Rates of SARS-CoV-2 Breakthrough Infection or Severe COVID-19 and Associated Risk Factors After Primary and Booster Vaccination Against COVID-19 in the Netherlands
Abstract
1. Introduction
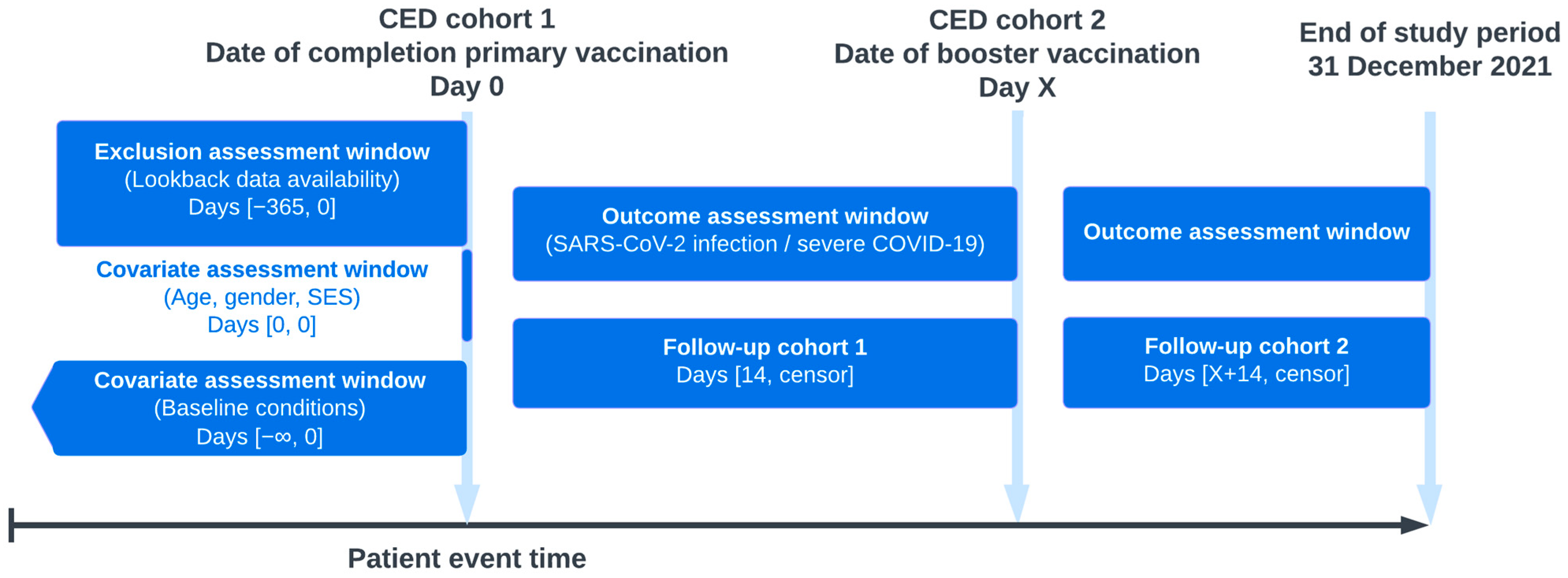
2. Methods
2.1. Data Setting
2.2. Study Population
2.3. Outcomes
2.4. Characteristics and Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Perez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Sadoff, J.; Gray, G.; Vandebosch, A.; Cardenas, V.; Shukarev, G.; Grinsztejn, B.; Goepfert, P.A.; Truyers, C.; Fennema, H.; Spiessens, B.; et al. Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against COVID-19. N. Engl. J. Med. 2021, 384, 2187–2201. [Google Scholar] [CrossRef] [PubMed]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Abu-Raddad, L.J.; Chemaitelly, H.; Ayoub, H.H.; AlMukdad, S.; Yassine, H.M.; Al-Khatib, H.A.; Smatti, M.K.; Tang, P.; Hasan, M.R.; Coyle, P.; et al. Effect of mRNA Vaccine Boosters against SARS-CoV-2 Omicron Infection in Qatar. N. Engl. J. Med. 2022, 386, 1804–1816. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.M.; et al. COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef]
- Ferdinands, J.M.; Rao, S.; Dixon, B.E.; Mitchell, P.K.; DeSilva, M.B.; Irving, S.A.; Lewis, N.; Natarajan, K.; Stenehjem, E.; Grannis, S.J.; et al. Waning of vaccine effectiveness against moderate and severe COVID-19 among adults in the US from the VISION network: Test negative, case-control study. BMJ 2022, 379, e072141. [Google Scholar] [CrossRef]
- Yan, Z.; Yang, M.; Lai, C.L. COVID-19 Vaccinations: A Comprehensive Review of Their Safety and Efficacy in Special Populations. Vaccines 2021, 9, 1097. [Google Scholar] [CrossRef]
- Notarte, K.I.; Ver, A.T.; Velasco, J.V.; Pastrana, A.; Catahay, J.A.; Salvagno, G.L.; Yap, E.P.H.; Martinez-Sobrido, L.; Torrelles, J.B.; Lippi, G.; et al. Effects of age, sex, serostatus, and underlying comorbidities on humoral response post-SARS-CoV-2 Pfizer-BioNTech mRNA vaccination: A systematic review. Crit. Rev. Clin. Lab. Sci. 2022, 59, 373–390. [Google Scholar] [CrossRef]
- Petras, M.; Macalik, R.; Janovska, D.; Celko, A.M.; Danova, J.; Selinger, E.; Dolecek, J.; Neradova, S.; Franklova, M.; Dlouhy, P.; et al. Risk factors affecting COVID-19 vaccine effectiveness identified from 290 cross-country observational studies until February 2022: A meta-analysis and meta-regression. BMC Med. 2022, 20, 461. [Google Scholar] [CrossRef]
