Mpox Incidence and Vaccine Uptake in Men Who Have Sex with Men and Are Living with HIV in Denmark
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Vaccination
2.3. Outcomes
- (1)
- A positive mpox test;
- (2)
- Receiving the mpox vaccine.
2.4. Covariates
2.5. Survey
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Incidence of Mpox Infection and Related Risk Factors
3.3. Determinants Associated with Vaccine Uptake
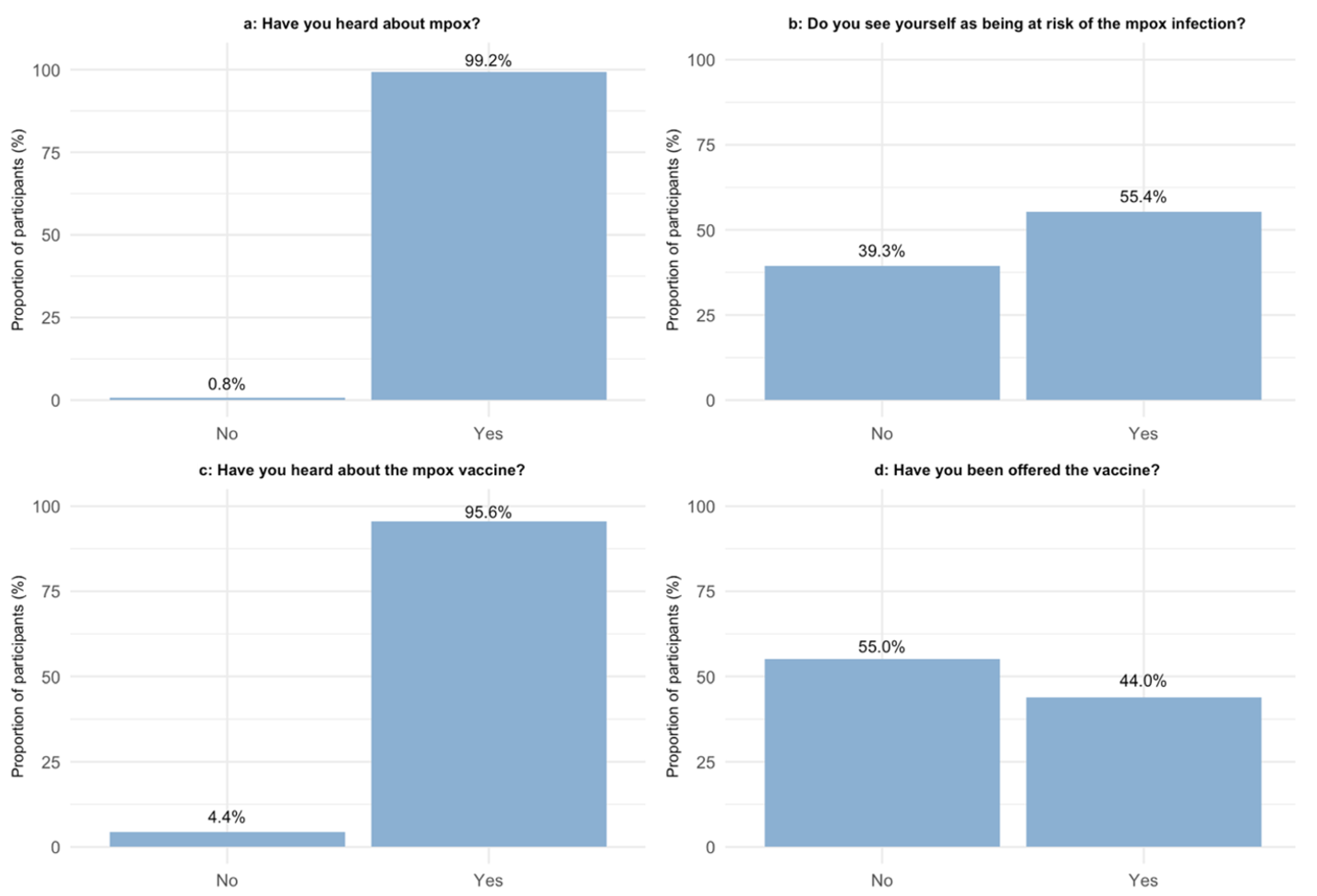
