.J.; Brubaker, R.R. Resistance to pesticin, storage of iron, and invasion of HeLa cells by Yersiniae. Infect. Immun. 1987, 55, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Curtiss, R. Rational considerations about development of live attenuated Yersinia pestis vaccines. Curr. Pharm. Biotechnol. 2013, 14, 878–886. [Google Scholar] [CrossRef]
- Sun, W.; Roland, K.L.; Curtiss, R., III. Developing live vaccines against plague. J. Infect. Dev. Ctries 2011, 5, 614–627. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Six, D.; Kuang, X.; Roland, K.L.; Raetz, C.R.; Curtiss, R., III. A live attenuated strain of Yersinia pestis KIM as a vaccine against plague. Vaccine 2011, 29, 2986–2998. [Google Scholar] [CrossRef]
- Sun, W.; Six, D.A.; Reynolds, C.M.; Chung, H.S.; Raetz, C.R.; Curtiss, R., III. Pathogenicity of Yersinia pestis synthesis of 1-dephosphorylated lipid a. Infect. Immun. 2013, 81, 1172–1185. [Google Scholar] [CrossRef] [PubMed]
- Heine, H.S.; Louie, A.; Sorgel, F.; Bassett, J.; Miller, L.; Sullivan, L.J.; Kinzig-Schippers, M.; Drusano, G.L. Comparison of 2 antibiotics that inhibit protein synthesis for the treatment of infection with Yersinia pestis delivered by aerosol in a mouse model of pneumonic plague. J. Infect. Dis. 2007, 196, 782–787. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Trevino, S.R.; Klimko, C.P.; Reed, M.C.; Aponte-Cuadrado, M.J.; Hunter, M.; Shoe, J.L.; Meyer, J.R.; Dankmeyer, J.L.; Biryukov, S.S.; Quirk, A.V.; et al. Disease progression in mice exposed to low-doses of aerosolized clinical isolates of Burkholderia pseudomallei. PLoS ONE 2018, 13, e0208277. [Google Scholar] [CrossRef]
- Burrows, T.W.; Jackson, S. The virulence-enhancing effect of iron on nonpigmented mutants of virulent strains of Pasturella pestis. Br. J. Exp. Pathol. 1956, 37, 577–583. [Google Scholar]
- Fetherston, J.D.; Schuetze, P.; Perry, R.D. Loss of the pigmentation phenotype in Yersinia pestis is due to the spontaneous deletion of 102 kb of chromosomal DNA which is flanked by a repetitive element. Mol. Microbiol. 1992, 6, 2693–2704. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, A.L.; Worsham, P.L.; Welkos, S.L. A strategy to verify the absence of the pgm locus in Yersinia pestis strain candidates for select agent exemption. J. Microbiol. Methods 2009, 77, 316–319. [Google Scholar] [CrossRef]
- Sodeinde, O.A.; Subrahmanyam, Y.V.; Stark, K.; Quan, T.; Bao, Y.; Goguen, J.D. A surface protease and the invasive character of plague. Science 1992, 258, 1004–1007. [Google Scholar] [CrossRef] [PubMed]
- Darwin, A.J.; Miller, V.L. The psp locus of Yersinia enterocolitica is required for virulence and for growth in vitro when the Ysc type III secretion system is produced. Mol. Microbiol. 2001, 39, 429–444. [Google Scholar] [CrossRef]
- Dworkin, J.; Jovanovic, G.; Model, P. The PspA protein of Escherichia coli is a negative regulator of sigma(54)-dependent transcription. J. Bacteriol. 2000, 182, 311–319. [Google Scholar] [CrossRef]
- Brasiale, V.; Nash, M.; Sinha, N.; Zudina, I.; Motin, V. Correlates of immunity elicited by live Yersinia pestis vaccine. In Frontiers in Research; Georgiev, V., Wester, K., McGowan, J., Eds.; Humana Press: Totawa, NJ, USA, 2009; NIH Volume 1, pp. 473–480. [Google Scholar]
- Qiu, Y.; Liu, Y.; Qi, Z.; Wang, W.; Kou, Z.; Zhang, Q.; Liu, G.; Liu, T.; Yang, Y.; Yang, X.; et al. Comparison of immunological responses of plague vaccines F1+rV270 and EV76 in chinese-origin rhesus macaque, Macaca mulatta. Scand. J. Immunol. 2010, 72, 425–433. [Google Scholar] [CrossRef]