- Van den Berg, J.M.; Remmelzwaal, S.; Blom, M.T.; van Hoek, B.; Swart, K.M.A.; Overbeek, J.A.; Burchell, G.L.; Herings, R.M.C.; Elders, P.J.M. Effectiveness of COVID-19 Vaccines in Adults with Diabetes Mellitus: A Systematic Review. Vaccines 2022, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, N.; Krastev, B.; Miteva, D.G.; Batselova, H.; Alexandrova, R.; Velikova, T. Effectiveness and safety of COVID-19 vaccines in patients with oncological diseases: State-of-the-art. World J. Clin. Oncol. 2023, 14, 343–356. [Google Scholar] [CrossRef]
- Bielopolski, D.; Libresco, G.; Barda, N.; Dagan, N.; Steinmetz, T.; Yahav, D.; Charytan, D.M.; Balicer, R.D.; Rozen-Zvi, B. BNT162b2 vaccine effectiveness in chronic kidney disease patients-an observational study. Clin. Kidney J. 2022, 15, 1838–1846. [Google Scholar] [CrossRef]
- Cheng, F.W.T.; Yan, V.K.C.; Wan, E.Y.F.; Chui, C.S.L.; Lai, F.T.T.; Wong, C.K.H.; Li, X.; Chan, C.I.Y.; Wang, B.; Tang, S.C.W.; et al. Vaccine Effectiveness of BNT162b2 and CoronaVac against SARS-CoV-2 Omicron BA.2 in CKD. Clin. J. Am. Soc. Nephrol. 2024, 19, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Kopel, H.; Nguyen, V.H.; Boileau, C.; Bogdanov, A.; Winer, I.; Ducruet, T.; Zeng, N.; Bonafede, M.; Esposito, D.B.; Martin, D.; et al. Comparative Effectiveness of Bivalent (Original/Omicron BA.4/BA.5) COVID-19 Vaccines in Adults. Vaccines 2023, 11, 1711. [Google Scholar] [CrossRef]
- Halloran, M.E.; Longini, I.M., Jr.; Struchiner, C.J. Design and interpretation of vaccine field studies. Epidemiol. Rev. 1999, 21, 73–88. [Google Scholar] [CrossRef]
- Crowcroft, N.S.; Klein, N.P. A framework for research on vaccine effectiveness. Vaccine 2018, 36, 7286–7293. [Google Scholar] [CrossRef]
- Dean, N.E.; Hogan, J.W.; Schnitzer, M.E. COVID-19 Vaccine Effectiveness and the Test-Negative Design. N. Engl. J. Med. 2021, 385, 1431–1433. [Google Scholar] [CrossRef] [PubMed]
- Habibzadeh, F.; Habibzadeh, P.; Yadollahie, M. On Measuring Vaccine Effectiveness with Observational Study Designs. Acta Med. Acad. 2022, 51, 134–146. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Patel, M.M.; Jewell, N.P.; Verani, J.R.; Kobayashi, M.; Tenforde, M.W.; Dean, N.E.; Cowling, B.J.; Lopman, B.A. Theoretical Framework for Retrospective Studies of the Effectiveness of SARS-CoV-2 Vaccines. Epidemiology 2021, 32, 508–517. [Google Scholar] [CrossRef]
- WHO. Guidance on Conducting Vaccine Effectiveness Evaluations in the Setting of New SARS-CoV-2 Variants. Addendum to Evaluation of COVID-19 Vaccine Effectiveness: Interim Guidance. Available online: https://iris.who.int/bitstream/handle/10665/343173/WHO-2019-nCoV-vaccine-effectiveness-variants-2021.1-eng.pdf?sequence=1 (accessed on 3 May 2025).