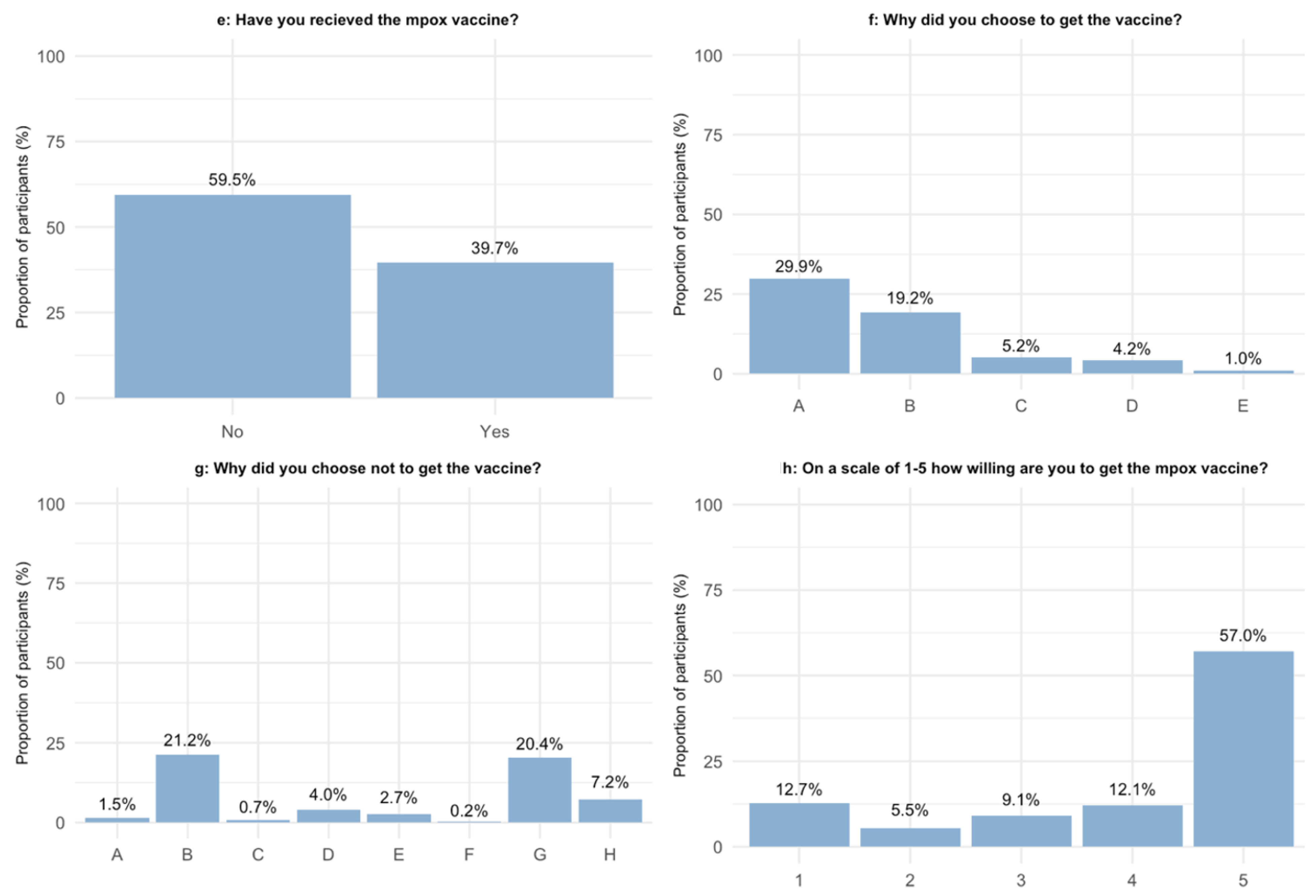
3.4. Survey Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Factsheet for Health Professionals on Mpox (Monkeypox). Available online: https://www.ecdc.europa.eu/en/all-topics-z/monkeypox/factsheet-health-professionals (accessed on 16 June 2023).
- Signs and Symptoms|Mpox|Poxvirus|CDC. Available online: https://www.cdc.gov/poxvirus/monkeypox/symptoms/index.html (accessed on 14 January 2023).
