1. Introduction
Healthcare workers are exposed to communicable diseases during the course of their work and are at risk of acquiring occupational infections. The Centers for Disease Control and Prevention (CDC) recommends healthcare workers to be vaccinated against a series of infectious diseases such as hepatitis B, measles, mumps, and rubella (MMR), varicella, pertussis, and meningococcal disease [
1].
Measles and varicella are highly contagious and can spread by respiratory aerosols [
2,
3]. In a hospital, cases of measles and varicella infection will require airborne precaution as part of infection control measures. Similarly, cases of disseminated herpes zoster infection caused by reactivation of the varicella-zoster virus (VZV) will also need airborne precaution [
4].
Infection prevention measures for healthcare workers exposed to the measles virus and VZV at work including contact tracing and medical management are essential to prevent and control the spread of disease in a hospital setting [
5,
6]. However, these processes are time-consuming, resource-intensive, and disrupts healthcare operations, especially if susceptible healthcare workers are required to take a leave of absence to prevent the spread of infection [
7,
8].
Measles and varicella infection are highly preventable with vaccination [
6,
9,
10,
11,
12]. Increased vaccination coverage against measles virus and VZV will protect healthcare workers from contracting occupational infections.
An internal audit conducted in a tertiary hospital in Singapore found most of its staff lacking in the documentation of immunity status against vaccine-preventable diseases such as measles and varicella. The Ministry of Health in Singapore recommends healthcare workers to be vaccinated against MMR, varicella, influenza, hepatitis B, tetanus, diphtheria, and pertussis (Tdap) [
13].
We aim to describe the implementation process of a measles and varicella vaccination program and report on the reduction in the number of susceptible healthcare workers exposed to measles, varicella, and disseminated zoster infection at the hospital. Vaccination against measles is performed as part of MMR vaccination. Although vaccination against measles and varicella for healthcare workers is widely advocated, a detailed description of the implementation process and direct outcomes during epidemiological investigation of exposed healthcare workers has not been widely reported.
2. Materials and Methods
A hospital-wide vaccination program, which includes vaccination against measles and varicella, was first planned in May 2015, in line with the recommendation from the Ministry of Health, Singapore [
13]. We used the Consolidated Framework for Implementation Research (CFIR) model to describe the planning and implementation of the vaccination program [
14]. CFIR consists of five major constructs: intervention characteristics, outer setting, inner setting, characteristics of the individuals involved, and the implementation process [
15].
The vaccination program for healthcare workers was implemented at the hospital in Singapore from October 2015 to September 2018.
Intervention characteristics: the vaccination program was an initiative from the hospital to protect its staff and patients against nosocomial infections. The program was introduced and communicated to the head of departments and nursing leaders via physical meetings and e-mails. The benefits of having documented immunity to measles and VZV were outlined to the relevant stakeholders to ensure support from all parties. A timeline for the completion of the project was set to three years. All costs were covered by the hospital. The heads of department then disseminated the vaccination program information to their team members.
Outer setting: the vaccination program ensured that the healthcare workers were vaccinated against vaccine-preventable diseases, in line with the vaccination recommendations from the Ministry of Health in Singapore.
Inner setting: the hospital was a large 1200-bedded tertiary hospital, with a staff strength of approximately 7000 workers. It also functioned as a teaching hospital, with over fifty medical, surgical, and dental specialties. All staff without immunization records were required to undergo a medical review under the vaccination program.
Characteristics of the individuals involved: all healthcare workers including physicians, nurses, allied health members, administrators, and housekeeping staff were targeted in the program. The healthcare workers may be employed by the hospital or external partners.