- Quenee, L.E.; Cornelius, C.A.; Ciletti, N.A.; Elli, D.; Schneewind, O. Yersinia pestis caf1 variants and the limits of plague vaccine protection. Infect. Immun. 2008, 76, 2025–2036. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Sanapala, S.; Henderson, J.C.; Sam, S.; Olinzock, J.; Trent, M.S.; Curtiss, R., III. LcrV delivered via type III secretion system of live attenuated Yersinia pseudotuberculosis enhances immunogenicity against pneumonic plague. Infect. Immun. 2014, 82, 4390–4404. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.D.; Eley, S.M.; Griffin, K.F.; Green, M.; Russell, P.; Leary, S.E.; Oyston, P.C.; Easterbrook, T.; Reddin, K.M.; Robinson, A.; et al. A new improved sub-unit vaccine for plague: The basis of protection. FEMS Immunol. Med. Microbiol. 1995, 12, 223–230. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Lyapina, A.M.; Khizhnyakova, M.A.; Zaitsev, S.S.; Saltykov, Y.V.; Motin, V.L. Yersinia pestis antigen F1 but not LcrV induced humoral and cellular immune responses in humans immunized with live plague vaccine-comparison of immunoinformatic and immunological approaches. Vaccines 2020, 8, 698. [Google Scholar] [CrossRef]
- Busch, R.A.; Jonker, M.A.; Pierre, J.F.; Heneghan, A.F.; Kudsk, K.A. Innate mucosal immune system response of BALB/c vs C57BL/6 mice to injury in the setting of enteral and parenteral feeding. J. Parenter. Enteral Nutr. 2016, 40, 256–263. [Google Scholar] [CrossRef]
- Sellers, R.S.; Clifford, C.B.; Treuting, P.M.; Brayton, C. Immunological variation between inbred laboratory mouse strains: Points to consider in phenotyping genetically immunomodified mice. Vet. Pathol. 2012, 49, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Plano, G.V.; Schesser, K. The Yersinia pestis type III secretion system: Expression, assembly and role in the evasion of host defenses. Immunol. Res. 2013, 57, 237–245. [Google Scholar] [CrossRef]
- Cowan, C.; Philipovskiy, A.V.; Wulff-Strobel, C.R.; Ye, Z.; Straley, S.C. Anti-LcrV antibody inhibits delivery of yops by Yersinia pestis KIM5 by directly promoting phagocytosis. Infect. Immun. 2005, 73, 6127–6137. [Google Scholar] [CrossRef]
- Mueller, C.A.; Broz, P.; Muller, S.A.; Ringler, P.; Erne-Brand, F.; Sorg, I.; Kuhn, M.; Engel, A.; Cornelis, G.R. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science 2005, 310, 674–676. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, J.; Holmstrom, A.; Hill, J.; Leary, S.; Frithz-Lindsten, E.; von Euler-Matell, A.; Carlsson, E.; Titball, R.; Forsberg, A.; Wolf-Watz, H. The V-antigen of Yersinia is surface exposed before target cell contact and involved in virulence protein translocation. Mol. Microbiol. 1999, 32, 961–976. [Google Scholar] [CrossRef]
- Philipovskiy, A.V.; Cowan, C.; Wulff-Strobel, C.R.; Burnett, S.H.; Kerschen, E.J.; Cohen, D.A.; Kaplan, A.M.; Straley, S.C. Antibody against V antigen prevents yop-dependent growth of Yersinia pestis. Infect. Immun. 2005, 73, 1532–1542. [Google Scholar] [CrossRef]
- Fetherston, J.D.; Perry, R.D. The pigmentation locus of Yersinia pestis KIM6+ is flanked by an insertion sequence and includes the structural genes for pesticin sensitivity and HMWP2. Mol. Microbiol. 1994, 13, 697–708. [Google Scholar] [CrossRef]
- Lathem, W.W.; Price, P.A.; Miller, V.L.; Goldman, W.E. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science 2007, 315, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Sebbane, F.; Uversky, V.N.; Anisimov, A.P. Yersinia pestis plasminogen activator. Biomolecules 2020, 10, 1554. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Fatal laboratory-acquired infection with an attenuated Yersinia pestis strain—Chicago, Illinois, 2009. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 201–205. [Google Scholar] [PubMed]
- Burrows, T.W.; Jackson, S. The pigmentation of Pasteurella pestis on a defined medium containing haemin. Br. J. Exp. Pathol. 1956, 37, 570–576. [Google Scholar] [PubMed]
- Quenee, L.E.; Hermanas, T.M.; Ciletti, N.; Louvel, H.; Miller, N.C.; Elli, D.; Blaylock, B.; Mitchell, A.; Schroeder, J.; Krausz, T.; et al. Hereditary hemochromatosis restores the virulence of plague vaccine strains. J. Infect. Dis. 2012, 206, 1050–1058. [Google Scholar] [CrossRef]
- Lee-Lewis, H.; Anderson, D.M. Absence of inflammation and pneumonia during infection with nonpigmented Yersinia pestis reveals a new role for the pgm locus in pathogenesis. Infect. Immun. 2010, 78, 220–230. [Google Scholar] [CrossRef]