- Kuiper, J.G.; Bakker, M.; Penning-van Beest, F.J.A.; Herings, R.M.C. Existing Data Sources for Clinical Epidemiology: The PHARMO Database Network. Clin. Epidemiol. 2020, 12, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Overbeek, J.A.; Swart, K.M.A.; Houben, E.; Penning-van Beest, F.J.A.; Herings, R.M.C. Completeness and Representativeness of the PHARMO General Practitioner (GP) Data: A Comparison with National Statistics. Clin. Epidemiol. 2023, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Garry, E.M.; Weckstein, A.R.; Quinto, K.; Bradley, M.C.; Lasky, T.; Chakravarty, A.; Leonard, S.; Vititoe, S.E.; Easthausen, I.J.; Rassen, J.A.; et al. Categorization of COVID-19 severity to determine mortality risk. Pharmacoepidemiol. Drug Saf. 2022, 31, 721–728. [Google Scholar] [CrossRef]
- Harris, M.; Hart, J.; Bhattacharya, O.; Russell, F.M. Risk factors for SARS-CoV-2 infection during the early stages of the COVID-19 pandemic: A systematic literature review. Front. Public Health 2023, 11, 1178167. [Google Scholar] [CrossRef]
- Bar-On, Y.M.; Goldberg, Y.; Mandel, M.; Bodenheimer, O.; Freedman, L.; Kalkstein, N.; Mizrahi, B.; Alroy-Preis, S.; Ash, N.; Milo, R.; et al. Protection of BNT162b2 Vaccine Booster against COVID-19 in Israel. N. Engl. J. Med. 2021, 385, 1393–1400. [Google Scholar] [CrossRef]
- Solante, R.; Alvarez-Moreno, C.; Burhan, E.; Chariyalertsak, S.; Chiu, N.C.; Chuenkitmongkol, S.; Dung, D.V.; Hwang, K.P.; Ortiz Ibarra, J.; Kiertiburanakul, S.; et al. Expert review of global real-world data on COVID-19 vaccine booster effectiveness and safety during the omicron-dominant phase of the pandemic. Expert Rev. Vaccines 2023, 22, 1–16. [Google Scholar] [CrossRef] [PubMed]
- McMenamin, M.E.; Nealon, J.; Lin, Y.; Wong, J.Y.; Cheung, J.K.; Lau, E.H.Y.; Wu, P.; Leung, G.M.; Cowling, B.J. Vaccine effectiveness of one, two, and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong: A population-based observational study. Lancet Infect. Dis. 2022, 22, 1435–1443. [Google Scholar] [CrossRef]
- Lauring, A.S.; Tenforde, M.W.; Chappell, J.D.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Ghamande, S.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; et al. Clinical severity of, and effectiveness of mRNA vaccines against, COVID-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: Prospective observational study. BMJ 2022, 376, e069761. [Google Scholar] [CrossRef]
- Thompson, M.G.; Natarajan, K.; Irving, S.A.; Rowley, E.A.; Griggs, E.P.; Gaglani, M.; Klein, N.P.; Grannis, S.J.; DeSilva, M.B.; Stenehjem, E.; et al. Effectiveness of a Third Dose of mRNA Vaccines Against COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance—VISION Network, 10 States, August 2021-January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 139–145. [Google Scholar] [CrossRef]
- RIVM. Risk Groups and COVID-19. Available online: https://www.rivm.nl/en/coronavirus-covid-19/risk-groups (accessed on 25 March 2025).