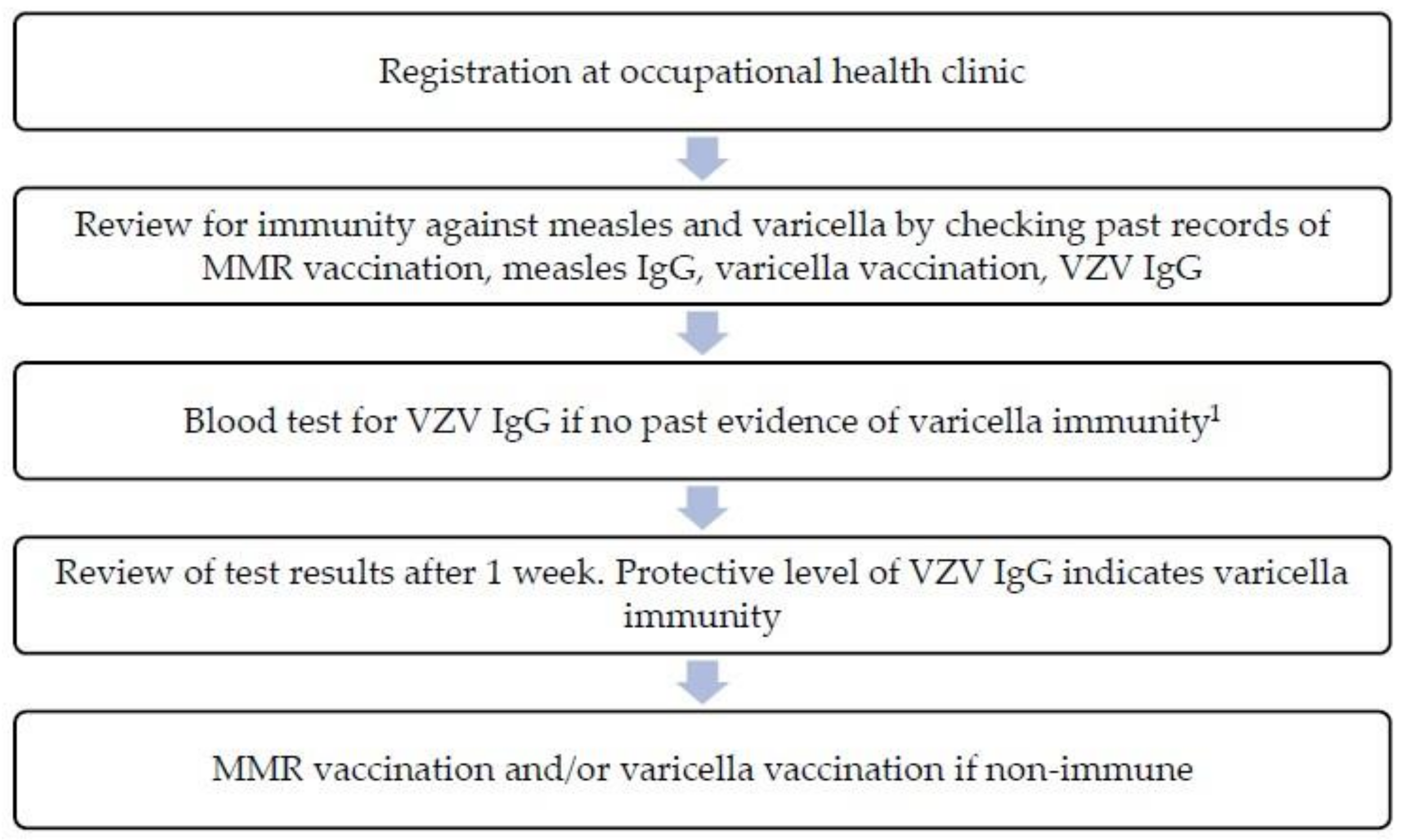
Implementation process: the vaccination review process was carried out by the hospital’s occupational health physician and nurses at the occupational health clinic (
Figure 1). Healthcare workers taking care of susceptible patients (e.g., patients at oncology wards, pediatric wards) and staff working at areas with high infectious disease exposure risk (e.g., Emergency Department) were given priority with earlier review sessions. For immunity against measles, healthcare workers were required to have a record of two MMR vaccine doses administered at least 28 days apart or protective level of measles immunoglobulin G (IgG) (laboratory reference ≥250 mIU/mL). Those without proof of MMR immunization were vaccinated. For immunity against varicella, healthcare workers were required to have a record of two doses of varicella-zoster vaccine or protective level of VZV IgG (laboratory reference ≥100 mIU/mL). Healthcare workers without previous varicella-zoster vaccination and a negative VZV IgG were vaccinated. Serum IgG antibodies against measles and varicella were measured using enzyme-linked immunosorbent assay (ELISA). All serology test results and records of vaccination were uploaded into the hospital’s electronic health records.