- Erova, T.E.; Rosenzweig, J.A.; Sha, J.; Suarez, G.; Sierra, J.C.; Kirtley, M.L.; van Lier, C.J.; Telepnev, M.V.; Motin, V.L.; Chopra, A.K. Evaluation of protective potential of Yersinia pestis outer membrane protein antigens as possible candidates for a new-generation recombinant plague vaccine. Clin. Vaccine Immunol. 2013, 20, 227–238. [Google Scholar] [CrossRef]
- Feodorova, V.A.; Lyapina, A.M.; Khizhnyakova, M.A.; Zaitsev, S.S.; Sayapina, L.V.; Arseneva, T.E.; Trukhachev, A.L.; Lebedeva, S.A.; Telepnev, M.V.; Ulianova, O.V.; et al. Humoral and cellular immune responses to Yersinia pestis Pla antigen in humans immunized with live plague vaccine. PLoS Negl. Trop. Dis. 2018, 12, e0006511. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.D.; Oyston, P.C.F. The natural history and incidence of Yersinia pestis and prospects for vaccination. J. Med. Microbiol. 2012, 61, 911–918. [Google Scholar] [CrossRef]
- Buchrieser, C.; Rusniok, C.; Frangeul, L.; Couve, E.; Billault, A.; Kunst, F.; Carniel, E.; Glaser, P. The 102-kilobase pgm locus of Yersinia pestis: Sequence analysis and comparison of selected regions among different Yersinia pestis and Yersinia pseudotuberculosis strains. Infect. Immun. 1999, 67, 4851–4861. [Google Scholar] [CrossRef]
- Perry, R.D.; Fetherston, J.D. Yersinia pestis—Etiologic agent of plague. Clin. Microbiol. Rev. 1997, 10, 35–66. [Google Scholar] [CrossRef]
- Robinson, V.L.; Oyston, P.C.; Titball, R.W. A dam mutant of Yersinia pestis is attenuated and induces protection against plague. FEMS Microbiol. Lett. 2005, 252, 251–256. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taylor, V.L.; Titball, R.W.; Oyston, P.C. Oral immunization with a dam mutant of Yersinia pseudotuberculosis protects against plague. Microbiology 2005, 151, 1919–1926. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cornelius, C.A.; Quenee, L.E.; Overheim, K.A.; Koster, F.; Brasel, T.L.; Elli, D.; Ciletti, N.A.; Schneewind, O. Immunization with recombinant V10 protects cynomolgus macaques from lethal pneumonic plague. Infect. Immun. 2008, 76, 5588–5597. [Google Scholar] [CrossRef]
- Hill, J.; Leary, S.E.; Griffin, K.F.; Williamson, E.D.; Titball, R.W. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect. Immun. 1997, 65, 4476–4482. [Google Scholar] [CrossRef]
- Leary, S.E.; Eley, S.M.; Williamson, E.D.; Titball, R.W. Expression of Yersinia pestis V antigen in attenuated Salmonella typhimurium: Development of a novel vaccine for plague. Contrib. Microbiol. Immunol. 1995, 13, 216–217. [Google Scholar] [PubMed]
- Leary, S.E.; Williamson, E.D.; Griffin, K.F.; Russell, P.; Eley, S.M.; Titball, R.W. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect. Immun. 1995, 63, 2854–2858. [Google Scholar] [CrossRef]
- Motin, V.L.; Nakajima, R.; Smirnov, G.B.; Brubaker, R.R. Passive immunity to Yersiniae mediated by anti-recombinant V antigen and protein A-V antigen fusion peptide. Infect. Immun. 1994, 62, 4192–4201. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Singh, A.K.; Sun, W. Protection and safety evaluation of live constructions derived from the Pgm(-) and pPCP1(-) Yersinia pestis strain. Vaccines 2020, 8, 95. [Google Scholar] [CrossRef]
- Bonecchi, R.; Bianchi, G.; Bordignon, P.P.; D’Ambrosio, D.; Lang, R.; Borsatti, A.; Sozzani, S.; Allavena, P.; Gray, P.A.; Mantovani, A.; et al. Differential expression of chemokine receptors and chemotactic responsiveness of type 1 T helper cells (Th1s) and Th2s. J. Exp. Med. 1998, 187, 129–134. [Google Scholar] [CrossRef]
- Muller, K.; Bischof, S.; Sommer, F.; Lohoff, M.; Solbach, W.; Laskay, T. Differential production of macrophage inflammatory protein 1gamma (MIP-1gamma), lymphotactin, and MIP-2 by CD4(+) Th subsets polarized in vitro and in vivo. Infect. Immun. 2003, 71, 6178–6183. [Google Scholar] [CrossRef]