- Yuan, S.; Jiang, S.C.; Zhang, Z.W.; Fu, Y.F.; Yang, X.Y.; Li, Z.L.; Hu, J. How and when does monkeypox (mpox) transmit: Implications for prevention and treatments. Front. Pharmacol. 2023, 13, 1109928. [Google Scholar] [CrossRef] [PubMed]
- Kumbhar, N.; Agarwala, P. The lurking threat of monkeypox in current times. Indian J. Med. Microbiol. 2022, 40, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Horita, N.; Fukumoto, T. Global case fatality rate from COVID-19 has decreased by 96.8% during 2.5 years of the pandemic. J. Med. Virol. 2023, 95, e28231. [Google Scholar] [CrossRef] [PubMed]
- Bragazzi, N.L.; Kong, J.D.; Mahroum, N.; Tsigalou, C.; Khamisy-Farah, R.; Converti, M.; Wu, J. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: A preliminary pooled data analysis and literature review. J. Med. Virol. 2022, 95, e27931. [Google Scholar] [CrossRef]
- Mpox and HIV|Mpox|Poxvirus|CDC. Available online: https://www.cdc.gov/poxvirus/monkeypox/prevention/hiv.html (accessed on 25 December 2022).
- UKHSA Finds Vaccination Offers Strong Protection against Monkeypox—GOV.UK. Available online: https://www.gov.uk/government/news/ukhsa-finds-vaccination-offers-strong-protection-against-monkeypox (accessed on 5 January 2023).
- Abekopper—Sundhedsstyrelsen. Available online: https://www.sst.dk/da/Viden/Abekopper (accessed on 25 December 2022).
- Ronit, A.; Haissman, J.; Kirkegaard-Klitbo, D.M.; Kristensen, T.S.; Lebech, A.-M.; Benfield, T.; Gerstoft, J.; Ullum, H.; Køber, L.; Kjær, A.; et al. Copenhagen comorbidity in HIV infection (COCOMO) study: A study protocol for a longitudinal, non-interventional assessment of non-AIDS comorbidity in HIV infection in Denmark. BMC Infect. Dis. 2016, 16, 713. [Google Scholar] [CrossRef]
- Imvanex|European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/imvanex#authorisation-details-section (accessed on 30 May 2023).
- Voldstedlund, M.; Haarh, M.; Mølbak, K.; MiBa Board of Representatives. The Danish Microbiology Database (MiBa) 2010 to 2013. Eurosurveillance 2014, 19, 29. [Google Scholar] [CrossRef]
- Krause, T.G.; Jakobsen, S.; Haarh, M.; Mølbak, K. The Danish vaccination register. Eurosurveillance 2012, 17, 20155. [Google Scholar] [CrossRef]
- Notat: Sundhedsstyrelsens Udmeldinger om Indtag af Alkohol—Sundhedsstyrelsen. Available online: https://www.sst.dk/da/udgivelser/2022/Notat-Sundhedsstyrelsens-udmeldinger-om-indtag-af-alkohol (accessed on 28 April 2023).
- Curran, K.G.; Eberly, K.; Russell, O.O.; Snyder, R.E.; Phillips, E.K.; Tang, E.C.; Peters, P.J.; Sanchez, M.A.; Hsu, L.; Cohen, S.E.; et al. HIV and Sexually Transmitted Infections Among Persons with Monkeypox—Eight U.S. Jurisdictions, 17 May–22 July 2022. MMWR. Morb. Mortal. Wkly. Rep. 2022, 71, 1141–1147. [Google Scholar] [CrossRef]
- Investigation into Monkeypox Outbreak in England: Technical Briefing 6—GOV.UK. Available online: https://www.gov.uk/government/publications/monkeypox-outbreak-technical-briefings/investigation-into-monkeypox-outbreak-in-england-technical-briefing-6 (accessed on 27 December 2022).