By the end of 2016, 3516 (58%) out of 7076 staff had completed their immunization review. By the end of the vaccination program in 2018, a total of 6770 (95%) out of 7083 healthcare workers had completed their vaccination review.
Cases of measles, varicella, and disseminated zoster in the hospital were reported to the hospital’s Epidemiology Unit for initiation of the contact tracing process. Verification of immunization status for healthcare workers with high-risk exposure was conducted by checking the electronic medical records. Healthcare workers with complete vaccination records or with previous protective IgG levels for the respective disease of exposure were considered immune. Healthcare workers without documented proof of immunity had to attend an urgent medical evaluation at the occupational health clinic to assess immunity against the disease of exposure. Reviewed staff without proof of vaccination underwent serological testing for VZV IgG or measles IgG for exposure to varicella, disseminated herpes zoster, or measles respectively. If the corresponding IgG result was negative, the worker was considered susceptible and was put on leave from work during the incubation period of the disease.
We report on the number of exposed, assessed (at the occupational health clinic), and susceptible healthcare workers for exposure to (a) measles cases and (b) varicella and disseminated herpes zoster infection cases for the years 2016, 2017, and 2018. The proportion of healthcare workers reviewed at the occupational health clinic and susceptible healthcare workers was reported as an outcome of the vaccination program. We used Stata 17 to perform a descriptive analysis of the outcome.
This study was approved by the National Healthcare Group, Domain-Specific Review Board, for exemption of a formal review.
3. Results
The number of healthcare workers assessed at the occupational health clinic for exposure to measles, varicella, and disseminated herpes zoster and the number of susceptible healthcare workers were reduced throughout the vaccination program.
In 2016, a total of 198 healthcare workers were exposed to measles cases (
Table 1). Out of the 198 staff members, 101 (51%) workers did not have documentation of measles immunity (two doses of MMR vaccine or previous protective level of measles IgG) and were assessed at the occupational health clinic. Twenty (10%) workers were not able to demonstrate past records of MMR vaccination and had titers of measles IgG below the protective level. These 20 workers were considered susceptible and had to be put on medical leave for several days to prevent the spread of nosocomial infection. In comparison, five (10%) out of 51 exposed healthcare workers were assessed at the occupational health clinic in 2018. No one was found susceptible to measles (
p < 0.01).
With respect to varicella and disseminated zoster, a total of 154 healthcare workers were exposed in 2016 (
Table 2). Out of the 154 exposed staff members, 114 (74%) workers did not have documentation of varicella immunity (two doses of VZV vaccine or previous protective level of VZV IgG) and were assessed at the occupational health clinic. Seven (5%) workers were not able to demonstrate past records of VZV vaccination and had titers of VZV IgG below the protective level. These seven workers were considered susceptible and were put on medical leave. In comparison, 17 (5%) out of 377 exposed healthcare workers were assessed at the occupational health clinic in 2018. Only two (1%) were considered susceptible (
p < 0.01).
4. Discussion
The vaccination program took approximately three years to complete, and successfully ensured immunity against measles and VZV for most of the healthcare workers. Based on CDC recommendations, healthcare workers were considered immune to measles after two doses of the MMR vaccine (administered at least 28 days apart) or if they had measles IgG [
1]. Similarly, healthcare workers were considered immune to VZV if they received two doses of the VZV vaccine or were able to show laboratory evidence of immunity [
1]. Commercial VZV IgG ELISAs are used for screening of VZV immunity. Both VZV-specific antibodies and VZV-specific T cells generated after primary VZV infection or vaccination confer immunity. While VZV IgG prevents primary VZV infection upon exogenous re-exposure of the virus, VZV-specific T cells limits severity, prevents reactivation, and aids in recovery of the disease [
16,
17,
18].
The high vaccination uptake rate can be attributed to several intrinsic and extrinsic factors. During the implementation phase of the program, measures were taken to address potential challenges such as vaccine hesitancy and the requirement for additional manpower and laboratory resources.