- Shang, X.Z.; Chiu, B.C.; Stolberg, V.; Lukacs, N.W.; Kunkel, S.L.; Murphy, H.S.; Chensue, S.W. Eosinophil recruitment in type-2 hypersensitivity pulmonary granulomas: Source and contribution of monocyte chemotactic protein-3 (CCL7). Am. J. Pathol. 2002, 161, 257–266. [Google Scholar] [CrossRef]
- Aujla, S.J.; Dubin, P.J.; Kolls, J.K. Th17 cells and mucosal host defense. Semin. Immunol. 2007, 19, 377–382. [Google Scholar] [CrossRef]
- Derbise, A.; Marin, A.C.; Ave, P.; Blisnick, T.; Huerre, M.; Carniel, E.; Demeure, C.E. An encapsulated Yersinia pseudotuberculosis is a highly efficient vaccine against pneumonic plague. PLoS Negl. Trop. Dis. 2012, 6, e1528. [Google Scholar] [CrossRef] [PubMed]
- Eyerich, K.; Dimartino, V.; Cavani, A. IL-17 and IL-22 in immunity: Driving protection and pathology. Eur. J. Immunol. 2017, 47, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.C.; Long, A.J.; Bennett, F.; Whitters, M.J.; Karim, R.; Collins, M.; Goldman, S.J.; Dunussi-Joannopoulos, K.; Williams, C.M.; Wright, J.F.; et al. An IL-17F/A heterodimer protein is produced by mouse Th17 cells and induces airway neutrophil recruitment. J. Immunol. 2007, 179, 7791–7799. [Google Scholar] [CrossRef]
- Liang, S.C.; Tan, X.Y.; Luxenberg, D.P.; Karim, R.; Dunussi-Joannopoulos, K.; Collins, M.; Fouser, L.A. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J. Exp. Med. 2006, 203, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Halstead, E.S.; Umstead, T.M.; Davies, M.L.; Kawasawa, Y.I.; Silveyra, P.; Howyrlak, J.; Yang, L.; Guo, W.; Hu, S.; Hewage, E.K.; et al. GM-CSF overexpression after influenza a virus infection prevents mortality and moderates M1-like airway monocyte/macrophage polarization. Respir. Res. 2018, 19, 3. [Google Scholar] [CrossRef]
- Fontenot, J.D.; Rasmussen, J.P.; Gavin, M.A.; Rudensky, A.Y. A function for interleukin 2 in foxp3-expressing regulatory T cells. Nat. Immunol. 2005, 6, 1142–1151. [Google Scholar] [CrossRef]
- Mostbock, S.; Lutsiak, M.E.; Milenic, D.E.; Baidoo, K.; Schlom, J.; Sabzevari, H. IL-2/anti-IL-2 antibody complex enhances vaccine-mediated antigen-specific CD8+ T cell responses and increases the ratio of effector/memory CD8+ T cells to regulatory T cells. J. Immunol. 2008, 180, 5118–5129. [Google Scholar] [CrossRef] [PubMed]
- Ebner, S.; Hofer, S.; Nguyen, V.A.; Furhapter, C.; Herold, M.; Fritsch, P.; Heufler, C.; Romani, N. A novel role for IL-3: Human monocytes cultured in the presence of IL-3 and IL-4 differentiate into dendritic cells that produce less IL-12 and shift Th cell responses toward a Th2 cytokine pattern. J. Immunol. 2002, 168, 6199–6207. [Google Scholar] [CrossRef]
- Herbert, D.R.; Douglas, B.; Zullo, K. Group 2 innate lymphoid cells (ILC2): Type 2 immunity and helminth immunity. Int. J. Mol. Sci. 2019, 20, 2276. [Google Scholar] [CrossRef] [PubMed]
- Steenwinckel, V.; Louahed, J.; Lemaire, M.M.; Sommereyns, C.; Warnier, G.; McKenzie, A.; Brombacher, F.; van Snick, J.; Renauld, J.C. IL-9 promotes IL-13-dependent paneth cell hyperplasia and up-regulation of innate immunity mediators in intestinal mucosa. J. Immunol. 2009, 182, 4737–4743. [Google Scholar] [CrossRef]
- Allard, J.B.; Rinaldi, L.; Wargo, M.J.; Allen, G.; Akira, S.; Uematsu, S.; Poynter, M.E.; Hogan, D.A.; Rincon, M.; Whittaker, L.A. Th2 allergic immune response to inhaled fungal antigens is modulated by TLR-4-independent bacterial products. Eur. J. Immunol. 2009, 39, 776–788. [Google Scholar] [CrossRef]
- Hartl, D.; Griese, M.; Kappler, M.; Zissel, G.; Reinhardt, D.; Rebhan, C.; Schendel, D.J.; Krauss-Etschmann, S. Pulmonary T(h)2 response in Pseudomonas aeruginosa-infected patients with cystic fibrosis. J. Allergy Clin. Immunol. 2006, 117, 204–211. [Google Scholar] [CrossRef]
- Kolls, J.K. Th17 cells in mucosal immunity and tissue inflammation. Semin. Immunopathol. 2010, 32, 1–2. [Google Scholar] [CrossRef]
- Kolls, J.K.; Khader, S.A. The role of Th17 cytokines in primary mucosal immunity. Cytokine Growth Factor Rev. 2010, 21, 443–448. [Google Scholar] [CrossRef]