- RIVM. Deelname COVID-19-Vaccinatie in Nederland. Available online: https://www.rivm.nl/sites/default/files/2022-01/COVID-19_Vaccinatie_Schattingen_WebSite_rapport_20220103_1259_def.pdf (accessed on 31 January 2024).
| Cohort 1 | Cohort 2 | |||||
|---|---|---|---|---|---|---|
| Vaccinated N (%) | SARS-CoV-2 Infection, n (IR/1000 PY) | Severe COVID-19, n (IR/1000 PY) | Vaccinated N (%) | SARS-CoV-2 Infection, n (IR/1000 PY) | Severe COVID-19, n (IR/1000 PY) | |
| Overall | 1,090,567 (100) | 12,050 (29.9) | 1233 (3.1) | 344,153 (100) | 38,637 (256.4) | 350 (2.3) |
| Gender | ||||||
| Female | 538,787 (49.4) | 5558 (29.1) | 719 (3.8) | 163,339 (47.5) | 18,323 (258.3) | 223 (3.1) |
| Male | 551,748 (50.6) | 6492 (30.7) | 514 (2.4) | 180,810 (52.5) | 20,314 (254.7) | 127 (1.6) |
| Age | ||||||
| 18–59 | 600,257 (55.0) | 7736 (39.9) | 248 (1.3) | 72,273 (21.0) | 13,971 (459.1) | 43 (1.5) |
| 60–69 | 169,530 (15.5) | 1633 (23.4) | 247 (3.5) | 97,834 (28.4) | 11,445 (274.6) | 99 (2.4) |
| 70–79 | 153,964 (14.1) | 1531 (21.0) | 350 (4.8) | 107,033 (31.1) | 9192 (189.9) | 96 (2.0) |
| 80+ | 83,780 (7.7) | 900 (18.1) | 380 (7.6) | 66,745 (19.4) | 3943 (122.1) | 112 (3.5) |
| Socioeconomic status | ||||||
| Low | 287,326 (26.3) | 2853 (27.0) | 386 (3.7) | 83,968 (24.4) | 7918 (223.3) | 102 (2.9) |
| Middle | 399,699 (36.7) | 4447 (29.5) | 492 (3.3) | 126,345 (36.7) | 13,094 (235.1) | 129 (2.3) |
| High | 397,653 (36.5) | 4690 (32.4) | 352 (2.4) | 113,824 (33.1) | 15,131 (296.7) | 107 (2.1) |
| Unknown | 5889 (0.5) | 60 (29.2) | 3 (1.5) | 20,016 (5.8) | 2494 (292.3) | 12 (1.4) |
| History of COVID-19 1 | ||||||