At a personal level, all staff was individually counseled by an occupational health doctor on the indications of vaccination against MMR and varicella. The personalized one-on-one interaction between the occupational health doctor and staff was identified as an important factor to reduce potential hesitancy towards vaccination [
19,
20,
21]. Strong emphasis was placed on the benefits, effectiveness, and safety profile of the vaccines since knowledge on the benefits and safety of a vaccine was important to increase vaccination uptake [
22,
23,
24,
25]. The healthcare workers were generally receptive to MMR and VZV vaccination. A personal sense of professional responsibility among the healthcare workers towards their patients could have also contributed to the high vaccination uptake [
21,
22,
25,
26].
Information about the vaccination program was disseminated to the staff from the head of the department and senior colleagues in the same department. Support from senior colleagues and peers can positively influence the healthcare workers to undergo vaccination [
27,
28].
The vaccination program was supported by the hospital’s management, as part of infection prevention measures for both staff and patients. The cost of serological tests and vaccines were borne by the hospital, eliminating financial burden as a potential barrier to vaccination. With the support of the hospital’s management, additional manpower was assigned to assist the vaccination program as required.
Departments were allocated staggered immunization review timings to ensure a smooth vaccination process without significant disruption to the clinical operations. The arrangement with different departments increased vaccine accessibility to the staff who otherwise might encounter difficulty finding additional time in their schedule to attend the vaccination session. A well-organized hospital-based vaccination program can encourage vaccination uptake among its staff [
28,
29].
The vaccination program was also given an adequate timeline for completion, to prevent overloading of cases seen at the occupational health clinic and overloading of serological testing at the laboratory. The systematic approach utilized ensured a high immunity coverage against the measles virus and VZV within an acceptable period, without needing a large number of additional manpower to complete the program. Priority was given to healthcare workers taking care of susceptible patients (e.g., patients at oncology wards, pediatric wards) and staff working in areas with high infectious disease exposure risk.
The benefits of vaccination against the measles virus and VZV have been extensively published and agreed upon. Prevention of nosocomial disease transmission among healthcare workers and patients remains the primary objective of vaccination amongst healthcare workers [
30]. Vaccination against vaccine-preventable diseases will also reduce perceived susceptibility and provide mental assurance among healthcare workers [
21]. Vaccination prevents large-scale outbreaks by reducing the number of nosocomial infections transmitted from infected healthcare workers [
9]. The wards in our hospital can accommodate up to eight beds per room. An infectious disease outbreak such as measles or varicella in wards with multiple beds in a room can be a major event, with numerous patients and healthcare workers potentially exposed to the disease. Investigation and control of a large infectious disease outbreak in a hospital are costly and result in many work-hours lost [
5,
7,
31].
Following the increase in vaccination coverage, the proportion of healthcare workers assessed at the occupational health clinic and the proportion of susceptible healthcare workers exposed to measles, varicella, and disseminated zoster significantly fell. The hospital’s Epidemiology Unit was able to quickly verify the immunity status of exposed staff during the contact tracing process due to the updated immunization records. Fewer healthcare workers without immunization status were reviewed at the occupational health clinic, resulting in a reduction of manpower resources, cost, and time spent identifying and assessing the affected staff. Each medical evaluation session for a healthcare worker exposed to measles, varicella, or disseminated herpes zoster takes approximately 30 min at the occupational health clinic.
Disruption to operations will be minimized and substantial time savings can be gained as a result of high vaccination coverage. In a department with multiple exposed staff members, a high immunity level will ensure that the healthcare workers are not susceptible and be put on medical leave during the incubation period of the disease. A cost-benefit analysis may be useful to demonstrate the resource savings in the long-term period.
5. Conclusions
Vaccination against vaccine-preventable diseases such as varicella and measles are beneficial for healthcare workers. A suitable implementation framework, such as the CFIR may be utilized to review various aspects of a vaccination program. In a healthcare setting without significant disease outbreaks, a vaccination program against varicella and measles can be paced, with prioritization for staff working with susceptible patients and staff with higher exposure risk.
Updated immunization records of healthcare workers will enable efficient epidemiological investigation and management of healthcare workers exposed to measles and varicella infections. Fewer healthcare workers will be required to undergo urgent immunity assessment following exposure to measles or varicella, and the number of susceptible healthcare workers will be significantly reduced. In addition to reducing the risk of infection to healthcare workers and patients under their care, disruption to operations will be minimized and substantial resource savings may be gained in the long run.