- Reyes-Urueña, J.; D’Ambrosio, A.; Croci, R.; Bluemel, B.; Cenciarelli, O.; Pharris, A.; Dukers-Muijrers, N.; Nutland, W.; Niaupari, S.; Badran, J.; et al. High monkeypox vaccine acceptance among male users of smartphone-based online gay-dating apps in Europe, 30 July to 12 August 2022. Eurosurveillance 2022, 27, 2200757. [Google Scholar] [CrossRef]
- Zheng, M.; Qin, C.; Qian, X.; Yao, Y.; Liu, J.; Yuan, Z.; Ma, L.; Fan, J.; Tao, R.; Zhou, F.; et al. Knowledge and vaccination acceptance toward the human monkeypox among men who have sex with men in China. Front. Public Health 2022, 10. [Google Scholar] [CrossRef]
- Allan-Blitz, L.-T.; Gandhi, M.; Adamson, P.; Park, I.; Bolan, G.; Klausner, J.D. A Position Statement on Mpox as a Sexually Transmitted Disease. Clin. Infect. Dis. 2023, 76, 1508–1512. [Google Scholar] [CrossRef] [PubMed]
- Thornhill, J.P.; Barkati, S.; Walmsley, S.; Rockstroh, J.; Antinori, A.; Harrison, L.B.; Palich, R.; Nori, A.; Reeves, I.; Habibi, M.S.; et al. Monkeypox Virus Infection in Humans across 16 Countries—April–June 2022. N. Engl. J. Med. 2022, 387, 679–691. [Google Scholar] [CrossRef] [PubMed]
- Philpott, D.; Hughes, C.M.; Alroy, K.A.; Kerins, J.L.; Pavlick, J.; Asbel, L.; Crawley, A.; Newman, A.P.; Spencer, H.; Feldpausch, A.; et al. Epidemiologic and Clinical Characteristics of Monkeypox Cases—United States, 17 May–22 July 2022. MMWR. Morb. Mortal. Wkly. Rep. 2022, 71, 1018–1022. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Bilinska, J.; Tam, J.C.H.; Fontoura, D.D.S.; Mason, C.Y.; Daunt, A.; Snell, L.B.; Murphy, J.; Potter, J.; Tuudah, C.; et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: Descriptive case series. BMJ 2022, 378, e072410. [Google Scholar] [CrossRef]
- Girometti, N.; Ogoina, D.; Tan, D.H.S.; Pozniak, A.; Klein, M.B. Intersecting HIV and mpox epidemics: More questions than answers. J. Int. AIDS Soc. 2022, 25, e26043. [Google Scholar] [CrossRef]
- Delaney, K.P.; Sanchez, T.; Hannah, M.; Edwards, O.W.; Carpino, T.; Agnew-Brune, C.; Renfro, K.; Kachur, R.; Carnes, N.; DiNenno, E.A.; et al. Strategies Adopted by Gay, Bisexual, and Other Men Who Have Sex with Men to Prevent Monkeypox virus Transmission—United States, August 2022. MMWR. Morb. Mortal. Wkly. Rep. 2022, 71, 1126–1130. [Google Scholar] [CrossRef]
- Gilbert, M.; Ablona, A.; Chang, H.-J.; Grennan, T.; Irvine, M.A.; Racey, C.S.; Salway, T.; Naus, M.; Dawar, M.; Ogilvie, G. Uptake of Mpox vaccination among transgender people and gay, bisexual and other men who have sex with men among sexually-transmitted infection clinic clients in Vancouver, British Columbia. Vaccine 2023, 41, 2485–2494. [Google Scholar] [CrossRef]
- Mangtani, P.; Breeze, E.; Kovats, S.; Ng, E.S.; Roberts, J.A.; Fletcher, A. Inequalities in influenza vaccine uptake among people aged over 74 years in Britain. Prev. Med. 2005, 41, 545–553. [Google Scholar] [CrossRef]
- Wada, K.; Smith, D.R. Influenza Vaccination Uptake among the Working Age Population of Japan: Results from a National Cross-Sectional Survey. PLoS ONE 2013, 8, e59272. [Google Scholar] [CrossRef]
- Jackson, S.E.; Paul, E.; Brown, J.; Steptoe, A.; Fancourt, D. Negative Vaccine Attitudes and Intentions to Vaccinate Against Covid-19 in Relation to Smoking Status: A Population Survey of UK Adults. Nicotine Tob. Res. 2021, 23, 1623–1628. [Google Scholar] [CrossRef]
- Zucman, D.; Fourn, E.; Touche, P.; Majerholc, C.; Vallée, A. Monkeypox Vaccine Hesitancy in French Men Having Sex with Men with PrEP or Living with HIV in France. Vaccines 2022, 10, 1629. [Google Scholar] [CrossRef] [PubMed]
- Lounis, M.; Riad, A. Monkeypox (MPOX)-Related Knowledge and Vaccination Hesitancy in Non-Endemic Countries: Concise Literature Review. Vaccines 2023, 11, 229. [Google Scholar] [CrossRef]
- Biasio, L.R.; Corsello, G.; Costantino, C.; Fara, G.M.; Giammanco, G.; Signorelli, C.; Vecchio, D.; Vitale, F. Communication about vaccination: A shared responsibility. Hum. Vaccines Immunother. 2016, 12, 2984–2987. [Google Scholar] [CrossRef] [PubMed]
- Risk Communication and Community Engagement Public Health Advice on Understanding, Preventing and Addressing Stigma and Discrimination Related to Monkeypox. Available online: https://www.who.int/publications/m/item/communications-and-community-engagement-interim-guidance-on-using-inclusive-language-in-understanding--preventing-and-addressing-stigma-and-discrimination-related-to-monkeypox (accessed on 26 June 2023).