- Nair, V.R.; Franco, L.H.; Zacharia, V.M.; Khan, H.S.; Stamm, C.E.; You, W.; Marciano, D.K.; Yagita, H.; Levine, B.; Shiloh, M.U. Microfold cells actively translocate Mycobacterium tuberculosis to initiate infection. Cell Rep. 2016, 16, 1253–1258. [Google Scholar] [CrossRef]
- Teitelbaum, R.; Schubert, W.; Gunther, L.; Kress, Y.; Macaluso, F.; Pollard, J.W.; McMurray, D.N.; Bloom, B.R. The M cell as a portal of entry to the lung for the bacterial pathogen Mycobacterium tuberculosis. Immunity 1999, 10, 641–650. [Google Scholar] [CrossRef]
- Eichelberger, K.R.; Goldman, W.E. Human neutrophil isolation and degranulation responses to Yersinia pestis infection. Methods Mol. Biol. 2019, 2010, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Eichelberger, K.R.; Jones, G.S.; Goldman, W.E. Inhibition of neutrophil primary granule release during Yersinia pestis pulmonary infection. mBio 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Grommes, J.; Soehnlein, O. Contribution of neutrophils to acute lung injury. Mol. Med. 2011, 17, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Jilg, W.; Schmidt, M.; Deinhardt, F. Vaccination against hepatitis b: Comparison of three different vaccination schedules. J. Infect. Dis. 1989, 160, 766–769. [Google Scholar] [CrossRef]
- Meites, E.; Kempe, A.; Markowitz, L.E. Use of a 2-dose schedule for human papillomavirus vaccination-updated recommendations of the advisory committee on immunization practices. Morb. Mortal. Wkly. Rep. 2016, 65, 1405–1408. [Google Scholar] [CrossRef]
- Cirelli, K.M.; Crotty, S. Germinal center enhancement by extended antigen availability. Curr. Opin. Immunol. 2017, 47, 64–69. [Google Scholar] [CrossRef]
- Slifka, M.K.; Amanna, I.J. Role of multivalency and antigenic threshold in generating protective antibody responses. Front. Immunol. 2019, 10, 956. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhao, Q.; Zhang, D.; Sun, C.; Bao, C.; Yi, M.; Xing, L.; Luo, D. Essential roles for platelets during neutrophil-dependent or lymphocyte-mediated defense against bacterial pathogens. Blood Coagul. Fibrinolysis 2016, 27, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Moore, T.A.; Newstead, M.W.; Hernandez-Alcoceba, R.; Tsai, W.C.; Standiford, T.J. Intrapulmonary expression of macrophage inflammatory protein 1alpha (CCL3) induces neutrophil and nk cell accumulation and stimulates innate immunity in murine bacterial pneumonia. Infect. Immun. 2003, 71, 1306–1315. [Google Scholar] [CrossRef] [PubMed]
- Aust, V.; Kress, E.; Abraham, S.; Schroder, N.; Kipp, M.; Stope, M.B.; Pufe, T.; Tauber, S.C.; Brandenburg, L.O. Lack of chemokine (c-c motif) ligand 3 leads to decreased survival and reduced immune response after bacterial meningitis. Cytokine 2018, 111, 246–254. [Google Scholar] [CrossRef]
- Tekamp-Olson, P.; Gallegos, C.; Bauer, D.; McClain, J.; Sherry, B.; Fabre, M.; van Deventer, S.; Cerami, A. Cloning and characterization of cDNAs for murine macrophage inflammatory protein 2 and its human homologues. J. Exp. Med. 1990, 172, 911–919. [Google Scholar] [CrossRef]
- Eisele, N.A.; Lee-Lewis, H.; Besch-Williford, C.; Brown, C.R.; Anderson, D.M. Chemokine receptor CXCR2 mediates bacterial clearance rather than neutrophil recruitment in a murine model of pneumonic plague. Am. J. Pathol. 2011, 178, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, R.S.; Nicholson, D.W. Apoptosis and caspases regulate death and inflammation in sepsis. Nat. Rev. Immunol. 2006, 6, 813–822. [Google Scholar] [CrossRef]
- Crawford, M.A.; Zhu, Y.; Green, C.S.; Burdick, M.D.; Sanz, P.; Alem, F.; O’Brien, A.D.; Mehrad, B.; Strieter, R.M.; Hughes, M.A. Antimicrobial effects of interferon-inducible CXC chemokines against Bacillus anthracis spores and bacilli. Infect. Immun. 2009, 77, 1664–1678. [Google Scholar] [CrossRef]
- Margulieux, K.R.; Fox, J.W.; Nakamoto, R.K.; Hughes, M.A. CXCL10 acts as a bifunctional antimicrobial molecule against Bacillus anthracis. mBio 2016, 7. [Google Scholar] [CrossRef]