Author Contributions
Conceptualization, A.S.T.L. and S.M.L.; methodology, A.S.T.L.; software, A.S.T.L.; formal analysis, A.S.T.L.; investigation, R.S.; resources, R.S.; data curation, R.S.; writing—original draft preparation, A.S.T.L.; writing—review and editing, R.S. and S.M.L.; visualization, A.S.T.L.; supervision, S.M.L.; project administration, S.M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study approved by the Institutional Review Board of National Healthcare Group, Domain-Specific Review Board, for exemption of a formal review (Ref: 2019/01053 2 January 2020).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are not publicly available due to institutional restrictions.
Acknowledgments
We would like to thank the hospital’s management and all the staff at the Occupational Health Clinic for their support and successful implementation of the vaccination program from 2016 to 2018. We would also like to thank the staff at the Epidemiology Unit for providing us with the data from their epidemiological investigations of measles, varicella, and disseminated herpes zoster cases in the hospital.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Advisory Committee on Immunization Practices and Centers for Disease Control and Prevention (CDC). Immunization of health-care personnel: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2011, 60, 1–45. [Google Scholar]
- Paules, C.I.; Marston, H.D.; Fauci, A.S. Measles in 2019—Going Backward. N. Engl. J. Med. 2019, 380, 2185–2187. [Google Scholar] [CrossRef]
- Heininger, U.; Seward, J.F. Varicella. Lancet 2006, 368, 1365–1376. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.I. Clinical practice: Herpes zoster. N. Engl. J. Med. 2013, 369, 255–263. [Google Scholar] [CrossRef]
- Yang, J.; Liu, J.; Xing, F.; Ye, H.; Dai, G.; Liu, M.; Lo, S.K.-F.; Lau, R.W.-T.; Chiu, K.H.-Y.; Chan, J.F.-W.; et al. Nosocomial transmission of chickenpox and varicella zoster virus seroprevalence rate amongst healthcare workers in a teaching hospital in China. BMC Infect. Dis. 2019, 19, 582. [Google Scholar] [CrossRef] [PubMed]
- Barbadoro, P.; Marigliano, A.; Di Tondo, E.; De Paolis, M.; Martini, E.; Prospero, E.; D’Errico, M.M.P. Measles among healthcare workers in a teaching hospital in central Italy. J. Occup. Health 2012, 54, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Faoagali, J.L.; Darcy, D. Chickenpox outbreak among the staff of a large, urban adult hospital: Costs of monitoring and control. Am. J. Infect. Control. 1995, 23, 247–250. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Wicker, S. Measles in health-care settings. Am. J. Infect. Control 2013, 41, 661–663. [Google Scholar] [CrossRef]
- Baxi, R.; Mytton, O.T.; Abid, M.; Maduma-Butshe, A.; Iyer, S.; Ephraim, A.; Brown, K.E.; O’Moore, É. Outbreak report: Nosocomial transmission of measles through an unvaccinated healthcare worker—Implications for public health. J. Public Health 2014, 36, 375–381. [Google Scholar] [CrossRef]
- Moss, W.J.; Griffin, D.E. Measles. Lancet 2012, 379, 153–164. [Google Scholar] [CrossRef]
- World Health Organization. Varicella and herpes zoster vaccines: WHO position paper, June 2014—Recommendation. Vaccine 2016, 34, 198–199. [Google Scholar] [CrossRef]
- Wutzler, P.; Bonanni, P.; Burgess, M.; Gershon, A.; Sáfadi, M.A.; Casabona, G. Varicella vaccination-the global experience. Expert Rev. Vaccines 2017, 16, 833–843. [Google Scholar] [CrossRef]
- Ministry of Health Singapore. Immunisation of Healthcare Workers—Latest Recommendations; MOH Circular No. 41/2018; Ministry of Health Singapore: Singapore, 2018.
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 1–15. [Google Scholar] [CrossRef]
- Constructs—The Consolidated Framework for Implementation Research. Available online: https://cfirguide.org/constructs/ (accessed on 8 March 2022).