| No | 1,049,850 (96.3) | 11,891 (30.6) | 993 (2.6) | 331,432 (96.3) | 38,002 (263.0) | 235 (1.6) |
| Yes | 40,717 (3.7) | 159 (11.1) | 240 (16.7) | 12,721 (3.7) | 635 (102.6) | 115 (18.6) |
| Recent hospitalization 2 | ||||||
| No | 1,087,104 (99.7) | 12,012 (29.9) | 1150 (2.9) | 342,614 (99.6) | 38,518 (256.7) | 324 (2.2) |
| Yes | 3463 (0.3) | 38 (26.1) | 83 (56.8) | 1539 (0.4) | 119 (176.8) | 26 (38.5) |
| Smoking status | ||||||
| Never | 202,309 (18.6) | 2039 (23.2) | 293 (3.3) | 101,577 (29.5) | 8856 (199.7) | 110 (2.5) |
| Current | 77,021 (7.1) | 743 (24.7) | 107 (3.6) | 25,901 (7.5) | 2235 (194.8) | 25 (2.2) |
| Former | 164,435 (15.1) | 2444 (32.5) | 486 (6.5) | 94,473 (27.5) | 11,852 (271.8) | 122 (2.8) |
| Unknown | 646,802 (59.3) | 6824 (32.5) | 347 (1.7) | 122,202 (35.5) | 15,694 (306.1) | 93 (1.8) |
| Timing of vaccination | ||||||
| Q1 2021 | 67,540 (6.2) | 1476 (32.0) | 199 (4.3) | NA | NA | NA |
| Q2 2021 | 444,925 (40.8) | 5784 (28.7) | 703 (3.5) | NA | NA | NA |
| Q3 2021 | 539,708 (49.5) | 4743 (31.0) | 290 (1.9) | NA | NA | NA |
| Q4 2021 | 38,394 (3.5) | 47 (18.6) | 41 (16.2) | 344,153 (100) | 38,637 (256.4) | 350 (2.3) |
| Comorbidities | ||||||
| Diabetes mellitus | 90,820 (8.3) | 1110 (27.0) | 325 (7.9) | 47,966 (13.9) | 4290 (198.0) | 92 (4.2) |
| Cardiovascular disease | 333,644 (30.6) | 3768 (24.7) | 897 (5.9) | 189,299 (55.0) | 18,041 (211.0) | 259 (3.0) |
| Neurological disease | 36,525 (3.3) | 406 (25.1) | 117 (7.2) | 16,723 (4.9) | 1558 (207.3) | 31 (4.1) |
| Lung disease | 192,112 (17.6) | 2458 (31.2) | 560 (7.1) | 73,757 (21.4) | 8413 (257.5) | 141 (4.3) |
| Malignancy | 125,129 (11.5) | 1435 (24.4) | 364 (6.2) | 74,810 (21.7) | 7339 (215.4) | 101 (3.0) |