- Levy, Y.; Vagima, Y.; Tidhar, A.; Aftalion, M.; Gur, D.; Nili, U.; Chitlaru, T.; Zauberman, A.; Mamroud, E. Targeting of the Yersinia pestis F1 capsular antigen by innate-like B1b cells mediates a rapid protective response against bubonic plague. NPJ Vaccines 2018, 3, 52. [Google Scholar] [CrossRef]
- Li, B.; Du, C.; Zhou, L.; Bi, Y.; Wang, X.; Wen, L.; Guo, Z.; Song, Z.; Yang, R. Humoral and cellular immune responses to Yersinia pestis infection in long-term recovered plague patients. Clin. Vaccine Immunol. 2012, 19, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Gupta, G.; Khan, A.A.; Rao, D.N. Cell-mediated immune response and Th/Th cytokine profile of B-T constructs of F1 and V antigen of Yersinia pestis. Scand. J. Immunol. 2010, 71, 186–198. [Google Scholar] [CrossRef] [PubMed]
- Szaba, F.M.; Kummer, L.W.; Duso, D.K.; Koroleva, E.P.; Tumanov, A.V.; Cooper, A.M.; Bliska, J.B.; Smiley, S.T.; Lin, J.S. Tnfα and IFNγ but not perforin are critical for CD8 T cell-mediated protection against pulmonary Yersinia pestis infection. PLoS Pathog. 2014, 10, e1004142. [Google Scholar] [CrossRef] [PubMed]
- Culbreth, M.J.; Biryukov, S.S.; Shoe, J.L.; Dankmeyer, J.L.; Hunter, M.; Klimko, C.P.; Rosario-Acevedo, R.; Fetterer, D.P.; Moreau, A.M.; Welkos, S.L.; et al. The use of analgesics during vaccination with a live attenuated Yersinia pestis vaccine alters the resulting immune response in mice. Vaccines 2019, 7, 205. [Google Scholar] [CrossRef]
- Li, B.; Zhou, L.; Guo, J.; Wang, X.; Ni, B.; Ke, Y.; Zhu, Z.; Guo, Z.; Yang, R. High-throughput identification of new protective antigens from a Yersinia pestis live vaccine by enzyme-linked immunospot assay. Infect. Immun. 2009, 77, 4356–4361. [Google Scholar] [CrossRef]
- Zvi, A.; Rotem, S.; Zauberman, A.; Elia, U.; Aftalion, M.; Bar-Haim, E.; Mamroud, E.; Cohen, O. Novel CTL epitopes identified through a Y. pestis proteome-wide analysis in the search for vaccine candidates against plague. Vaccine 2017, 35, 5995–6006. [Google Scholar] [CrossRef] [PubMed]
| pspC Primers for Mutant Construction and Screening | |
|---|---|
| pspCI-XhoI | CCGCTCGAGGGAACCCGCTTAACACCCAGTAG |
| pcpCI-BamHI | CGGGATCCCAGTTTGAACGCCGTATTGACCAT |
| pspCI-lower-del | GTAGTTTTGTAGAAAATTCAACCG |
| pspCI-upper-del | TTATGACTGTCTCCAGTTAGGGTG |
| pspCII-lower-del | CATTATGACTGTCTCCAGTTAGGGTG |
| pcpCII-upper-del | TAGTTTTGTAGAAAATTCAACCG |
| pspA Primers for Mutant Construction and Screening | |
| clone pspA 3′ | CGGCAGGGATTAAACAGAGAAAAC |
| clone pspA 5′ | AACGCGGGCAGATTATCATTGGTG |
| delete pspA 3′ | TAGTTAATTTTCCGTATTTATTAG |
| delete pspA 5′ | CATAATTTACGTCCCCTTTGACT |
| screen pspA 3′ | GCGCGTGTAGGGGCAGGATT |
| screen pspA 5′ | ATAAACCGAACGCTCTACCACATTT |
| Screening for pCD1 | |
| lcrV-1 | AGGGTGGAACAACTTACTG |
| lcrV-2 | GTGCCACTACTAGACAGATGC |
| Screening for pMT | |
| Ymt-5′ | TTTCGGCCAATCTCCAACAGTA |
| Ymt-3′ | TCCGACCGCCCACATCA |
| CapAG-5′ | AAAAATCAGTTCCGTTATCG |
| CapAG-3′ | CTGCCCGTAGCCAAGAC |
| Screening for pPst | |
| Pla-5′ | TGGCTTCCGGGTCAGGTA |
| Pla-3′ | AGCCGGATGTCTTCTCACG |
| Y. pestis | LD50 by Route (no. CFU) a | ||||
|---|---|---|---|---|---|
| Strain b | Characteristics c | SC | Aerosol | Intranasal | References d |
| CO92 | wild type | 1−2 × 100 f | 6.8 × 104 f | 1.4 × 103 f | 41, 50 |
| CO92 pgm- pPst- | pgm- (102 kb deleted by serial passage on congo red agar), pPst- (cured by serial passage on agar 4 °C) | >1.0 × 108 f | nd e | nd | 6, 42, 54 |
| CO92 ∆tatA | in frame deletion of tatA | 1.5 × 107 | >9.4 × 105 | 2.4 × 103 | 38 |
| CO92 ∆yscN | in frame deletion of yscN | >3.2 × 107 | nd | nd | 27, 43 |
| CO92 ∆pspA | in frame deletion of pspA | 6 × 102 | >1.0 × 106 | nd | Current study |
| CO92 ∆pspCI | out of frame (potentially polar) deletion of pspC | >2.1 × 105 | >4.5 × 106 | nd | Current study |
| CO92 ∆pcpCII | in frame deletion of pcpC | 3.1 × 103 | >1.9 × 106 | nd | Current study |