- Weinberg, A.; Levin, M.J. VZV T Cell-Mediated Immunity BT—Varicella-zoster Virus; Abendroth, A., Arvin, A.M., Moffat, J.F., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; pp. 341–357. [Google Scholar]
- Laing, K.J.; Ouwendijk, W.J.D.; Koelle, D.M.; Verjans, G.M.G.M. Immunobiology of Varicella-Zoster Virus Infection. J. Infect. Dis. 2018, 218, S68–S74. [Google Scholar] [CrossRef]
- Arvin, A.M. Humoral and Cellular Immunity to Varicella-Zoster Virus: An Overview. J. Infect. Dis. 2008, 197, S58–S60. [Google Scholar] [CrossRef]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef]
- Dubé, È.; Ward, J.K.; Verger, P.; MacDonald, N.E. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu. Rev. Public Health 2021, 42, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Doornekamp, L.; van Leeuwen, L.; van Gorp, E.; Voeten, H.; Goeijenbier, M. Determinants of Vaccination Uptake in Risk Populations: A Comprehensive Literature Review. Vaccines 2020, 8, 480. [Google Scholar] [CrossRef] [PubMed]
- Little, K.E.; Goodridge, S.; Lewis, H.; Lingard, S.W.; Din, S.; Tidley, M.; Roberts, R.J.; Williams, N.S.; Hayes, S. Occupational vaccination of health care workers: Uptake, attitudes and potential solutions. Public Health 2015, 129, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Harrison, N.; Brand, A.; Forstner, C.; Tobudic, S.; Burgmann, K.; Burgmann, H. Knowledge, risk perception and attitudes toward vaccination among Austrian health care workers: A cross-sectional study. Hum. Vaccines Immunother. 2016, 12, 2459–2463. [Google Scholar] [CrossRef] [PubMed]
- Verger, P.; Botelho-Nevers, E.; Garrison, A.; Gagnon, D.; Gagneur, A.; Gagneux-Brunon, A.; Dubé, E. Vaccine hesitancy in health-care providers in Western countries: A narrative review. Expert Rev. Vaccines 2022, 21, 909–927. [Google Scholar] [CrossRef]
- Truong, J.; Bakshi, S.; Wasim, A.; Ahmad, M.; Majid, U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot. Int. 2022, 37, daab105. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Poland, G.A. Immunization of Health-Care Providers: Necessity and Public Health Policies. Healthcare 2016, 4, 47. [Google Scholar] [CrossRef]
- Corace, K.; Prematunge, C.; McCarthy, A.; Nair, R.C.; Roth, V.; Hayes, T.; Suh, K.N.; Balfour, L.; Garber, G. Predicting influenza vaccination uptake among health care workers: What are the key motivators? Am. J. Infect. Control. 2013, 41, 679–684. [Google Scholar] [CrossRef]
- Boey, L.; Bral, C.; Roelants, M.; De Schryver, A.; Godderis, L.; Hoppenbrouwers, K.; Vandermeulen, C. Attitudes, believes, determinants and organisational barriers behind the low seasonal influenza vaccination uptake in healthcare workers—A cross-sectional survey. Vaccine 2018, 36, 3351–3358. [Google Scholar] [CrossRef] [PubMed]
- Taddei, C.; Ceccherini, V.; Niccolai, G.; Porchia, B.R.; Boccalini, S.; Levi, M.; Tiscione, E.; Santini, M.G.; Baretti, S.; Bonanni, P.; et al. Attitude toward immunization and risk perception of measles, rubella, mumps, varicella, and pertussis in health care workers working in 6 hospitals of Florence, Italy 2011. Hum. Vaccin. Immunother. 2014, 10, 2612. [Google Scholar] [CrossRef] [PubMed]
- Torner, N.; Solano, R.; Rius, C. Human Vaccines & Immunotherapeutics Implication of health care personnel in measles transmission the need for updated immunization status in the move towards eradication of measles in Catalonia. Vaccines Immunother. 2015, 11, 288–292. [Google Scholar] [CrossRef]
- Pike, J.; Leidner, A.J.; Gastañaduy, P.A. A Review of Measles Outbreak Cost Estimates from the United States in the Posteliminatiofroma (2004–2017): Estimates by Perspective and Cost Type. Clin. Infect. Dis. 2020, 71, 1568–1576. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).