| Kidney disease | 55,627 (5.1) | 647 (23.6) | 264 (9.6) | 33,950 (9.9) | 2776 (176.0) | 73 (4.6) |
| Immune deficiency | 102,940 (9.4) | 1469 (31.9) | 444 (9.6) | 41,578 (12.1) | 4786 (254.2) | 95 (5.0) |
| Obesity | 115,175 (10.6) | 1567 (31.8) | 282 (5.7) | 52,294 (15.2) | 5573 (240.6) | 71 (3.1) |
| SARS-CoV-2 Infection | Severe COVID-19 | |||
|---|---|---|---|---|
| Primary Vaccination, IRR (95% CI) | Booster Vaccination, IRR (95% CI) | Primary Vaccination, IRR (95% CI) | Booster Vaccination, IRR (95% CI) | |
| N = 1,090,567 | N = 344,153 | N = 1,090,567 | N = 344,153 | |
| Gender | ||||
| Female | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Male | 0.84 (0.78–0.89) *** | 0.98 (0.94–1.03) NS | 1.48 (1.25–1.75) *** | 2.00 (1.42–2.81) *** |
| Age | ||||
| 18–59 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| 60–69 | 0.78 (0.71–0.85) *** | 0.62 (0.59–0.66) *** | 2.94 (2.18–3.97) *** | 1.56 (0.91–2.69) NS |
| 70–79 | 0.78 (0.72–0.86) *** | 0.49 (0.47–0.52) *** | 4.96 (3.80–6.47) *** | 1.23 (0.71–2.13) NS |
| 80+ | 0.83 (0.75–0.92) *** | 0.36 (0.34–0.39) *** | 9.90 (7.68–12.8) *** | 1.91 (1.11–3.31) * |
| Socioeconomic status | ||||
| Low | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Middle | 1.18 (1.08–1.28) *** | 1.05 (0.99–1.12) NS | 0.92 (0.76–1.13) NS | 0.90 (0.59–1.37) NS |
| High | 1.20 (1.11–1.31) *** | 1.33 (1.26–1.41) *** | 0.67 (0.54–0.83) *** | 0.88 (0.57–1.35) NS |
| Unknown | 0.93 (0.57–1.54) NS | 1.23 (1.11–1.35) *** | 0.41 (0.07–2.26) NS | 0.60 (0.24–1.48) NS |
| History of COVID-19 1 | ||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Yes | 0.30 (0.22–0.41) *** | 0.38 (0.32–0.45) *** | 4.86 (3.85–6.15) *** | 14.8 (10.5–20.7) *** |