| C12 | F1- CO92; site directed mutagenesis of caf1A | 9 × 100 f | 7.7 × 104 f | nd | 7 |
| C12 ∆yscN | in frame deletion of yscN, caf1A | >2.0 × 107 f | nd | nd | Current study |
| KIM6+ | wild type | <1.0 × 101 | nd | ~1.0 × 102 | 45 |
| KIM6+ χ10030/ pCD1Ap1 | lpxL, crp (See references) | >1.0 × 108 | nd | >1.0 × 106 | 46–48 |
| Vaccine | Challenge | ||||
|---|---|---|---|---|---|
| Strain a | Dose (no. CFU) b | No. mice c | Survival (%) d | Route e | Survival (%) |
| KIM 6+ χ10030/pCD1Ap f | 4.6 × 106 | 10 | 0 | SC | nd g |
| 7.2 × 105 | 20 | 35 | SC | nd | |
| CO92 pgm-pPst- | 6.2 × 106 | 10 | 100 | SC | 100 |
| CO92 ∆yscN | 7.2 × 106 | 10 | 100 | SC | 100 |
| C12 ∆yscN | 1.7 × 107 | 10 | 100 | SC | 30 |
| CO92 mutants g | 0.5–1.2 × 107 | 10 | 0 | nd | nd |
| Kphos | NA | 10 | 100 | SC | 0 |
| CO92 pgm-pPst- | 7.6 × 106 | 10 | 100 | AERO | 100 |
| CO92 ∆yscN | 1.0 × 107 | 10 | 90 | AERO | 100 |
| C12 ∆yscN | 1.7 × 107 | 10 | 100 | AERO | 0 |
| Kphos | NA | 10 | 100 | AERO | 0 |
| Vaccine | Challenge | ||||
|---|---|---|---|---|---|
| Strain a | Dose (no. CFU) b | No. Mice c | Survival (%) d | Route e | Survival (%) e |
| CO92 pgm-pPst- | 8.2 × 106 | 10 | 100 | SC | 100 |
| CO92 ∆yscN | 9.4 × 106 | 10 | 100 | SC | 100 |
| Kphos | NA | 10 | 100 | SC | 30 |
| CO92 pgm-pPst- | 7.6 × 106 | 10 | 100 | AERO | 60 |
| CO92 ∆yscN | 1.0 × 107 | 10 | 100 | AERO | 20 |
| Kphos | NA | 10 | 100 | AERO | 0 |
| IgG c | |||
|---|---|---|---|
| Vaccine a,b | Capture Antigen | Geo Mean | (GSE) |
| Kphos a* | CO92 | 50 | (1.08) |
| C12 | 50 | (1.08) | |
| F1-V | 50 | (1.08) | |
| CO92 pgm-pPst- | CO92 | 5572 | (1.45) |
| C12 | 3592 | (1.51) | |
| F1-V | 160,000 | (1.16) | |
| CO92 ΔyscN | CO92 | 348 | (1.38) |
| C12 | 470 | (1.41) | |
| F1-V | 89,797 | (1.24) | |
| C12 ΔyscN a** | CO92 | 1819 | (1.53) |
| C12 | 2604 | (1.79) | |
| F1-V | 61 | (1.17) | |
| CO92 ΔyscN + C12 ΔyscN | CO92 | 1008 | (1.68) |
| C12 | 1158 | (1.67) | |
| F1-V | 40,317 | (1.71) | |
| Vaccine Dose (no. CFU) b | Challenge c | |||||
|---|---|---|---|---|---|---|
| Strain a | 1st | 2nd | No. Mice | Survival (%) | Route | Survival (%) |
| CO92 ∆yscN × 2 d | 1.03 × 107 | 0.85 × 107 | 10 | 100 | SC | 100 |
| C12 ∆yscN × 2 | 1.27 × 107 | 0.93 × 107 | 10 | 100 | SC | 40 |
| Combo × 2 | 0.95 × 107 | 0.93 × 107 | 10 | 100 | SC | 100 |
| CO92 ∆yscN | NA | 0.85 × 107 | 10 | 100 | SC | 100 |
| C12 ∆yscN | NA | 0.93 × 107 | 10 | 100 | SC | 30 |
| Combo | NA | 0.93 × 107 | 10 | 100 | SC | 90 |
| Kphos | NA | NA | 10 | 100 | SC | 0 |
| CO92 ∆yscN × 2 | 1.03 × 107 | 0.85 × 107 | 10 | 100 | AERO | 100 |
| C12 ∆yscN × 2 | 1.27 × 107 | 0.93 × 107 | 10 | 100 | AERO | 0 |
| Combo × 2 | 0.95 × 107 | 0.93 × 107 | 10 | 100 | AERO | 90 |
| Kphos | NA | NA | 10 | 100 | AERO | 0 |
| IgG a | |||
|---|---|---|---|
| Vaccine b,c | Capture Antigen | Geo Mean (GSE) | |
| Kphos | F1 | 50 | (1) |
| V | 50 | (1) | |
| CO92 pgm-pPst- | F1 | 312,691 | (1.18) |
| V | 235 | (1.42) | |
| CO92 ΔyscN | F1 | 23,829 | (1.40) |
| V | 51 | (1.04) | |
| C12 ΔyscN b* | F1 | 50 | (1) |
| V | 50 | (1) | |
| CO92 ΔyscN + C12 ΔyscN | F1 | 6400 | (1.45) |
| V | 50 | (1) | |
| CO92 pgm- pPst- ×2 b** | F1 | 926,252 | (1.17) |
| V | 729 | (2.22) | |
| CO92 ΔyscN × 2 | F1 | 113,137 | (1.27) |
| V | 120 | (1.32) | |
| C12 ΔyscN × 2 b* | F1 | 50 | (1) |
| V | 59 | (1.12) | |
| CO92 ΔyscN + C12 ΔyscN × 2 | F1 | 118,488 | (1.27) |
| V | 71 | (1.13) | |
| Vaccine b,c | Capture Antigen | IgG a | IgG1 a | IgG2a a | Ratio IgG2a/IgG1 | |||
|---|---|---|---|---|---|---|---|---|
| Geo Mean (GSE) | Geo Mean (GSE) | Geo Mean (GSE) | ||||||
| Kphos | CO92 | 50 | (1) | 50 | (1) | 50 | (1) | |
| C12 | 50 | (1) | 50 | (1) | 50 | (1) | ||
| CO92 pgm-pPst- | CO92 | 5572 | (1.45) | 9902 | (1.54) b,* | 312 | (1.68) b,* | 0.03 |
| C12 | 3592 | (1.51) | 16,977 | (1.40) b,* | 352 | (1.54) * | 0.02 | |
| CO92 ΔyscN | CO92 | 746 | (1.68) | 1213 | (1.82) | 118 | (1.54) | 0.10 |
| C12 | 650 | (1.64) | 1477 | (1.77) | 132 | (1.59) | 0.09 | |