- Yang, Z.; Liu, X.; Zhu, Z.; Zhang, L.; Han, S.; Fu, Y.; Lu, H. Combating Stigma and Health Inequality of Monkeypox: Experience from HIV. Infect. Drug Resist. 2022, 15, 5941–5943. [Google Scholar] [CrossRef] [PubMed]
| Clinical Characteristics | All Participants (n = 727) |
|---|---|
| Age (years) | 55.7 (48.3–62.8) |
| Men | 727 (100.0%) |
| Alcohol (grams per week) | 7 (2–14) |
| Alcohol (more than 10 units per week) | 256 (35% [31–39%]) |
| Smoking status | |
| Ex-smoker | 263 (36% [31–39%]) |
| Never smoked | 248 (34% [31–38%]) |
| Current smoker | 205 (28% [25–32%]) |
| Origin | |
| Scandinavian | 557 (77% [73–80%]) |
| Other European | 83 (11% [9–14%]) |
| Other | 87 (12% [10–15%]) |
| Plasma HIV RNA < 50 copies/mL | 686 (94.4% [92–96%]) |
| Blood CD4+ lymphocyte count, cells/µL | 695 (260.6) |
| Education | |
| No education or a short education | 329 (45% [42–49%]) |
| Long education | 367 (50% [47–54%]) |
| STD in the preceding two years | 184 (25% [22–29%]) |
| Clinical Characteristics | Unvaccinated (n = 489) | Vaccinated (n = 238) | p-Value | aOR [95% Confidence Interval] |
|---|---|---|---|---|
| Age (years) | 56.9 (48.6–64.6) | 53.8 54 (48.0–59.6) | <0.001 | 0.9 [0.9–1.0] |
| Alcohol (units per week) | 7 (2–15) | 6 (1.2–13) | 0.3 | 1.0 [0.9–1.0] |
| Alcohol (more than 10 unit per week) | 175 (36% [32–40%]) | 81 (34% [28–40%]) | 0.7 | 1.0 [0.7–1.4] |
| Smoking status | 0.01 | |||
| Ex-smoker | 178 (36% [32–41%]) | 85 (36% [30–42%]) | 0.9 [0.6–1.4] | |
| Never smoked | 153 (31% [27–36%]) | 95 (40% [34–46%]) | 1.7 [1.2–2.6] | |
| Current smoker | 153 (31% [27–36%]) | 52 (22% [17–28%]) | 0.6 [0.4–0.9] | |
| Origin | 0.3 | |||
| Scandinavian | 378 (77% [73–81%]) | 189 (79% [74–84%]) | 1.5 [0.9–2.6] | |
| Other European | 61 (12% [10–16%]) | 22 (9% [6–14%]) | 1.1 [0.5–2.2] | |
| Other | 60 (12% [9–16%]) | 27 (11% [8–16%]) | 0.7 [0.4–1.2] | |
| Plasma HIV RNA < 50 copies/mL | 464 (94% [93–96.6%]) | 222 (93% [89–96%]) | 0.5 | 0.7 [0.4–1.4] |
| Blood CD4+ lymphocyte count, cells/µL | 691.3 (253) | 702.6 (276.2) | 1.0 [1.0–1.0] | |
| Education | 0.3 | |||
| No education or a short education | 227 (46% [42–51%]) | 102 (43% [36–49%]) | 0.9 [0.6–1.2] | |
| Long education | 239 (49% [44–53%]) | 128 (54% [47–60%]) | Model did not converge | |
| STD in the preceding two years | 85 (17% [14–21%]) | 99 (42% [35–48%]) | <0.001 | 3.1 [2.2–4.6] |
| Clinical Characteristics | Did Not Answer Survey (n = 326) | Answered Survey (n = 401) | p-Value |
|---|---|---|---|
| Age (years) | 55.3 (47.2–62.9) | 56 (49.2–62.6) | 0.3 |
| Men | 326 (100.0%) | 401 (100.0%) | 0.2 |
| Alcohol (units per week) | 6 (0.0–13.0) | 8 (3.0–15.0) | 0.03 |
| Alcohol (more than 10 unit per week) | 109 (33% [28–39%]) | 147 (37% [32–42%]) | 0.4 |
| Smoking status | 0.003 | ||
| Ex-smoker | 115 (35% [30–41%]) | 148 (37% [32–42%]) | |
| Never smoked | 93 (29% [24–34%]) | 155 (39% [34–44%]) | |