| Recent hospitalization 2 | ||||
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Yes | 0.84 (0.47–1.50) NS | 0.71 (0.48–1.04) NS | 20.7 (14.9–28.8) *** | 19.3 (10.5–35.3) *** |
| Smoking status | ||||
| Current | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Former | 1.62 (1.41–1.88) *** | 1.51 (1.37–1.66) *** | 1.94 (1.41–2.67) *** | 1.27 (0.65–2.48) NS |
| Never | 1.03 (0.89–1.20) NS | 1.09 (0.98–1.20) NS | 1.01 (0.72–1.41) NS | 1.15 (0.58–2.26) NS |
| Unknown | 1.16 (1.01–1.33) * | 1.50 (1.36–1.65) *** | 0.43 (0.31–0.61) *** | 0.82 (0.41–1.63) NS |
| Timing of vaccination | ||||
| Q1 2021 | 1.00 (ref) | NA | 1.00 (ref) | NA |
| Q2 2021 | 0.58 (0.53–0.63) *** | NA | 0.59 (0.48–0.73) *** | NA |
| Q3 2021 | 0.42 (0.38–0.46) *** | NA | 0.19 (0.15–0.26) *** | NA |
| Q4 2021 | 0.08 (0.02–0.23) *** | NA | 0.32 (0.08–1.20) NS | NA |
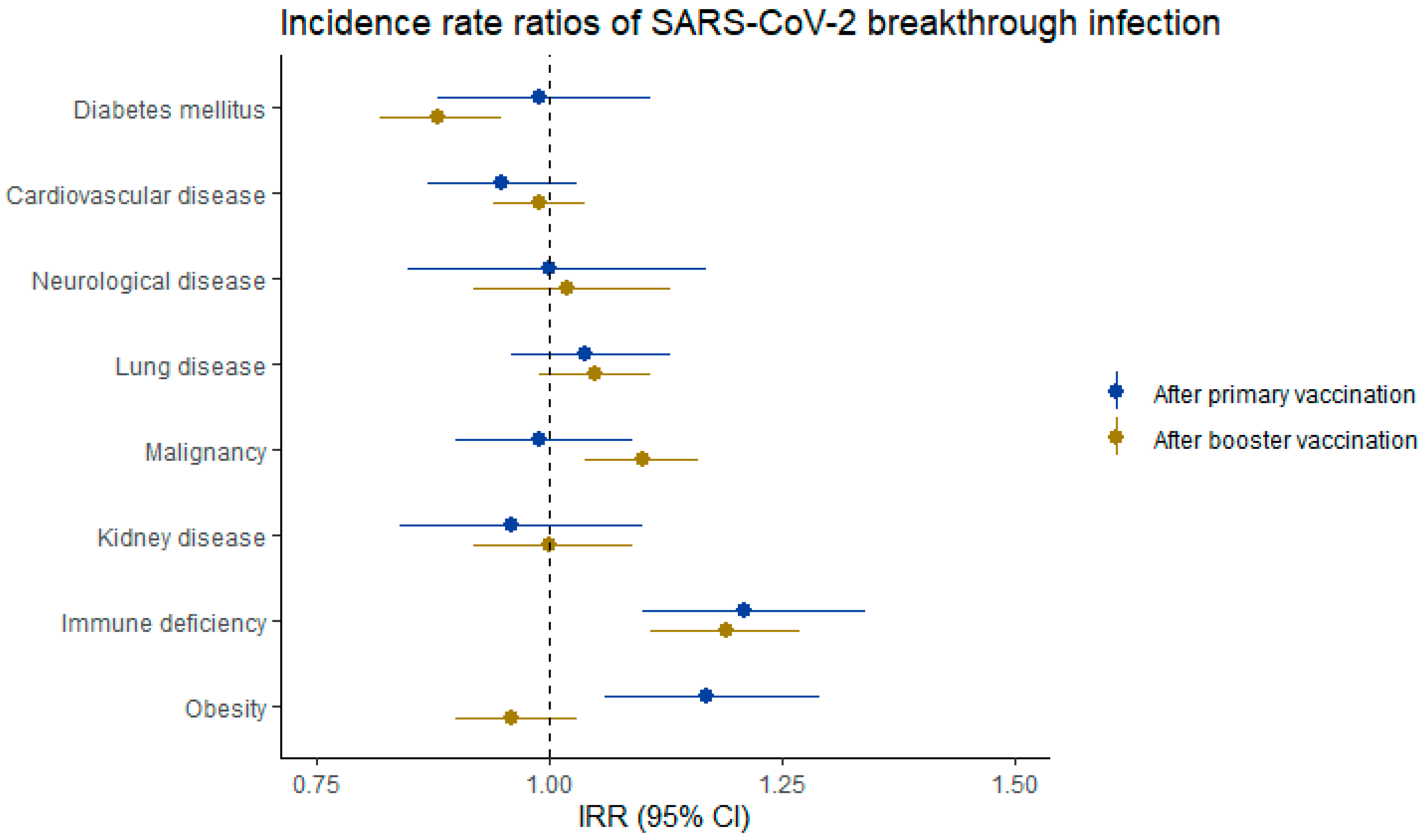
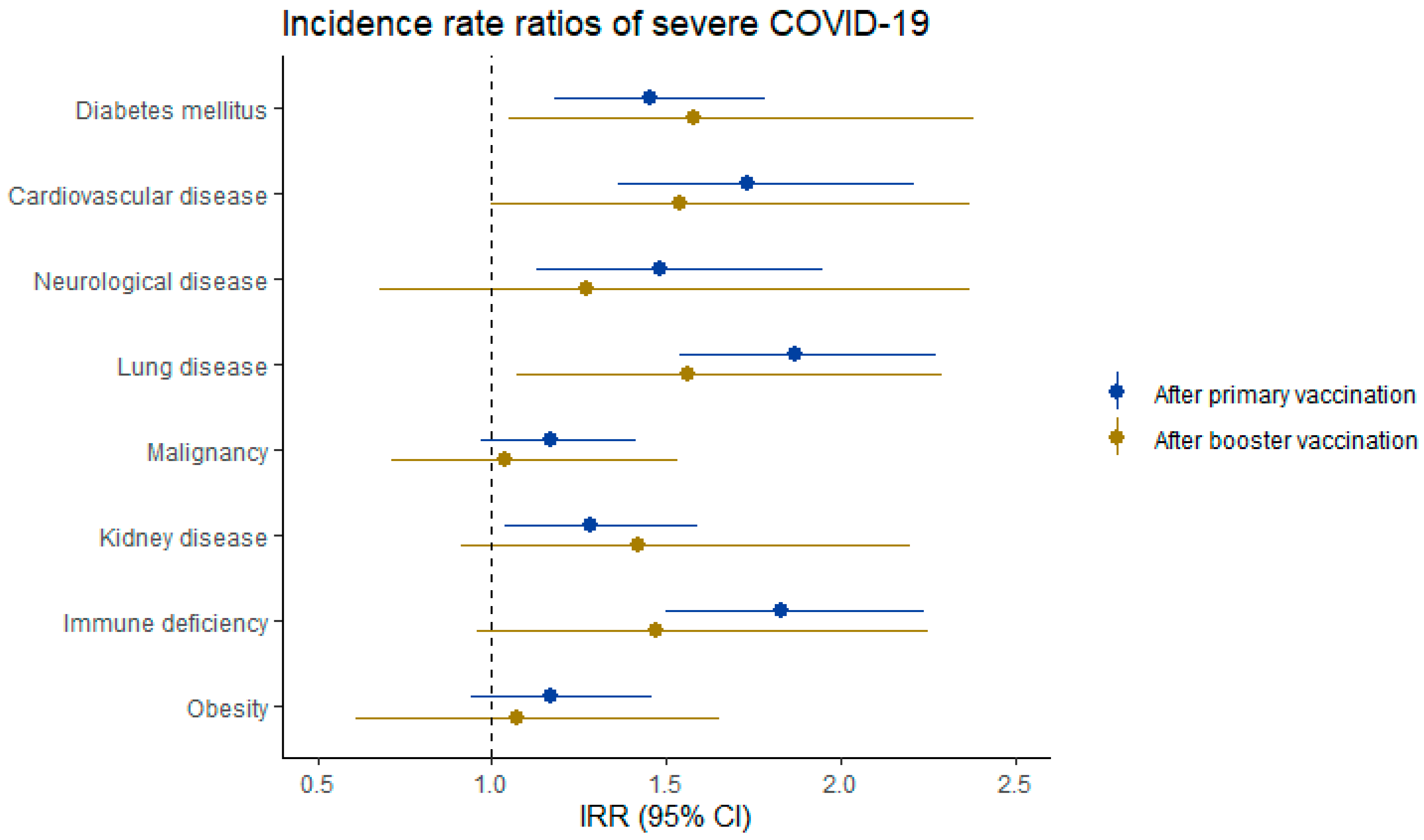
| Comorbidities | ||||
| Diabetes mellitus | 0.99 (0.88–1.11) NS | 0.88 (0.82–0.95) *** | 1.45 (1.18–1.78) *** | 1.58 (1.05–2.38) * |
| Cardiovascular disease | 0.95 (0.87–1.03) NS | 0.99 (0.94–1.04) NS | 1.73 (1.36–2.21) *** | 1.54 (1.00–2.37) NS |
| Neurological disease | 1.00 (0.85–1.17) NS | 1.02 (0.92–1.13) NS | 1.48 (1.13–1.95) ** | 1.27 (0.68–2.37) NS |
| Lung disease | 1.04 (0.96–1.13) NS | 1.05 (0.99–1.11) NS | 1.87 (1.54–2.27) *** | 1.56 (1.07–2.29) * |
| Malignancy | 0.99 (0.90–1.09) NS | 1.10 (1.04–1.16) *** | 1.17 (0.97–1.41) NS | 1.04 (0.71–1.53) NS |
| Kidney disease | 0.96 (0.84–1.10) NS | 1.00 (0.92–1.09) NS | 1.28 (1.04–1.59) * | 1.42 (0.91–2.20) NS |