| C12 ΔyscN | CO92 | 504 | (1.68) | 1241 | (1.78) | 83 | (1.34) | 0.07 |
| C12 | 540 | (1.77) | 1080 | (1.69) | 107 | (1.42) | 0.10 | |
| CO92 ΔyscN + C12 ΔyscN | CO92 | 276 | (1.62) | 696 | (1.56) | 89 | (1.35) | 0.13 |
| C12 | 449 | (1.62) | 504 | (1.38) | 98 | (1.37) | 0.19 | |
| CO92 pgm-pPst- ×2 b,** | CO92 | 320,000 | (1.21) | 485,029 | (1.19) | 12,222 | (1.37) | 0.03 |
| C12 | 320,000 | (1.26) | 884,424 | (1.54) | 16,127 | (1.21) | 0.02 | |
| CO92 ΔyscN ×2 | CO92 | 19,097 | (1.25) | 61,110 | (1.28) | 2202 | (1.97) | 0.04 |
| C12 | 19,543 | (1.32) | 44,221 | (1.33) | 2416 | (1.91) | 0.05 | |
| C12 ΔyscN ×2 b,* | CO92 | 37,998 | (1.41) | 45,920 | (1.96) | 1553 | (2.22) | 0.03 |
| C12 | 22,202 | (1.46) | 36,378 | (2.11) | 1142 | (2.05) | 0.03 | |
| CO92 ΔyscN + C12 ΔyscN ×2 | CO92 | 27,007 | (1.33) | 97,006 | (1.33) | 1711 | (1.90) | 0.02 |
| C12 | 29,622 | (1.26) | 122,204 | (1.43) | 2106 | (1.70) | 0.02 | |
| Vaccine b,c | Capture Antigen (Temp. Shift) | IgG a | IgG1 a | IgG2a a | Ratio IgG2a/IgG1 | |||
|---|---|---|---|---|---|---|---|---|
| Geo Mean (GSE) | Geo Mean (GSE) | Geo Mean (GSE) | ||||||
| Kphos | CO92 | 51 | (1) | 50 | (1) | 50 | (1) | |
| C12 | 54 | (1) | 50 | (1) | 50 | (1) | ||
| CO92 pgm-pPst- | CO92 | 42,559 | (1.23) | 144,009 | (1.19) | 1754 | (1.36) | 0.01 |
| C12 | 9,263 | (1.34) | 23,886 | (1.33) | 558 | (1.38) b* | 0.02 | |
| CO92 ΔyscN | CO92 | 17,688 | (1.28) | 20,319 | (1.36) | 1213 | (1.52) | 0.06 |
| C12 | 1,459 | (1.67) | 1925 | (1.70) | 235 | (1.62) | 0.12 | |
| C12 ΔyscN b,* | CO92 | 933 | (1.83) | 1034 | (1.77) | 205 | (1.67) | 0.20 |
| C12 | 864 | (1.80) | 1444 | (1.89) | 143 | (1.50) | 0.10 | |
| CO92 ΔyscN + C12 ΔyscN | CO92 | 8844 | (1.48) | 12,498 | (1.64) | 439 | (1.82) | 0.04 |
| C12 | 579 | (1.58) | 566 | (1.71) | 219 | (1.57) | 0.39 d | |
| CO92 pgm-pPst- ×2 b,** | CO92 | 403,175 | (1.21) | 583,502 | (1.37) | 20,319 | (1.34) | 0.03 |
| C12 | 115,782 | (1.27) | 305,549 | (1.43) | 3850 | (1.58) | 0.01 | |
| CO92 ΔyscN ×2 | CO92 | 44,221 | (1.24) | 116,700 | (1.18) | 11,633 | (1.47) | 0.10 |
| C12 | 32,748 | (1.33) | 34,324 | (1.47) | 2154 | (1.87) | 0.06 | |
| C12 ΔyscN ×2 b,* | CO92 | 52,072 | (2.06) | 106,315 | (1.58) | 3813 | (2.04) | 0.04 |
| C12 | 27,284 | (1.92) | 23,557 | (1.73) | 1367 | (2.23) | 0.06 | |
| CO92 ΔyscN + C12 ΔyscN ×2 | CO92 | 113,945 | (1.44) | 272,860 | (1.33) | 8412 | (2.08) | 0.03 |
| C12 | 80,508 | (1.43) | 34,243 | (1.4) | 1452 | (2.32) | 0.04 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cote, C.K.; Biryukov, S.S.; Klimko, C.P.; Shoe, J.L.; Hunter, M.; Rosario-Acevedo, R.; Fetterer, D.P.; Moody, K.L.; Meyer, J.R.; Rill, N.O.; et al. Protection Elicited by Attenuated Live Yersinia pestis Vaccine Strains against Lethal Infection with Virulent Y. pestis. Vaccines 2021, 9, 161. https://doi.org/10.3390/vaccines9020161
Cote CK, Biryukov SS, Klimko CP, Shoe JL, Hunter M, Rosario-Acevedo R, Fetterer DP, Moody KL, Meyer JR, Rill NO, et al. Protection Elicited by Attenuated Live Yersinia pestis Vaccine Strains against Lethal Infection with Virulent Y. pestis. Vaccines. 2021; 9(2):161. https://doi.org/10.3390/vaccines9020161
Chicago/Turabian StyleCote, Christopher K., Sergei S. Biryukov, Christopher P. Klimko, Jennifer L. Shoe, Melissa Hunter, Raysa Rosario-Acevedo, David P. Fetterer, Krishna L. Moody, Joshua R. Meyer, Nathaniel O. Rill, and et al. 2021. "Protection Elicited by Attenuated Live Yersinia pestis Vaccine Strains against Lethal Infection with Virulent Y. pestis" Vaccines 9, no. 2: 161. https://doi.org/10.3390/vaccines9020161
APA StyleCote, C. K., Biryukov, S. S., Klimko, C. P., Shoe, J. L., Hunter, M., Rosario-Acevedo, R., Fetterer, D. P., Moody, K. L., Meyer, J. R., Rill, N. O., Dankmeyer, J. L., Worsham, P. L., Bozue, J. A., & Welkos, S. L. (2021). Protection Elicited by Attenuated Live Yersinia pestis Vaccine Strains against Lethal Infection with Virulent Y. pestis. Vaccines, 9(2), 161. https://doi.org/10.3390/vaccines9020161