| Current smoker | 111 (34.0% [29–40%]) | 111 (28% [23–32%]) | |
| Origin | 0.01 | ||
| Scandinavian | 234 (71.8% [30–41%]) | 323 (81% [76–84%]) | |
| Other European | 42 (12.9% [30–41%]) | 41 (10% [7–14%]) | |
| Other | 50 (15.3% [30–41%]) | 37 (9% [7–12%]) | |
| Plasma HIV RNA < 50 copies/mL | 307 (94.2% [92–97%]) | 379 (95% [92–97%]) | 0.9 |
| Blood CD4+ lymphocyte count, cells/µL | 706.4 (270.6) | 686.4 (253) | 0.4 |
| Education | 0.9 | ||
| No education or a short education | 144 (44% [39–50%]) | 185 (46% [41–51%]) | |
| Long education | 162 (50% [44–55%]) | 205 (51% [46–56%]) | |
| STD in the preceding two years | 86 (26% [22–32%]) | 98 (24% [20–29%]) | 0.6 |
| Survey Question | Unvaccinated (n = 246) | Vaccinated (n = 155) | p-Value |
|---|---|---|---|
| On a scale of 1–5, how worried are you about getting infected with mpox? | <0.001 | ||
| 1 | 94 (41.2%) | 20 (12.9%) | |
| 2 | 64 (28.1%) | 42 (27.1%) | |
| 3 | 38 (16.7%) | 46 (29.7%) | |
| 4 | 24 (10.5%) | 30 (19.4%) | |
| 5 | 8 (3.5%) | 14 (9.0%) | |
| How many partners have you had in the last 12 weeks? | <0.001 | ||
| 0–1 | 89 (58.6%) | 22 (14.8%) | |
| 1–5 | 49 (32.2%) | 79 (53.0%) | |
| >5 | 14 (9.2%) | 48 (32.2%) | |
| Had at least one STD in the preceding two years | <0.001 | ||
| Yes | 33 (14.2%) | 60 (38.7%) | |
| No | 199 (85.8%) | 95 (61.3%) | |
| On a scale of 1–5, how willing are you to get the mpox vaccine? | Been offered a vaccine | Not been offered a vaccine | <0.001 |
| 1 | 10 (6.0%) | 35 (18.2%) | |
| 2 | 5 (3.0%) | 15 (7.8%) | |
| 3 | 4 (2.4%) | 28 (14.6%) | |
| 4 | 12 (7.2%) | 31 (16.1%) | |
| 5 | 132 (79.0%) | 74 (38.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Svartstein, A.-S.W.; Knudsen, A.D.; Heidari, S.-L.; Heftdal, L.D.; Gelpi, M.; Benfield, T.; Nielsen, S.D. Mpox Incidence and Vaccine Uptake in Men Who Have Sex with Men and Are Living with HIV in Denmark. Vaccines 2023, 11, 1167. https://doi.org/10.3390/vaccines11071167
Svartstein A-SW, Knudsen AD, Heidari S-L, Heftdal LD, Gelpi M, Benfield T, Nielsen SD. Mpox Incidence and Vaccine Uptake in Men Who Have Sex with Men and Are Living with HIV in Denmark. Vaccines. 2023; 11(7):1167. https://doi.org/10.3390/vaccines11071167
Chicago/Turabian StyleSvartstein, Anne-Sophie Winther, Andreas Dehlbæk Knudsen, Safura-Luise Heidari, Line Dam Heftdal, Marco Gelpi, Thomas Benfield, and Susanne Dam Nielsen. 2023. "Mpox Incidence and Vaccine Uptake in Men Who Have Sex with Men and Are Living with HIV in Denmark" Vaccines 11, no. 7: 1167. https://doi.org/10.3390/vaccines11071167
APA StyleSvartstein, A.-S. W., Knudsen, A. D., Heidari, S.-L., Heftdal, L. D., Gelpi, M., Benfield, T., & Nielsen, S. D. (2023). Mpox Incidence and Vaccine Uptake in Men Who Have Sex with Men and Are Living with HIV in Denmark. Vaccines, 11(7), 1167. https://doi.org/10.3390/vaccines11071167