| Immune deficiency | 1.21 (1.10–1.34) *** | 1.19 (1.11–1.27) *** | 1.83 (1.50–2.24) *** | 1.47 (0.96–2.25) NS |
| Obesity | 1.17 (1.06–1.29) ** | 0.96 (0.90–1.03) NS | 1.17 (0.94–1.46) NS | 1.07 (0.69–1.65) NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van den Berg, J.M.; Blom, M.T.; Overbeek, J.A.; Remmelzwaal, S.; Herings, R.M.C.; Elders, P.J.M. Rates of SARS-CoV-2 Breakthrough Infection or Severe COVID-19 and Associated Risk Factors After Primary and Booster Vaccination Against COVID-19 in the Netherlands. Vaccines 2025, 13, 564. https://doi.org/10.3390/vaccines13060564
van den Berg JM, Blom MT, Overbeek JA, Remmelzwaal S, Herings RMC, Elders PJM. Rates of SARS-CoV-2 Breakthrough Infection or Severe COVID-19 and Associated Risk Factors After Primary and Booster Vaccination Against COVID-19 in the Netherlands. Vaccines. 2025; 13(6):564. https://doi.org/10.3390/vaccines13060564
Chicago/Turabian Stylevan den Berg, Jesse M., Marieke T. Blom, Jetty A. Overbeek, Sharon Remmelzwaal, Ron M. C. Herings, and Petra J. M. Elders. 2025. "Rates of SARS-CoV-2 Breakthrough Infection or Severe COVID-19 and Associated Risk Factors After Primary and Booster Vaccination Against COVID-19 in the Netherlands" Vaccines 13, no. 6: 564. https://doi.org/10.3390/vaccines13060564
APA Stylevan den Berg, J. M., Blom, M. T., Overbeek, J. A., Remmelzwaal, S., Herings, R. M. C., & Elders, P. J. M. (2025). Rates of SARS-CoV-2 Breakthrough Infection or Severe COVID-19 and Associated Risk Factors After Primary and Booster Vaccination Against COVID-19 in the Netherlands. Vaccines, 13(6), 564. https://doi.org/10.3390/vaccines13060564






